Clinical characteristics and acute complication of COVID-19 patients with diabetes: a multicenter, retrospective study in Southern China
et al., Frontiers in Endocrinology, doi:10.3389/fendo.2023.1237832, Aug 2023
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
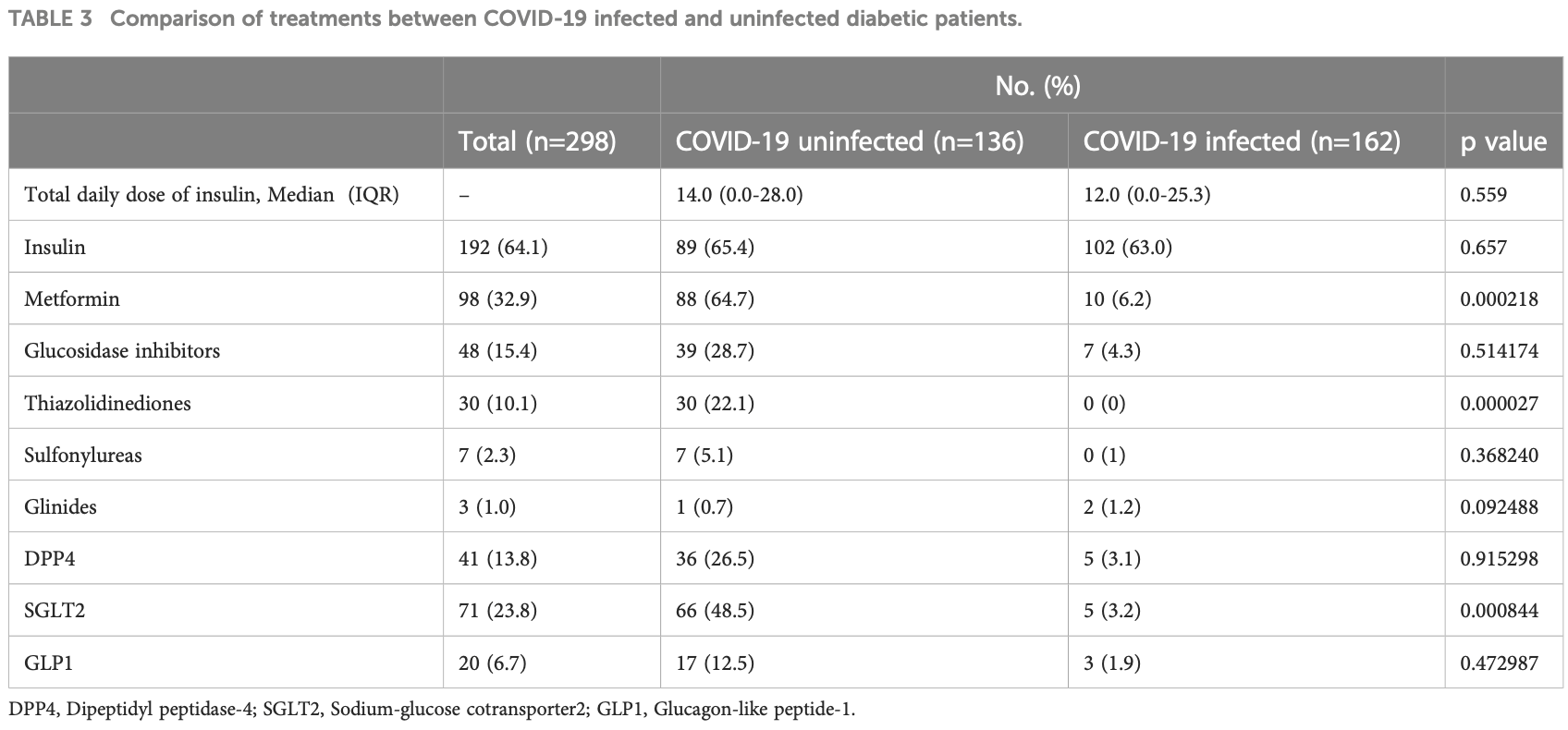
Retrospective 298 hospitalized type 2 diabetes patients in China showing metformin use associated with not having COVID-19, however the analysis considers treatment during hospitalization, and authors note that in this population metformin may have been specifically discontinued for COVID-19 patients.
This study is excluded in meta-analysis:
substantial unadjusted confounding by indication likely.
Zhou et al., 12 Aug 2023, retrospective, China, peer-reviewed, 14 authors, study period 1 December, 2022 - 1 February, 2023.
Clinical characteristics and acute complication of COVID-19 patients with diabetes: a multicenter, retrospective study in Southern China
Frontiers in Endocrinology, doi:10.3389/fendo.2023.1237832
This study aims to describe the clinical characteristics, laboratory data and complications of hospitalized COVID-19 patients with type 2 diabetes mellitus (T2DM) since epidemic prevention and control optimization was adjusted in December 2022 in China. Methods: This retrospective multicenter study included 298 patients with confirmed type 2 diabetes mellitus with or without COVID-19. We collected data from the first wave of the pandemic in The Fifth Affiliated
Ethics statement The studies involving humans were approved by the Fifth Affiliated of Guangzhou Medical University Research Ethics Committee (GYWY-L2023-64). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions C-pZ and W-pS performed the general development and design of the study and contributed to critical revisions. X-yZ is the first author who contributed to the design, statistical analysis and manuscript writing of the study. S-fH wrote sections of the manuscript. S-fH, J-xL, H-nZ, LX, X-zW, K-hG, LZ, TL, H-mY, M-rL, and X-yL contributed to data collection and helped perform the analysis with constructive discussion. All authors contributed to the article and approved the submitted version.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Agyeman, Chin, Landersdorfer, Liew, Ofori-Asenso, Smell and taste dysfunction in patients with COVID-19: A systematic review and meta-analysis
Alguwaihes, Me, Megdad, Albader, Alsari et al., Diabetes and Covid-19 among hospitalized patients in Saudi Arabia: a singlecentre retrospective study, Cardiovasc Diabetol, doi:10.1186/s12933-020-01184-4
Baidya, Singh, Bajaj, Zargar, Singh et al., Diabetes and COVID-19: A review, J ASEAN Fed Endocr Soc, doi:10.15605/jafes.035.01.06
Bi, Zhang, Li, Kan, Li et al., Contributing factors of fatigue in patients with type 2 diabetes: A systematic review, Psychoneuroendocrinology, doi:10.1016/j.psyneuen.2021.105280
Bornstein, Rubino, Khunti, Mingrone, Hopkins et al., Practical recommendations for the management of diabetes in patients with
Carboni, Carta, Carboni, Can pioglitazone be potentially useful therapeutically in treating patients with COVID-19? Med Hypotheses, doi:10.1016/j.mehy.2020.109776
Cariou, Hadjadj, Wargny, Pichelin, Al-Salameh et al., Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study, Diabetologia, doi:10.1007/s00125-020-05180-x
Chen, Yang, Cheng, Chen, Peng et al., Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucoselowering medication, Diabetes Care, doi:10.2337/dc20-0660
Chu, Tsang, Tang, Lam, Lai et al., Soleimani M. Acute kidney injury in SARS-coV-2 infection: Direct effect of virus on kidney proximal tubule cells, Int J Mol Sci, doi:10.3390/ijms21093275
Conway, Gould, Westley, Raju, Oklopcic et al., Characteristics of patients with diabetes hospitalised for COVID-19 infection-a brief case series report, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108460
Freeman, Management of hypoglycemia in older adults with type 2 diabetes, Postgrad Med, doi:10.1080/00325481.2019.1578590
Glaser, Kruger, Merkel, Bramlage, Herth, Chronic obstructive pulmonary disease and diabetes mellitus: a systematic review of the literature, Respiration, doi:10.1159/000369863
Guo, Li, Dong, Zhou, Zhang et al., Diabetes is a risk factor for the progression and prognosis of COVID-19, Diabetes Metab Res Rev, doi:10.1002/dmrr.3319
Hamming, Timens, Bulthuis, Lely, Navis et al., Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis, J Pathol, doi:10.1002/path.1570
Hirsch, Ng, Ross, Sharma, Shah et al., Acute kidney injury in patients hospitalized with COVID-19, Kidney Int, doi:10.1016/j.kint.2020.05.006
Hoier, Chaaban, Andersen, Possibilities for maintaining appetite in recovering COVID-19 patients, Foods, doi:10.3390/foods10020464
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, Lancet, doi:10.1016/S0140-6736(20)30183-5
Kamrath, Monkemoller, Biester, Rohrer, Warncke et al., Ketoacidosis in children and adolescents with newly diagnosed type 1 diabetes during the COVID-19 pandemic in Germany, JAMA, doi:10.1001/jama.2020.13445
Klein, Krishnan, Glick, Smith, Systematic review of the association between lung function and Type 2 diabetes mellitus, Diabetes Med, doi:10.1111/j.1464-5491.2010.03073.x
Klein, Smith, Tipping, Peng, Williams, Reduced diffusion lung capacity in patients with type 2 diabetes mellitus predicts hospitalization for pneumonia, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2010.12.012
Li, Bai, Hashikawa, The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients, J Med Virol, doi:10.1002/jmv.25728
Li, Wang, Chen, Zuo, Zhang et al., COVID-19 infection may cause ketosis and ketoacidosis, Diabetes Obes Metab, doi:10.1111/dom.14057
Mcgurnaghan, Weir, Bishop, Kennedy, Blackbourn et al., Risks of and risk factors for COVID-19 disease in people with diabetes: a cohort study of the total population of Scotland, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30405-8
Mithal, Jevalikar, Sharma, Singh, Farooqui et al., High prevalence of diabetes and other comorbidities in hospitalized patients with COVID-19 in Delhi, India, and their association with outcomes, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.12.029
Muller, Gross, Conzelmann, Kruger, Merle et al., SARS-CoV-2 infects and replicates in cells of the human endocrine and exocrine pancreas, Nat Metab, doi:10.1038/s42255-021-00347-1
Narasimhulu, Singla, Mechanisms of COVID-19 pathogenesis in diabetes, Am J Physiol Heart Circ Physiol, doi:10.1152/ajpheart.00204.2022
Nguyen, Ho, Nguyen, Ho, Li et al., Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: A meta-analysis, Metabolism, doi:10.1016/j.metabol.2022.155196
Pelle, Zaffina, Provenzano, Moirano, Arturi, COVID-19 and diabetes-Two giants colliding: From pathophysiology to management, Front Endocrinol (Lausanne), doi:10.3389/fendo.2022.974540
Rayman, Lumb, Kennon, Cottrell, Nagi et al., Guidance on the management of Diabetic Ketoacidosis in the exceptional circumstances of the COVID-19 pandemic, Nat Rev Endocrinol, doi:10.1038/s41574-020-00435-4
Renzo, Gualtieri, Pivari, Soldati, Attina et al., Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey, J Transl Med, doi:10.1186/s12967-020-02399-5
Richardson, Hirsch, Narasimhan, Crawford, Mcginn et al., Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area, JAMA, doi:10.1001/jama.2020.6775
Santi, Zoppini, Locatelli, Finocchio, Cappa et al., Type 2 diabetes is associated with an increased prevalence of respiratory symptoms as compared to the general population, BMC Pulm Med, doi:10.1186/s12890-017-0443-1
Scheen, SGLT2 inhibition during the COVID-19 epidemic: Friend or foe?, Diabetes Metab, doi:10.1016/j.diabet.2020.06.003
Shi, Zhang, Jiang, Zhang, Hu et al., Clinical characteristics and risk factors for mortality of COVID-19 patients with diabetes in Wuhan, China: A two-center, retrospective study, Diabetes Care, doi:10.2337/dc20-0598
Singh, Khunti, COVID-19 and diabetes, Annu Rev Med, doi:10.1146/annurev-med-042220-011857
Sinha, Cheng, Schaffer, Aldape, Schiff et al., In vitro and in vivo identification of clinically approved drugs that modify ACE2 expression, Mol Syst Biol, doi:10.15252/msb.20209628
Soler, Wysocki, Batlle, ACE2 alterations in kidney disease, Nephrol Dial Transplant, doi:10.1093/ndt/gft320
Stewart, Role of exercise training on cardiovascular disease in persons who have type 2 diabetes and hypertension, Cardiol Clin, doi:10.1016/j.ccl.2004.06.007
Tian, Nie, Sun, Ye, The epidemiological features of the SARS-CoV-2 omicron subvariant BA.5 and its evasion of the neutralizing activity of vaccination and prior infection, Vaccines (Basel), doi:10.3390/vaccines10101699
Vieira, Souto, Sanchez-Lopez, Machado, Severino et al., Sugar-lowering drugs for type 2 diabetes mellitus and metabolic syndrome-strategies for in Vivo administration: Part-II, J Clin Med, doi:10.3390/jcm8091332
Vinik, Maser, Mitchell, Freeman, Diabetic autonomic neuropathy, Diabetes Care, doi:10.2337/diacare.26.5.1553
Wang, Du, Zhu, Glycosylated hemoglobin is associated with systemic inflammation, hypercoagulability, and prognosis of COVID-19 patients, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108214
Wang, Gao, Zhang, Huang, Zhang et al., Prevalence and ethnic pattern of diabetes and prediabetes in China, JAMA, doi:10.1001/jama.2017.7596
Wu, Lidsky, Lee, Cheng, Nakayama, SARS-CoV-2 infects human pancreatic beta cells and elicits beta cell impairment, Cell Metab, doi:10.1016/j.cmet.2021.05.013
Yan, Yang, Wang, Ren, Zhang et al., Clinical characteristics and outcomes of patients with severe covid-19 with diabetes, BMJ Open Diabetes Res Care, doi:10.1136/bmjdrc-2020-001343
Zheng, Wu, Yan, Potential biochemical mechanisms of lung injury in diabetes, Aging Dis, doi:10.14336/AD.2016.0627
