The causal effect of physical activity intensity on COVID-19 susceptibility, hospitalization, and severity: Evidence from a mendelian randomization study
et al., Frontiers in Physiology, doi:10.3389/fphys.2023.1089637, Mar 2023
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
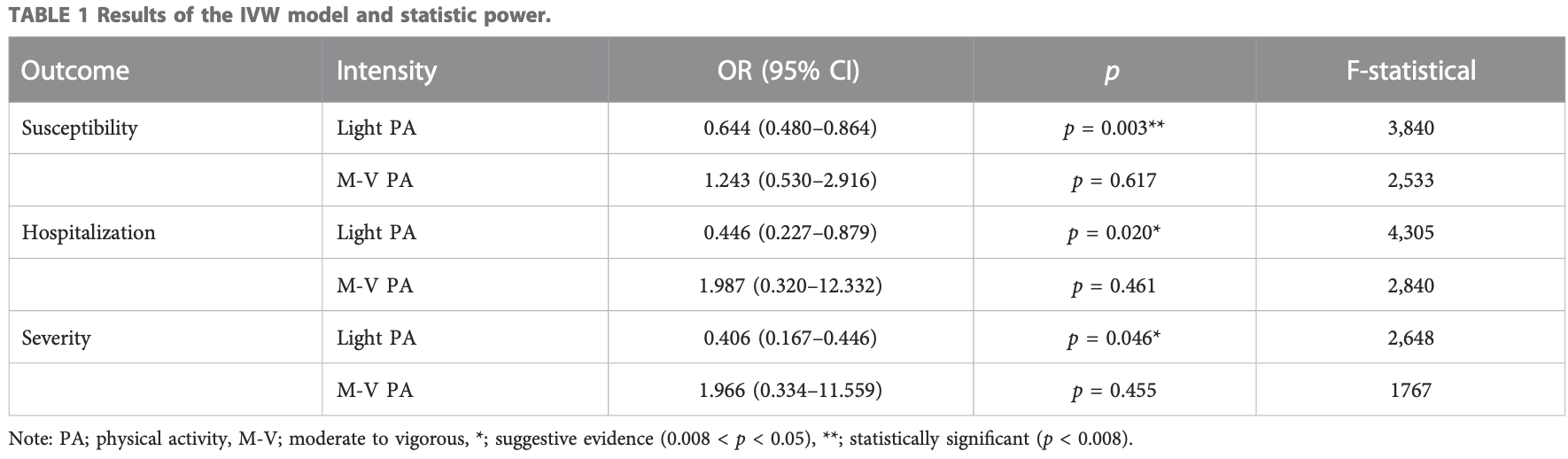
Mendelian randomization study showing lower risk of COVID-19 severity, hospitalization, and cases with light physical activity, but no significant difference for moderate-to-vigorous physical activity. Authors note that they were unable to analyze moderate intensity physical activity because the database only provides two categories (light and moderate-to-vigorous).
Zhang et al., 8 Mar 2023, United Kingdom, peer-reviewed, 4 authors.
Contact: hanson-swu@foxmail.com.
The causal effect of physical activity intensity on COVID-19 susceptibility, hospitalization, and severity: Evidence from a mendelian randomization study
Frontiers in Physiology, doi:10.3389/fphys.2023.1089637
The protection of physical activity (PA) against COVID-19 is a rising research interest. However, the role of physical activity intensity on this topic is yet unclear. To bridge the gap, we performed a Mendelian randomization (MR) study to verify the causal influence of light and moderate-to-vigorous PA on COVID-19 susceptibility, hospitalization, and severity. The Genome-Wide Association Study (GWAS) dataset of PA (n = 88,411) was obtained from the UK biobank and the datasets of COVID-19 susceptibility (n = 1,683,768), hospitalization (n = 1,887,658), and severity (n = 1,161,073) were extracted from the COVID-19 Host Genetics Initiative. A random-effect inverse variance weighted (IVW) model was carried out to estimate the potential causal effects. A Bonferroni correction was used for counteracting. The problem of multiple comparisons. MR-Egger test, MR-PRESSO test, Cochran's Q statistic, and Leave-One-Out (LOO) were used as sensitive analysis tools. Eventually, we found that light PA significantly reduced the risk of COVID-19 infection (OR = 0.644, 95% CI: 0.480-0.864, p = 0.003). Suggestive evidence indicated that light PA reduced the risks of COVID-19 hospitalization (OR = 0.446, 95% CI: 0.227 to 0.879, p = 0.020) and severe complications (OR = 0.406, 95% CI: 0.167-0.446, p = 0.046). By comparison, the effects of moderate-to-vigorous PA on the three COVID-19 outcomes were all non-significant. Generally, our findings may offer evidence for prescribing personalized prevention and treatment programs. Limited by the available datasets and the quality of evidence, further research is warranted to reexamine the effects of light PA on COVID-19 when new GWAS datasets emerge.
Author contributions Conceptualization, HL; data curation, XZ; formal analysis, XZ; investigation, XZ and HL; project administration, SF and HL; supervision, SF and HL; writing-original draft, XZ and HL; writing-review and editing, XZ, XY, and HL. All authors have read and agreed to the published version of the manuscript.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2023.1089637/ full#supplementary-material
References
Bahls, Leitzmann, Karch, Teumer, Dörr et al., Physical activity, sedentary behavior and risk of coronary artery disease, myocardial infarction and ischemic stroke: A two-sample mendelian randomization study, Clin. Res. Cardiol, doi:10.1007/s00392-021-01846-7
Bowden, Davey Smith, Burgess, Mendelian randomization with invalid instruments: Effect estimation and bias detection through egger regression, Int. J. Epidemiol, doi:10.1093/ije/dyv080
Brion, Shakhbazov, Visscher, Calculating statistical power in Mendelian randomization studies, Int. J. Epidemiol, doi:10.1093/ije/dyt179
Burgess, Thompson, Burgess, Bowden, Fall et al., Sensitivity analyses for robust causal inference from Mendelian randomization analyses with multiple genetic variants, Epidemiol. Camb. Mass.), doi:10.1097/EDE.0000000000000559
Chen, Hong, Gao, Luo, Cai et al., Causal relationship between physical activity, leisure sedentary behaviors and COVID-19 risk: A mendelian randomization study, J. Transl. Med, doi:10.1186/s12967-022-03407-6
Chen, Xu, Wang, Li, Shuai et al., New-onset autoimmune phenomena post-COVID-19 vaccination, Immunology, doi:10.1111/imm.13443
Covid19-Hgi, The COVID-19 Host Genetics Initiative, a global initiative to elucidate the role of host genetic factors in susceptibility and severity of the SARS-CoV-2 virus pandemic, Eur. J. Hum. Genet, doi:10.1038/s41431-020-0636-6
Cui, Tian, Using genetic variants to evaluate the causal effect of serum vitamin D concentration on COVID-19 susceptibility, severity and hospitalization traits: A mendelian randomization study, J. Transl. Med, doi:10.1186/s12967-021-02973-5
Davies, Holmes, Smith, Reading mendelian randomisation studies: A guide, glossary, and checklist for clinicians, Bmj, doi:10.1136/bmj.k601
Diamond, Kanneganti, Innate immunity: The first line of defense against SARS-CoV-2, Nat. Immunol, doi:10.1038/s41590-021-01091-0
Greenhalgh, Jimenez, Prather, Tufekci, Fisman et al., Ten scientific reasons in support of airborne transmission of SARS-CoV-2, lancet, doi:10.1016/S0140-6736(21)00869-2
Hamer, Kivimäki, Gale, Batty, Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK, Brain, Behav. Immun, doi:10.1016/j.bbi.2020.05.059
Hebert, Moderate to vigorous physical activity and risk of upper-respiratory tract infection, Med. Sci. sports Exerc, doi:10.1097/00005768-200208000-00003
Hemani, Bowden, Smith, Evaluating the potential role of pleiotropy in Mendelian randomization studies, Hum. Mol. Genet, doi:10.1093/hmg/ddy163
Jee, Physical exercise for strengthening innate immunity during COVID-19 pandemic: 4th series of scientific evidence, J. Exerc. rehabilitation, doi:10.12965/jer.2040712.356
Kanai, Tanaka, Okada, Empirical estimation of genome-wide significance thresholds based on the 1000 Genomes Project data set, J. Hum. Genet
Karim, Oliveira, New SARS-CoV-2 variants-Clinical, public health, and vaccine implications, N. Engl. J. Med, doi:10.1056/NEJMc2100362
Larsson, Bäck, Rees, Mason, Burgess, Body mass index and body composition in relation to 14 cardiovascular conditions in UK biobank: A mendelian randomization study, Eur. heart J, doi:10.1093/eurheartj/ehz388
Leong, Cole, Brenner, Meigs, Florez et al., Cardiometabolic risk factors for COVID-19 susceptibility and severity: A mendelian randomization analysis, PLoS Med, doi:10.1371/journal.pmed.1003553
Lin, Yang, Fu, Lin, Zhang et al., Impairment of kidney function and kidney cancer: A bidirectional mendelian randomization study, Cancer Med, doi:10.1002/cam4.5204/cam4.5204
Liu, Zhang, Li, Liu, Tong et al., A Mendelian Randomization Study of plasma homocysteine levels and cerebrovascular and neurodegenerative diseases, Front. Genet, doi:10.3389/fgene.2021.653032
Matthews, Ockene, Freedson, Rosal, Merriam, None
Nieman, Nigro, Polito, Alfieri, Mancini et al., Exercise, upper respiratory tract infection, and the immune system, Med. Sci. sports Exerc, doi:10.1249/00005768-199402000-00002
Papadimitriou, Dimou, Gill, Tzoulaki, Murphy et al., Genetically predicted circulating concentrations of micronutrients and risk of breast cancer: A mendelian randomization study, Eur. J. Appl. Physiology, doi:10.1002/ijc.33246
Qi, Dutta, Leroux, Ray, Muschelli et al., None
Ren, Simons, Wesselius, Stehouwer, Brouwers, None
Scarmeas, Luchsinger, Schupf, Brickman, Cosentino et al., Physical activity, diet, and risk of Alzheimer disease, Jama, doi:10.1001/jama.2009.1144
Sekula, Del Greco, Pattaro, Köttgen, Mendelian randomization as an approach to assess causality using observational data, J. Am. Soc. Nephrol, doi:10.1681/ASN.2016010098
Singanayagam, Hakki, Dunning, Madon, Crone et al., Community transmission and viral load kinetics of the SARS-CoV-2 delta (B. 1.617. 2) variant in vaccinated and unvaccinated individuals in the UK: A prospective, longitudinal, cohort study, Lancet Infect. Dis, doi:10.1016/S1473-3099(21)00648-4
Smith, Hemani, Mendelian randomization: Genetic anchors for causal inference in epidemiological studies, Hum. Mol. Genet, doi:10.1093/hmg/ddu328
Steenkamp, Saggers, Bandini, Stranges, Choi et al., Small steps, strong shield: Directly measured, moderate physical activity in 65 361 adults is associated with significant protective effects from severe COVID-19 outcomes, Br. J. SPORTS Med, doi:10.1136/bjsports-2021-105159
Verbanck, Chen, Neale, Do, Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases, Nat. Genet, doi:10.1038/s41588-018-0099-7
Wannamethee, Shaper, Physical activity in the prevention of cardiovascular disease: An epidemiological perspective, SPORTS Med, doi:10.2165/00007256-200131020-00003
Weber, Insaf, Hall, Talbot, Huff, Assessing the impact of fine particulate matter (PM2.5) on respiratory-cardiovascular chronic diseases in the New York City Metropolitan area using Hierarchical Bayesian Model estimates, Environ. Res, doi:10.1016/j.envres.2016.07.012
Woods, Hutchinson, Powers, Roberts, Gomez-Cabrera et al., The COVID-19 pandemic and physical activity, Sports Med. Health Sci, doi:10.1016/j.smhs.2020.05.006
Yeung, Li, He, Kwok, Schooling et al., Addiction., Association of smoking, lung function and COPD in COVID-19 risk: A two-step mendelian randomization study
Yuki, Fujiogi, Koutsogiannaki, COVID-19 pathophysiology: A review, Clin. Immunol, doi:10.1016/j.clim.2020.108427
Zhang, Browning, Luo, Li, Can sports cartoon watching in childhood promote adult physical activity and mental health? A pathway analysis in Chinese adults
Zhang, Feng, Peng, Li, Using structural equation modeling to examine pathways between physical activity and sleep quality among Chinese TikTok users, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph19095142
Zhang, Li, Sun, He, Xu et al., Physical activity and COVID-19: An observational and mendelian randomisation study, J. Glob. health, doi:10.7189/jogh.10.020514
Zhang, Liang, Yu, Du, Cheng et al., A systematic review of vaccine breakthrough infections by SARS-CoV-2 delta variant, Int. J. Biol. Sci, doi:10.7150/ijbs.68973
Zhang, None
DOI record:
{
"DOI": "10.3389/fphys.2023.1089637",
"ISSN": [
"1664-042X"
],
"URL": "http://dx.doi.org/10.3389/fphys.2023.1089637",
"abstract": "<jats:p>The protection of physical activity (PA) against COVID-19 is a rising research interest. However, the role of physical activity intensity on this topic is yet unclear. To bridge the gap, we performed a Mendelian randomization (MR) study to verify the causal influence of light and moderate-to-vigorous PA on COVID-19 susceptibility, hospitalization, and severity. The Genome-Wide Association Study (GWAS) dataset of PA (<jats:italic>n</jats:italic> = 88,411) was obtained from the UK biobank and the datasets of COVID-19 susceptibility (<jats:italic>n</jats:italic> = 1,683,768), hospitalization (<jats:italic>n</jats:italic> = 1,887,658), and severity (<jats:italic>n</jats:italic> = 1,161,073) were extracted from the COVID-19 Host Genetics Initiative. A random-effect inverse variance weighted (IVW) model was carried out to estimate the potential causal effects. A Bonferroni correction was used for counteracting. The problem of multiple comparisons. MR-Egger test, MR-PRESSO test, Cochran’s Q statistic, and Leave-One-Out (LOO) were used as sensitive analysis tools. Eventually, we found that light PA significantly reduced the risk of COVID-19 infection (OR = 0.644, 95% CI: 0.480–0.864, <jats:italic>p</jats:italic> = 0.003). Suggestive evidence indicated that light PA reduced the risks of COVID-19 hospitalization (OR = 0.446, 95% CI: 0.227 to 0.879, <jats:italic>p</jats:italic> = 0.020) and severe complications (OR = 0.406, 95% CI: 0.167–0.446, <jats:italic>p</jats:italic> = 0.046). By comparison, the effects of moderate-to-vigorous PA on the three COVID-19 outcomes were all non-significant. Generally, our findings may offer evidence for prescribing personalized prevention and treatment programs. Limited by the available datasets and the quality of evidence, further research is warranted to re-examine the effects of light PA on COVID-19 when new GWAS datasets emerge.</jats:p>",
"alternative-id": [
"10.3389/fphys.2023.1089637"
],
"author": [
{
"affiliation": [],
"family": "Zhang",
"given": "Xing",
"sequence": "first"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Xinyue",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Feng",
"given": "Siyuan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Hansen",
"sequence": "additional"
}
],
"container-title": "Frontiers in Physiology",
"container-title-short": "Front. Physiol.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2023,
3,
8
]
],
"date-time": "2023-03-08T04:49:05Z",
"timestamp": 1678250945000
},
"deposited": {
"date-parts": [
[
2023,
3,
8
]
],
"date-time": "2023-03-08T04:49:09Z",
"timestamp": 1678250949000
},
"indexed": {
"date-parts": [
[
2023,
3,
9
]
],
"date-time": "2023-03-09T05:40:20Z",
"timestamp": 1678340420095
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
3,
8
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
3,
8
]
],
"date-time": "2023-03-08T00:00:00Z",
"timestamp": 1678233600000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fphys.2023.1089637/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2023,
3,
8
]
]
},
"published-online": {
"date-parts": [
[
2023,
3,
8
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1056/NEJMc2100362",
"article-title": "New SARS-CoV-2 variants—Clinical, public health, and vaccine implications",
"author": "Abdool Karim",
"doi-asserted-by": "publisher",
"first-page": "1866",
"journal-title": "N. Engl. J. Med.",
"key": "B1",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1007/s00392-021-01846-7",
"article-title": "Physical activity, sedentary behavior and risk of coronary artery disease, myocardial infarction and ischemic stroke: A two-sample mendelian randomization study",
"author": "Bahls",
"doi-asserted-by": "publisher",
"first-page": "1564",
"journal-title": "Clin. Res. Cardiol.",
"key": "B2",
"volume": "110",
"year": "2021"
},
{
"DOI": "10.1093/ije/dyv080",
"article-title": "Mendelian randomization with invalid instruments: Effect estimation and bias detection through egger regression",
"author": "Bowden",
"doi-asserted-by": "publisher",
"first-page": "512",
"journal-title": "Int. J. Epidemiol.",
"key": "B3",
"volume": "44",
"year": "2015"
},
{
"DOI": "10.1093/ije/dyt179",
"article-title": "Calculating statistical power in Mendelian randomization studies",
"author": "Brion",
"doi-asserted-by": "publisher",
"first-page": "1497",
"journal-title": "Int. J. Epidemiol.",
"key": "B4",
"volume": "42",
"year": "2013"
},
{
"DOI": "10.1007/s10654-017-0255-x",
"article-title": "Interpreting findings from Mendelian randomization using the MR-Egger method",
"author": "Burgess",
"doi-asserted-by": "publisher",
"first-page": "377",
"journal-title": "Eur. J. Epidemiol.",
"key": "B5",
"volume": "32",
"year": "2017"
},
{
"DOI": "10.1097/EDE.0000000000000559",
"article-title": "Sensitivity analyses for robust causal inference from Mendelian randomization analyses with multiple genetic variants",
"author": "Burgess",
"doi-asserted-by": "publisher",
"first-page": "30",
"journal-title": "Epidemiol. Camb. Mass.)",
"key": "B6",
"volume": "28",
"year": "2017"
},
{
"DOI": "10.1186/s12967-022-03407-6",
"article-title": "Causal relationship between physical activity, leisure sedentary behaviors and COVID-19 risk: A mendelian randomization study",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "216",
"journal-title": "J. Transl. Med.",
"key": "B7",
"volume": "20",
"year": "2022"
},
{
"DOI": "10.1111/imm.13443",
"article-title": "New-onset autoimmune phenomena post-COVID-19 vaccination",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "386",
"journal-title": "Immunology",
"key": "B8",
"volume": "165",
"year": "2022"
},
{
"DOI": "10.1038/s41431-020-0636-6",
"article-title": "The COVID-19 Host Genetics Initiative, a global initiative to elucidate the role of host genetic factors in susceptibility and severity of the SARS-CoV-2 virus pandemic",
"doi-asserted-by": "publisher",
"first-page": "715",
"journal-title": "Eur. J. Hum. Genet.",
"key": "B9",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1186/s12967-021-02973-5",
"article-title": "Using genetic variants to evaluate the causal effect of serum vitamin D concentration on COVID-19 susceptibility, severity and hospitalization traits: A mendelian randomization study",
"author": "Cui",
"doi-asserted-by": "publisher",
"first-page": "300",
"journal-title": "J. Transl. Med.",
"key": "B10",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1093/hmg/ddu328",
"article-title": "Mendelian randomization: Genetic anchors for causal inference in epidemiological studies",
"author": "Davey Smith",
"doi-asserted-by": "publisher",
"first-page": "R89",
"journal-title": "Hum. Mol. Genet.",
"key": "B11",
"volume": "23",
"year": "2014"
},
{
"DOI": "10.1136/bmj.k601",
"article-title": "Reading mendelian randomisation studies: A guide, glossary, and checklist for clinicians",
"author": "Davies",
"doi-asserted-by": "publisher",
"first-page": "k601",
"journal-title": "Bmj",
"key": "B12",
"volume": "362",
"year": "2018"
},
{
"DOI": "10.1038/s41590-021-01091-0",
"article-title": "Innate immunity: The first line of defense against SARS-CoV-2",
"author": "Diamond",
"doi-asserted-by": "publisher",
"first-page": "165",
"journal-title": "Nat. Immunol.",
"key": "B13",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1016/S0140-6736(21)00869-2",
"article-title": "Ten scientific reasons in support of airborne transmission of SARS-CoV-2",
"author": "Greenhalgh",
"doi-asserted-by": "publisher",
"first-page": "1603",
"journal-title": "lancet",
"key": "B14",
"volume": "397",
"year": "2021"
},
{
"DOI": "10.1016/j.bbi.2020.05.059",
"article-title": "Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK",
"author": "Hamer",
"doi-asserted-by": "publisher",
"first-page": "184",
"journal-title": "Brain, Behav. Immun.",
"key": "B15",
"volume": "87",
"year": "2020"
},
{
"DOI": "10.1093/hmg/ddy163",
"article-title": "Evaluating the potential role of pleiotropy in Mendelian randomization studies",
"author": "Hemani",
"doi-asserted-by": "publisher",
"first-page": "R208",
"journal-title": "Hum. Mol. Genet.",
"key": "B16",
"volume": "27",
"year": "2018"
},
{
"DOI": "10.12965/jer.2040712.356",
"article-title": "Physical exercise for strengthening innate immunity during COVID-19 pandemic: 4th series of scientific evidence",
"author": "Jee",
"doi-asserted-by": "publisher",
"first-page": "383",
"journal-title": "J. Exerc. rehabilitation",
"key": "B17",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.1038/jhg.2016.72",
"article-title": "Empirical estimation of genome-wide significance thresholds based on the 1000 Genomes Project data set",
"author": "Kanai",
"doi-asserted-by": "publisher",
"first-page": "861",
"journal-title": "J. Hum. Genet.",
"key": "B18",
"volume": "61",
"year": "2016"
},
{
"DOI": "10.1093/eurheartj/ehz388",
"article-title": "Body mass index and body composition in relation to 14 cardiovascular conditions in UK biobank: A mendelian randomization study",
"author": "Larsson",
"doi-asserted-by": "publisher",
"first-page": "221",
"journal-title": "Eur. heart J.",
"key": "B19",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1371/journal.pmed.1003553",
"article-title": "Cardiometabolic risk factors for COVID-19 susceptibility and severity: A mendelian randomization analysis",
"author": "Leong",
"doi-asserted-by": "publisher",
"first-page": "e1003553",
"journal-title": "PLoS Med.",
"key": "B20",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1002/cam4.5204/cam4.5204",
"article-title": "Impairment of kidney function and kidney cancer: A bidirectional mendelian randomization study",
"author": "Lin",
"doi-asserted-by": "publisher",
"first-page": "3610",
"journal-title": "Cancer Med.",
"key": "B21",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.3389/fgene.2021.653032",
"article-title": "A Mendelian Randomization Study of plasma homocysteine levels and cerebrovascular and neurodegenerative diseases",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "653032",
"journal-title": "Front. Genet.",
"key": "B22",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1097/00005768-200208000-00003",
"article-title": "Moderate to vigorous physical activity and risk of upper-respiratory tract infection",
"author": "Matthews",
"doi-asserted-by": "publisher",
"first-page": "1242",
"journal-title": "Med. Sci. sports Exerc.",
"key": "B23",
"volume": "34",
"year": "2002"
},
{
"DOI": "10.1249/00005768-199402000-00002",
"article-title": "Exercise, upper respiratory tract infection, and the immune system",
"author": "Nieman",
"doi-asserted-by": "publisher",
"first-page": "128",
"journal-title": "Med. Sci. sports Exerc.",
"key": "B24",
"volume": "26",
"year": "1994"
},
{
"DOI": "10.1007/s00421-020-04484-5",
"article-title": "Molecular mechanisms involved in the positive effects of physical activity on coping with COVID-19",
"author": "Nigro",
"doi-asserted-by": "publisher",
"first-page": "2569",
"journal-title": "Eur. J. Appl. Physiology",
"key": "B25",
"volume": "120",
"year": "2020"
},
{
"DOI": "10.1002/ijc.33246",
"article-title": "Genetically predicted circulating concentrations of micronutrients and risk of breast cancer: A mendelian randomization study",
"author": "Papadimitriou",
"doi-asserted-by": "publisher",
"first-page": "646",
"journal-title": "Int. J. cancer",
"key": "B26",
"volume": "148",
"year": "2021"
},
{
"DOI": "10.1002/gepi.22441",
"article-title": "Genome‐wide association studies of 27 accelerometry‐derived physical activity measurements identified novel loci and genetic mechanisms",
"author": "Qi",
"doi-asserted-by": "publisher",
"first-page": "122",
"journal-title": "Genet. Epidemiol.",
"key": "B27",
"volume": "46",
"year": "2022"
},
{
"DOI": "10.1002/hep.32534",
"article-title": "Relationship between nafld and coronary artery disease: A mendelian randomization study",
"author": "Ren",
"doi-asserted-by": "publisher",
"first-page": "230",
"journal-title": "Hepatology",
"key": "B28",
"volume": "77",
"year": "2022"
},
{
"DOI": "10.1001/jama.2009.1144",
"article-title": "Physical activity, diet, and risk of Alzheimer disease",
"author": "Scarmeas",
"doi-asserted-by": "publisher",
"first-page": "627",
"journal-title": "Jama",
"key": "B29",
"volume": "302",
"year": "2009"
},
{
"DOI": "10.1681/ASN.2016010098",
"article-title": "Mendelian randomization as an approach to assess causality using observational data",
"author": "Sekula",
"doi-asserted-by": "publisher",
"first-page": "3253",
"journal-title": "J. Am. Soc. Nephrol.",
"key": "B30",
"volume": "27",
"year": "2016"
},
{
"DOI": "10.1016/S1473-3099(21)00648-4",
"article-title": "Community transmission and viral load kinetics of the SARS-CoV-2 delta (B. 1.617. 2) variant in vaccinated and unvaccinated individuals in the UK: A prospective, longitudinal, cohort study",
"author": "Singanayagam",
"doi-asserted-by": "publisher",
"first-page": "183",
"journal-title": "Lancet Infect. Dis.",
"key": "B31",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1136/bjsports-2021-105159",
"article-title": "Small steps, strong shield: Directly measured, moderate physical activity in 65 361 adults is associated with significant protective effects from severe COVID-19 outcomes",
"author": "Steenkamp",
"doi-asserted-by": "publisher",
"first-page": "568",
"journal-title": "Br. J. SPORTS Med.",
"key": "B32",
"volume": "56",
"year": "2022"
},
{
"DOI": "10.1038/s41588-018-0099-7",
"article-title": "Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases",
"author": "Verbanck",
"doi-asserted-by": "publisher",
"first-page": "693",
"journal-title": "Nat. Genet.",
"key": "B33",
"volume": "50",
"year": "2018"
},
{
"DOI": "10.2165/00007256-200131020-00003",
"article-title": "Physical activity in the prevention of cardiovascular disease: An epidemiological perspective",
"author": "Wannamethee",
"doi-asserted-by": "publisher",
"first-page": "101",
"journal-title": "SPORTS Med.",
"key": "B34",
"volume": "31",
"year": "2001"
},
{
"DOI": "10.1016/j.envres.2016.07.012",
"article-title": "Assessing the impact of fine particulate matter (PM2.5) on respiratory-cardiovascular chronic diseases in the New York City Metropolitan area using Hierarchical Bayesian Model estimates",
"author": "Weber",
"doi-asserted-by": "publisher",
"first-page": "399",
"journal-title": "Environ. Res.",
"key": "B35",
"volume": "151",
"year": "2016"
},
{
"DOI": "10.1016/j.smhs.2020.05.006",
"article-title": "The COVID-19 pandemic and physical activity",
"author": "Woods",
"doi-asserted-by": "publisher",
"first-page": "55",
"journal-title": "Sports Med. Health Sci.",
"key": "B36",
"volume": "2",
"year": "2020"
},
{
"article-title": "Association of smoking, lung function and COPD in COVID-19 risk: A two-step mendelian randomization study",
"author": "Yeung",
"journal-title": "Addiction",
"key": "B37",
"year": "2022"
},
{
"DOI": "10.1002/art.42239",
"article-title": "Genetic liability to rheumatoid arthritis in relation to coronary artery disease and stroke risk",
"author": "Yuan",
"doi-asserted-by": "publisher",
"first-page": "1638",
"journal-title": "Arthritis and Rheumatology",
"key": "B38",
"volume": "74",
"year": "2022"
},
{
"DOI": "10.1016/j.clim.2020.108427",
"article-title": "COVID-19 pathophysiology: A review",
"author": "Yuki",
"doi-asserted-by": "publisher",
"first-page": "108427",
"journal-title": "Clin. Immunol.",
"key": "B39",
"volume": "215",
"year": "2020"
},
{
"DOI": "10.7189/jogh.10.020514",
"article-title": "Physical activity and COVID-19: An observational and mendelian randomisation study",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "020514",
"journal-title": "J. Glob. health",
"key": "B40",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1016/j.heliyon.2022.e09417",
"author": "Zhang",
"doi-asserted-by": "crossref",
"key": "B41",
"volume-title": "Can sports cartoon watching in childhood promote adult physical activity and mental health? A pathway analysis in Chinese adults",
"year": ""
},
{
"DOI": "10.3390/ijerph19095142",
"article-title": "Using structural equation modeling to examine pathways between physical activity and sleep quality among Chinese TikTok users",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "5142",
"journal-title": "Int. J. Environ. Res. Public Health",
"key": "B42",
"volume": "19",
"year": ""
},
{
"DOI": "10.7150/ijbs.68973",
"article-title": "A systematic review of vaccine breakthrough infections by SARS-CoV-2 delta variant",
"author": "Zhang M.",
"doi-asserted-by": "publisher",
"first-page": "889",
"journal-title": "Int. J. Biol. Sci.",
"key": "B43",
"volume": "18",
"year": "2022"
}
],
"reference-count": 43,
"references-count": 43,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fphys.2023.1089637/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Physiology (medical)",
"Physiology"
],
"subtitle": [],
"title": "The causal effect of physical activity intensity on COVID-19 susceptibility, hospitalization, and severity: Evidence from a mendelian randomization study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "14"
}
