Acetylsalicylic Acid Compared with Enoxaparin for the Prevention of Thrombosis and Mechanical Ventilation in COVID-19 Patients: A Retrospective Cohort Study
et al., Clinical Drug Investigation, doi:10.1007/s40261-021-01061-2, Jul 2021
Retrospective 225 hospitalized patients in Egypt, showing significantly lower thromboembolic events with aspirin treatment, but no significant difference in the need for mechanical ventilation.
|
risk of mechanical ventilation, 7.8% higher, RR 1.08, p = 0.93, treatment 11 of 31 (35.5%), control 6 of 36 (16.7%), adjusted per study, odds ratio converted to relative risk.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Abdelwahab et al., 30 Jul 2021, retrospective, Egypt, peer-reviewed, 17 authors.
Acetylsalicylic Acid Compared with Enoxaparin for the Prevention of Thrombosis and Mechanical Ventilation in COVID-19 Patients: A Retrospective Cohort Study
Clinical Drug Investigation, doi:10.1007/s40261-021-01061-2
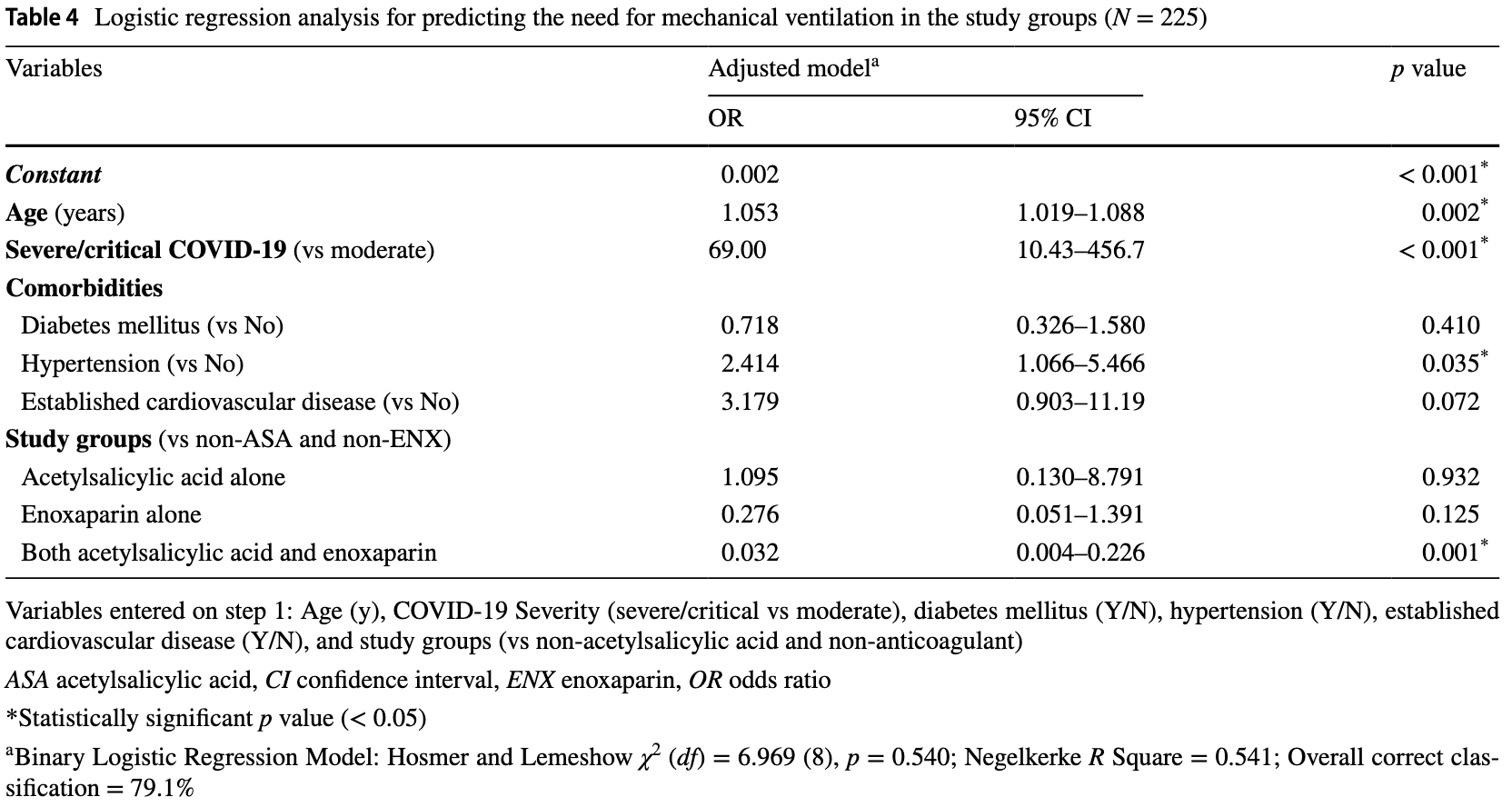
Background and Objective Low-dose acetylsalicylic acid (ASA, aspirin) is a well-known and frequently studied drug for primary and secondary prevention of disease due to its anti-inflammatory and coagulopathic effects. COVID-19 complications are attributed to the role of thrombo-inflammation. Studies regarding the use of low-dose ASA in COVID-19 are limited. For this reason, we propose that the use of low-dose ASA may have protective effects in COVID-19-related thromboembolism and lung injury. This study was conducted to assess the efficacy of low-dose ASA compared with enoxaparin, an anticoagulant, for the prevention of thrombosis and mechanical ventilation. Methods We conducted a retrospective cohort study on COVID-19-confirmed hospitalized patients at the Mansoura University Quarantine Hospital, outpatients, and home-isolated patients from September to December 2020 in Mansoura governorate, Egypt. Binary logistic regression analysis was used to assess the effect of ASA compared with enoxaparin on thromboembolism, and mechanical ventilation needs. Results This study included 225 COVID-19 patients. Use of ASA-only (81-162 mg orally daily) was significantly associated with reduced thromboembolism (OR 0.163, p = 0.020), but both low-dose ASA and enoxaparin, and enoxaparin-only (0.5 mg/kg subcutaneously (SC) daily as prophylactic dose or 1 mg/kg SC every 12 hours as therapeutic dose) were more protective (odds ratio [OR] 0.010, OR 0.071, respectively, p < 0.001). Neither ASA-only nor enoxaparin-only were associated with a reduction in mechanical ventilation needs. Concomitant use of low-dose ASA and enoxaparin was associated with reduced mechanical ventilation (OR 0.032, 95% CI 0.004-0.226, p = 0.001). Conclusions Low-dose ASA-only use may reduce the incidence of COVID-19-associated thromboembolism, but the reduction may be less than that of enoxaparin-only, and both ASA and enoxaparin. Concomitant use of ASA and enoxaparin demonstrates promising results with regard to the reduction of thrombotic events, and mechanical ventilation needs.
Declarations Funding No financial support was obtained from any individual, institutions, agencies, drug industries or organizations.
Competing interests The authors declare that they have no competing interests.
Ethics approval This study was approved by the Mansoura Institutional Research Board Ethics (code number: R.20.08.971), which waived the need for informed consent.
Consent to participate The Ethics Committee of Mansoura University waived the need for informed consent from the study population for the collection, analysis, and publication of the retrospectively obtained and anonymized data for this non-interventional study.
Consent to publish Not applicable. Author contributions HWA, SWS, and HASA contributed equally to this work and share first authorship. HA put the idea of the research, built the research team, designed the study, revised the manuscript, and approved the final version of manuscript. HWA and SWS participated in designing the study, collected the data, revised the manuscript, and approved the final version of manuscript. HASA participated in designing the study, wrote the manuscript draft, and approved the final version of manuscript. AMF participated in designing the study, analyzed the data, revised the manuscript, and approved the final version of manuscript. AM and AGA participated in designing the study and in statistical analysis, revised the manuscript, and approved the final version. EM, ED, JBR, GF, and GFN participated in designing..
References
Ackermann, Verleden, Kuehnel, Haverich, Welte et al., Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19, N Engl J Med, doi:10.1056/NEJMoa2015432
Ahmed, Merrell, Ismail, Joudeh, Riley et al., Rationales and uncertainties for aspirin use in COVID-19: a narrative review, Fam Med Com Health, doi:10.1136/fmch-2020-000741
Bikdeli, Madhavan, Jimenez, Chuich, Dreyfus et al., COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review, J Am Coll Cardiol, doi:10.1016/j.jacc.2020.04.031
Bilaloglu, Aphinyanaphongs, Jones, Iturrate, Hochman et al., Thrombosis in hospitalized patients with COVID-19 in a New York City health system, JAMA, doi:10.1001/jama.2020.13372
Cheruiyot, Kipkorir, Ngure, Misiani, Munguti et al., Arterial thrombosis in coronavirus disease 2019 patients: a rapid systematic review, Ann Vasc Surg, doi:10.1016/j.avsg.2020.08.087
Cho, A paradigm shift in platelet transfusion therapy, Blood, doi:10.1182/blood-2015-04-640649
Chow, Khanna, Kethireddy, Yamane, Levine et al., Aspirin use is associated with decreased mechanical ventilation, ICU admission, and in-hospital mortality in hospitalized patients with COVID-19, Anesth Analg, doi:10.1213/ANE.0000000000005292
Cohen, Harrington, Goldhaber, Hull, Wiens et al., Extended thromboprophylaxis with betrixaban in acutely ill medical patients, N Engl J Med, doi:10.1056/NEJMoa1601747
Cohen, Spiro, Büller, Haskell, Hu et al., Rivaroxaban for thromboprophylaxis in acutely ill medical patients, N Engl J Med, doi:10.1056/NEJMoa1111096
Cook, Meade, Guyatt, Walter, Heels-Ansdell, PROTECT Investigators for the Canadian Critical Care Trials Group and the Australian and New Zealand Intensive Care Society Clinical Trials Group, N Engl J Med, doi:10.1056/NEJMoa1014475
Diaz, Trachtenberg, Abraham, Kosagisharaf, Aa, Aspirin bioactivity for prevention of cardiovascular injury in COVID-19, Front Cardiovasc Med, doi:10.3389/fcvm.2020.562708
Dzeshka, Shantsila, Lip, Effects of aspirin on endothelial function and hypertension, Curr Hypertens Rep, doi:10.1007/s11906-016-0688-8
Eikelboom, Hirsh, Spencer, Baglin, Weitz, Antiplatelet drugs: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines, Chest, doi:10.1378/chest.11-2293
Glatthaar-Saalmüller, Mair, Saalmüller, Antiviral activity of aspirin against RNA viruses of the respiratory tract-an in vitro study, Influenza Other Respir Viruses, doi:10.1111/irv.12421
Godino, Scotti, Maugeri, Mancini, Fominskiy et al., Antithrombotic therapy in patients with COVID-19?-rationale and evidence, Int J Cardiol, doi:10.1016/j.ijcard.2020.09.064
Goldhaber, Leizorovicz, Kakkar, Haas, Merli et al., Apixaban versus enoxaparin for thromboprophylaxis in medically ill patients, N Engl J Med, doi:10.1056/NEJMoa1110899
Goshua, Pine, Meizlish, Chang, Zhang et al., Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study, Lancet Haematol, doi:10.1016/S2352-3026(20)30216-7
Griffin, Jensen, Khan, Chin, Chin et al., Arterial thromboembolic complications in COVID-19 in low-risk patients despite prophylaxis, Br J Haematol, doi:10.1111/bjh.16792
Hansell, Bankier, Macmahon, Mcloud, Müller, Fleischner Society: glossary of terms for thoracic imaging, Radiology, doi:10.1148/radiol.2462070712
Klok, Kruip, Van Der Meer, Arbous, Gommers et al., Incidence of thrombotic complications in critically ill ICU patients with COVID-19, Thromb Res, doi:10.1016/j.thromres.2020.04.013
Kunutsor, Laukkanen, Incidence of venous and arterial thromboembolic complications in COVID-19: a systematic review and meta-analysis, Thromb Res, doi:10.1016/j.thromres.2020.08.022
Liu, Li, Arnold, Pawlinski, Key, Using heparin molecules to manage COVID-2019, Res Pract Thromb Haemost, doi:10.1002/rth2.12353
Lodigiani, Iapichino, Carenzo, Cecconi, Ferrazzi et al., Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy, Thromb Res, doi:10.1016/j.thromres.2020.04.024
Martha, Pranata, Lim, Wibowo, Akbar, Active prescription of low-dose aspirin during or prior to hospitalization and mortality in COVID-19: a systematic review and meta-analysis of adjusted effect estimates, Int J Infect Dis, doi:10.1016/j.ijid.2021.05.016
Masoud, Elassal, Hassany, Shawky, Hakim et al., Management Protocol for COVID-19 Patients MoHP Protocol for COVID19 November
Meizlish, Goshua, Liu, Fine, Amin et al., Intermediate-dose anticoagulation, aspirin, and in-hospital mortality in COVID-19: a propensity score-matched analysis, Am J Hematol, doi:10.1002/ajh.26102
Miano, Cuker, Christie, Martin, Smith et al., Comparative effectiveness of enoxaparin vs dalteparin for thromboprophylaxis after traumatic injury, Chest, doi:10.1016/j.chest.2017.08.008
Okoye, Gelbard, Inaba, Esparza, Belzberg et al., Dalteparin versus enoxaparin for the prevention of venous thromboembolic events in trauma patients, Eur J Trauma Emerg Surg, doi:10.1007/s00068-013-0333-z
Oran, Topol, Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review, Ann Intern Med, doi:10.7326/M20-3012
Pan, Ye, Sun, Gui, Liang et al., Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19), Radiology, doi:10.1148/radiol.2020200370
Porfidia, Valeriani, Pola, Porreca, Rutjes et al., Venous thromboembolism in patients with COVID-19: systematic review and meta-analysis, Thromb Res, doi:10.1016/j.thromres.2020.08.020
Roomi, Saddique, Ullah, Haq, Ashfaq et al., Anticoagulation in COVID-19: a single-center retrospective study, J Community Hosp Intern Med Perspect, doi:10.1080/20009666.2020.1835297
Sahai, Bhandari, Godwin, Mcintyre, Chung et al., Effect of aspirin on short-term outcomes in hospitalized patients with COVID-19, Vasc Med, doi:10.1177/1358863X211012754
Salah, Mehta, Meta-analysis of the effect of aspirin on mortality in COVID-19, Am J Cardiol, doi:10.1016/j.amjcard.2020.12.073
Shawkat, Merrell, Fadel, Amzuta, Amin et al., Multiple thrombotic events in a 67-year-old man 2 weeks after testing positive for SARS-CoV-2: a case report, Am J Case Rep, doi:10.12659/AJCR.925786
Varga, Flammer, Steiger, Haberecker, Andermatt et al., Endothelial cell infection and endotheliitis in COVID-19, Lancet, doi:10.1016/S0140-6736(20)30937-5
Wang, Li, Gu, Wang, Liu et al., Effect of antiplatelet therapy on acute respiratory distress syndrome and mortality in critically ill patients: a meta-analysis, PLoS ONE, doi:10.1371/journal.pone.0154754
Yuan, Chen, Li, Chen, Wang et al., Mortality and pre-hospitalization use of low-dose aspirin in COVID-19 patients with coronary artery disease, J Cell Mol Med, doi:10.1111/jcmm.16198
Zeng, Huang, Guo, Yin, Chen et al., Association of inflammatory markers with the severity of COVID-19: a meta-analysis, Int J Infect Dis, doi:10.1016/j.ijid.2020.05.055
Zhou, Li, Yang, Antiplatelet therapy after percutaneous coronary intervention in patients with COVID-19: implications from clinical features to pathologic findings, Circulation, doi:10.1161/CIRCULATIONAHA.120.046988
DOI record:
{
"DOI": "10.1007/s40261-021-01061-2",
"ISSN": [
"1173-2563",
"1179-1918"
],
"URL": "http://dx.doi.org/10.1007/s40261-021-01061-2",
"alternative-id": [
"1061"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "6 July 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 2,
"value": "30 July 2021"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Funding",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "No financial support was obtained from any individual, institutions, agencies, drug industries or organizations."
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "The authors declare that they have no competing interests."
},
{
"group": {
"label": "Ethics approval",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "This study was approved by the Mansoura Institutional Research Board Ethics (code number: R.20.08.971), which waived the need for informed consent."
},
{
"group": {
"label": "Consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 5,
"value": "The Ethics Committee of Mansoura University waived the need for informed consent from the study population for the collection, analysis, and publication of the retrospectively obtained and anonymized data for this non-interventional study."
},
{
"group": {
"label": "Consent to publish",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 6,
"value": "Not applicable."
},
{
"group": {
"label": "Code availability",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 7,
"value": "Not applicable."
},
{
"group": {
"label": "Availability of data and materials",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 8,
"value": "The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request."
},
{
"group": {
"label": "Author contributions",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 9,
"value": "HWA, SWS, and HASA contributed equally to this work and share first authorship. HA put the idea of the research, built the research team, designed the study, revised the manuscript, and approved the final version of manuscript. HWA and SWS participated in designing the study, collected the data, revised the manuscript, and approved the final version of manuscript. HASA participated in designing the study, wrote the manuscript draft, and approved the final version of manuscript. AMF participated in designing the study, analyzed the data, revised the manuscript, and approved the final version of manuscript. AM and AGA participated in designing the study and in statistical analysis, revised the manuscript, and approved the final version. EM, ED, JBR, GF, and GFN participated in designing this study parallel to another IRB in USA, revised this manuscript, and approved the final version. RS, ME-f, KS, JS, and HA participated in designing the study, revised the manuscript, and approved the final version."
},
{
"label": "Free to read",
"name": "free",
"value": "This content has been made available to all."
}
],
"author": [
{
"affiliation": [],
"family": "Abdelwahab",
"given": "Heba Wagih",
"sequence": "first"
},
{
"affiliation": [],
"family": "Shaltout",
"given": "Shaker Wagih",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sayed Ahmed",
"given": "Hazem A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fouad",
"given": "Ahmed Mahmoud",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Merrell",
"given": "Eric",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Riley",
"given": "Jeffrey B.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Salama",
"given": "Rasha",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abdelrahman",
"given": "Ahmed Gharib",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Darling",
"given": "Edward",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fadel",
"given": "Ghada",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Elfar",
"given": "Mohamed S. A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sabry",
"given": "Khaled",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8961-218X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Shah",
"given": "Jaffer",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Amin",
"given": "Hossam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nieman",
"given": "Gary F.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mishriky",
"given": "Adel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Aiash",
"given": "Hani",
"sequence": "additional"
}
],
"container-title": "Clinical Drug Investigation",
"container-title-short": "Clin Drug Investig",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2021,
7,
30
]
],
"date-time": "2021-07-30T11:02:55Z",
"timestamp": 1627642975000
},
"deposited": {
"date-parts": [
[
2021,
8,
10
]
],
"date-time": "2021-08-10T04:07:49Z",
"timestamp": 1628568469000
},
"indexed": {
"date-parts": [
[
2024,
3,
24
]
],
"date-time": "2024-03-24T07:37:29Z",
"timestamp": 1711265849167
},
"is-referenced-by-count": 11,
"issue": "8",
"issued": {
"date-parts": [
[
2021,
7,
30
]
]
},
"journal-issue": {
"issue": "8",
"published-print": {
"date-parts": [
[
2021,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.springer.com/tdm",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
7,
30
]
],
"date-time": "2021-07-30T00:00:00Z",
"timestamp": 1627603200000
}
},
{
"URL": "https://www.springer.com/tdm",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
7,
30
]
],
"date-time": "2021-07-30T00:00:00Z",
"timestamp": 1627603200000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s40261-021-01061-2.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s40261-021-01061-2/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s40261-021-01061-2.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"page": "723-732",
"prefix": "10.1007",
"published": {
"date-parts": [
[
2021,
7,
30
]
]
},
"published-online": {
"date-parts": [
[
2021,
7,
30
]
]
},
"published-print": {
"date-parts": [
[
2021,
8
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.7326/M20-3012",
"author": "DP Oran",
"doi-asserted-by": "publisher",
"first-page": "362",
"issue": "5",
"journal-title": "Ann Intern Med",
"key": "1061_CR1",
"unstructured": "Oran DP, Topol EJ. Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann Intern Med. 2020;173(5):362–7. https://doi.org/10.7326/M20-3012.",
"volume": "173",
"year": "2020"
},
{
"DOI": "10.15557/PiMR.2020.0004",
"doi-asserted-by": "crossref",
"key": "1061_CR2",
"unstructured": "World Health Organization. Clinical management of COVID-19: interim guidance, 27 May 2020. World Health Organization. License: CC BY-NC-SA 3.0 IGO. https://www.who.int/publications/i/item/clinical-management-of-covid-19. Accessed 8 Dec 2020."
},
{
"DOI": "10.1016/j.ijid.2020.05.055",
"author": "F Zeng",
"doi-asserted-by": "publisher",
"first-page": "467",
"journal-title": "Int J Infect Dis",
"key": "1061_CR3",
"unstructured": "Zeng F, Huang Y, Guo Y, Yin M, Chen X, Xiao L, et al. Association of inflammatory markers with the severity of COVID-19: a meta-analysis. Int J Infect Dis. 2020;96:467–74. https://doi.org/10.1016/j.ijid.2020.05.055.",
"volume": "96",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30937-5",
"author": "Z Varga",
"doi-asserted-by": "publisher",
"first-page": "1417",
"issue": "10234",
"journal-title": "Lancet",
"key": "1061_CR4",
"unstructured": "Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–8. https://doi.org/10.1016/S0140-6736(20)30937-5.",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2015432",
"author": "M Ackermann",
"doi-asserted-by": "publisher",
"first-page": "120",
"issue": "2",
"journal-title": "N Engl J Med",
"key": "1061_CR5",
"unstructured": "Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020;383(2):120–8. https://doi.org/10.1056/NEJMoa2015432.",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1016/S2352-3026(20)30216-7",
"author": "G Goshua",
"doi-asserted-by": "publisher",
"first-page": "e575",
"issue": "8",
"journal-title": "Lancet Haematol.",
"key": "1061_CR6",
"unstructured": "Goshua G, Pine AB, Meizlish ML, Chang CH, Zhang H, Bahel P, et al. Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020;7(8):e575–82. https://doi.org/10.1016/S2352-3026(20)30216-7.",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/j.thromres.2020.04.024",
"author": "C Lodigiani",
"doi-asserted-by": "publisher",
"first-page": "9",
"journal-title": "Thromb Res",
"key": "1061_CR7",
"unstructured": "Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. https://doi.org/10.1016/j.thromres.2020.04.024.",
"volume": "191",
"year": "2020"
},
{
"DOI": "10.1016/j.thromres.2020.04.013",
"author": "FA Klok",
"doi-asserted-by": "publisher",
"first-page": "145",
"journal-title": "Thromb Res",
"key": "1061_CR8",
"unstructured": "Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–7. https://doi.org/10.1016/j.thromres.2020.04.013.",
"volume": "191",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.13372",
"author": "S Bilaloglu",
"doi-asserted-by": "publisher",
"first-page": "799",
"issue": "8",
"journal-title": "JAMA",
"key": "1061_CR9",
"unstructured": "Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in hospitalized patients with COVID-19 in a New York City health system. JAMA. 2020;324(8):799–801. https://doi.org/10.1001/jama.2020.13372.",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1016/j.thromres.2020.08.020",
"author": "A Porfidia",
"doi-asserted-by": "publisher",
"first-page": "67",
"journal-title": "Thromb Res",
"key": "1061_CR10",
"unstructured": "Porfidia A, Valeriani E, Pola R, Porreca E, Rutjes AWS, Di Nisio M. Venous thromboembolism in patients with COVID-19: systematic review and meta-analysis. Thromb Res. 2020;196:67–74. https://doi.org/10.1016/j.thromres.2020.08.020.",
"volume": "196",
"year": "2020"
},
{
"DOI": "10.12659/AJCR.925786",
"author": "A Shawkat",
"doi-asserted-by": "publisher",
"journal-title": "Am J Case Rep.",
"key": "1061_CR11",
"unstructured": "Shawkat A, Merrell ET, Fadel GA, Amzuta I, Amin H, Shah AJ, et al. Multiple thrombotic events in a 67-year-old man 2 weeks after testing positive for SARS-CoV-2: a case report. Am J Case Rep. 2020;21: e925786. https://doi.org/10.12659/AJCR.925786.",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1016/j.jacc.2020.04.031",
"author": "B Bikdeli",
"doi-asserted-by": "publisher",
"first-page": "2950",
"issue": "23",
"journal-title": "J Am Coll Cardiol",
"key": "1061_CR12",
"unstructured": "Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75(23):2950–73. https://doi.org/10.1016/j.jacc.2020.04.031.",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1007/s11906-016-0688-8",
"author": "MS Dzeshka",
"doi-asserted-by": "publisher",
"first-page": "83",
"issue": "11",
"journal-title": "Curr Hypertens Rep",
"key": "1061_CR13",
"unstructured": "Dzeshka MS, Shantsila A, Lip GY. Effects of aspirin on endothelial function and hypertension. Curr Hypertens Rep. 2016;18(11):83. https://doi.org/10.1007/s11906-016-0688-8.",
"volume": "18",
"year": "2016"
},
{
"DOI": "10.1136/fmch-2020-000741",
"author": "HA Sayed Ahmed",
"doi-asserted-by": "publisher",
"issue": "2",
"journal-title": "Fam Med Com Health.",
"key": "1061_CR14",
"unstructured": "Sayed Ahmed HA, Merrell E, Ismail M, Joudeh AI, Riley JB, Shawkat A, et al. Rationales and uncertainties for aspirin use in COVID-19: a narrative review. Fam Med Com Health. 2021;9(2): e000741. https://doi.org/10.1136/fmch-2020-000741.",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1111/irv.12421",
"author": "B Glatthaar-Saalmüller",
"doi-asserted-by": "publisher",
"first-page": "85",
"issue": "1",
"journal-title": "Influenza Other Respir Viruses",
"key": "1061_CR15",
"unstructured": "Glatthaar-Saalmüller B, Mair KH, Saalmüller A. Antiviral activity of aspirin against RNA viruses of the respiratory tract-an in vitro study. Influenza Other Respir Viruses. 2017;11(1):85–92. https://doi.org/10.1111/irv.12421.",
"volume": "11",
"year": "2017"
},
{
"key": "1061_CR16",
"unstructured": "The European Society for Cardiology. ESC Guidance for the Diagnosis and Management of CV Disease during the COVID-19 Pandemic. https://www.escardio.org/static-file/Escardio/Education-General/Topic%20pages/Covid-19/ESC%20Guidance%20Document/ESC-Guidance-COVID-19-Pandemic.pdf. Accessed 5 Mar 2021."
},
{
"key": "1061_CR17",
"unstructured": "COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health. https://files.covid19treatmentguidelines.nih.gov/guidelines/covid19treatmentguidelines.pdf. Accessed 8 Dec 2020."
},
{
"DOI": "10.1111/bjh.16792",
"author": "DO Griffin",
"doi-asserted-by": "publisher",
"first-page": "e11",
"issue": "1",
"journal-title": "Br J Haematol",
"key": "1061_CR18",
"unstructured": "Griffin DO, Jensen A, Khan M, Chin J, Chin K, Parnell R, Awwad C, Patel D. Arterial thromboembolic complications in COVID-19 in low-risk patients despite prophylaxis. Br J Haematol. 2020;190(1):e11–3. https://doi.org/10.1111/bjh.16792.",
"volume": "190",
"year": "2020"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.046988",
"author": "X Zhou",
"doi-asserted-by": "publisher",
"first-page": "1736",
"issue": "22",
"journal-title": "Circulation",
"key": "1061_CR19",
"unstructured": "Zhou X, Li Y, Yang Q. Antiplatelet therapy after percutaneous coronary intervention in patients with COVID-19: implications from clinical features to pathologic findings. Circulation. 2020;141(22):1736–8. https://doi.org/10.1161/CIRCULATIONAHA.120.046988.",
"volume": "141",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0154754",
"author": "L Wang",
"doi-asserted-by": "publisher",
"issue": "5",
"journal-title": "PLoS ONE",
"key": "1061_CR20",
"unstructured": "Wang L, Li H, Gu X, Wang Z, Liu S, Chen L. Effect of antiplatelet therapy on acute respiratory distress syndrome and mortality in critically ill patients: a meta-analysis. PLoS ONE. 2016;11(5): e0154754. https://doi.org/10.1371/journal.pone.0154754.",
"volume": "11",
"year": "2016"
},
{
"DOI": "10.1213/ANE.0000000000005292",
"author": "JH Chow",
"doi-asserted-by": "publisher",
"first-page": "930",
"issue": "4",
"journal-title": "Anesth Analg",
"key": "1061_CR21",
"unstructured": "Chow JH, Khanna AK, Kethireddy S, Yamane D, Levine A, Jackson AM, et al. Aspirin use is associated with decreased mechanical ventilation, ICU admission, and in-hospital mortality in hospitalized patients with COVID-19. Anesth Analg. 2021;132(4):930–41. https://doi.org/10.1213/ANE.0000000000005292.",
"volume": "132",
"year": "2021"
},
{
"DOI": "10.1002/ajh.26102",
"author": "ML Meizlish",
"doi-asserted-by": "publisher",
"first-page": "471",
"issue": "4",
"journal-title": "Am J Hematol",
"key": "1061_CR22",
"unstructured": "Meizlish ML, Goshua G, Liu Y, Fine R, Amin K, Chang E, et al. Intermediate-dose anticoagulation, aspirin, and in-hospital mortality in COVID-19: a propensity score-matched analysis. Am J Hematol. 2021;96(4):471–9. https://doi.org/10.1002/ajh.26102.",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2021.05.016",
"author": "JW Martha",
"doi-asserted-by": "publisher",
"first-page": "6",
"journal-title": "Int J Infect Dis",
"key": "1061_CR23",
"unstructured": "Martha JW, Pranata R, Lim MA, Wibowo A, Akbar MR. Active prescription of low-dose aspirin during or prior to hospitalization and mortality in COVID-19: a systematic review and meta-analysis of adjusted effect estimates. Int J Infect Dis. 2021;108:6–12. https://doi.org/10.1016/j.ijid.2021.05.016.",
"volume": "108",
"year": "2021"
},
{
"DOI": "10.1111/jcmm.16198",
"author": "S Yuan",
"doi-asserted-by": "publisher",
"first-page": "1263",
"issue": "2",
"journal-title": "J Cell Mol Med",
"key": "1061_CR24",
"unstructured": "Yuan S, Chen P, Li H, Chen C, Wang F, Wang DW. Mortality and pre-hospitalization use of low-dose aspirin in COVID-19 patients with coronary artery disease. J Cell Mol Med. 2020;25(2):1263–73. https://doi.org/10.1111/jcmm.16198.",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.1016/j.amjcard.2020.12.073",
"author": "HM Salah",
"doi-asserted-by": "publisher",
"first-page": "158",
"journal-title": "Am J Cardiol",
"key": "1061_CR25",
"unstructured": "Salah HM, Mehta JL. Meta-analysis of the effect of aspirin on mortality in COVID-19. Am J Cardiol. 2021;142:158–9. https://doi.org/10.1016/j.amjcard.2020.12.073.",
"volume": "142",
"year": "2021"
},
{
"DOI": "10.1148/radiol.2462070712",
"author": "DM Hansell",
"doi-asserted-by": "publisher",
"first-page": "697",
"issue": "3",
"journal-title": "Radiology",
"key": "1061_CR26",
"unstructured": "Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008;246(3):697–722. https://doi.org/10.1148/radiol.2462070712.",
"volume": "246",
"year": "2008"
},
{
"DOI": "10.1148/radiol.2020200370",
"author": "F Pan",
"doi-asserted-by": "publisher",
"first-page": "715",
"issue": "3",
"journal-title": "Radiology",
"key": "1061_CR27",
"unstructured": "Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19). Radiology. 2020;295(3):715–21. https://doi.org/10.1148/radiol.2020200370.",
"volume": "295",
"year": "2020"
},
{
"key": "1061_CR28",
"unstructured": "Masoud HH, Elassal, G, Hassany M, Shawky A, Abdel Hakim M, Zaky, S, et al. Management Protocol for COVID-19 Patients MoHP Protocol for COVID19 November 2020. https://www.researchgate.net/publication/345813633_Management_Protocol_for_COVID-19_Patients_MoHP_Protocol_for_COVID19_November_2020/link/5faeb3df92851cf24cca8643/download. Accessed 9 Mar 2021."
},
{
"DOI": "10.1378/chest.11-2293",
"author": "JW Eikelboom",
"doi-asserted-by": "publisher",
"first-page": "e89S",
"issue": "2",
"journal-title": "Chest",
"key": "1061_CR29",
"unstructured": "Eikelboom JW, Hirsh J, Spencer FA, Baglin TP, Weitz JI. Antiplatelet drugs: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2):e89S-e119S. https://doi.org/10.1378/chest.11-2293.",
"volume": "141",
"year": "2012"
},
{
"DOI": "10.1182/blood-2015-04-640649",
"author": "J Cho",
"doi-asserted-by": "publisher",
"first-page": "3523",
"issue": "23",
"journal-title": "Blood",
"key": "1061_CR30",
"unstructured": "Cho J. A paradigm shift in platelet transfusion therapy. Blood. 2015;125(23):3523–5. https://doi.org/10.1182/blood-2015-04-640649.",
"volume": "125",
"year": "2015"
},
{
"DOI": "10.1016/j.avsg.2020.08.087",
"author": "I Cheruiyot",
"doi-asserted-by": "publisher",
"first-page": "273",
"journal-title": "Ann Vasc Surg",
"key": "1061_CR31",
"unstructured": "Cheruiyot I, Kipkorir V, Ngure B, Misiani M, Munguti J, Ogeng’o J. Arterial thrombosis in coronavirus disease 2019 patients: a rapid systematic review. Ann Vasc Surg. 2021;70:273–81. https://doi.org/10.1016/j.avsg.2020.08.087.",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.1016/j.thromres.2020.08.022",
"author": "SK Kunutsor",
"doi-asserted-by": "publisher",
"first-page": "27",
"journal-title": "Thromb Res",
"key": "1061_CR32",
"unstructured": "Kunutsor SK, Laukkanen JA. Incidence of venous and arterial thromboembolic complications in COVID-19: a systematic review and meta-analysis. Thromb Res. 2020;196:27–30. https://doi.org/10.1016/j.thromres.2020.08.022.",
"volume": "196",
"year": "2020"
},
{
"DOI": "10.3389/fcvm.2020.562708",
"author": "T Diaz",
"doi-asserted-by": "publisher",
"journal-title": "Front Cardiovasc Med.",
"key": "1061_CR33",
"unstructured": "Diaz T, Trachtenberg BH, Abraham SJK, KosagiSharaf R, Durant-Archibold AA. Aspirin bioactivity for prevention of cardiovascular injury in COVID-19. Front Cardiovasc Med. 2020;7: 562708. https://doi.org/10.3389/fcvm.2020.562708.",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1002/rth2.12353",
"author": "J Liu",
"doi-asserted-by": "publisher",
"first-page": "518",
"issue": "4",
"journal-title": "Res Pract Thromb Haemost.",
"key": "1061_CR34",
"unstructured": "Liu J, Li J, Arnold K, Pawlinski R, Key NS. Using heparin molecules to manage COVID-2019. Res Pract Thromb Haemost. 2020;4(4):518–23. https://doi.org/10.1002/rth2.12353.",
"volume": "4",
"year": "2020"
},
{
"DOI": "10.1016/j.ijcard.2020.09.064",
"author": "C Godino",
"doi-asserted-by": "publisher",
"first-page": "261",
"journal-title": "Int J Cardiol",
"key": "1061_CR35",
"unstructured": "Godino C, Scotti A, Maugeri N, Mancini N, Fominskiy E, Margonato A, et al. Antithrombotic therapy in patients with COVID-19?—rationale and evidence. Int J Cardiol. 2021;324:261–6. https://doi.org/10.1016/j.ijcard.2020.09.064.",
"volume": "324",
"year": "2021"
},
{
"DOI": "10.1177/1358863X211012754",
"author": "A Sahai",
"doi-asserted-by": "publisher",
"journal-title": "Vasc Med",
"key": "1061_CR36",
"unstructured": "Sahai A, Bhandari R, Godwin M, McIntyre T, Chung MK, Iskandar JP, et al. Effect of aspirin on short-term outcomes in hospitalized patients with COVID-19. Vasc Med. 2021. https://doi.org/10.1177/1358863X211012754.",
"year": "2021"
},
{
"DOI": "10.1213/ANE.0000000000005401",
"author": "M Giorgi-Pierfranceschi",
"doi-asserted-by": "publisher",
"first-page": "e89",
"issue": "5",
"journal-title": "Anesth Analg",
"key": "1061_CR37",
"unstructured": "Giorgi-Pierfranceschi M. Is aspirin effective in preventing ICU admission in patients with COVID-19 pneumonia? Anesth Analg. 2021;132(5):e89–90. https://doi.org/10.1213/ANE.0000000000005401.",
"volume": "132",
"year": "2021"
},
{
"DOI": "10.1080/20009666.2020.1835297",
"author": "SS Roomi",
"doi-asserted-by": "publisher",
"first-page": "17",
"issue": "1",
"journal-title": "J Community Hosp Intern Med Perspect.",
"key": "1061_CR38",
"unstructured": "Roomi SS, Saddique M, Ullah W, Haq S, Ashfaq A, Madara J, et al. Anticoagulation in COVID-19: a single-center retrospective study. J Community Hosp Intern Med Perspect. 2021;11(1):17–22. https://doi.org/10.1080/20009666.2020.1835297.",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/j.chest.2017.08.008",
"author": "TA Miano",
"doi-asserted-by": "publisher",
"first-page": "133",
"issue": "1",
"journal-title": "Chest",
"key": "1061_CR39",
"unstructured": "Miano TA, Cuker A, Christie JD, Martin N, Smith B, Makley AT, et al. Comparative effectiveness of enoxaparin vs dalteparin for thromboprophylaxis after traumatic injury. Chest. 2018;153(1):133–42. https://doi.org/10.1016/j.chest.2017.08.008.",
"volume": "153",
"year": "2018"
},
{
"DOI": "10.1056/NEJMoa1014475",
"author": "D Cook",
"doi-asserted-by": "publisher",
"first-page": "1305",
"issue": "14",
"journal-title": "N Engl J Med",
"key": "1061_CR40",
"unstructured": "PROTECT Investigators for the Canadian Critical Care Trials Group and the Australian and New Zealand Intensive Care Society Clinical Trials Group, Cook D, Meade M, Guyatt G, Walter S, Heels-Ansdell D, et al. Dalteparin versus unfractionated heparin in critically ill patients. N Engl J Med. 2011;364(14):1305–14. https://doi.org/10.1056/NEJMoa1014475.",
"volume": "364",
"year": "2011"
},
{
"DOI": "10.1007/s00068-013-0333-z",
"author": "OT Okoye",
"doi-asserted-by": "publisher",
"first-page": "183",
"issue": "2",
"journal-title": "Eur J Trauma Emerg Surg",
"key": "1061_CR41",
"unstructured": "Okoye OT, Gelbard R, Inaba K, Esparza M, Belzberg H, Talving P, Teixeira PG, et al. Dalteparin versus enoxaparin for the prevention of venous thromboembolic events in trauma patients. Eur J Trauma Emerg Surg. 2014;40(2):183–9. https://doi.org/10.1007/s00068-013-0333-z.",
"volume": "40",
"year": "2014"
},
{
"DOI": "10.1056/NEJMoa1601747",
"author": "AT Cohen",
"doi-asserted-by": "publisher",
"first-page": "534",
"issue": "6",
"journal-title": "N Engl J Med",
"key": "1061_CR42",
"unstructured": "Cohen AT, Harrington RA, Goldhaber SZ, Hull RD, Wiens BL, Gold A, Hernandez AF, Gibson CM, APEX Investigators. Extended thromboprophylaxis with betrixaban in acutely ill medical patients. N Engl J Med. 2016;375(6):534–44. https://doi.org/10.1056/NEJMoa1601747.",
"volume": "375",
"year": "2016"
},
{
"DOI": "10.1056/NEJMoa1111096",
"author": "AT Cohen",
"doi-asserted-by": "publisher",
"first-page": "513",
"issue": "6",
"journal-title": "N Engl J Med",
"key": "1061_CR43",
"unstructured": "Cohen AT, Spiro TE, Büller HR, Haskell L, Hu D, Hull R, Mebazaa A, Merli G, Schellong S, Spyropoulos AC, Tapson V, MAGELLAN Investigators. Rivaroxaban for thromboprophylaxis in acutely ill medical patients. N Engl J Med. 2013;368(6):513–23. https://doi.org/10.1056/NEJMoa1111096.",
"volume": "368",
"year": "2013"
},
{
"DOI": "10.1056/NEJMoa1110899",
"author": "SZ Goldhaber",
"doi-asserted-by": "publisher",
"first-page": "2167",
"issue": "23",
"journal-title": "N Engl J Med",
"key": "1061_CR44",
"unstructured": "Goldhaber SZ, Leizorovicz A, Kakkar AK, Haas SK, Merli G, Knabb RM, Weitz JI, ADOPT Trial Investigators. Apixaban versus enoxaparin for thromboprophylaxis in medically ill patients. N Engl J Med. 2011;365(23):2167–77. https://doi.org/10.1056/NEJMoa1110899.",
"volume": "365",
"year": "2011"
}
],
"reference-count": 44,
"references-count": 44,
"relation": {},
"resource": {
"primary": {
"URL": "https://link.springer.com/10.1007/s40261-021-01061-2"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Pharmacology (medical)",
"General Medicine"
],
"subtitle": [],
"title": "Acetylsalicylic Acid Compared with Enoxaparin for the Prevention of Thrombosis and Mechanical Ventilation in COVID-19 Patients: A Retrospective Cohort Study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "41"
}