The association between inflammatory and immune system biomarkers and the dietary inflammatory index in patients with COVID-19
et al., Frontiers in Nutrition, doi:10.3389/fnut.2023.1075061, Mar 2023
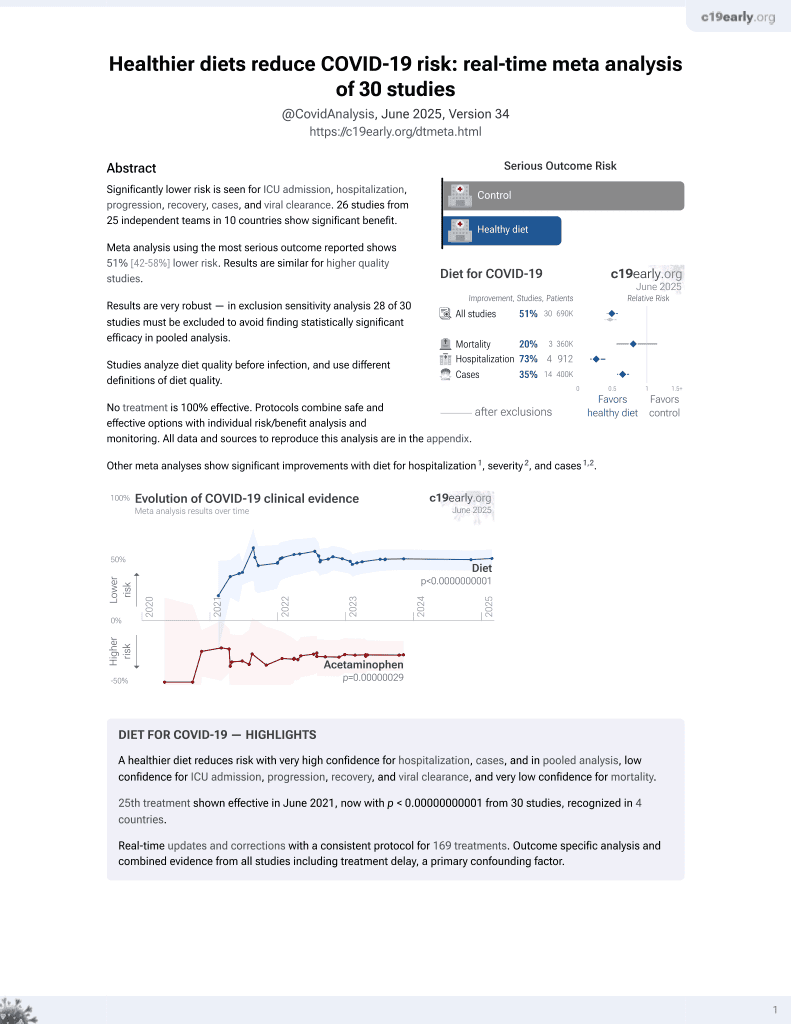
Diet for COVID-19
26th treatment shown to reduce risk in
June 2021, now with p < 0.00000000001 from 30 studies, recognized in 4 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 500 COVID-19 patients, showing dietary inflammatory index (DII) and energy-adjusted dietary inflammatory index (E-DII) associated with COVID-19 severity.
|
risk of ICU admission, 98.7% lower, RR 0.01, p < 0.001, higher quality diet 0 of 125 (0.0%), lower quality diet 37 of 125 (29.6%), NNT 3.4, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), DII, quartile I vs. quartile IV.
|
|
risk of ICU admission, 98.1% lower, RR 0.02, p < 0.001, higher quality diet 0 of 125 (0.0%), lower quality diet 26 of 125 (20.8%), NNT 4.8, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), E-DII, quartile I vs. quartile IV.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Barania Adabi et al., 31 Mar 2023, retrospective, Iran, peer-reviewed, survey, mean age 40.3, 5 authors, study period March 2021 - September 2021.
Contact: daneghian.s@umsu.ac.ir.
R and Shivappa N ( ) The association between inflammatory and immune system biomarkers and the dietary inflammatory index in patients with COVID-.
Ethics statement The studies involving human participants were reviewed and approved by the Ethics Committee of Urmia University of Medical Sciences, Urmia, Iran (Ethics Code IR.UMSU.REC.1399.367). The patients/participants provided their written informed consent to participate in this study.
Author contributions All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023. 1075061/full#supplementary-material
References
Aghababayan, Mobarakeh, Qorbani, Tiznobeyk, Aminianfar et al., Higher dietary inflammatory index scores are associated with increased odds of benign breast diseases in a case-control study, J Inflamm Res, doi:10.2147/JIR.S232157
Alley, Seeman, Kim, Karlamangla, Hu et al., Socioeconomic status and C-reactive protein levels in the US population: NHANES IV, Brain Behav Immun, doi:10.1016/j.bbi.2005.10.003
Aminnejad, Roumi, Ardekanizadeh, Vahid, Gholamalizadeh et al., Association of dietary antioxidant index with body mass index in adolescents, Obes Sci Pract, doi:10.1002/osp4.639
Bousquet, Anto, Iaccarino, Czarlewski, Haahtela et al., Is diet partly responsible for differences in COVID-19 death rates between and within countries?, Clin Transl Allergy, doi:10.1186/s13601-020-00323-0
Butler, Barrientos, The impact of nutrition on COVID-19 susceptibility and long-term consequences, Brain Behav Immun, doi:10.1016/j.bbi.2020.04.040
Bárcena, Quirós, Durand, Mayoral, Rodríguez et al., Methionine restriction extends lifespan in progeroid mice and alters lipid and bile acid metabolism, Cell Rep, doi:10.1016/j.celrep.2018.07.089
Cartier, Côté, Lemieux, Pérusse, Tremblay et al., Sex differences in inflammatory markers: what is the contribution of visceral adiposity?, Am J Clin Nutr, doi:10.3945/ajcn.2008.27030
Chait, Kim, Saturated fatty acids and inflammation: who pays the toll?, Arterioscler Thromb Vasc Biol, doi:10.1161/ATVBAHA.110.203984
Davillas, Benzeval, Kumari, Socio-economic inequalities in Creactive protein and fibrinogen across the adult age span: findings from Understanding Society, Sci Rep, doi:10.1038/s41598-017-02888-6
Doaei, Gholami, Rastgoo, Gholamalizadeh, Bourbour et al., The effect of omega-3 fatty acid supplementation on clinical and biochemical parameters of critically ill patients with COVID-19: a randomized clinical trial, J Transl Med, doi:10.1186/s12967-021-02795-5
Duntas, Selenium and inflammation: underlying anti-inflammatory mechanisms, Horm Metab Res, doi:10.1055/s-0029-1220724
Dwyer, Peterson, Tea and flavonoids: where we are, where to go next, Am J Clin Nutr, doi:10.3945/ajcn.113.059584
Ebrahimzadeh, Taghizadeh, Milajerdi, Major dietary patterns in relation to disease severity, symptoms, and inflammatory markers in patients recovered from COVID-19, Front Nutr, doi:10.3389/fnut.2022.929384
Ellulu, Rahmat, Patimah, Khaza'ai, Abed, Effect of vitamin C on inflammation and metabolic markers in hypertensive and/or diabetic obese adults: a randomized controlled trial, Drug Des Devel Ther, doi:10.2147/DDDT.S83144
Eva, Islam, Afrin, Islam, Bayazid, Role of dietary habit and nutritional status on the severity of COVID-19 treatment: a hospital based cross-sectional study, J Curr Med Pract
Faghfouri, Baradaran, Khabbazi, Bishak, Zarezadeh et al., Profiling inflammatory cytokines following zinc supplementation: a systematic review and meta-analysis of controlled trials, Br J Nutr, doi:10.1017/S0007114521000192
Faghfouri, Zarrin, Maleki, Payahoo, Khajebishak et al., A comprehensive mechanistic review insight into the effects of micronutrients on toll-like receptors functions, Pharmacol Res, doi:10.1017/S0007114511005460
Firoozi, Masoumi, Ranjbar, Shivappa, Hebert et al., The association between energy-adjusted dietary inflammatory index, body composition, and anthropometric indices in COVID-19-infected patients: a casecontrol study in Shiraz, Iran, Int J Clin Pract, doi:10.1155/2022/5452488
Gaillard, Rifas-Shiman, Perng, Oken, Gillman, Maternal inflammation during pregnancy and childhood adiposity, Obesity, doi:10.1002/oby.21484
Garcia, Fumeaux, Guerci, Heuberger, Montomoli et al., Prognostic factors associated with mortality risk and disease progression in 639 critically ill patients with COVID-19 in Europe: initial report of the international RISC-19-ICU prospective observational cohort, eClinicalMedicine, doi:10.1016/j.eclinm.2020.100449
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients, doi:10.3390/nu12040988
Górnicka, Drywień, Zielinska, Hamułka, Dietary and lifestyle changes during COVID-19 and the subsequent lockdowns among Polish adults: a cross-sectional online survey PLifeCOVID-19 study, Nutrients, doi:10.3390/nu12082324
Haddad, Malhab, Sacre, Salameh, Smoking and COVID-19: a scoping review, Tob Use Insights, doi:10.1177/1179173X21994612
Hajipour, Afsharfar, Jonoush, Ahmadzadeh, Gholamalizadeh et al., The effects of dietary fiber on common complications in critically ill patients; with a special focus on viral infections: a systematic review, Immun Inflamm Dis, doi:10.1002/iid3.613
Hruby, Jacques, Dietary protein and changes in biomarkers of inflammation and oxidative stress in the Framingham heart study offspring cohort, Curr Dev Nutr, doi:10.1093/cdn/nzz019
Hu, Lin, Kaminga, Xu, Impact of the COVID-19 epidemic on lifestyle behaviors and their association with subjective well-being among the general population in mainland China: cross-sectional study, J Med Int Res, doi:10.2196/21176
Kang, Kim, Astaxanthin and β-carotene in Helicobacter pylori-induced gastric inflammation: a mini-review on action mechanisms, J Cancer Prev, doi:10.15430/JCP.2017.22.2.57
Karimi, Yarizadeh, Setayesh, Sajjadi, Ghodoosi et al., High carbohydrate intakes may predict more inflammatory status than high fat intakes in pre-menopause women with overweight or obesity: a cross-sectional study, BMC Res Notes, doi:10.1186/s13104-021-05699-1
Kavyani, Musazadeh, Fathi, Faghfouri, Dehghan et al., Efficacy of the omega-3 fatty acids supplementation on inflammatory biomarkers: an umbrella meta-analysis, Int Immunopharmacol, doi:10.1016/j.intimp.2022.109104
Kim, Park, Association between the dietary inflammatory index and risk of frailty in older individuals with poor nutritional status, Nutrients, doi:10.3390/nu10101363
Klang, Kassim, Soffer, Freeman, Levin et al., Severe obesity as an independent risk factor for COVID-19 mortality in hospitalized patients younger than 50, Silver Spring), doi:10.1002/oby.22913
Koelman, Markova, Seebeck, Hornemann, Rosenthal et al., Effects of high and low protein diets on inflammatory profiles in people with morbid obesity: a 3-week intervention study, Nutrients, doi:10.3390/nu12123636
Krishnan, Hamilton, Alqahtani, Woreta, COVID-19: an overview and a clinical update, World J Clin Cases, doi:10.12998/wjcc.v9.i1.8
Laird, Rhodes, Kenny, Vitamin D and inflammation: potential implications for severity of Covid-19, Ir Med J
Lee, Lee, Shin, Kim, Lee et al., Gender difference and determinants of C-reactive protein level in Korean adults, Clin Chem Lab Med, doi:10.1515/CCLM.2009.196
Liu, Yan, Xiang, Liu, Viral dynamics in mild and severe cases of COVID-19, Lancet Infec, doi:10.1016/S1473-3099(20)30232-2
Lomax, Calder, Probiotics, immune function, infection and inflammation: a review of the evidence from studies conducted in humans, Curr Pharm Des, doi:10.2174/138161209788168155
Louie, Tingling, Dray, Hussain, Mckim et al., Dietary cholesterol causes inflammatory imbalance and exacerbates morbidity in mice infected with influenza A virus, J Immunol, doi:10.4049/jimmunol.2100927
Maiorino, Bellastella, Longo, Caruso, Esposito, Mediterranean diet and COVID-19: hypothesizing potential benefits in people with diabetes, Front Endocrinol, doi:10.3389/fendo.2020.574315
Majidi, Bahadori, Shekari, Gholamalizadeh, Tajadod et al., Effects of supplementation with low-dose group B vitamins on clinical and biochemical parameters in critically ill patients with COVID-19: a randomized clinical trial, Exp Rev Anti-infect Ther, doi:10.3389/fimmu.2021.717816
Malekshah, Kimiagar, Saadatian-Elahi, Pourshams, Nouraie et al., Validity and reliability of a new food frequency questionnaire compared to 24 h recalls and biochemical measurements: pilot phase of Golestan cohort study of esophageal cancer, Eur J Clin Nutr, doi:10.1038/sj.ejcn.1602407
Meneguelli, Hinkelmann, Novaes, Cdob, Filgueiras et al., Dietary inflammatory index is associated with excessive body weight and dietary patterns in subjects with cardiometabolic risk, J Food Nutr Res, doi:10.12691/jfnr-7-7-2
Mishra, Pandey, Singh, Gupta, Sahu et al., Descriptive statistics and normality tests for statistical data, Ann Card Anaesth, doi:10.4103/aca.ACA_157_18
Moludi, Qaisar, Alizadeh, Vayghan, Naemi et al., The relationship between Dietary Inflammatory Index and disease severity and inflammatory status: a case-control study of COVID-19 patients, Brit J Nutr, doi:10.1017/S0007114521003214
Mosca, Crudele, Smeriglio, Braghini, Panera et al., Antioxidant activity of hydroxytyrosol and vitamin E reduces systemic inflammation in children with paediatric NAFLD, Dig Liver Dis, doi:10.1016/j.dld.2020.09.021
Nielsen, Magnesium deficiency and increased inflammation: current perspectives, J Inflamm Res, doi:10.2147/JIR.S136742
Perez-Araluce, Martinez-Gonzalez, Fernández-Lázaro, Bes-Rastrollo, Gea et al., Mediterranean diet and the risk of COVID-19 in the 'Seguimiento Universidad de Navarra'cohort, Clin Nutr, doi:10.1016/j.clnu.2021.04.001
Phillips, Shivappa, Hébert, Perry, Dietary inflammatory index and biomarkers of lipoprotein metabolism, inflammation and glucose homeostasis in adults, Nutrients, doi:10.3390/nu10081033
Ravaut, Légiot, Bergeron, Mounier, Monounsaturated fatty acids in obesity-related inflammation, Int J Mol Sci, doi:10.3390/ijms22010330
Reifen, Vitamin A as an anti-inflammatory agent, Proc Nutr Soc, doi:10.1079/PNS2002172
Ren, Zhao, Wang, Meng, Szeto et al., Association between dietary inflammatory index, C-reactive protein and metabolic syndrome: a crosssectional study, Nutrients, doi:10.3390/nu10070831
Rocha, Bressan, Hermsdorff, The role of dietary fatty acid intake in inflammatory gene expression: a critical review, São Paulo Med J, doi:10.1590/1516-3180.2016.008607072016
Romain, Sviri, Linton, Stav, Van Heerden, The role of Vitamin B12 in the critically ill-a review, Anaesth Intensive Care, doi:10.1177/0310057X1604400410
Sharma, Dixon, Jung, Graff, Forney et al., Dietary methionine restriction reduces inflammation independent of FGF21 action, Silver Spring), doi:10.1002/oby.22534
Shivappa, Hébert, Rietzschel, Buyzere, Langlois et al., Associations between dietary inflammatory index and inflammatory markers in the Asklepios Study, Brit J Nutr, doi:10.1017/S000711451400395X
Shivappa, Hébert, Veronese, Caruso, Notarnicola et al., Dietary inflammatory index as a potential determinant of a length of hospitalization among surgical patients treated for colorectal cancer, J Affect Disord, doi:10.1038/ejcn.2014.120
Shivappa, Schneider, Hebert, Koenig, Peters et al., Association between dietary inflammatory index, and cause-specific mortality in the MONICA/KORA Augsburg Cohort Study, Eur J Public Health, doi:10.1093/eurpub/ckx060
Shivappa, Steck, Hurley, Hussey, Hébert, Designing and developing a literature-derived, population-based dietary inflammatory index, Public Health Nutr, doi:10.1017/S1368980013002115
Shivappa, Steck, Hurley, Hussey, Ma et al., A population-based dietary inflammatory index predicts levels of C-reactive protein in the seasonal variation of blood cholesterol study (SEASONS), Public Health Nutr, doi:10.1017/S1368980013002565
Sidor, Rzymski, Dietary choices and habits during COVID-19 lockdown: experience from Poland, Nutrients, doi:10.3390/nu12061657
Silveira, Oliveira, Andrade, Hermsdorff, Rosa et al., Dietary pattern and macronutrients profile on the variation of inflammatory biomarkers: scientific update, Cardiol Res Pract, doi:10.1155/2018/4762575
Soto, González, Sance, Galmarini, Organosulfur and phenolic content of garlic (Allium sativum L.) and onion (Allium cepa L.) and its relationship with antioxidant activity, Acta Horticult, doi:10.17660/ActaHortic.2016.1143.39
Spinas, Saggini, Kritas, Cerulli, Caraffa et al., Iron homeostasis and the inflammatory response, J Biol Regul Homeost Agents, doi:10.1146/annurev.nutr.012809.104804
Subramanian, Han, Chiba, Mcmillen, Wang et al., Dietary cholesterol worsens adipose tissue macrophage accumulation and atherosclerosis in obese LDL receptor-deficient mice, Arterioscler Thromb Vasc Biol, doi:10.1161/ATVBAHA.107.157685
Swann, Kilpatrick, Breslin, Oddy, Dietary fiber and its associations with depression and inflammation, Nutr Rev, doi:10.1093/nutrit/nuz072
Vahid, Bourbour, Gholamalizadeh, Shivappa, Hébert et al., A pro-inflammatory diet increases the likelihood of obesity and overweight in adolescent boys: a case-control study, Diabetol Metab Syndr, doi:10.1186/s13098-020-00536-0
Visser, Bouter, Mcquillan, Wener, Harris, Elevated Creactive protein levels in overweight and obese adults, JAMA, doi:10.1001/jama.282.22.2131
Wang, Yang, Li, Huang, Jiang et al., Specific cytokines in the inflammatory cytokine storm of patients with COVID-19-associated acute respiratory distress syndrome and extrapulmonary multiple-organ dysfunction, Virol J, doi:10.1186/s12985-021-01588-y
Wiersinga, Rhodes, Cheng, Peacock, Prescott, Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review, JAMA, doi:10.1001/jama.2020.12839
Willett, Nutritional Epidemiology, doi:10.1093/acprof:oso/9780199754038.001.0001
Williamson, Walker, Bhaskaran, Bacon, Bates et al., Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Wirth, Sevoyan, Hofseth, Shivappa, Hurley et al., The Dietary Inflammatory Index is associated with elevated white blood cell counts in the National Health and Nutrition Examination Survey, Brain Behav Immun, doi:10.1016/j.bbi.2017.12.003
Woeste, Müller, Bechstein, Wullstein, Increased serum levels of Creactive protein precede anastomotic leakage in colorectal surgery, World J Surg, doi:10.1007/s00268-009-0304-z
Yd, Ding, Dong, Zhang, Azkur et al., Risk factors for severe and critically ill COVID-19 patients: a review, Allergy, doi:10.1111/all.14657
Zabetakis, Lordan, Norton, Tsoupras, COVID-19: the inflammation link and the role of nutrition in potential mitigation, Nutrients, doi:10.3390/nu12051466
Zarezadeh, Faghfouri, Aghapour, Rostamkhani, Malekahmadi et al., Investigation of the clinical efficacy of Zn supplementation in improvement of oxidative stress parameters: a systematic review and dose-response meta-analysis of controlled clinical trials, Int J Clin Pract, doi:10.1111/ijcp.14777
Zemel, Sun, Sobhani, Wilson, Effects of dairy compared with soy on oxidative and inflammatory stress in overweight and obese subjects, Am J Clin Nutr, doi:10.3945/ajcn.2009.28468
Özbey, Uçar, Shivappa, Hebert, Wood et al., The relationship between dietary inflammatory index, pulmonary functions and asthma control in asthmatics, Iran J Allergy Asthma Immunol, doi:10.1111/cea.12323
DOI record:
{
"DOI": "10.3389/fnut.2023.1075061",
"ISSN": [
"2296-861X"
],
"URL": "http://dx.doi.org/10.3389/fnut.2023.1075061",
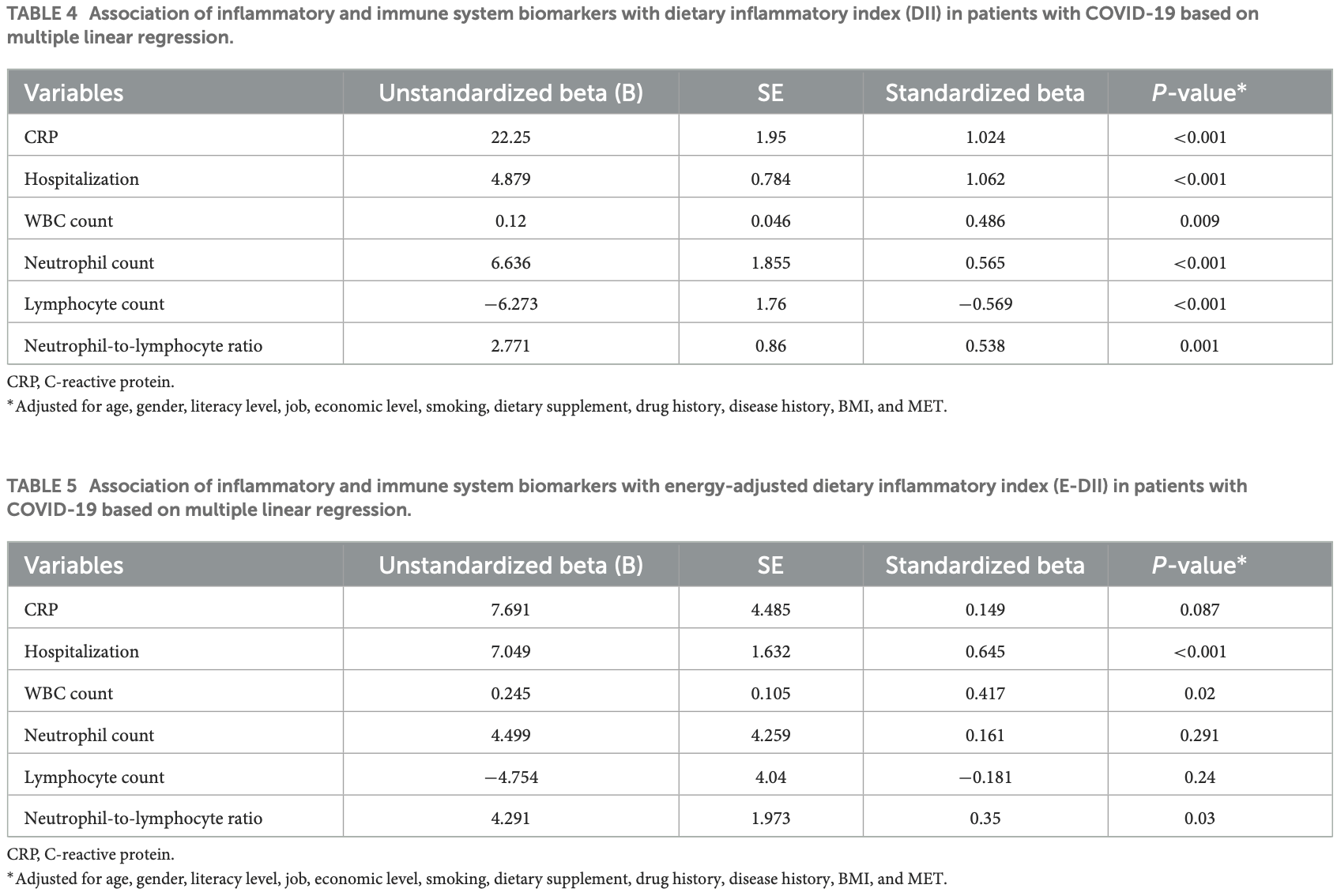
"abstract": "<jats:sec><jats:title>Background</jats:title><jats:p>Inflammation and cytokine storm have been reported to be the main cause of acute symptoms of coronavirus disease (COVID-19). Diet-induced inflammation may affect the condition of patients with COVID-19. Therefore, this study aimed to investigate the relationship between disease severity, inflammatory and immune system biomarkers, and the dietary inflammatory index (DII) in patients with COVID-19.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>This cross-sectional study was conducted on 500 adult patients with COVID-19. Patients were divided into mild, moderate, and severe conditions based on clinical and laboratory evidence. A validated food frequency questionnaire (FFQ) was used to determine DII and energy-adjusted DII (E-DII) scores. The serum C-reactive protein (CRP) level and blood cell count were measured for all patients. Multiple linear regression was used to explore the association between DII and E-DII and CRP, blood cell counts, and hospitalization in patients with COVID-19.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Coronavirus disease (COVID-19) patients with higher DII had higher consumption of fat and carbohydrate and lower intakes of protein, anti-inflammatory nutrients, garlic, caffeine, tea, onion, and fiber (<jats:italic>P</jats:italic> &lt; 0.05). There was a positive association between DII and CRP (β = 1.024, <jats:italic>P</jats:italic> &lt; 0.001), hospitalization (β = 1.062, <jats:italic>P</jats:italic> &lt; 0.001), WBC count (β = 0.486, <jats:italic>P</jats:italic> &lt; 0.009), neutrophil count (β = 0.565, <jats:italic>P</jats:italic> &lt; 0.001), and neutrophil-to-lymphocyte ratio (β = 0.538, <jats:italic>P</jats:italic> &lt; 0.001) and a negative association between DII and the lymphocyte count (β = −0.569, <jats:italic>P</jats:italic> &lt; 0.001). There was a positive association between E-DII and hospitalization (β = 1.645, <jats:italic>P</jats:italic> &lt; 0.001), WBC count (β = 0.417, <jats:italic>P</jats:italic> &lt; 0.02), and neutrophil-to-lymphocyte ratio (β = 0.35, <jats:italic>P</jats:italic> &lt; 0.03).</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>There is a positive correlation between DII and inflammation, immune hyperactivation, and length of hospital stay in patients with COVID-19. Further longitudinal studies are necessary.</jats:p></jats:sec>",
"alternative-id": [
"10.3389/fnut.2023.1075061"
],
"author": [
{
"affiliation": [],
"family": "Barania Adabi",
"given": "Somayyeh",
"sequence": "first"
},
{
"affiliation": [],
"family": "Daneghian",
"given": "Sevana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Khalkhali",
"given": "Hamidreaza",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nejadrahim",
"given": "Rahim",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shivappa",
"given": "Nitin",
"sequence": "additional"
}
],
"container-title": "Frontiers in Nutrition",
"container-title-short": "Front. Nutr.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2023,
3,
31
]
],
"date-time": "2023-03-31T12:49:19Z",
"timestamp": 1680266959000
},
"deposited": {
"date-parts": [
[
2023,
3,
31
]
],
"date-time": "2023-03-31T12:49:54Z",
"timestamp": 1680266994000
},
"indexed": {
"date-parts": [
[
2023,
4,
1
]
],
"date-time": "2023-04-01T04:51:49Z",
"timestamp": 1680324709793
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
3,
31
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
3,
31
]
],
"date-time": "2023-03-31T00:00:00Z",
"timestamp": 1680220800000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fnut.2023.1075061/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2023,
3,
31
]
]
},
"published-online": {
"date-parts": [
[
2023,
3,
31
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1186/s12967-021-02795-5",
"article-title": "The effect of omega-3 fatty acid supplementation on clinical and biochemical parameters of critically ill patients with COVID-19: a randomized clinical trial",
"author": "Doaei",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Transl Med.",
"key": "B1",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.12998/wjcc.v9.i1.8",
"article-title": "COVID-19: an overview and a clinical update",
"author": "Krishnan",
"doi-asserted-by": "publisher",
"first-page": "8",
"journal-title": "World J Clin Cases.",
"key": "B2",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1186/s12985-021-01588-y",
"article-title": "Specific cytokines in the inflammatory cytokine storm of patients with COVID-19-associated acute respiratory distress syndrome and extrapulmonary multiple-organ dysfunction",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Virol J.",
"key": "B3",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1111/all.14657",
"article-title": "Risk factors for severe and critically ill COVID-19 patients: a review",
"author": "Gao",
"doi-asserted-by": "publisher",
"first-page": "428",
"journal-title": "Allergy.",
"key": "B4",
"volume": "76",
"year": "2020"
},
{
"DOI": "10.1016/j.eclinm.2020.100449",
"article-title": "Prognostic factors associated with mortality risk and disease progression in 639 critically ill patients with COVID-19 in Europe: initial report of the international RISC-19-ICU prospective observational cohort",
"author": "Wendel Garcia",
"doi-asserted-by": "publisher",
"first-page": "100449",
"journal-title": "eClinicalMedicine.",
"key": "B5",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"article-title": "Factors associated with COVID-19-related death using OpenSAFELY",
"author": "Williamson",
"doi-asserted-by": "publisher",
"first-page": "430",
"journal-title": "Nature.",
"key": "B6",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.3390/nu12040988",
"article-title": "Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths",
"author": "Grant",
"doi-asserted-by": "publisher",
"first-page": "988",
"journal-title": "Nutrients.",
"key": "B7",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1002/oby.22913",
"article-title": "Severe obesity as an independent risk factor for COVID-19 mortality in hospitalized patients younger than 50",
"author": "Klang",
"doi-asserted-by": "publisher",
"first-page": "1595",
"journal-title": "Obesity (Silver Spring).",
"key": "B8",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1186/s13601-020-00323-0",
"article-title": "Is diet partly responsible for differences in COVID-19 death rates between and within countries?",
"author": "Bousquet",
"doi-asserted-by": "publisher",
"first-page": "16",
"journal-title": "Clin Transl Allergy.",
"key": "B9",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1177/1179173X21994612",
"article-title": "Smoking and COVID-19: a scoping review",
"author": "Haddad",
"doi-asserted-by": "publisher",
"first-page": "1179173x21994612",
"journal-title": "Tob Use Insights.",
"key": "B10",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1016/S1473-3099(20)30232-2",
"article-title": "Viral dynamics in mild and severe cases of COVID-19",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "656",
"journal-title": "Lancet Infec.",
"key": "B11",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1016/j.clnu.2021.04.001",
"article-title": "Mediterranean diet and the risk of COVID-19 in the 'Seguimiento Universidad de Navarra'cohort",
"author": "Perez-Araluce",
"doi-asserted-by": "publisher",
"first-page": "3061",
"journal-title": "Clin Nutr.",
"key": "B12",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.1017/S0007114521003214",
"article-title": "The relationship between Dietary Inflammatory Index and disease severity and inflammatory status: a case-control study of COVID-19 patients",
"author": "Moludi",
"doi-asserted-by": "publisher",
"first-page": "773",
"journal-title": "Brit J Nutr.",
"key": "B13",
"volume": "127",
"year": "2022"
},
{
"DOI": "10.3389/fnut.2022.929384",
"article-title": "Major dietary patterns in relation to disease severity, symptoms, and inflammatory markers in patients recovered from COVID-19",
"author": "Ebrahimzadeh",
"doi-asserted-by": "publisher",
"first-page": "929384",
"journal-title": "Front Nutr.",
"key": "B14",
"volume": "9",
"year": "2022"
},
{
"article-title": "Role of dietary habit and nutritional status on the severity of COVID-19 treatment: a hospital based cross-sectional study",
"author": "Eva",
"journal-title": "J Curr Med Pract.",
"key": "B15",
"year": ""
},
{
"DOI": "10.1080/14787210.2022.2125867",
"article-title": "Effects of supplementation with low-dose group B vitamins on clinical and biochemical parameters in critically ill patients with COVID-19: a randomized clinical trial",
"author": "Majidi",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Exp Rev Anti-infect Ther.",
"key": "B16",
"volume": "30",
"year": "2022"
},
{
"DOI": "10.3389/fimmu.2021.717816",
"article-title": "The effect of Vitamin C on pathological parameters and survival duration of critically ill coronavirus disease 2019 patients: a randomized clinical trial",
"author": "Majidi",
"doi-asserted-by": "publisher",
"first-page": "717",
"journal-title": "Front Immun.",
"key": "B17",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1002/iid3.613",
"article-title": "The effects of dietary fiber on common complications in critically ill patients; with a special focus on viral infections: a systematic review",
"author": "Hajipour",
"doi-asserted-by": "publisher",
"first-page": "e613",
"journal-title": "Immun Inflamm Dis.",
"key": "B18",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1017/S0007114521000192",
"article-title": "Profiling inflammatory cytokines following zinc supplementation: a systematic review and meta-analysis of controlled trials",
"author": "Faghfouri",
"doi-asserted-by": "publisher",
"first-page": "1441",
"journal-title": "Br J Nutr.",
"key": "B19",
"volume": "126",
"year": "2021"
},
{
"DOI": "10.1016/j.phrs.2019.104619",
"article-title": "A comprehensive mechanistic review insight into the effects of micronutrients on toll-like receptors functions",
"author": "Faghfouri",
"doi-asserted-by": "publisher",
"first-page": "104619",
"journal-title": "Pharmacol Res.",
"key": "B20",
"volume": "152",
"year": "2020"
},
{
"DOI": "10.1017/S0007114511005460",
"article-title": "Dietary factors and low-grade inflammation in relation to overweight and obesity",
"author": "Calder",
"doi-asserted-by": "publisher",
"first-page": "S5",
"journal-title": "Br J Nutr.",
"key": "B21",
"volume": "3",
"year": "2011"
},
{
"DOI": "10.3390/nu12051466",
"article-title": "COVID-19: the inflammation link and the role of nutrition in potential mitigation",
"author": "Zabetakis",
"doi-asserted-by": "publisher",
"first-page": "1466",
"journal-title": "Nutrients.",
"key": "B22",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1017/S1368980013002565",
"article-title": "A population-based dietary inflammatory index predicts levels of C-reactive protein in the seasonal variation of blood cholesterol study (SEASONS)",
"author": "Shivappa",
"doi-asserted-by": "publisher",
"first-page": "1825",
"journal-title": "Public Health Nutr.",
"key": "B23",
"volume": "17",
"year": "2014"
},
{
"DOI": "10.1017/S000711451400395X",
"article-title": "Associations between dietary inflammatory index and inflammatory markers in the Asklepios Study",
"author": "Shivappa",
"doi-asserted-by": "publisher",
"first-page": "665",
"journal-title": "Brit J Nutr.",
"key": "B24",
"volume": "113",
"year": "2015"
},
{
"DOI": "10.1186/s13098-020-00536-0",
"article-title": "A pro-inflammatory diet increases the likelihood of obesity and overweight in adolescent boys: a case-control study",
"author": "Vahid",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Diabetol Metab Syndr.",
"key": "B25",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1002/osp4.639",
"article-title": "Association of dietary antioxidant index with body mass index in adolescents",
"author": "Aminnejad",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Obes Sci Pract.",
"key": "B26",
"volume": "2022",
"year": "2022"
},
{
"DOI": "10.1016/j.bbi.2017.12.003",
"article-title": "The Dietary Inflammatory Index is associated with elevated white blood cell counts in the National Health and Nutrition Examination Survey",
"author": "Wirth",
"doi-asserted-by": "publisher",
"first-page": "296",
"journal-title": "Brain Behav Immun.",
"key": "B27",
"volume": "69",
"year": "2018"
},
{
"DOI": "10.1001/jama.2020.12839",
"article-title": "Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review",
"author": "Wiersinga",
"doi-asserted-by": "publisher",
"first-page": "782",
"journal-title": "JAMA.",
"key": "B28",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1001/jama.282.22.2131",
"article-title": "Elevated C-reactive protein levels in overweight and obese adults",
"author": "Visser",
"doi-asserted-by": "publisher",
"first-page": "2131",
"journal-title": "JAMA.",
"key": "B29",
"volume": "282",
"year": "1999"
},
{
"DOI": "10.1002/oby.21484",
"article-title": "Maternal inflammation during pregnancy and childhood adiposity",
"author": "Gaillard",
"doi-asserted-by": "publisher",
"first-page": "1320",
"journal-title": "Obesity.",
"key": "B30",
"volume": "24",
"year": "2016"
},
{
"DOI": "10.1007/s00268-009-0304-z",
"article-title": "Increased serum levels of C-reactive protein precede anastomotic leakage in colorectal surgery",
"author": "Woeste",
"doi-asserted-by": "publisher",
"first-page": "140",
"journal-title": "World J Surg.",
"key": "B31",
"volume": "34",
"year": "2010"
},
{
"DOI": "10.1093/eurpub/ckx060",
"article-title": "Association between dietary inflammatory index, and cause-specific mortality in the MONICA/KORA Augsburg Cohort Study",
"author": "Shivappa",
"doi-asserted-by": "publisher",
"first-page": "167",
"journal-title": "Eur J Public Health.",
"key": "B32",
"volume": "28",
"year": "2018"
},
{
"DOI": "10.1038/sj.ejcn.1602407",
"article-title": "Validity and reliability of a new food frequency questionnaire compared to 24 h recalls and biochemical measurements: pilot phase of Golestan cohort study of esophageal cancer",
"author": "Malekshah",
"doi-asserted-by": "publisher",
"first-page": "971",
"journal-title": "Eur J Clin Nutr.",
"key": "B33",
"volume": "60",
"year": "2006"
},
{
"DOI": "10.1017/S1368980013002115",
"article-title": "Designing and developing a literature-derived, population-based dietary inflammatory index",
"author": "Shivappa",
"doi-asserted-by": "publisher",
"first-page": "1689",
"journal-title": "Public Health Nutr.",
"key": "B34",
"volume": "17",
"year": "2014"
},
{
"DOI": "10.4103/aca.ACA_157_18",
"article-title": "Descriptive statistics and normality tests for statistical data",
"author": "Mishra",
"doi-asserted-by": "publisher",
"first-page": "67",
"journal-title": "Ann Card Anaesth.",
"key": "B35",
"volume": "22",
"year": "2019"
},
{
"DOI": "10.18502/ijaai.v18i6.2173",
"article-title": "The relationship between dietary inflammatory index, pulmonary functions and asthma control in asthmatics",
"author": "Özbey",
"doi-asserted-by": "publisher",
"first-page": "605",
"journal-title": "Iran J Allergy Asthma Immunol.",
"key": "B36",
"volume": "18",
"year": "2019"
},
{
"DOI": "10.1111/cea.12323",
"article-title": "Dietary inflammatory index is related to asthma risk, lung function and systemic inflammation in asthma",
"author": "Wood",
"doi-asserted-by": "publisher",
"first-page": "177",
"journal-title": "Clin Exp Allergy.",
"key": "B37",
"volume": "45",
"year": "2015"
},
{
"DOI": "10.1155/2022/5452488",
"article-title": "The association between energy-adjusted dietary inflammatory index, body composition, and anthropometric indices in COVID-19-infected patients: a case-control study in Shiraz, Iran",
"author": "Firoozi",
"doi-asserted-by": "publisher",
"first-page": "5452488",
"journal-title": "Int J Clin Pract.",
"key": "B38",
"volume": "2022",
"year": "2022"
},
{
"DOI": "10.3390/nu10081033",
"article-title": "Dietary inflammatory index and biomarkers of lipoprotein metabolism, inflammation and glucose homeostasis in adults",
"author": "Phillips",
"doi-asserted-by": "publisher",
"first-page": "1033",
"journal-title": "Nutrients.",
"key": "B39",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.3390/nu10070831",
"article-title": "Association between dietary inflammatory index, C-reactive protein and metabolic syndrome: a cross-sectional study",
"author": "Ren",
"doi-asserted-by": "publisher",
"first-page": "831",
"journal-title": "Nutrients.",
"key": "B40",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.1016/j.jad.2018.04.014",
"article-title": "The relationship between the dietary inflammatory index (DII(®)) and incident depressive symptoms: a longitudinal cohort study",
"author": "Shivappa",
"doi-asserted-by": "publisher",
"first-page": "39",
"journal-title": "J Affect Disord.",
"key": "B41",
"volume": "235",
"year": "2018"
},
{
"DOI": "10.1038/ejcn.2014.120",
"article-title": "Dietary inflammatory index as a potential determinant of a length of hospitalization among surgical patients treated for colorectal cancer",
"author": "Galas",
"doi-asserted-by": "publisher",
"first-page": "1168",
"journal-title": "Eur J Clin Nutr.",
"key": "B42",
"volume": "68",
"year": "2014"
},
{
"DOI": "10.3389/fendo.2020.574315",
"article-title": "Mediterranean diet and COVID-19: hypothesizing potential benefits in people with diabetes",
"author": "Maiorino",
"doi-asserted-by": "publisher",
"first-page": "574315",
"journal-title": "Front Endocrinol.",
"key": "B43",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.bbi.2020.04.040",
"article-title": "The impact of nutrition on COVID-19 susceptibility and long-term consequences",
"author": "Butler",
"doi-asserted-by": "publisher",
"first-page": "53",
"journal-title": "Brain Behav Immun.",
"key": "B44",
"volume": "87",
"year": "2020"
},
{
"DOI": "10.3390/nu10101363",
"article-title": "Association between the dietary inflammatory index and risk of frailty in older individuals with poor nutritional status",
"author": "Kim",
"doi-asserted-by": "publisher",
"first-page": "1363",
"journal-title": "Nutrients.",
"key": "B45",
"volume": "10",
"year": "2018"
},
{
"article-title": "Vitamin D and inflammation: potential implications for severity of Covid-19",
"author": "Laird",
"first-page": "81",
"journal-title": "Ir Med J.",
"key": "B46",
"volume": "113",
"year": "2020"
},
{
"DOI": "10.1016/j.dld.2020.09.021",
"article-title": "Antioxidant activity of hydroxytyrosol and vitamin E reduces systemic inflammation in children with paediatric NAFLD",
"author": "Mosca",
"doi-asserted-by": "publisher",
"first-page": "1154",
"journal-title": "Dig Liver Dis.",
"key": "B47",
"volume": "53",
"year": "2021"
},
{
"DOI": "10.1079/PNS2002172",
"article-title": "Vitamin A as an anti-inflammatory agent",
"author": "Reifen",
"doi-asserted-by": "publisher",
"first-page": "397",
"journal-title": "Proc Nutr Soc.",
"key": "B48",
"volume": "61",
"year": "2002"
},
{
"DOI": "10.2147/DDDT.S83144",
"article-title": "Effect of vitamin C on inflammation and metabolic markers in hypertensive and/or diabetic obese adults: a randomized controlled trial",
"author": "Ellulu",
"doi-asserted-by": "publisher",
"first-page": "3405",
"journal-title": "Drug Des Devel Ther.",
"key": "B49",
"volume": "9",
"year": "2015"
},
{
"DOI": "10.15430/JCP.2017.22.2.57",
"article-title": "Astaxanthin and β-carotene in Helicobacter pylori-induced gastric inflammation: a mini-review on action mechanisms",
"author": "Kang",
"doi-asserted-by": "publisher",
"first-page": "57",
"journal-title": "J Cancer Prev.",
"key": "B50",
"volume": "22",
"year": "2017"
},
{
"DOI": "10.2147/JIR.S136742",
"article-title": "Magnesium deficiency and increased inflammation: current perspectives",
"author": "Nielsen",
"doi-asserted-by": "publisher",
"first-page": "25",
"journal-title": "J Inflamm Res.",
"key": "B51",
"volume": "11",
"year": "2018"
},
{
"DOI": "10.1111/ijcp.14777",
"article-title": "Investigation of the clinical efficacy of Zn supplementation in improvement of oxidative stress parameters: a systematic review and dose-response meta-analysis of controlled clinical trials",
"author": "Zarezadeh",
"doi-asserted-by": "publisher",
"first-page": "e14777",
"journal-title": "Int J Clin Pract.",
"key": "B52",
"volume": "75",
"year": "2021"
},
{
"DOI": "10.1055/s-0029-1220724",
"article-title": "Selenium and inflammation: underlying anti-inflammatory mechanisms",
"author": "Duntas",
"doi-asserted-by": "publisher",
"first-page": "443",
"journal-title": "Horm Metab Res.",
"key": "B53",
"volume": "41",
"year": "2009"
},
{
"DOI": "10.6084/M9.FIGSHARE.3860199.V1",
"article-title": "Crosstalk between vitamin B and immunity",
"author": "Spinas",
"doi-asserted-by": "publisher",
"first-page": "283",
"journal-title": "J Biol Regul Homeost Agents.",
"key": "B54",
"volume": "29",
"year": "2015"
},
{
"DOI": "10.1146/annurev.nutr.012809.104804",
"article-title": "Iron homeostasis and the inflammatory response",
"author": "Wessling-Resnick",
"doi-asserted-by": "publisher",
"first-page": "105",
"journal-title": "Annu Rev Nutr.",
"key": "B55",
"volume": "30",
"year": "2010"
},
{
"DOI": "10.30574/gscbps.2020.11.3.0155",
"article-title": "Can vitamin B12 be an adjuvant to COVID-19 treatment?",
"author": "dos Santos",
"doi-asserted-by": "publisher",
"first-page": "001",
"journal-title": "GSC Biol Pharmaceut Sci.",
"key": "B56",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1177/0310057X1604400410",
"article-title": "The role of Vitamin B12 in the critically ill—a review",
"author": "Romain",
"doi-asserted-by": "publisher",
"first-page": "447",
"journal-title": "Anaesth Intensive Care.",
"key": "B57",
"volume": "44",
"year": "2016"
},
{
"DOI": "10.2147/JIR.S232157",
"article-title": "Higher dietary inflammatory index scores are associated with increased odds of benign breast diseases in a case-control study",
"author": "Aghababayan",
"doi-asserted-by": "publisher",
"first-page": "61",
"journal-title": "J Inflamm Res.",
"key": "B58",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.12691/jfnr-7-7-2",
"article-title": "Dietary inflammatory index is associated with excessive body weight and dietary patterns in subjects with cardiometabolic risk",
"author": "Meneguelli",
"doi-asserted-by": "publisher",
"first-page": "491",
"journal-title": "J Food Nutr Res.",
"key": "B59",
"volume": "7",
"year": "2019"
},
{
"DOI": "10.1016/j.intimp.2022.109104",
"article-title": "Efficacy of the omega-3 fatty acids supplementation on inflammatory biomarkers: an umbrella meta-analysis",
"author": "Kavyani",
"doi-asserted-by": "publisher",
"first-page": "109104",
"journal-title": "Int Immunopharmacol.",
"key": "B60",
"volume": "111",
"year": "2022"
},
{
"DOI": "10.1093/nutrit/nuz072",
"article-title": "Dietary fiber and its associations with depression and inflammation",
"author": "Swann",
"doi-asserted-by": "publisher",
"first-page": "394",
"journal-title": "Nutr Rev.",
"key": "B61",
"volume": "78",
"year": "2019"
},
{
"DOI": "10.1093/cdn/nzz019",
"article-title": "Dietary protein and changes in biomarkers of inflammation and oxidative stress in the Framingham heart study offspring cohort",
"author": "Hruby",
"doi-asserted-by": "publisher",
"first-page": "nzz019",
"journal-title": "Curr Dev Nutr.",
"key": "B62",
"volume": "3",
"year": "2019"
},
{
"DOI": "10.3390/nu12123636",
"article-title": "Effects of high and low protein diets on inflammatory profiles in people with morbid obesity: a 3-week intervention study",
"author": "Koelman",
"doi-asserted-by": "publisher",
"first-page": "3636",
"journal-title": "Nutrients.",
"key": "B63",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.celrep.2018.07.089",
"article-title": "Methionine restriction extends lifespan in progeroid mice and alters lipid and bile acid metabolism",
"author": "Bárcena",
"doi-asserted-by": "publisher",
"first-page": "2392",
"journal-title": "Cell Rep.",
"key": "B64",
"volume": "24",
"year": "2018"
},
{
"DOI": "10.1002/oby.22534",
"article-title": "Dietary methionine restriction reduces inflammation independent of FGF21 action",
"author": "Sharma",
"doi-asserted-by": "publisher",
"first-page": "1305",
"journal-title": "Obesity (Silver Spring).",
"key": "B65",
"volume": "27",
"year": "2019"
},
{
"DOI": "10.3945/ajcn.2009.28468",
"article-title": "Effects of dairy compared with soy on oxidative and inflammatory stress in overweight and obese subjects",
"author": "Zemel",
"doi-asserted-by": "publisher",
"first-page": "16",
"journal-title": "Am J Clin Nutr.",
"key": "B66",
"volume": "91",
"year": "2010"
},
{
"DOI": "10.1155/2018/4762575",
"article-title": "Dietary pattern and macronutrients profile on the variation of inflammatory biomarkers: scientific update",
"author": "Silveira",
"doi-asserted-by": "publisher",
"first-page": "4762575",
"journal-title": "Cardiol Res Pract.",
"key": "B67",
"volume": "2018",
"year": "2018"
},
{
"DOI": "10.2174/138161209788168155",
"article-title": "Probiotics, immune function, infection and inflammation: a review of the evidence from studies conducted in humans",
"author": "Lomax",
"doi-asserted-by": "publisher",
"first-page": "1428",
"journal-title": "Curr Pharm Des.",
"key": "B68",
"volume": "15",
"year": "2009"
},
{
"DOI": "10.3390/ijms22010330",
"article-title": "Monounsaturated fatty acids in obesity-related inflammation",
"author": "Ravaut",
"doi-asserted-by": "publisher",
"first-page": "330",
"journal-title": "Int J Mol Sci.",
"key": "B69",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1590/1516-3180.2016.008607072016",
"article-title": "The role of dietary fatty acid intake in inflammatory gene expression: a critical review",
"author": "Rocha",
"doi-asserted-by": "publisher",
"first-page": "157",
"journal-title": "São Paulo Med J.",
"key": "B70",
"volume": "135",
"year": "2017"
},
{
"DOI": "10.1161/ATVBAHA.110.203984",
"article-title": "Saturated fatty acids and inflammation: who pays the toll?",
"author": "Chait",
"doi-asserted-by": "publisher",
"first-page": "692",
"journal-title": "Arterioscler Thromb Vasc Biol.",
"key": "B71",
"volume": "30",
"year": "2010"
},
{
"DOI": "10.1161/ATVBAHA.107.157685",
"article-title": "Dietary cholesterol worsens adipose tissue macrophage accumulation and atherosclerosis in obese LDL receptor-deficient mice",
"author": "Subramanian",
"doi-asserted-by": "publisher",
"first-page": "685",
"journal-title": "Arterioscler Thromb Vasc Biol.",
"key": "B72",
"volume": "28",
"year": "2008"
},
{
"DOI": "10.4049/jimmunol.2100927",
"article-title": "Dietary cholesterol causes inflammatory imbalance and exacerbates morbidity in mice infected with influenza A virus",
"author": "Louie",
"doi-asserted-by": "publisher",
"first-page": "2523",
"journal-title": "J Immunol.",
"key": "B73",
"volume": "208",
"year": "2022"
},
{
"DOI": "10.1186/s13104-021-05699-1",
"article-title": "High carbohydrate intakes may predict more inflammatory status than high fat intakes in pre-menopause women with overweight or obesity: a cross-sectional study",
"author": "Karimi",
"doi-asserted-by": "publisher",
"first-page": "279",
"journal-title": "BMC Res Notes.",
"key": "B74",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.3945/ajcn.113.059584",
"article-title": "Tea and flavonoids: where we are, where to go next",
"author": "Dwyer",
"doi-asserted-by": "publisher",
"journal-title": "Am J Clin Nutr.",
"key": "B75",
"year": "2013"
},
{
"DOI": "10.17660/ActaHortic.2016.1143.39",
"article-title": "Organosulfur and phenolic content of garlic (Allium sativum L",
"author": "Soto",
"doi-asserted-by": "publisher",
"first-page": "277",
"journal-title": "Acta Horticult.",
"key": "B76",
"volume": "2016",
"year": "2016"
},
{
"DOI": "10.3390/nu12082324",
"article-title": "Dietary and lifestyle changes during COVID-19 and the subsequent lockdowns among Polish adults: a cross-sectional online survey PLifeCOVID-19 study",
"author": "Górnicka",
"doi-asserted-by": "publisher",
"first-page": "2324",
"journal-title": "Nutrients.",
"key": "B77",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.3390/nu12061657",
"article-title": "Dietary choices and habits during COVID-19 lockdown: experience from Poland",
"author": "Sidor",
"doi-asserted-by": "publisher",
"first-page": "1657",
"journal-title": "Nutrients.",
"key": "B78",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.2196/21176",
"article-title": "Impact of the COVID-19 epidemic on lifestyle behaviors and their association with subjective well-being among the general population in mainland China: cross-sectional study",
"author": "Hu",
"doi-asserted-by": "publisher",
"first-page": "e21176",
"journal-title": "J Med Int Res.",
"key": "B79",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1515/CCLM.2009.196",
"article-title": "Gender difference and determinants of C-reactive protein level in Korean adults",
"author": "Lee",
"doi-asserted-by": "publisher",
"first-page": "863",
"journal-title": "Clin Chem Lab Med.",
"key": "B80",
"volume": "47",
"year": "2009"
},
{
"DOI": "10.3945/ajcn.2008.27030",
"article-title": "Sex differences in inflammatory markers: what is the contribution of visceral adiposity?",
"author": "Cartier",
"doi-asserted-by": "publisher",
"first-page": "1307",
"journal-title": "Am J Clin Nutr.",
"key": "B81",
"volume": "89",
"year": "2009"
},
{
"DOI": "10.1016/j.socscimed.2009.12.014",
"article-title": "Lifecourse socioeconomic trajectories and C-reactive protein levels in young adults: findings from a Brazilian birth cohort",
"author": "Nazmi",
"doi-asserted-by": "publisher",
"first-page": "1229",
"journal-title": "Soc Sci Med.",
"key": "B82",
"volume": "70",
"year": "2010"
},
{
"DOI": "10.1038/s41598-017-02888-6",
"article-title": "Socio-economic inequalities in C-reactive protein and fibrinogen across the adult age span: findings from Understanding Society",
"author": "Davillas",
"doi-asserted-by": "publisher",
"first-page": "2641",
"journal-title": "Sci Rep.",
"key": "B83",
"volume": "7",
"year": "2017"
},
{
"DOI": "10.1016/j.bbi.2005.10.003",
"article-title": "Socioeconomic status and C-reactive protein levels in the US population: NHANES IV",
"author": "Alley",
"doi-asserted-by": "publisher",
"first-page": "498",
"journal-title": "Brain Behav Immun.",
"key": "B84",
"volume": "20",
"year": "2006"
},
{
"DOI": "10.1093/acprof:oso/9780199754038.001.0001",
"author": "Willett",
"doi-asserted-by": "crossref",
"key": "B85",
"volume-title": "Nutritional Epidemiology",
"year": "2012"
}
],
"reference-count": 85,
"references-count": 85,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fnut.2023.1075061/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Nutrition and Dietetics",
"Endocrinology, Diabetes and Metabolism",
"Food Science"
],
"subtitle": [],
"title": "The association between inflammatory and immune system biomarkers and the dietary inflammatory index in patients with COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "10"
}