Correlation of vitamin D level with the clinical-radiological severity of COVID-19 in geriatric patients
et al., Journal of Health Sciences and Medicine, doi:10.32322/jhsm.1063405, May 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
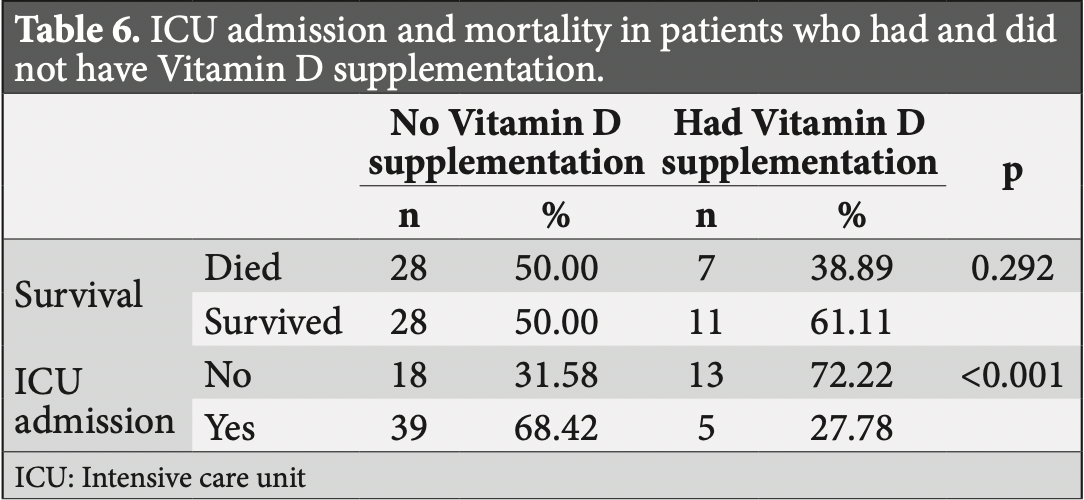
Retrospective 75 patients in Turkey showing lower ICU admission with vitamin D treatment in unadjusted results subject to confounding by time and indication (treatment was given to patients with low levels and only during a certain period). There was no significant difference in outcomes based on vitamin D levels.
Cholecalciferol was used in this study.
Meta-analysis shows that late stage treatment with calcitriol / calcifediol (or
paricalcitol, alfacalcidol, etc.) is more effective than cholecalciferol: 66% [47‑78%] lower risk vs. 45% [34‑54%] lower risk.
Cholecalciferol requires two hydroxylation steps to become activated - first
in the liver to calcifediol, then in the kidney to calcitriol. Calcitriol,
paricalcitol, and alfacalcidol are active vitamin D analogs that do not
require conversion. This allows them to have more rapid onset of action
compared to cholecalciferol. The time delay for cholecalciferol to increase
serum calcifediol levels can be 2-3 days, and the delay for converting
calcifediol to active calcitriol can be up to 7 days.
Bolus treatment is less effective.
Pharmacokinetics and the potential side effects of high bolus doses suggest
that ongoing treatment spread over time is more appropriate.
Research has confirmed that lower dose regular treatment with vitamin D is more
effective than intermittent high-dose bolus treatment for various conditions,
including rickets and acute respiratory infections1,2. The biological mechanisms supporting these
findings involve the induction of enzymes such as 24-hydroxylase and
fibroblast growth factor 23 (FGF23) by high-dose bolus treatments. These
enzymes play roles in inactivating vitamin D, which can paradoxically reduce
levels of activated vitamin D and suppress its activation for extended periods
post-dosage. Evidence indicates that 24-hydroxylase activity may remain
elevated for several weeks following a bolus dose, leading to reduced levels
of the activated form of vitamin D. Additionally, FGF23 levels can increase
for at least three months after a large bolus dose, which also contributes to
the suppression of vitamin D activation1.
This is the 85th of 135 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
40 studies are RCTs, which show efficacy with p=0.0000001.
|
risk of death, 22.2% lower, RR 0.78, p = 0.43, treatment 7 of 18 (38.9%), control 28 of 56 (50.0%), NNT 9.0, excluded in exclusion analyses:
unadjusted results with no group details; significant confounding by time possible due to separation of groups in different time periods.
|
|
risk of ICU admission, 59.4% lower, RR 0.41, p = 0.005, treatment 5 of 18 (27.8%), control 39 of 57 (68.4%), NNT 2.5, excluded in exclusion analyses:
unadjusted results with no group details; significant confounding by time possible due to separation of groups in different time periods.
|
|
risk of death, 8.0% higher, RR 1.08, p = 0.80, high D levels (≥20ng/mL) 11 of 20 (55.0%), low D levels (<20ng/mL) 28 of 55 (50.9%), outcome based on serum levels.
|
|
risk of ICU admission, 4.8% lower, RR 0.95, p = 1.00, high D levels (≥20ng/mL) 9 of 20 (45.0%), low D levels (<20ng/mL) 26 of 55 (47.3%), NNT 44, outcome based on serum levels.
|
|
risk of progression, 6.1% lower, RR 0.94, p = 0.77, high D levels (≥20ng/mL) 14 of 20 (70.0%), low D levels (<20ng/mL) 41 of 55 (74.5%), NNT 22, severe/critical, outcome based on serum levels.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Baykal et al., 30 May 2022, retrospective, Turkey, peer-reviewed, 2 authors, study period 1 April, 2020 - 1 March, 2021, dosage 300,000IU single dose.
Contact: drhusnubaykal@hotmail.com.
Correlation of vitamin D level with the clinical-radiological severity of COVID-19 in geriatric patients
Journal of Health Sciences and Medicine, doi:10.32322/jhsm.1063405
Objective: This study was planned to investigate the effect of 25-OH-Vitamin D (Vit D) deficiency on clinical and radiological findings of coronavirus disease-2019 (COVID-19) in geriatric patients hospitalized due to COVID-19. Material and Method: Seventy-five patients who were treated for COVID-19 were reviewed retrospectively, and grouped in relation with their ages [(1) 65-74, (2) 75-84, (3) >84 years] and the severity of Vit D deficiency [(1) severe deficiency: <10 ng/ mL, (2) moderate deficiency: 10-20 ng/mL, (3) minor deficiency: 21-30 ng/mL, (4) normal: >30 ng/mL]. The complaints on admission, comorbidities, intensive care unit (ICU) need, length of hospital stay, laboratory data, and mortality of the ones who had and did not have Vit D replacement (n=18/75) were recorded. The patients were analyzed for COVID-19 severity using radiological and clinical markers. Results: Moderate Vit D deficiency (10-20 ng/mL) was frequently detected. When the disease severity and Vit D levels were analyzed, it was found that the disease was more severe (46.6%) in the Vit D <10 ng/ml group, and milder (37.5%) in the >30 ng/ml group, but there was no statistically significant difference among the groups. Low or high Vit D levels did not show any significant correlations with the severity of pneumonia or the thorax CT findings. The intensive care unit (ICU) admission rate was significantly lower in those who had Vit D replacement (p<0.001).
Conclusion: The ICU admission rate was lower in patients who had Vit D replacement, however, serum Vit D concentrations were not correlated with COVID-19 severity or mortality risk.
References
Annweiler, Corvaisier, Gautier, Vitamin D supplementation associated to better survival in hospitalized frail elderly COVID-19 patients: The GERIA-COVID quasiexperimental study, Nutrients
Baktash, Hosack, Patel, Vitamin D status and outcomes for hospitalized older patients with COVID-19, Postgrad Med J
Bassatne, Basbous, Chakhtoura, El Zein, Rahme et al., The link between COVID-19 and Vitamin D (VIVID): a systematic review and meta-analysis, Metabolism
Bertoldi, Gianesello, Calò, Letter: ACE2, Rho kinase inhibition and the potential role of vitamin D against COVID-19, Aliment Pharmacol Ther
Bulut, Karamanlı, Şahin, Çelik, Biber, Association between vitamin D levels and frequency of disease exacerbations and hospitalizations in patients with COPD, J Health Sci Med
Cereda, Bogliolo, Klersy, Lobascio, Masi et al., Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital, Clin Nutr
Cheng, Du, Hong, Factors associated to serum 25-hydroxyvitamin D levels among older adult populations in urban and suburban communities in Shanghai, China, BMC Geriatr
Daneshkhah, Agrawal, Eshein, Subramanian, Roy et al., Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients, Aging Clin Exp Res
Ebadi, Montano-Loza, Perspective: improving vitamin D status in the management of COVID-19, Eur J Clin Nutr
Glinsky, Tripartite combination of candidate pandemic mitigation agents: vitamin D, Quercetin, and Estradiol manifest properties of medicinal agents for targeted mitigation of the COVID-19 pandemic defined by genomics-guided tracing of SARS-CoV-2 targets in human cells, Biomedicines
Grant, Lahore, Mcdonnell, Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients
Hanley, Cranney, Jones, Guidelines committee of the scientific advisory council of osteoporosis Canada. Vitamin D in adult health and disease: a review and guideline statement from Osteoporosis Canada, CMAJ
Hastie, Mackay, Ho, Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr
Hastie, Pell, Sattar, Vitamin D and COVID-19 infection and mortality in UK Biobank, Eur J Nutr
Hernandez, Nan, Fernandez-Ayala, Garcia-Unzueta, Hernandez-Hernandez et al., Vitamin D status in hospitalized patients with SARS-CoV-2 infection, J Clin Endocrinol Metab
Huang, Wang, Li, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin Exp Res
Im, Je, Baek, Chung, Kwon et al., Nutritional status of patients with COVID-19, Int J Infect Dis
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers, Sci Rep
Kweder, Eidi, Vitamin D deficiency in elderly: Risk factors and drugs impact on vitamin D status, Avicenna J Med
Maghbooli, Sahraian, Ebrahimi, Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection, PLoS One
Murai, Fernandes, Sales, Pinto, Goessler et al., Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial, JAMA
Ohaegbulam, Swalih, Patel, Smith, Perrin, Vitamin D supplementation in COVID-19 patients: a clinical case series, Am J Ther
Oscanoa, Amado, Vidal, Laird, Ghashut et al., The relationship between the severity and mortality of SARS-CoV-2 infection and 25-hydroxyvitamin D concentration-a metaanalysis, Adv Respir Med
Panagiotou, Tee, Ihsan, Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity, Clin Endocrinol (Oxf)
Rhodes, Subramanian, Laird, Griffin, Kenny, Perspective: Vitamin D deficiency and COVID-19 severityplausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis, J Intern Med
Sassi, Tamone, Amelio, Vitamin D: nutrient, hormone, and immunomodulator, Nutrients
Shah, Saxena, Mavalankar, Vitamin D supplementation, COVID-19 and disease severity: a meta-analysis, QJM
Simpson, Kay, Abbara, Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA-Secondary Publication, J Thorac Imaging
Sloka, Silva, Wang, Yong, Predominance of Th2 polarization by vitamin D through a STAT6-dependent mechanism, J Neuroinflammation
Smet, Smet, Herroelen, Gryspeerdt, Martens, Serum 25(OH)D level on hospital admission associated with COVID-19 stage and mortality, Am J Clin Pathol
Sulli, Gotelli, Casabella, Vitamin D and lung outcomes in elderly COVID-19 patients, Nutrients
Tan, Ho, Kalimuddin, Cherng, Teh et al., A cohort study to evaluate the effect of combination Vitamin D, Magnesium and Vitamin B12 (DMB) on progression to severe outcome in older COVID-19 patients, medRxiv
Wyskida, Wieczorowska-Tobis, Chudek, Prevalence and factors promoting the occurrence of vitamin D deficiency in the elderly, Postepy Hig Med Dosw (Online
Yildiz, Senel, Kavurgaci, Ozturk, Ozturk, The prognostic significance of vitamin D deficiency in patients with COVID-19 pneumonia, Bratisl Lek Listy
Zhao, Cytokine storm and immunomodulatory therapy in COVID-19: Role of chloroquine and anti-IL-6 monoclonal antibodies, Int J Antimicrob Agents
DOI record:
{
"DOI": "10.32322/jhsm.1063405",
"ISSN": [
"2636-8579"
],
"URL": "http://dx.doi.org/10.32322/jhsm.1063405",
"abstract": "<jats:p xml:lang=\"en\">Objective: This study was planned to investigate the effect of 25-OH-Vitamin D (Vit D) deficiency on clinical and radiological findings of coronavirus disease-2019 (COVID-19) in geriatric patients hospitalized due to COVID-19.
\nMaterial and Method: Seventy-five patients who were treated for COVID-19 were reviewed retrospectively, and grouped in relation with their ages [(1) 65-74, (2) 75-84, (3) >84 years] and the severity of Vit D deficiency [(1) severe deficiency: 30 ng/mL]. The complaints on admission, comorbidities, intensive care unit (ICU) need, length of hospital stay, laboratory data, and mortality of the ones who had and did not have Vit D replacement (n=18/75) were recorded. The patients were analyzed for COVID-19 severity using radiological and clinical markers. 
\nResults: Moderate Vit D deficiency (10-20 ng/mL) was frequently detected. When the disease severity and Vit D levels were analyzed, it was found that the disease was more severe (46.6%) in the Vit D 30 ng/ml group, but there was no statistically significant difference among the groups. Low or high Vit D levels did not show any significant correlations with the severity of pneumonia or the thorax CT findings. The intensive care unit (ICU) admission rate was significantly lower in those who had Vit D replacement (p</jats:p>",
"accepted": {
"date-parts": [
[
2022,
4,
4
]
]
},
"author": [
{
"affiliation": [
{
"name": "SAĞLIK BİLİMLERİ ÜNİVERSİTESİ, ANKARA ATATÜRK GÖĞÜS HASTALIKLARI VE GÖĞÜS CERRAHİSİ SAĞLIK UYGULAMA VE ARAŞTIRMA MERKEZİ, DAHİLİ TIP BİLİMLERİ BÖLÜMÜ, GÖĞÜS HASTALIKLARI ANABİLİM DALI"
}
],
"family": "BAYKAL",
"given": "Hüsnü",
"sequence": "first"
},
{
"affiliation": [
{
"name": "SAĞLIK BİLİMLERİ ÜNİVERSİTESİ, ANKARA ATATÜRK GÖĞÜS HASTALIKLARI VE GÖĞÜS CERRAHİSİ SAĞLIK UYGULAMA VE ARAŞTIRMA MERKEZİ, DAHİLİ TIP BİLİMLERİ BÖLÜMÜ, GÖĞÜS HASTALIKLARI ANABİLİM DALI"
}
],
"family": "ÜLGER",
"given": "Ayşe Füsun",
"sequence": "additional"
}
],
"container-title": "Journal of Health Sciences and Medicine",
"container-title-short": "J Health Sci Med / JHSM",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
5,
31
]
],
"date-time": "2022-05-31T09:48:02Z",
"timestamp": 1653990482000
},
"deposited": {
"date-parts": [
[
2022,
5,
31
]
],
"date-time": "2022-05-31T09:48:18Z",
"timestamp": 1653990498000
},
"indexed": {
"date-parts": [
[
2022,
7,
9
]
],
"date-time": "2022-07-09T13:37:50Z",
"timestamp": 1657373870418
},
"is-referenced-by-count": 0,
"issue": "3",
"issued": {
"date-parts": [
[
2022,
5,
30
]
]
},
"journal-issue": {
"issue": "3",
"published-online": {
"date-parts": [
[
2022,
5,
30
]
]
}
},
"language": "en",
"member": "17352",
"original-title": [],
"page": "771-777",
"prefix": "10.32322",
"published": {
"date-parts": [
[
2022,
5,
30
]
]
},
"published-online": {
"date-parts": [
[
2022,
5,
30
]
]
},
"publisher": "Journal of Health Sciences and Medicine",
"reference": [
{
"DOI": "10.3390/biomedicines8050129",
"doi-asserted-by": "crossref",
"key": "ref1",
"unstructured": "Glinsky GV. Tripartite combination of candidate pandemic mitigation agents: vitamin D, Quercetin, and Estradiol manifest properties of medicinal agents for targeted mitigation of the COVID-19 pandemic defined by genomics-guided tracing of SARS-CoV-2 targets in human cells. Biomedicines 2020; 8: 129."
},
{
"DOI": "10.1007/s40520-020-01570-8",
"doi-asserted-by": "crossref",
"key": "ref2",
"unstructured": "Ilie PC, Stefanescu S, Smith L. The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality. Aging Clin Exp Res 2020; 32: 1195-98."
},
{
"DOI": "10.3390/nu12113377",
"doi-asserted-by": "crossref",
"key": "ref3",
"unstructured": "Annweiler G, Corvaisier M, Gautier J, et al. Vitamin D supplementation associated to better survival in hospitalized frail elderly COVID-19 patients: The GERIA-COVID quasi-experimental study. Nutrients 2020; 12: 3377."
},
{
"DOI": "10.2903/j.efsa.2010.1468",
"doi-asserted-by": "crossref",
"key": "ref4",
"unstructured": "EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). Scientific Opinion on the substantiation of health claims related to vitamin D and normal function of the immune system and inflammatory response (ID 154, 159), maintenance of normal muscle function (ID 155) and maintenance of normal cardiovascular function (ID 159) pursuant to Article 13(1) of Regulation (EC) No 1924/2006. EFSA J 2010; 8: 1-17."
},
{
"DOI": "10.3390/nu10111656",
"doi-asserted-by": "crossref",
"key": "ref5",
"unstructured": "Sassi F, Tamone C, D'Amelio P. Vitamin D: nutrient, hormone, and immunomodulator. Nutrients 2018; 10: 1656."
},
{
"DOI": "10.3390/nu12040988",
"doi-asserted-by": "crossref",
"key": "ref6",
"unstructured": "Grant WB, Lahore H, McDonnell SL, et al. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients 2020; 12: 988."
},
{
"DOI": "10.1186/1742-2094-8-56",
"doi-asserted-by": "crossref",
"key": "ref7",
"unstructured": "Sloka S, Silva C, Wang J, Yong VW. Predominance of Th2 polarization by vitamin D through a STAT6-dependent mechanism. J Neuroinflammation 2011; 8: 56."
},
{
"DOI": "10.1111/apt.15895",
"doi-asserted-by": "crossref",
"key": "ref8",
"unstructured": "Bertoldi G, Gianesello L, Calò LA. Letter: ACE2, Rho kinase inhibition and the potential role of vitamin D against COVID-19. Aliment Pharmacol Ther 2020; 52: 577-8."
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"doi-asserted-by": "crossref",
"key": "ref9",
"unstructured": "Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497-506."
},
{
"DOI": "10.1007/s40520-020-01677-y",
"doi-asserted-by": "crossref",
"key": "ref10",
"unstructured": "Daneshkhah A, Agrawal V, Eshein A, Subramanian H, Roy HK, Backman V. Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients. Aging Clin Exp Res 2020; 32: 2141-58."
},
{
"DOI": "10.1111/joim.13149",
"doi-asserted-by": "crossref",
"key": "ref11",
"unstructured": "Rhodes JM, Subramanian S, Laird E, Griffin G, Kenny RA. Perspective: Vitamin D deficiency and COVID-19 severity-plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis. J Intern Med 2021; 289: 97-115."
},
{
"DOI": "10.5604/01.3001.0010.3804",
"doi-asserted-by": "crossref",
"key": "ref12",
"unstructured": "Wyskida M, Wieczorowska-Tobis K, Chudek J. Prevalence and factors promoting the occurrence of vitamin D deficiency in the elderly. Postepy Hig Med Dosw (Online) 2017; 71: 198-204."
},
{
"DOI": "10.1186/s12877-017-0632-z",
"doi-asserted-by": "crossref",
"key": "ref13",
"unstructured": "Cheng Q, Du Y, Hong W, et al. Factors associated to serum 25-hydroxyvitamin D levels among older adult populations in urban and suburban communities in Shanghai, China. BMC Geriatr 2017; 17: 246."
},
{
"DOI": "10.1016/j.ijantimicag.2020.105982",
"doi-asserted-by": "crossref",
"key": "ref14",
"unstructured": "Zhao M. Cytokine storm and immunomodulatory therapy in COVID-19: Role of chloroquine and anti-IL-6 monoclonal antibodies. Int J Antimicrob Agents 2020; 55: 105982."
},
{
"DOI": "10.1038/s41430-020-0661-0",
"doi-asserted-by": "crossref",
"key": "ref15",
"unstructured": "Ebadi M, Montano-Loza AJ. Perspective: improving vitamin D status in the management of COVID-19. Eur J Clin Nutr 2020; 74: 856-9."
},
{
"DOI": "10.1016/j.ijid.2020.08.018",
"doi-asserted-by": "crossref",
"key": "ref16",
"unstructured": "Im JH, Je YS, Baek J, Chung MH, Kwon HY, Lee JS. Nutritional status of patients with COVID-19. Int J Infect Dis 2020; 100: 390-3."
},
{
"DOI": "10.1371/journal.pone.0239799",
"doi-asserted-by": "crossref",
"key": "ref17",
"unstructured": "Maghbooli Z, Sahraian MA, Ebrahimi M, et al. Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection. PLoS One 2020; 15: e0239799."
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"doi-asserted-by": "crossref",
"key": "ref18",
"unstructured": "Hastie CE, Mackay DF, Ho F, et al. Vitamin D concentrations and COVID-19 infection in UK Biobank. Diabetes Metab Syndr 2020; 14: 561-5."
},
{
"DOI": "10.5603/ARM.a2021.0037",
"doi-asserted-by": "crossref",
"key": "ref19",
"unstructured": "Oscanoa TJ, Amado J, Vidal X, Laird E, Ghashut RA, Romero-Ortuno R. The relationship between the severity and mortality of SARS-CoV-2 infection and 25-hydroxyvitamin D concentration-a metaanalysis. Adv Respir Med 2021; 89: 145-57."
},
{
"DOI": "10.4149/BLL_2021_119",
"doi-asserted-by": "crossref",
"key": "ref20",
"unstructured": "Yildiz M, Senel MU, Kavurgaci S, Ozturk FE, Ozturk A. The prognostic significance of vitamin D deficiency in patients with COVID-19 pneumonia. Bratisl Lek Listy 2021; 122: 744-7."
},
{
"DOI": "10.1007/s00394-020-02372-4",
"doi-asserted-by": "crossref",
"key": "ref21",
"unstructured": "Hastie CE, Pell JP, Sattar N. Vitamin D and COVID-19 infection and mortality in UK Biobank. Eur J Nutr 2021; 60: 545-8."
},
{
"DOI": "10.4103/ajm.AJM_20_18",
"doi-asserted-by": "crossref",
"key": "ref22",
"unstructured": "Kweder H, Eidi H. Vitamin D deficiency in elderly: Risk factors and drugs impact on vitamin D status. Avicenna J Med 2018; 8: 139-46."
},
{
"DOI": "10.1503/cmaj.080663",
"doi-asserted-by": "crossref",
"key": "ref23",
"unstructured": "Hanley DA, Cranney A, Jones G, et al; Guidelines committee of the scientific advisory council of osteoporosis Canada. Vitamin D in adult health and disease: a review and guideline statement from Osteoporosis Canada. CMAJ 2010; 182: E610-8."
},
{
"DOI": "10.1097/RTI.0000000000000524",
"doi-asserted-by": "crossref",
"key": "ref24",
"unstructured": "Simpson S, Kay FU, Abbara S, et al. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA-Secondary Publication. J Thorac Imaging 2020; 35: 219-27."
},
{
"DOI": "10.32322/jhsm.1050722",
"doi-asserted-by": "crossref",
"key": "ref25",
"unstructured": "Bulut S, Karamanlı H, Şahin ME, Çelik D, Biber Ç. Association between vitamin D levels and frequency of disease exacerbations and hospitalizations in patients with COPD. J Health Sci Med 2022; 5: 471-7."
},
{
"DOI": "10.1093/ajcp/aqaa252",
"doi-asserted-by": "crossref",
"key": "ref26",
"unstructured": "De Smet D, De Smet K, Herroelen P, Gryspeerdt S, Martens GA. Serum 25(OH)D level on hospital admission associated with COVID-19 stage and mortality. Am J Clin Pathol 2021; 155: 381-8."
},
{
"DOI": "10.1016/j.metabol.2021.154753",
"doi-asserted-by": "crossref",
"key": "ref27",
"unstructured": "Bassatne A, Basbous M, Chakhtoura M, El Zein O, Rahme M, El-Hajj Fuleihan G. The link between COVID-19 and Vitamin D (VIVID): a systematic review and meta-analysis. Metabolism 2021; 119: 154753."
},
{
"DOI": "10.1136/postgradmedj-2020-138712",
"doi-asserted-by": "crossref",
"key": "ref28",
"unstructured": "Baktash V, Hosack T, Patel N, et al. Vitamin D status and outcomes for hospitalized older patients with COVID-19. Postgrad Med J 2021; 97: 442-7."
},
{
"DOI": "10.3390/nu13030717",
"doi-asserted-by": "crossref",
"key": "ref29",
"unstructured": "Sulli A, Gotelli E, Casabella A, et al. Vitamin D and lung outcomes in elderly COVID-19 patients. Nutrients 2021; 13: 717."
},
{
"DOI": "10.1016/j.clnu.2020.10.055",
"doi-asserted-by": "crossref",
"key": "ref30",
"unstructured": "Cereda E, Bogliolo L, Klersy C, Lobascio F, Masi S, Crotti S. Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital. Clin Nutr 2021; 40: 2469-72."
},
{
"DOI": "10.1210/clinem/dgaa733",
"doi-asserted-by": "crossref",
"key": "ref31",
"unstructured": "Hernandez JL, Nan D, Fernandez-Ayala M, Garcia-Unzueta M, Hernandez-Hernandez MA, Lopez-Hoyos M. Vitamin D status in hospitalized patients with SARS-CoV-2 infection. J Clin Endocrinol Metab 2021; 106: e1343. e135."
},
{
"DOI": "10.1038/s41598-020-77093-z",
"doi-asserted-by": "crossref",
"key": "ref32",
"unstructured": "Jain A, Chaurasia R, Sengar NS, Singh M, Mahor S, Narain S. Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers. Sci Rep 2020; 10: 1-8."
},
{
"DOI": "10.1097/MJT.0000000000001222",
"doi-asserted-by": "crossref",
"key": "ref33",
"unstructured": "Ohaegbulam KC, Swalih M, Patel P, Smith MA, Perrin R. Vitamin D supplementation in COVID-19 patients: a clinical case series. Am J Ther 2020; 27: e485-90."
},
{
"DOI": "10.1093/qjmed/hcab009",
"doi-asserted-by": "crossref",
"key": "ref34",
"unstructured": "Shah K, Saxena D, Mavalankar D. Vitamin D supplementation, COVID-19 and disease severity: a meta-analysis. QJM 2021; 114: 175-81."
},
{
"DOI": "10.1111/cen.14276",
"doi-asserted-by": "crossref",
"key": "ref35",
"unstructured": "Panagiotou G, Tee SA, Ihsan Y, et al. Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity. Clin Endocrinol (Oxf) 2020; 93: 508-11."
},
{
"DOI": "10.1101/2020.06.01.20112334",
"doi-asserted-by": "crossref",
"key": "ref36",
"unstructured": "Tan CW, Ho LP, Kalimuddin S, Cherng BPZ, Teh YE, Thien SY. A cohort study to evaluate the effect of combination Vitamin D, Magnesium and Vitamin B12 (DMB) on progression to severe outcome in older COVID-19 patients. medRxiv 2020"
},
{
"DOI": "10.1001/jama.2020.26848",
"doi-asserted-by": "crossref",
"key": "ref37",
"unstructured": "Murai IH, Fernandes AL, Sales LP, Pinto AJ, Goessler KF, Duran CS. Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial. JAMA 2021; 17: 2021."
}
],
"reference-count": 37,
"references-count": 37,
"relation": {},
"resource": {
"primary": {
"URL": "https://dergipark.org.tr/en/doi/10.32322/jhsm.1063405"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Correlation of vitamin D level with the clinical-radiological severity of COVID-19 in geriatric patients",
"type": "journal-article",
"volume": "5"
}
