Effects of high dose vitamin c on patient outcomes in ARDS patients admitted to intensive care with COVID-19; multi-center retrospective study
et al., Intensive Care Medicine Experimental, 9:S1, 001458, doi:10.1186/s40635-021-00413-8, Sep 2020
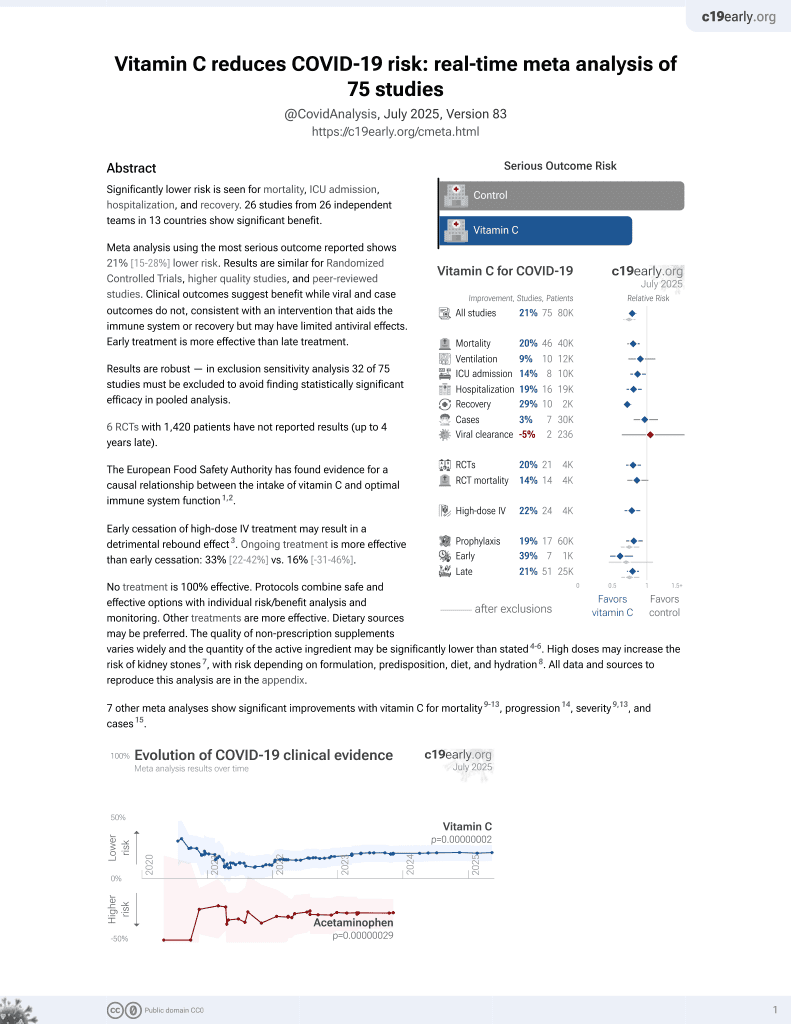
Vitamin C for COVID-19
6th treatment shown to reduce risk in
September 2020, now with p = 0.000000068 from 74 studies, recognized in 22 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
PSM retrospective 86 ICU patients on mechanical ventilation in Turkey, showing lower mortality with high-dose vitamin C treatment (≥200mg/kg for 4 days).
This is the 3rd of 74 COVID-19 controlled studies for vitamin C, which collectively show efficacy with p=0.000000068.
21 studies are RCTs, which show efficacy with p=0.0012.
This study is excluded in the after exclusion results of meta-analysis:
very late stage, ICU patients.
|
risk of death, 18.8% lower, RR 0.81, p = 0.04, treatment 31 of 42 (73.8%), control 40 of 44 (90.9%), NNT 5.8, propensity score matching.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Yüksel et al., 20 Sep 2020, retrospective, Turkey, preprint, 13 authors, dosage 200mg/kg days 1-4.
ESICM LIVES 2021: Part 1
Intensive Care Medicine Experimental, doi:10.1186/s40635-021-00413-8
Introduction. The optimal integration between adequate protein intake and exercise in critically ill patients may have an impact on short and long-term outcomes, but this hypothesis has not been tested in studies with good methodology. In the given context, we conducted a prospective randomized controlled trial to evaluate the efficacy of high protein intake and early exercise versus guidelines recommended protein intake and routine physiotherapy on outcome of critically ill patients. Methods. We randomized mechanically ventilated patients expected to stay in the intensive care unit (ICU) for at least 4 days. We used indirect calorimetry to determine energy expenditure and guide caloric provision to the patients randomized to the high protein and early exercise (HPE) group and the control group. Protein intakes were 2.0 g/ kg/day and 1.4 g/kg/day respectively; while the former was submitted to two daily sessions of cycle ergometry exercise, the latter received routine physiotherapy. We evaluated the primary outcome physical component summary (PCS) score at 3 and 6 months) and the secondary outcomes (handgrip strength at ICU discharge and ICU and hospital mortality). Results. We analyzed 181 patients in the HPE (87) and control (94) group. There was no significant difference between groups in relation to the calories received. However, the amount of protein received by the HPE group was significantly higher than that received by the control group (p < 0.0001). The PCS score was significantly higher in the HPE group at 3 months (p = 0.01) and 6 months (p = 0.01). The hospital mortality was expressively higher in the control group (p = 0.006). We found an independent association between age and 3-month PCS and that between age and group and 6-month PCS.
Conclusion. This study showed that a high-protein intake and resistive exercise increase the survival rate and the physical quality of life of critically ill patients.
Conflict of interest: FILMARRAY ® Pneumonia Plus Panels and QC-material was sponsored by BioMérieux SA along with cost of shipment. All agreements have been revised and approved by the Unit for Research an Innovation, The Capital Region of Denmark.
Determination of Serum Zinc and Copper Levels and Their Relation with Mortality in Critically Ill Patients M. Yildirim, 1 ; B. Kesikli, 2 ; L. Talan, 3 ; MA. Tekes, 4 ; N. Yazıhan, 2 ; ND. Altintas 3 000320 The effect of high flow oxygen via tracheostomy on diaphragm function in patients with prolonged weaning from mechanical ventilation: a randomized crossover study E. Lytra 1 ; I. Poularas 2 ; D. Cokkinos 1 ; Y. Papachatzakis 2 ; V. Vlachakos 2 ; P. Ampatzis 1 ; D. Exarchos 1 ; D. Filippiadis 3 ; S. Zakynthinos 2 ; C. Routsi 2 1 Department of radiology, Evangelismos Hospital, Athens, Greece; ICMx 2021, 9(Suppl 1):51 Results. 65 patients were included. 90-day mortality in this series was 30.8% (n = 20). Table 1 shows the variables that proved statistically significant impact on 90-day mortality in this subset of patients.
Variables
Conclusion. This study brings perspective on how clinical evolution during ICU stay of the patients who underwent mechanical ventilation due to severe COVID-19 predicts 90-day mortality. In fact, a higher SAPS II score and aaCCI significantly decrease the odds of being alive 90 days after ICU admission. Higher PaO2/FiO2 ratios thoughout days 2 to 5 of IMV significantly increase the odds of a..
References
Acheampong, Vincent, A positive fluid balance is an independent prognostic factor in patients with sepsis, Critical Care
Acker, Bakker 8 ; B. Abella 2 1 Departments of emergency medicine, anesthesiology & critical care, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, United States of America; 2 Department of emergency medicine, Perelman School of Medicine at the University of Pennsylvania
Acosta, Cabrera, Necrotizing tracheobronchitis with endotracheal tube obstruction in COVID-19 patients, Rev Clin Esp, doi:10.1016/j.rce.2020.05.002
Acosta, Cabrera, Necrotizing tracheobronchitis with endotracheal tube obstruction in COVID-19 patients, Rev Clin Esp, doi:10.1016/j.rce.2020.05.002
Agerstrand, Schellongowski 8 ; G. Vojka 9 ; T. Duburcq 10 ; AA. Hssain 11 ; V. Fanelli 12 ; F. Tuzzolino 13 ; M
Alhazzani, Evans, Alshamsi, Møller, Ostermann et al., Surviving Sepsis Campaign Guidelines on the Management of Adults With Coronavirus Disease 2019 (COVID-19) in the ICU: First Update, Critical Care Medicine
Alonso 1 ;, Silva, Obregón 1 ; C. Marian Crespo 1 1 Intensive care, Hospital Universitario de Guadalajara, Calle Donante de Sangre
Altznauer, Inflammation-associated cell cycle-independent block of apoptosis by survivin in terminally differentiated neutrophils, J. Exp. Med
Amato, Meade, Slutsky, Brochard, Driving pressure and survival in the acute respiratory distress syndrome, New England Journal Medicine
Amcgrath, Wallace, Bonvento, Lynch, Coe, Dougal Atksinon; Executive Summary Key Standards and recommendations
Amrein, Schnedl, Holl, Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial, JAMA
Andersen, Geskus, De Witte, Putter, Competing risks in epidemiology: possibilities and pitfalls, Int J Epidemiol
Andrews, Shiber, Jaruga-Killeen, Roy, Sadowitz et al., Early application of airway pressure release ventilation may reduce mortality in high-risk trauma patients: a systematic review of observational trauma ARDS literature, Journal of Trauma and Acute Care Surgery
Andrikopoulou, Symptoms and Critical Illness Among Obstetric Patients With Coronavirus Disease 2019 (COVID-19) Infection, Obstet Gynecol
Anesthesiology, Hôpitaux Universitaires de Genève (HUG)
Appelros, Stegmayr, Terént, Sex Differences in Stroke Epidemiology, Stroke
Arabi, Azoulay, Al-Dorzi, Phua, Salluh et al., How the COVID-19 pandemic will change the future of critical care, Intensive Care Med, doi:10.1007/s00134-021-06352-y
Arentz, Yim, Klaff, Lokhandwala, Riedo et al., Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State, JAMA, doi:10.1001/jama.2020.4326
Arentz, Yim, Klaff, Lokhandwala, Riedo et al., Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State, JAMA, doi:10.1001/jama.2020.4326
Armstrong, Kane, Cook, Outcomes from intensive care in patients with COVID-19: a systematic review and meta-analysis of observational studies, Anaesthesia
Armstrong, Kane, Cook, Outcomes from intensive care in patients with COVID-19: a systematic review and meta-analysis of observational studies, Anaesthesia
Armstrong, Kane, Kursumovic, Oglesby, Cook, Mortality in patients admitted to intensive care with COVID-19: an updated systematic review and meta-analysis of observational studies, Anaesthesia, doi:10.1111/anae.15425
Armstrong, Kane, Kursumovic, Oglesby, Cook, Mortality in patients admitted to intensive care with COVID-19: an updated systematic review and meta-analysis of observational studies, Anaesthesia, doi:10.1111/anae.15425
Aronson, Meyler's Side Effects of Drugs: The International Encyclopedia of Adverse Drug Reactions and Interactions (6 Volume Set
Ashbaugh, Bigelow, Petty, Acute respiratory distress in adults, Lancet
Aubier, Effects of Digoxin on Diaphragmatic Strength Generation in Patients with Chronic Obstructive Pulmonary Disease During Acute Respiratory Failure, Am Rev Resp Dis
Aziz, Managing ICU surge during the COVID-19 crisis: Rapid Guidelines, Intensive Care Med
Azoulay, Vincent, Herridge, Recovery after critical illness: putting the puzzle togheter-a consensus of 29, Crit Care
Bachmann, Morais, Bugedo, Bruhn, Morales et al., Electrical Impedance Tomography in Acute Respiratory Distress Syndrome, Crit. Care. Critical Care
Bagshaw, Uchino, Bellomo, Septic acute kidney injury in critically ill patients: clinical characteristics and outcomes, CJASN
Bakeer, James, Roy, Sickle cell anemia mice develop a unique cardiomyopathy with restrictive physiology, Proc Natl Acad Sci U S A
Bangalore, Sharma, Slotwiner, ST-Segment Elevation in Patients with Covid-19-A Case Series, N Engl J Med, doi:10.1056/NEJMc2009020
Barbar, Noventa, Rossetto, A risk assessment model for the identification of hospitalized medical patients at risk for venous thromboembolism: the Padua Prediction Score, J Thromb Haemost
Barnes, Enk, Ventilation for low dissipated energy achieved using flow control during both inspiration and expiration, Trends in Anaesthesia and Critical Care
Barret, Lester, Heparin versus saline flushing solutions in a small community hospital, Hosp Pharm
Bartlett, Ogino, Brodie, Initial ELSO Guidance Document: ECMO for COVID-19 patients with severe cardiopulmonary failure, Asaio J
Bass, Fields, Goto, Turissini, Dey et al., Clinical Decision Rules for Pulmonary Embolism in Hospitalized Patients: A Systematic Literature Review and Meta-analysis, Thromb Haemost
Baumstarck, Alessandrini, Hamidou, Auquier, Leroy et al., Assessment of coping: a new french four-factor structure of the brief COPE inventory, Health Qual Life Outcomes
Beduneau, Pham, Schotgen, Epidemiology of weaning outcome according to a new definition; The WIND Study, American Journal of Respiratory and Critical Care Medicine
Beigel, Tomashek, Dodd, Mehta, Zingman et al., Remdesivir for the Treatment of Covid-19-Final Report, N Engl J Med
Bellani, Epidemiology, Patterns of Care and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries, JAMA
Bellani, Grasselli, Cecconi, Antolini, Borelli et al., 2021 Reference(s) a. Timing of Tracheostomy for Patients With COVID-19 in the ICU-Setting Precedent in Unprecedented Times: JAMA Otolaryngology-Head & Neck Surgery October
Bellani, Laffey, Pham, Brochard, Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Reference(s)
Bellani, Laffey, Pham, Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries, JAMA
Bellani, Laffey, Pham, Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries, JAMA
Beltrami, Nguyen, Pichereau, Fleury, Fagondes, Sleep in the intensive care unit, J Bras Pneumol, doi:10.1590/S1806-37562015000000056
Berger, Appelberg, Reintam-Blaser, Prevalence of hypophosphatemia in the ICU-Results of an international one-day point prevalence survey, Clin Nutr Edinb Scotl. Published online December, doi:10.1016/j.clnu.2020.12.017
Bergman, Basu, Lei, Niezgoda, Zhuang, Development of a Manikin-Based Performance Evaluation Method for Loose-Fitting Powered Air-Purifying Respirators, J Int Soc Respir Prot
Berlin, Gulick, Martinez, Severe Covid-19, New England Journal of Medicine
Bertaina, Nuñez-Gil, Franchin, HOPE COVID-19 investigators. Non-invasive ventilation for SARS-CoV-2 acute respiratory failure: a subanalysis from the HOPE COVID-19 registry, Emerg Med J
Bhatraju, Ghassemieh, Nichols, Kim, Jerome et al., Covid-19 in Critically Ill Patients in the Seattle Region-Case Series, N Engl J Med, doi:10.1056/NEJMoa2004500
Bilaloglu, Aphinyanaphongs, Jones, Iturrate, Hochman et al., Thrombosis in Hospitalized Patients With COVID-19 in a New York City Health System, JAMA, doi:10.1001/jama.2020.13372
Bonnet, Martin, Boubaya, High flow nasal oxygen therapy to avoid invasive mechanical ventilation in SARS-CoV-2 pneumonia: a retrospective study, Ann. Intensive Care, doi:10.1186/s13613-021-00825-5
Borgi, Tsiouris, Hodari, Cogan, Paone et al., Significance of postoperative acute renal failure after continuous-flow left ventricular assist device implantation, Ann Thorac Surg
Boston, None
Bouadma, Karpanen, Elliott, Chlorhexidine use in adult patients on ICU, Intensive Care Med, doi:10.1007/s00134-018-5137-5.20
Bourenne, Sedation and neuromuscular agents blocking in acute respiratory syndrome, Ann Transl Med, doi:10.21037/atm.2017.07.19
Boussuges, Md, Phd; Yoann Gole, Blanc, Md, Diaphragmatic Motion Studied byM-Mode Ultrasonography.Methods, Reproducibility, and Normal Values
Boussuges, Rives, Finance, Brégeon, Assessment of diaphragmatic function by ultrasonography: Current approach and perspectives, World J Clin Cases
Bower, Matthay, Morris, Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome, New England Journal Medicine
Brahier, Meuwly, Pantet, Vez, Donnet et al., Lung ultrasonography for risk stratification in patients with COVID-19: a prospective observational cohort study, Clin Infect Dis, doi:10.1093/cid/ciaa1408
Branson, Ba, RRT Prone Positioning and Inhaled Nitric Oxide: Synergistic Therapies for Acute Respiratory Distress Syndrome, The Journal of Trauma: Injury, Infection, and Critical Care
Bravata, Perkins, Myers, Association of Intensive Care Unit Patient Load and Demand With Mortality Rates in US Department of Veterans Affairs Hospitals During the COVID-19 Pandemic, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.34266
Brenner, Gupta, ABO phenotype and death in critically ill patients with COVID-19, Br J Haematol
Brindle, Saharinen, Alitalo, Signaling and functions of angiopoietin-1 in vascular protection, Circ Res
Brivio, None, L. Grazioli
Broccard, Shapiro, Schmitz, Adams, Marini, Prone positioning attenuates and redistributes ventilator-induced lung injury in dogs, Crit. Care Med
Brochard, Slutsky, Pesenti, 001020 Differences in the emotional state in COVID-19 and non-COVID-19 ICU survivors at early phases of the post-ICU recovery N, Am J Respir Crit Care Med
Brochner-Mortensen, A simple method for the determination of glomerular filtration rate, Scand J Clin Lab Invest
Brodie, None, J. Fraser
Broman, Holzgraefe, Palmer, The Stockholm experience: interhospital transports on extracorporeal membrane oxygenation, Crit Care
Brun-Buisson, Minelli, Bertolini, Epidemiology and outcome of acute lung injury in European intensive care units. Results from the ALIVE study, Intensive Care Med
Bräunlich, Incidence and outcome of barotrauma in patients with coronavirus disease 2019 (COVID-19) on invasive mechanical ventilation E. Abril Palomares 1 ; A. Pavalascu 1 ; ÁL. Córdoba Sánchez 1 ; Á. Algaba Calderón 1, International Journal of Chronic Obstructive Pulmonary Disease, doi:10.2147/COPD.S104616
Burkert, Niederreiter, Dichtl, Case report of a COVID-19-associated myocardial infarction with no obstructive coronary arteries: the mystery of the phantom embolus or local endothelitis, Eur Heart J Case Rep, doi:10.1093/ehjcr/ytaa521
Burki, Mani, Herth, Schmidt, Teschler et al., A novel extracorporeal CO(2) removal system: Results of a pilot study of hypercapnic respiratory failure in patients with COPD, Chest
Calligaro, Lalla, Audley, Gina, Miller et al., The utility of high-flow nasal oxygen for severe COVID-19 pneumonia in a resource-constrained setting: A multi-centre prospective observational study, The Lancet
Camprubí-Rimblas, Tantinyà, Guillamat-Prats, Bringué, Puig et al., Effects of nebulized antithrombin and heparin on inflammatory and coagulation alterations in an acute lung injury model in rats, J Thromb Haemost, doi:10.1111/jth.14685
Canadian, A Cross Sectional Analysis of Intensive Care Unit Patient and Caregiver Needs P. Gregoire 1 ; E. Balcom, 2 ; M. Douma, 1 ; V. Lau, 1 ; P. Brindley 1 1 Critical Care Medicine
Candeias, None, JM. Ribeiro, 1 ; SM. Fernandes
Cantón-Bulnes, Garnacho-Montero, Antisepsia orofaríngea en el paciente crítico y en el paciente sometido a ventilación mecánica, Med Intensiva, doi:10.1016/j.medin.2018.06.011.52
Cao, Yu, Chai, Pathological alteration and therapeutic implications of sepsis-induced immune cell apoptosis, Cell Death Dis
Caravita, Baratto, Marco, Calabrese, Balestrieri et al., Haemodynamic characteristics of COVID-19 patients with acute respiratory distress syndrome requiring mechanical ventilation. An invasive assessment using right heart catheterization, Europ J Heart Fail
Cardiology, Düsseldorf, Düsseldorf, Germany, Department of intensive care, Medical intensive care unit
Care, Doce De Octubre, Madrid, Intensive care, Hospital Doce de Octubre, Madrid, Spain Correspondence: A. Marcos-Morales Intensive Care Medicine Experimental
Carrera-Hernández, Aizpitarte-Pejenaute, Zugazagoitia-Ciarrusta, Viguria, Percepción del sueño de los pacientes en una Unidad de Cuidados Intensivos, Enferm Intensiva
Carron, Complications of Non-Invasive Ventilation Techniques: A Comprehensive Qualitative Review of Randomized Trials, British Journal of Anaesthesia, doi:10.1093/bja/aet070
Carsana, Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-centre descriptive study, Lancet Infect Dis
Carsana, Sonzogni, Nasr, Rossi, Pellegrinelli et al., Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-centre descriptive study, Lancet Infect Dis, doi:10.1016/S1473-3099(20)30434-5
Carsetti, Paciarini, Marini, Pantanetti, Adrario et al., Prolonged prone position ventilation for SARS-CoV-2 patients is feasible and effective, Critical Care. 15 de mayo de
Carver, You want to measure coping but your protocol's too long: Consider the Brief COPE, Int J Behav Med
Casas-Rojo, Antón-Santos, Millán-Núñez-Cortés, Lumbreras-Bermejo, Ramos-Rincón et al., Clinical characteristics of patients hospitalized with COVID-19 in Spain: results from the SEMI-COVID-19 Registry, Revista Clínica Española
Cattelan, Castellano, Merdji, Audusseau, Feuillassier, Psychological effects of remote-only communication among Reference persons of ICU patients during COVID-19 pandemic, J intensive care
Cecconi, Evans, Levy, Rhodes, Sepsis and septic shock, The Lancet
Ceruti, Saporito, Glotta 4 ; P. Maida, 5 ; C. Garzoni, 5 1 Department of critical care, Clinica Luganese Moncucco
Chandel, Patolia, Brown, Collins, Sahjwani et al., High-flow nasal cannula in COVID-19: Outcomes of application and examination of the ROX index to predict success, Respiratory Care
Chen, Chen, Wei, Li, Zhang et al., The effect of serum neutrophil gelatinase-associated lipocalin on the discontinuation of continuous renal replacement therapy in critically ill patients with acute kidney injury, Blood Purification, doi:10.1159/000499026
Chen, Dubrawski, Clermont, Hravnak, Pinsky, Modelling Risk of Cardio-Respiratory Instability as a Heterogeneous Process
Chen, Dubrawski, Hravnak, Clermont, Pinsky, Forecasting cardio-respiratory instability in monitored patients: a machine learning approach, Crit Care Med
Chen, Janz, Shaver, Bernard, Bastarache et al., Clinical Characteristics and Outcomes Are Similar in ARDS Diagnosed by Oxygen Saturation/Fio2 Ratio Compared With Pao2/Fio2 Ratio, Chest. Dec, doi:10.1378/chest.15-0169
Chen, Lu, Yi, Chen, Chest Compression With Personal Protective Equipment During Cardiopulmonary Resuscitation: A Randomized Crossover Simulation Study, Medicine
Chen, None
Chen, Ogundele, Clermont, Hravnak, Pinsky et al., Dynamic and Personalized Risk Forecast in Step-Down Units. Implications for Monitoring Paradigms, Annals
Chen, Zhang, Zhu, Liu, Yan et al., Clinical characteristics and treatment of critically ill patients with COVID-19 in Hebei, Ann Palliat Med
Chocron, Loeb, Lamhaut, Jost, Adnet et al., Ambulance Density and Outcomes After Out-of-Hospital Cardiac Arrest, Circulation, doi:10.1161/CIRCULATIONAHA.118.035113
Choi, Lee, Lee, Serum neutrophil gelatinase-associated lipocalin at 3 h after return of spontaneous circulation in patients with cardiac arrest and therapeutic hypothermia: early predictor of acute kidney injury, BMC Nephrol, doi:10.1186/s12882-020-02054-7
Cis, Saint-Étienne, None
Cis, St-Priest-En-Jarez, France, None
Clarke, Curtis, Luce, Levy, Danis et al., Robert Wood Johnson Foundation Critical Care End-Of-Life Peer Workgroup Members. Quality indicators for end-of-life care in the intensive care unit, Crit Care Med, doi:10.1097/01.CCM.0000084849.96385.85
Clement, Hetzer, None, AJ. Fritschi 3 ; M. Renes, 1 ; J. Droogh
Clerkin, Fried, Raikhelkar, Sayer, Griffin et al., COVID-19 and Cardiovascular Disease. Circulation, doi:10.1161/CIRCULATIONAHA.120.046941
Clover, London trust with most covid-19 deaths: We serve a vulnerable population, Health Service Journal
Cohen, Kogan, Sahar, Lev, Vidne et al., Hypophosphatemia following open heart surgery: incidence and consequences, Eur J Cardiothorac Surg, doi:10.1016/j.ejcts.2004.03.004
Combes, Hajage, Capellier, Demoule, Lavoue et al., Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome, N Engl J Med, doi:10.1056/NEJMoa1800385
Commereuc, Guérot, Charles-Nelson, ICU Patients Requiring Renal Replacement Therapy Initiation: Fewer Survivors and More Dialysis Dependents From 80 Years Old, Crit Care Med, doi:10.1097/CCM.0000000000002407
Contou, Fraissé, Pajot, Tirolien, Mentec et al., Comparison between first and second wave among critically ill COVID-19 patients admitted to a French ICU: no prognostic improvement during the second wave?, Crit Care, doi:10.1186/s13054-020-03449-6
Cook, El-Boghdadly, Mcguire, Mcnarry, Patel et al., Consensus guidelines for managing the airway in patients with COVID-19: Guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists
Coppo, Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study, Lancet Respir Med
Corona, Richini 1 ; M. Pasqua 1 ; C. Santorsola 1 ; I. Gatti 1 ; A. Capone 1
Couper, Yeung, Soar, Berg, Andersen et al., Prophylactic antibiotics following return of spontaneous circulation in adults: Consensus on Science with Treatment Recommendations
Courcelle, Gaudry, Serck, Blonz, Lascarrou et al., Neuromuscular blocking agents (NMBA) for COVID-19 acute respiratory distress syndrome: a multicenter observational study, Crit Care
Courcelle, Neuromuscular blocking agents (NMBA) for COVID-19 acute respiratory distress syndrome: a multicenter observational study, Crit Care, doi:10.1186/s13054-020-03164-2
Cournoyer, Grand'maison, Lonergan, Lessard, Chauny et al., Oxygen Therapy and Risk of Infection for Health Care Workers Caring for Patients With Viral Severe Acute Respiratory Infection: A Systematic Review and Meta-analysis, Ann Emerg Med, doi:10.1016/j.annemergmed.2020.06.037
Covid-19, Artificial intelligence-based prevention. Illustrious College of Physicians Las palmas de Gran Canaria
Covid-19, Artificial intelligence-based prevention. Illustrious College of Physicians Las palmas de Gran Canaria 000376 Clinical-histopathologic correlation of severe pulmonary SARS-CoV-2 infection
Covid-19, Artificial intelligence-based prevention. Illustrious College of Physicians Las palmas de Gran Canaria Reference(s)
Cressoni, Cadringher, Chiurazzi, Amini, Gallazzi et al., Lung inhomogeneity in patients with acute respiratory distress syndrome, Am. J. Respir. Crit. Care Med
Critical, Center, Estadual Getulio, Vargas, Janeiro et al., Hospital Getúlio Vargas, Rio de Janeiro, Brazil Correspondence: S. Oliveira Intensive Care Medicine Experimental
Cucinotta, Vanelli, WHO Declares COVID-19 a Pandemic, doi:10.23750/abm.v91i1.9397
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
Cutuli, Artigas, Fumagalli, Monti, Ranieri et al., Polymyxin-B hemoperfusion in septic patients: analysis of a multicenter registry, Ann Intensive Care, doi:10.1186/s13613-016-0178-9
D'elia, Caselli, Kosmala, Normal Global Longitudinal Strain: An Individual Patient Meta-Analysis, JACC Cardiovasc Imaging
Dagens, Sigfrid, Cai, Scope, quality, and inclusivity of clinical guidelines produced early in the covid-19 pandemic: rapid review, BMJ
Dale, Starcher, Chang, Surge effects and survival to hospital discharge in critical care patients with COVID-19 during the early pandemic: a cohort study, Crit Care, doi:10.1186/s13054-021-03504-w
Dalfino, None, Interact. Cardiovasc. Thorac. Surg
Daltrozzo, Predicting coma and other low responsive patients outcome using event-related brain potentials: A meta-analysis, Clinical Neurophysiology
Dauner, Dauner, Summary of adverse drug events for hydroxychloroquine, azithromycin, and chloroquine during the COVID-19 pandemic, J Am Pharm Assoc
Davies, Jarvis, CMMID COVID-19 Working Group. et al. Increased mortality in community-tested cases of SARS-CoV-2 lineage B.1.1.7, Nature, doi:10.1038/s41586-021-03426-1
De Felice, Tovar-Moll, Moll, Munoz, Ferreira, Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and the Central Nervous System, Trends Neurosci, doi:10.1016/j.tins.2020.04.004
De Lassence, Timsit, Tafflet, Pneumothorax in the Intensive Care Unit Incidence, Risk Factors, and Outcome, Anesthesiology, doi:10.1097/00000542-200601000-00003
Deitch, Livingston, Lavery, Monaghan, Bongu et al., Hormonally active women tolerate shock-trauma better than do men: a prospective study of over 4000 trauma patients, Ann Surg
Dellinger, Levy, Carlet, Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2008, Intensive Care Med, doi:10.1007/s00134-007-0934-2
Demoule, Baron, Darmon, Beurton, Géri et al., High-Flow Nasal Cannula in Critically Ill Patients with Severe COVID-19, American Journal of Respiratory and Critical Care Medicine
Department, Fondazione, Ca, Ospedale, Policlinico, Intensive care medicine
Descalzo, Acute eosinophilic pneumonia associated with SARS-CoV2 Infection, Arch Bronconeumol
Deschepper, Waegeman, Eeckloo, Vogelaers, Blot, Effects of chlorhexidine gluconate oral care on hospital mortality: a hospital-wide, observational cohort study, Intensive Care Med, doi:10.1007/s00134-018-5171-3
Diddle, Almodovar, Rajagopal, Rycus, Thiagarajan, Extracorporeal membrane oxygenation for the support of adults with acute myocarditis, Crit Care Med
Disease, Godinne, None
Donato, Analytical performance of an immunoassay to measure proenkephalin, Clin Biochem
Donchin, Seagull, The hostile environment of the intensive care unit, Curr Opin Crit Care
Donoghue, Kou, Good, Eiger, Nash et al., Best Pharmaceuticals for Children Act-Pediatric Trials Network. Impact of Personal Protective Equipment on Pediatric Cardiopulmonary Resuscitation Performance: A Controlled Trial, Pediatr Emerg Care
Dr, Schepens is supported by a grant from Research Foundation-Flanders
Ebner, Moseby-Knappe, Mattsson-Carlgren, Serum GFAP and UCH-L1 for the prediction of neurological outcome in comatose cardiac arrest patients, Resuscitation
Egawa, Hifumi, Kawakita, Okauchi, Shindo et al., Impact of neurointensivist-managed intensive care unit implementation on patient outcomes after aneurysmal subarachnoid hemorrhage, Journal of critical care, doi:10.1016/j.jcrc.2015.11.008
Eggins, Slade, Communication in clinical handover: improving the safety and quality of the patient experience, Journal of Public Health Research
Eldridge, Ford, Perimortem caesarean deliveries, Int J Obstet Anesth, doi:10.1016/j.ijoa.2016.02.008
Embriaco, Papazian, Kentish-Barnes, Pochard, Azoulay, Burnout syndrome among critical care healthcare workers, Curr Opin Crit Care
England, Delivering Diabetes Care during the COVID-19 Pandemic-the 'new normal
Eren, None
Fayed, Hady, Shaaban, Fikry, Use of ultrasound to assess diaphragmatic thickness as a weaning parameter in invasively ventilated chronic obstructive pulmonary disease patients, J Am Sci
Fergusson, Hébert, Mazer, A comparison of aprotinin and lysine analogues in high-risk cardiac surgery, N Engl J Med, doi:10.1056/NEJMoa0802395
Fernandez, Bassi, Rohrs, Ornowska, Nicholas et al., Temporary Transvenous Diaphragm Neurostimulation Therapy With Mechanical Ventilation Mitigates Atrophy in All Diaphragm Myofiber Types, Chest, doi:10.1016/j.chest.2020.08.1939
Ferrara, Sant, None, J. Montomoli Intensive Care Medicine Experimental
Ferrari, Diaphragm ultrasound as a new index of discontinuation from mechanical ventilation, Critical Ultrasound Journal
Ferreira, Bota, Bross, Melot, Vincent, Serial evaluation of the SOFA score to predict outcome in critically ill patients, JAMA
Fiaccadori, None
Fitzgerald, Millar, Blackwood, Extracorporeal carbon dioxide removal for patients with acute respiratory failure secondary to the acute respiratory distress syndrome: a systematic review, Crit Care
Flaatten, De Lange, Morandi, The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥ 80 years), Intensive Care Med, doi:10.1007/s00134-017-4940-8
Flaatten, The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥ 80 years)
Flaatten, The status of intensive care medicine research and a future agenda for very old patients in the ICU, Intensive Care Med
Fogarty, Tarantino, Brainsky, Selective validation of the WHO Bleeding Scale in patients with chronic immune thrombocytopenia, Curr Med Res Opin
Forsyth, None, J. Laffey
Foti, Giannini, Bottino, Castelli, Cecconi et al., Management of critically ill patients with COVID-19: suggestions and instructions from the coordination of intensive care units of Lombardy, Minerva Anestesiol (Internet)
Francis, Hoffer, Reynolds, Ultrasonographic evaluation of diaphragm thickness during mechanical ventilation in intensive care patient, Am J Crit Care
François, Cariou, Clere-Jehl, Dequin, Renon-Carron et al., Prevention of Early Ventilator-Associated Pneumonia after Cardiac Arrest, N Engl J Med
Frat, Thille, Mercat, Cirault, Ragot et al., High-Flow Oxygen through Nasal Cannula in Acute Hypoxemic Respiratory Failure, The New England Journal of Medicine
Frat, Thille, Mercat, Girault, Ragot et al., FLORALI Study Group; REVA Network. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure, N Engl J Med
Furriols, None
Földi, Farkas, Kiss, Zádori, Váncsa et al., Obesity is a risk factor for developing critical condition in COVID-19 patients: A systematic review and meta-analysis, Obesity Reviews
Gabler, Ratcliffe, Wagner, Asch, Rubenfeld et al., Reducing the burden of bed shortages in COVID-19 pandemic by identifying modifiable risk factors that contribute to a prolonged stay in the Intensive Care Unit D. Pérez-Torres 1, JÁ. Berezo-García 1 ; C. Cuenca-Rubio, doi:10.1164/rccm.201304-0622OC
Ganatra, Hammond, Nohria, The Novel Coronavirus Disease (COVID-19) Threat for Patients With Cardiovascular Disease and Cancer, JACC CardioOncol, doi:10.1016/j.jaccao.2020.03.001
Gao, Ma, Ma, Wang, Wei et al., Clinical efficacy and safety of different antiviral regimens in patients with coronavirus disease, doi:10.3760/cma.j.cn121430-20201019-00679
Garcia-Vidal, Sanjuan, Moreno-García, Incidence of coinfections and superinfections in hospitalized patients with COVID-19: a retrospective cohort study, Clin Microbiol Infect
Gardiner, Shemie, Manara, Opdam, International perspective on the diagnosis of death, Br J Anaesth
Gattinoni, Coppola, Cressoni, Busana, Rossi et al., COVID-19 does not lead to a "typical" acute respiratory distress syndrome, Am J Respir Crit Care Med
Gattinoni, Tonetti, Cressoni, Ventilator-related causes of lung injury: the mechanical power, Intensive Care Medicine
Genbrugge, Meex, Boer, Increase in cerebral oxygenation during advanced life support in out-of-hospital patients is associated with return of spontaneous circulation, Crit Care
Gibson, Qin, Puah, COVID-19 acute respiratory distress syndrome (ARDS): clinical features and differences from typical pre-COVID-19 ARDS, Med J Aust
Girard, Pandharipande, Ely, Delirium in the intensive care unit, Crit Care, doi:10.1186/cc6149
Giustino, Croft, Oates, Takotsubo Cardiomyopathy in COVID-19, J Am Coll Cardiol, doi:10.1016/j.jacc.2020.05.068
Giustino, Pinney, Coronavirus and Cardiovascular Disease, Myocardial Injury, and Arrhythmia: JACC Focus Seminar, J Am Coll Cardiol, doi:10.1016/j.jacc.2020.08.059
Gopinathannair, Merchant, Lakkireddy, Etheridge, Feigofsky et al., COVID-19 and cardiac arrhythmias: a global perspective on arrhythmia characteristics and management strategies, J Interv Card Electrophysiol
Gormsen, Svart, Thomsen, None, J Am Heart Ass
Gorospe, Ayala-Carbonero, Ureña-Vacas, Spontaneous Pneumomediastinum in Patients With COVID-19: A Case Series of Four Patients, Archivos de Bronconeumología (English Edition), doi:10.1016/j.arbr.2020.06.004
Grams, Estrella, Coresh, Brower, Liu, Fluid balance, diuretic use, and mortality in acute kidney injury, Clin J Am Soc Nephrol, doi:10.2215/cjn.08781010
Grasselli, Cattaneo, Florio, Mechanical ventilation parameters in critically ill COVID-19 patients: a scoping review, Crit Care
Grasselli, Md, Zangrillo, Md, Zanella et al., Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy, JAMA
Grasselli, Pesenti, Cecconi, Critical Care Utilization for the COVID-19 Outbreak, JAMA, doi:10.1056/nejmoa2002032
Grasselli, Zangrillo, Zanella, Antonelli, Cabrini et al., Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Jama
Grasselli, Zangrillo, Zanella, Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy, JAMA
Grasselli, Zangrillo, Zanella, Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy, JAMA, doi:10.1001/jama.2020.5394
Grieco, Bongiovanni, Chen, Menga, Cutuli et al., Respiratory physiology of COVID-19-induced respiratory failure compared to ARDS of other etiologies, Crit Care, doi:10.1186/s13054-020-03253-2
Griffin, Resar, IHI Global Trigger Tool for Measuring Adverse Events
Gross, None
Grosu, Lee, Lee, Eden, Eikermann et al., Diaphragm muscle thinning in patients who are mechanically ventilated, Chest, doi:10.1378/chest.11-1638
Grosu, Ost, Lee, Diaphragm muscle thinning in subjects receiving mechanical ventilation and its effect on extubation, Respir Care, doi:10.4187/respcare.05370
Guan, Ni, Hu, Liang, Ou et al., Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med
Guan, Ni, Hu, Liang, Ou et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, EClinicalMedicine
Guarino, None, L. Mascia
Guidet, The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study, Intensive care medicine
Guillon, Laurent, Godillon, Long-term mortality of elderly patients after intensive care unit admission for COVID-19, Intensive Care Med, doi:10.1007/s00134-021-06399-x
Guo, Fan, Chen, Wu, Zhang et al., Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19), JAMA Cardiol, doi:10.1001/jamacardio.2020.1017
Gupta, Coca, Chan, AKI Treated with Renal Replacement Therapy in Critically Ill Patients with COVID-19, Journal of the American Society of Nephrology, doi:10.1681/ASN.2020060897
Gupta, Hayek, Wang, Factors Associated With Death in Critically Ill Patients With Coronavirus Disease 2019 in the US, JAMA Intern Med
Gupta, Madhavan, Sehgal, Nair, Mahajan et al., Extrapulmonary manifestations of COVID-19, Nat Med
Guérin, Albert, Beitler, Gattinoni, Jaber et al., Prone position in ARDS patients: why, when, how and for whom, Intensive Care Med. 1 de diciembre de
Guérin, Reignier, Richard, Beuret, Gacouin et al., Prone positioning in severe acute respiratory distress syndrome, N Engl J Med
Habashi, Other approaches to open-lung ventilation: airway pressure release ventilation, Critical care medicine
Hahn, Patel, Dull, Human glycocalyx shedding: Systematic review and critical appraisal, Acta Anaesthesiol Scand, doi:10.1111/aas.13797
Hajdu, None, C. Rookes, 1 ; R. Whittaker
Hamilton, Chu, Herridge, Determinants of depressive symptoms at 1 year following ICU discharge in survivors of > 7 days of mechanical ventilation, Chest
Han, Ma, Li, Liu, Zhao et al., Profiling serum cytokines in COVID-19 patients reveals IL-6 and IL-10 are disease severity predictors, Emerg Microbes Infect, doi:10.1080/22221751.2020.1770129
Hao, Xu, Ma, Xu, Lyu et al., In-hospital cardiac arrest outcomes among patients with COVID-19 pneumonia in Wuhan, Resuscitation
Harris, Taylor, Minor, Elliott, The REDCap Consortium: Building an International Community of Software Platform Partners, J Biomed Inform
Harrison, Lone, Haddow, Macgillivray, Khan et al., External validation of the intensive care national audit & research centre (ICNARC) risk prediction model in critical care units in Scotland, BMC Anesthesiol
Hasan, Capstick, Ahmed, Kow, Mazhar et al., Mortality in COVID-19 patients with acute respiratory distress syndrome and corticosteroids use: a systematic review and meta-analysis, Expert Rev Respir Med
Hatch, Young, Barber, Griffiths, Harrison et al., Anxiety, Depression and Post Traumatic Stress Disorder after critical illness: a UK-wide prospective cohort study, Critical Care, doi:10.1186/s13054-018-2223-6
Hawkins, Dugaiczyl, The human serum albumin gene: structure of a unique locus, Gene
He, A multicentre RCT of noninvasive ventilation in pneumoniainduced early acute respiratory distress syndrome, Critical Care
Helms, Tacquard, Severac, High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study, Intensive Care Med
Helms, Tacquard, Severac, Leonard-Lorant, Ohana et al., Investigators I. Effect of Intermediate-Dose vs Standard-Dose Prophylactic Anticoagulation on Thrombotic Events, Extracorporeal Membrane Oxygenation Treatment, or Mortality Among Patients With COVID-19 Admitted to the Intensive Care Unit: The INSPIRA-TION Randomized Clinical Trial, J community Hosp Intern Med Perspect, doi:10.1007/s11239-020-02138-z
Herridge, Cameron, One-year outcomes in caregivers of critically ill patients, N Eng J Med
Herridge, Cheung, Tansey, One-Year Outcomes in Survivors of the Acute Respiratory Distress Syndrome, New Engl J Med
Herridge, Moss, Hough, Hopkins, Rice et al., Recovery and outcomes after the acute respiratory distress syndrome (ARDS) in patients and their family caregivers, Intensive Care Med, doi:10.1007/s00134-016-4321-8
Herridge, Tansey, Mattè, Functional Disability 5 Years after Acute Respiratory Distress Syndrome, New Engl J Med
Hert, Staender, Fritsch, Pre-operative evaluation of adults undergoing elective noncardiac surgery: Updated guideline from the European Society of Anaesthesiology, Eur J Anaesthesiol, doi:10.1097/EJA.0000000000000817
Hilder, Herbstreit, Adamzik, Beiderlinden, Bürschen et al., Comparison of mortality prediction models in acute respiratory distress syndrome undergoing extracorporeal membrane oxygenation and development of a novel prediction score: the PREdiction of Survival on ECMO Therapy-Score (PRESET-Score), Critical Care
Hoiting, Hölters 8 ; M. Van Der Steen 9 ; W. Jacobs 10 ; V. Versluijs 10 ; H. Endeman 11 ; EJ
Honarmand, Lalli, Priestap, Natural history of cognitive impairment in critical illness survivors a systematic review, Am J Respir Crit Care Med
Hooper, Nápoles, Ej, COVID-19 and Racial/Ethnic Disparities, JAMA
Hopkins, Herridge, Quality of life, emotional abnormalities,and cognitive dysfunction in survivors of acute lung injury/acute respiratory distress syndrome, Clin Chest Med
Hopkins, Weaver, Lk, Collingridge, Two years cognitive, emotional, and quality of life outcomes in acute respiratory distress syndrome, Am J RespirCrit Care Med
Horby, Lim, Emberson, Dexamethasone in Hospitalized Patients with Covid-19-Preliminary Report, N Engl J Med, doi:10.1056/NEJMoa2021436
Horby, Lim, Emberson, Mafham, Bell et al., Dexamethasone in Hospitalized Patients with Covid-19, N Engl J Med
Hoste, Bagshaw, Bellomo, Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study, Intensive Care Med
Hravnak, None, J Clin Monit Comput
Hravnak, None, J Electrocardiol
Hu, Zhou, Zheng, Li, Ling et al., Application of high-flow nasal cannula in hypoxemic patients with COVID-19: a retrospective cohort study, BMC Pulmonary Medicine
Huang, Wang, Li, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Huang, Wang, Li, Ren, Zhao, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, The Lancet
Huh, Weix, Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin, Eur Heart J
Huntley, Rates of Maternal and Perinatal Mortality and Vertical Transmission in Pregnancies Complicated by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-Co-V-2) Infection: A Systematic Review, Obstet Gynecol
Hunziker, None
Iannaccone, Scacciavillani, Buono, Camilli, Ronco et al., Weathering the cytokine storm in COVID-19: therapeutic implications, CardioRenal Med, doi:10.1159/000509483
Ics, Guidelines for the Provision of Intensive Care Services, Version 2. ICS
Icu, Belgium, Department of intensive care, J. Berg Intensive Care Medicine Experimental
Icu, Health, Kuwait, None
Icu, Hospital, Greece; 2 Laboratory, Sismanogleio General Hospital, Z. Athanasa (Athanassa) Intensive Care Medicine Experimental
Icu, Insular-Materno Infantil
Icu, Vallecamonica, Department of internal medicine, A. CORONA Intensive Care Medicine Experimental
Intensive, Madrid, Spain, Servicio medicina intensiva, hospital universitario virgen macarena
Ischaki, Nasal High Flow Therapy: A Novel Treatment Rather than a More Expensive Oxygen Device, European Respiratory Review, doi:10.1183/16000617.0028-2017
Ishii, Majerus, Thrombomodulin is present in human plasma and urine, J Clin Invest
Itu, Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom Correspondence: M. Chotalia Intensive Care Medicine Experimental
Iyer, None, Crit. Care Resusc
Jain, Kollisch-Singule, Sadowitz, Dombert, Satalin et al., The 30-year evolution of airway pressure release ventilation (APRV)
Jakobsen, Wetterslev, Winkel, Lange, Gluud, Thresholds for statistical and clinical significance in systematic reviews with meta-analytic methods, BMC Med Res Metodol
Janssen, Kamps, Spontaneous pneumomediastinum in a male adult with COVID-19 pneumonia, The American Journal of Emergency Medicine, doi:10.1016/j.ajem.2020.07.066
Jardine, Nmpa, Team, Maternity Admissions to Intensive Care in England, Wales and Scotland in 2015/16: A Report from the National Maternity and Perinatal Audit
Jci, Communicating Clearly and Effectively to Patients How to Overcome Common Communication Challenges in Health Care. 11
Jedlicka, Becker, Chappell, Glycocalyx, None, Crit Care Clin
Jeffs, Darbyshire, Measuring Sleep in the Intensive Care Unit: A Critical Appraisal of the Use of Subjective Methods, Journal of Intensive Care Medicine, doi:10.1177/0885066617712197
Jeitziner, End-of-life care during the COVID-19 pandemic-What makes the difference?, Nurs Crit Care
Jennett, Snoek, Bond, Brooks, Disability after severe head injury: observations on the use of the Glasgow Outcome Scale, Neurosurgery, and Psychiatry, doi:10.1136/jnnp.44.4.285
Jentzer, Chonde, Dezfulian, None, Biomed Res Int
Johannigman, Md; Davis, Md; Miller, Md; Campbell, Rrt; Luchette et al., None
Johansen, Johansson, Ostrowski, Bestle, Hein et al., Profound Endothelial Damage Predicts Impending Organ Failure and Death in Sepsis, Semin Thromb Hemost
Johansson, Stensballe, Ostrowski, Shock induced endotheliopathy (SHINE) in acute critical illness-a unifying pathophysiologic mechanism, Crit Care
Johnson, Pollard, Shen, Hl, Feng et al., MIMIC-III, a freely accessible critical care database, Scientific data
Jones, A Position Paper on Nasogastric Tube Safety
Jones, Nakamura, Mccabe, Cardiogenic shock: evolving definitions and future directions in managementOpen, Heart, doi:10.1136/openhrt-2018-000960
Jongman, Partial Deletion of Tie2 Affects Microvascular Endothelial Responses to Critical Illness in A Vascular Bed and Organ-Specific Way. Shock, doi:10.1097/SHK.0000000000001226
Kallet, Lipnick, End-tidal-to-arterial pco2 ratio as signifier for physiologic deadspace ratio and oxygenation dysfunction in acute respiratory distress syndrome, Respir Care
Kandy, Lanka, None, Critical Care, National Hospital
Kaneko, Fujita, Ogino, Yamamoto, Tsuruta et al., Serum neutrophil gelatinase-associated lipocalin levels predict the neurological outcomes of out-of-hospital cardiac arrest victims, BMC Cardiovasc Disord, doi:10.1186/s12872-017-0545-y
Kaneko, Tocilizumab in rheumatoid arthritis: efficacy, safety and its place in therapy, Ther Adv Chronic Dis, doi:10.1177/2040622312466908
Kariyanna, Ramalanjaona, Al-Sadawi, Jayarangaiah, Hegde et al., Coronary Embolism and Myocardial Infarction: A Scoping Study, Am J Med Case Rep, doi:10.12691/ajmcr-8-2-1
Karlsen, Wiberg, Laigaard, Pedersen, Rokamp et al., A systematic review of trial registry entries for randomized clinical trials investigating COVID-19 medical prevention and treatment, PLoS One
Karunathilake, Karunadasa, Kulasiri H R 2, World Health Organization. COVID-19 Weekly Epidemiological Update 22
Keep, Messmer, Sladden, Burrell, Pinate et al., National early warning score at Emergency Department triage may allow earlier identification of patients with severe sepsis and septic shock: a retrospective observational study, Emergency Medicine Journal
Kelm, Perrin, Cartin-Ceba, Gajic, Schenck et al., Fluid Overload in Patients With Severe Sepsis and Septic Shock Treated With Early Goal-Directed Therapy Is Associated With Increased Acute Need for Fluid-Related Medical Interventions and Hospital Death, Shock
Khalid, Khalid, Qabajah, Barnard, Qushmaq, Healthcare Workers Emotions, Perceived Stressors and Coping Strategies During a MERS-CoV Outbreak, Clin Med Res
Khan, High Incidence of Barotrauma in Patients with Severe Coronavirus Disease, Journal of Intensive Care Medicine
Khawaja, Jafri, Siddiqui, Hashmi, Ghani, The utility of neutrophil gelatinase-associated lipocalin (NGAL) as a marker of acute kidney injury (AKI) in critically ill patients, Biomarker research, doi:10.1186/s40364-019-0155-1
Khwaja, KDIGO clinical practice guidelines for acute kidney injury, Nephron Clin Pract, doi:10.1159/000339789
Khwaja, KIDGO clinical practice guidelines for acute kidney injury, Nephron Clin Pract
Kindermann, Barth, Mahfoud, Ukena, Lenski et al., Update on Myocarditis, Journal of the American College of Cardiology
King, None, J Adv Nurs
Klitgaard, Schjørring, Lange, Møller, Perner et al., Bayesian and heterogeneity of treatment effect analyses of the HOT-ICU trial-a secondary analysis protocol, Acta Anaesthesiol Scand
Klompas, Li, Kleinman, Szumita, Massaro, Associations between ventilator bundle components and outcomes, JAMA Intern Med, doi:10.1001/jamainternmed.2016.2427
Klompas, Speck, Howell, Greene, Berenholtz, Reappraisal of routine oral care with chlorhexidine gluconate for patients receiving mechanical ventilation: systematic review and meta-analysis, JAMA Intern Med, doi:10.1001/jamainternmed.2014.359
Kluge, Janssens, Welte, Weber-Carstens, Marx et al., S2k-Leitlinie-Empfehlungen zur intensivmedizinischen Therapie von Patienten mit COVID-19, doi:10.5414/ATX02525
Knott, Ryou, Sun, None, Am J Physiol Heart Circ Physiol
Koenig, Kaplan, Clinical Applications for EPs in the ICU, J Clin Neurophysiol
Koers, Schlack, Hollmann, De Hert, Preckel, European implementation of the, doi:10.23736/S0375-9393.16.11504-4
Kompaniyets, Ga, Belay, Body Mass Index and Risk for COVID-19-Related Hospitalization, Intensive Care Unit Admission, Invasive Mechanical Ventilation, and Death -United States, MMWR Morb Mortal
Konstantinides, Torbicki, Agnelli, Danchin, Fitzmaurice et al., 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism, Eur Heart J
Kopczynska, Sharif, Cleaver, Spencer, Kurani et al., Sepsisrelated deaths in the at-risk population on the wards: attributable fraction of mortality in a large point-prevalence study, BMC research notes
Koulouras, Papathanakos, Papathanasiou, Nakos, Efficacy of prone position in acute respiratory distress syndrome patients: A pathophysiology-based review, World journal of critical care medicine, doi:10.5492/wjccm.v5.i2.121
Kramer, Kiggins, Zimmerman, intensive care unit readmissions in U.S. hospitals: Patient characteristics, risk factors, and outcomes, Critical Care Medicine, doi:10.1097/CCM.0b013e31822d751e
Kramer, Lo, Dickert, CPR in the covid-19 era-an ethical framework, N Engl J Med
Kraut, Madias, Metabolic acidosis: pathophysiology, diagnosis and management, Nat Rev Nephrol
Kristensen, Knuuti, Saraste, ESC/ESA Guidelines on noncardiac surgery: cardiovascular assessment and management: The Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA), doi:10.1093/eurheartj/ehu282
Kubitz, Annecke, Forkl, Kemming, Kronas et al., Validation of pulse contour derived stroke volume variation during modifications of cardiac afterload, Br J Anaesth
Kuiper, Lilja 1 ; T. Pellis, 10 ; C. Rylander 11, R. Siemund
Kumari, Dembra, Dembra, The Role of Vitamin C as Adjuvant Therapy in COVID-19, Cureus, doi:10.7759/cureus.11779
Kurtz, Fitts, Sumer, Jalon, Cooke et al., How Does Care Differ for Neurological Patients Admitted to a Neurocritical Care Unit Versus a General ICU?, Neurocritical Care, doi:10.1007/s12028-011-9539-2
Labuzzeta, Rosand, Vranceanu, Review: Post-Intensive Care Syndrome: Unique Challenges in the Neurointensive Care Unit, Neurocrit Care, doi:10.1007/s12028-019-00826-0
Landrigan, Rahman, Sullivan, Vittinghoff, Barger et al., Effect on Patient Safety of a Resident Physician Schedule without 24-Hour Shifts, The New England Journal of Medicine
Laurent, Fournier, Lheureux, Delgado, Bocci et al., An international tool to measure perceived stressors in intensive care units: the PS-ICU scale, Annals of intensive care. Accepted ICMx
Lavallée, Gray, Dumville, The effects of care bundles on patient outcomes: a systematic review and meta-analysis, Implementation Sci, doi:10.1186/s13012-017-0670-0
Leaver, None
Lebreton, Extracorporeal membrane oxygenation network organisation and clinical outcomes during the COVID-19 pandemic in Greater Paris, France: a multicentre cohort study, Lancet Respir Dis
Ledoux, None
Lellouche, Taillé, Maggiore, Qader, Her et al., Influence of ambient air and ventilator output temperature on performances of heated-wire humidifiers, Am J Respir Crit Care Med
Lemiale, Dumas, Mongardon, None, Intensive Care Med
Lemiale, Intensive care unit mortality after cardiac arrest: the relative contribution of shock and brain injury in a large cohort, Intensive Care Med
Levine, Nguyen, Taylor, Rapid Disuse Atrophy of Diaphragm Fibers in Mechanically Ventilated Humans, N Engl J Med
Li, Wang, Feng, Xu, Xu et al., Sex-Specific Associations of Smoking with Spontaneous Subarachnoid Hemorrhage: Findings from Observational Studies, Journal of Stroke and Cerebrovascular Diseases
Libby, Lüscher, COVID-19 is, in the end, an endothelial disease, Eur Heart J
Lichtenstein, Mezière, Relevance of lung ultrasound in the diagnosis of acute respiratory failure the BLUE protocol, Chest, doi:10.1378/chest.07-2800
Liu, Corticosteroid treatment in severe COVID-19 patients with acute respiratory distress syndrome, J Clin Invest, doi:10.1172/JCI140617
Liu, Li, Chen, Gao, Zeng et al., Dynamic interleukin-6 level changes as a prognostic indicator in patients with COVID-19, Front Pharmacol, doi:10.3389/fphar.2020.01093
Liu, Liu, Xu, Xu, Huang et al., Ventilatory ratio in hypercapnic mechanically ventilated patients with COVID-19-associated acute respiratory distress syndrome, Am J Resp Crit Care Med, doi:10.1164/rccm.202002-0373LE
Liu, Zhang, Yang, Ma, Li et al., The role of interleukin-6 in monitoring severe case of coronavirus disease 2019, EMBO Mol Med, doi:10.15252/emmm.202012421
Lloyd, Tang, Benson, Diaphragmatic paralysis: the use of M mode ultrasound for diagnosis in adults, Spinal Cord
Lobo-Valbuena, García-Arias, Pérez, Delgado, Gordo, Characteristics of critical patients with COVID-19 in a Spanish secondlevel hospital, Medicina Intensiva, doi:10.1016/j.medin.2020.06.020
Lorusso, Centofanti, Gelsomino, Barili, Mauro et al., Venoarterial Extracorporeal Membrane Oxygenation for Acute Fulminant Myocarditis in Adult Patients: A 5-Year Multi-Institutional Experience, Ann Thorac Surg
Luca Grieco, Md, Menga, Md, Cesarano et al., Effect of Helmet Noninvasive Ventilation vs High-Flow Nasal Oxygen on Days Free of Respiratory Support in Patients With COVID-19 and Moderate to Severe Hypoxemic Respiratory Failure. The HENIVOT Randomized Clinical Trial, JAMA
Maas, Stocchetti, Bullock, Moderate and severe traumatic brain injury in adults, The Lancet.Neurology, doi:10.1016/S1474-4422(08)70164-9
Macintyre, Evidence-Based Guidelines for Weaning and Discontinuing Ventilatory Support, Chest
Mahase, Covid-19: Intensive care mortality has fallen by a third since pandemic began, researchers find, BMJ
Makdisi, Wang, Extra Corporeal Membrane Oxygenation (ECMO) review of a lifesaving technology, J Thorac Dis, doi:10.3978/j.issn.2072-1439.2015.07.17
Malbrain, None, Critical Care Med
Malbrain, None, Minerva Anestesiol
Malysz, Dabrowski, Böttiger, Smereka, Kulak et al., Resuscitation of the patient with suspected/confirmed COVID-19 when wearing personal protective equipment: A randomized multicenter crossover simulation trial, Cardiol J
Mandigers, Termorshuizen, Keizer, Rietdijk, Gommers et al., Higher 1-year mortality in women admitted tot he intensive care units after cardiac arrest: A nationwide overview from the Netherlands between 2010-2018, Journal of Critical Care
Marchioni, Castaniere, Tonelli, Fantini, Fontana et al., Ultrasound-assessed diaphragmatic impairment is a predictor of outcomes in patients with acute exacerbation of chronic obstructive pulmonary disease undergoing noninvasive ventilation, Crit Care
Marik, Bedigian, Refeeding hypophosphatemia in critically ill patients in an intensive care unit. A prospective study, doi:10.1001/archsurg.1996.01430220037007
Marshall, None, Crit Care
Martinelli, COVID-19 and Pneumothorax: A Multicentre Retrospective Case Series, Eur Respir J
Martinelli, Ingle, Newman, COVID-19 and Pneumothorax: A Multicentre Retrospective Case Series, European Respiratory Journal, doi:10.1183/13993003.02697-2020
Martinez-Losas, Lopez De Sa, Armada, Rosillo, Monedero et al., Neuron-specific enolase kinetics: An additional tool for neurological prognostication after cardiac arrest, Rev. Esp. Cardiol
Marvaki, Papachristidis, Nakou, Toth, Gallagher et al., Innovative transthoracic echocardiographic imaging on prone ventilated patients with COVID-19 using a transesophageal probe, JACC: Cardiovascular Imaging
Masclans, Early non-invasive ventilation treatment for severe influenza pneumonia, Clinical Microbiology and Infection
Masseoudi, Ammous 3 ; S. Ben Lakhal 1 1 Intensive care unit, Hospital la Rabta, Tunisia Correspondence: A. Trifi Intensive Care Medicine Experimental
Matamis, Soilemezi, Tsagourias, Sonographic evaluation of the diaphragm in critically ill patients. Technique and clinical applications, Intensive Care Med
Matta, Chaudhary, Lo, Dejoy R 3rd, Gul et al., Timing of Intubation and Its Implications on Outcomes in Critically Ill Patients With Coronavirus Disease 2019 Infection, Crit Care Explor, doi:10.1097/CCE.0000000000000262
Mattsson, Zetterberg, Nielsen, Serum tau and neurological outcome in cardiac arrest, Ann Neurol
Mauri, Turrini, Eronia, Grasselli, Volta et al., Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory failure, Am J Respir Crit Care Med
Maury, Vassal, Offenstadt, Cardiac contractility during severe ketoacidosis, N Engl J Med
Mccoy, Chertow, Chang, Patterns of diuretic use in the intensive care unit, PLoS ONE, doi:10.1371/hiyrbak.prone.0217911
Mcdonald, Heggie, Jones, Thorne, Hulme, Rescuer fatigue under the 2010 ERC guidelines, and its effect on cardiopulmonary resuscitation (CPR) performance, Emerg Med J
Mcgonagle, Frcpi, Bridgewood, James, Meaney et al., A tricompartmental model of lung oxygenation disruption to explain pulmonary and systemic pathology in severe COVID-19 Prof, doi:10.1016/S2213-2600(21)00213-7
Mcguinness, Zhan, Rosenberg, Increased Incidence of Barotrauma in Patients with COVID-19 on Invasive Mechanical Ventilation, Radiology
Mclean, Huang, Right heart assessment, Critical Care Ultrasound Manual
Mclean, The Definition of Death: Contemporary Controversies
Mcwilliams, Weblin, Hodson, Veenith, Whitehouse, Snelson, C., and the QEHB COVID-19 Research Team. Rehabilitation Levels in COVID-19 Patients Admitted to Intensive Care Requiring Invasive Ventilation: An Observational Study, Annals of the American Thoracic Society, doi:10.1513/AnnalsATS.202005-560OC
Melo F De Af, Macedo, Bezerra, A systematic review and meta-analysis of acute kidney injury in the intensive care units of developed and developing countries, PLoS One
Mendelson, Nel, Blumberg, Madhi, Dryden et al., Long-COVID: An evolving problem with an extensive impact, South African Med J, doi:10.7196/SAMJ.2021.v111i1.15433
Menk, Estenssoro, Sahetya, Neto, Sinha et al., Current and evolving standards of care for patients with ARDS, Intensive Care Med. 1 de diciembre de
Menter, Postmortem examination of COVID-19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings in lungs and other organs suggesting vascular dysfunction, Histopathology
Messmer, Zingg, Müller, Gerber, Schefold et al., Fluid Overload and Mortality in Adult Critical Care Patients-A Systematic Review and Meta-Analysis of Observational Studies*, Critical Care Medicine
Methangkool, Tollinche, Sparling, Agarwala, Communication: Is There a Standard Handover Technique to Transfer Patient Care, International Anesthesiology Clinics
Micu, Center, Ljubljana, Cesta, Ljubljana et al., Department of medical and surgical sciences
Middeldorp, Coppens, Van Haaps, Incidence of venous thromboembolism in hospitalized patients with COVID-19, J Thromb Haemost
Mikkelsen, Shull, Biester, Taichman, Lynch et al., Cognitive, mood and quality of life impairments in a select population of ARDS survivors, Respirology, doi:10.1111/j.1440-1843.2008.01419.x
Min, Predictive Modeling of the Hospital Readmission Risk from Patients' Claims Data Using Machine learning: A Case Study on COPD, Scientific Reports, doi:10.1038/s41598-019-39071-y
Mitaka, Kuno, Takagi, Patrawalla, Incidence and mortality of COVID-19-associated pulmonary aspergillosis: A systematic review and meta-analysis, Mycoses, doi:10.1111/myc.13292
Mohamed, Al-Shokri, Yousaf, Danjuma, Parambil et al., Frequency of abnormalities detected by point-of-care lung ultrasound in symptomatic COVID-19 patients: Systematic review and meta-analysis
Mohan, Tauseen, Spontaneous pneumomediastinum in COVID-19, BMJ Case Reports CP, doi:10.1136/bcr-2020-236519
Mokhtari, Hassani, Ghaffari, Ebrahimi, Yarahmadi et al., COVID-19 and multiorgan failure: a narrative review on potential mechanisms, J Mol Histol, doi:10.1007/s10735-020-09915-3
Monti, Leggieri, Fominskiy, Two months quality of life of COVID-19 invasively ventilated survivors; an Italian single-center study, Acta Anaesthesiol Scand
Moore, June, Cytokine release syndrome in severe COVID-19, Science
Morelli, Sorbo, Pesenti, Ranieri, Extracorporeal carbondioxide removal (ECCO2R) in patients with acute respiratory failure, Intensive Care Med
Moreno, Vincent, Matos, The use of maximum SOFA score to quantify organ dysfunction/failure in intensive care. Results of a prospective, multicentre study, Intensive Care Medicine
Morimura, Takahashi, Doi, A pilot study of quantitative capillary refill time to identify high blood lactate levels in critically ill patients, Emerg Med J
Morris, Conway, Chb, Hay, Frca; Swann et al., Reducing ventilator-associated pneumonia in intensive care: Impact of implementing a care bundle, Critical Care Medicine, doi:10.1097/CCM.0b013e3182227d52
Moseby-Knappe, Mattsson, Nielsen, Serum Neurofilament Light Chain for Prognosis of Outcome After Cardiac Arrest, JAMA neurology
Moseby-Knappe, Pellis, Dragancea, Head computed tomography for prognostication of poor outcome in comatose patients after cardiac arrest and targeted temperature management, Resuscitation
Mueller, None, Triaging Interhospital Transfers' PSNET
Murao, Saito Atsishi, Acute eosinophilic pneumonia as a complication of Influenza A (H1N1) pulmonary infection. Sarcoidosis Vasc Diffuse Lung disease
Murao, Saito, Kuronuma, Acute eosinohpilic pneumonia accompanied with COVID-19: a case report
Musher, Abers, Vf, Acute Infection and Myocardial Infarction, N Engl J Med, doi:10.1056/NEJMra1808137
Mündel, Mechanisms of Nasal High Flow on Ventilation during Wakefulness and Sleep, Journal of Applied Physiology, doi:10.1152/japplphysiol.01308.2012
Navarro, None, MC. Martín Delgado
Navas-Blanco, Dudaryk, Management of Respiratory Distress Syndrome due to COVID-19 infection, BMC Anesthesiol, doi:10.1186/s12871-020â•fi01,095-7
Needham, Davidson, Cohen, Hopkins, Weinert et al., Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders' conference, Crit Care Med, doi:10.1097/CCM.0b013e318232da75
Neilsen, Wetterslev, Cronberg, Erlinge, Gasche et al., Targeted temperature management at 33 oC versus 36 oC after cardiac arrest, N Engl J Med
Neumann, Sousa-Uva, Ahlsson, Alfonso, Banning et al., ESC/ EACTS Guidelines on myocardial revascularization, Eur Heart J, doi:10.1093/eurheartj/ehy394
Newcombe, Baker, Burnstein, Tasker, Menon, Clinical communication with families in the age of covid-19: a challenge for critical care teams. The BMJ Opinion
Nhlbi Ards Network, Tools ; Shtml D. Talmor, Sarge, Malhotra, Donnell et al., Effect of Titrating Positive End-Expiratory Pressure (PEEP) With an Esophageal Pressure-Guided Strategy vs an Empirical High PEEP-Fio2 Strategy on Death and Days Free From Mechanical Ventilation Among Patients With Acute Respiratory Distress Syndrome: A Randomized Clinical Trial, New England Journal of Medicine
Nicholson, Wolmarans, Park, The role of albumin in critical illness, British Journal of Anaesthesia
Nicole, Sameena, Beniot, Outcomes of post-cardiac surgery patients with persistent hyperlactatemia in the intensive care unit: a matched cohort study, J Cardiothorac Surg
Niederman, Fein, Sepsis syndrome, the adult respiratory distress syndrome, and nosocomial pneumonia. A common clinical sequence, Clin Chest Med
Nielsen, Moller, Gormsen, None, Circulation
Nielsen, Wetterslev, Cronberg, Erlinge, Gasche et al., the TTM Trial Investigators Targeted Temperature Management at 33 °C versus 36 °C after Cardiac Arrest, Arrest Treatment J. Guo
Nolan, European Resuscitation Council and European Society of Intensive Care Medicine Guidelines for Post-resuscitation Care
Nolan, Neuroprognostication of the comatose adult patient after resuscitation from cardiac arrest
Nolan, None, Resuscitation
Nolan, Sandroni, Bottiger, European Resuscitation Council and European Society of Intensive Care Medicine guidelines 2021: postresuscitation care, Intensive Care Med
Nolan, Soar, Cariou, Cronberg, Moulaert et al., European Resuscitation Council and European Society of Intensive Care Medicine 2015 guidelines for post-resuscitation care, Emergency Room F. Cardoso 1 ; R. Passos 1 ; D. Alves, 1 ; L. Pereira 1 ; A. Colmente, 1 ; J. Abreu 1 ; R. Corga 1 ; J. Caldeiro, doi:10.1007/s00134-015-4051-3
None, None
Näätänen, The mismatch negativity (MMN)-a unique window to disturbed central auditory processing in ageing and different clinical conditions, Clin Neurophysiol
Oddo, Rossetti, Predicting neurological outcome after cardiac arrest, Curr Opin Crit Care
Oi, Sato, Nogaki, Association between venous blood lactate levels and differences in quantitative capillary refill time, Acute Med Surg
Oliveira, None, G. Costanza
Onders, Elmo, Kaplan, Katirji, Schilz, Extended Use of Diaphragm Pacing in Patients with Unilateral of Bilateral Diaphragm Dysfunction: A New Therapeutic Option, Surgery
Onders, Elmo, Kaplan, Schilz, Katirji et al., Long-term experience with diaphragm pacing for traumatic spinal cord injury: Early implantation should be considered, Surgery
Onders, Markowitz, Ho, Hardacre, Novitsky et al., Completed FDA feasibility trial of surgically placed temporary diaphragm pacing electrodes: A promising option to prevent and treat respiratory failure, Am J Surg
Ong, Short-Course Adjunctive Gentamicin as Empirical Therapy in Patients With Severe Sepsis and Septic Shock: A Prospective Observational Cohort Study, Clinical Infectious Diseases
Osadnik, Non-Invasive Ventilation for the Management of Acute Hypercapnic Respiratory Failure Due to Exacerbation of Chronic Obstructive Pulmonary Disease, Cochrane Database of Systematic Reviews, doi:10.1002/14651858.CD004104.pub4
Oshima, Delsoglio, Dupertuis, Singer, Waele et al., The clinical evaluation of the new indirect calorimeter developed by the ICALIC project, Clin Nutr
Page, Mckenzie, Bossuyt, Boutron, Hoffmann et al., The PRISMA 2020 statement: an updated guideline for reporting systematic reviewsBMJ, doi:10.1136/bmj.n71
Palevsky, Renal replacement therapy in acute kidney injury, Adv Chronic Kidney Dis
Pandharipande, Girard, Jackson, Long-Term Cognitive Impairment after Critical Illness, N Engl J Med
Pandya, Kaur, Sacher, 'corragain, Salerno et al., Ventilatory Mechanics in Early vs Late Intubation in a Cohort of Coronavirus Disease, Patients With ARDS: A Single Center's Experience. Chest, doi:10.1016/j.chest.2020.08.2084
Pape, Is there an association between female gender and outcome in severe trauma? A multi-center analysis in the Netherlands, Scand J Trauma Resusc Emerg Med, doi:10.1186/s13049-019-0589-3
Papoutsi, Giannakoulis, Xourgia, Routsi, Kotanidou et al., Effect of timing of intubation on clinical outcomes of critically ill patients with COVID-19: a systematic review and meta-analysis of nonrandomized cohort studies, Crit Care
Parikh, Angiopoietins and Tie2 in vascular inflammation, Curr Opin Hematol, doi:10.1097/MOH.0000000000000361
Park, Ahn, Lee, Kim, Min et al., Plasma neutrophil gelatinase-associated lipocalin as an early predicting biomarker of acute kidney injury and clinical outcomes after recovery of spontaneous circulation in out-of-hospital cardiac arrest patients, Resuscitation, doi:10.1016/j.resuscitation.2016.01.005
Park, Hwang, Lee, Park, Kim et al., Are loose-fitting powered air-purifying respirators safe during chest compression? A simulation study, doi:10.1016/j.ajem.2020.03.054
Parke, Nasal High-Flow Therapy Delivers Low Level Positive Airway Pressure, British Journal of Anaesthesia, doi:10.1093/bja/aep280
Patel, Chowdhury, Mills, Marron, Gangemi et al., ROX Index Predicts Intubation in Patients with COVID-19 Pneumonia and Moderate to Severe Hypoxemic Respiratory Failure Receiving High Flow Nasal Therapy
Patel, Menon, Tebbs, Hawker, Hutchinson et al., Specialist neurocritical care and outcome from head injury, Intensive Care Medicine, doi:10.1007/s00134-002-1235-4
Paul, Beta lactam antibiotic monotherapy versus beta lactamaminoglycoside antibiotic combination therapy for sepsis
Peck, Hibbert, Recent advances in the understanding and management of ARDS, doi:10.12688/f1000research.20411.1
Peek, Mugford, Tiruvoipati, Wilson, Allen et al., Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial, Lancet, doi:10.1016/S0140-6736(09)61069-2
Pelosi, Andrea, Vitale, Pesenti, Gattinoni, Vertical Gradient of Regional Lung Inflation in Adult Respiratory Distress Syndrome, Am J Respir Crit Care Med
Peng, Wang, Zhang, Findings of lung ultrasonography of novel corona virus pneumonia during the 2019-2020 epidemic, Intensive Care Med, doi:10.1007/s00134-020-05996-6
Pereira, Ef, De, Bethlem, Vieira et al., Lung Ultrasound in Covid 19 Pandemic, Winfocus
Perkins, European Resuscitation Council Guidelines 2021: Executive summary, Resuscitation, doi:10.1016/j.resuscitation.2021.02.003
Perren, Zürcher, Schefold, Clinical Approaches to Assess Post-extubation Dysphagia (PED) in the Critically Ill, Dysphagia, doi:10.1007/s00455-019-09977-w
Petran, Muelly, Dembinski, Steuer, Arens et al., Validation of RESP and PRESERVE score for ARDS patients with pumpless extracorporeal lung assist (pECLA), BMC anesthesiology
Pett, Leung, Taylor, Chong, Hla et al., Critical care transfers and COVID-19: Managing capacity challenges through critical care networks, Journal of the Intensive Care Society, doi:10.1177/1751143720980270
Philips, Turner-Stokes, Wade, Walton, British Society of Rehabilitation Medicine
Phua, Badia, Adhikari, Has mortality from acute respiratory distress syndrome decreased over time?: A systematic review, Am J Respir Crit Care Med
Pickkers, De Keizer, Dusseljee, Weerheijm, Van Der Hoeven et al., Body mass index is associated with hospital mortality in critically ill patients: an observational cohort study, Crit Care Med
Plummer, Gracey, Consensus conference on artificial airways in patients receiving mechanical ventilation, Chest
Pollard, Johnson, Raffa, Celi, Mark et al., The eICU Collaborative Research Database, a freely available multi-center database for critical care research, doi:10.1038/sdata.2018.178
Popkin, Du, Green, Beck, Algaith et al., Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships, Obesity Reviews
Powell, Kim, Roberge, Powered air-purifying respirator use in healthcare: Effects on thermal sensations and comfort, J Occup Environ Hyg
Powner, Ackerman, Grenvik, Medical diagnosis of death in adults: Historical contributions to current controversies, Lancet. Lancet Publishing Group
Price, Maclennan, Selective digestive or oropharyngeal decontamination and topical oropharyngeal chlorhexidine for prevention of death in general intensive care: systematic review and network meta-analysis, BMJ, doi:10.1136/bmj.g2197.17
Puig, Herrero, Guillamat-Prats, Gómez, Tijero et al., A new experimental model of acid-and endotoxin-induced acute lung injury in rats, Am J Physiol Lung Cell Mol Physiol, doi:10.1152/ajplung.00390.2015
Pun, Badenes, Prevalence and risk factors for delirium in critically ill patients with COVID-19 (COVID-D): a multicentre cohort study, Lancet Respir Med
Qanadli, Hajjam, Vieillard-Baron, Joseph, Mesurolle et al., New CT Index to Quantify Arterial Obstruction in Pulmonary Embolism, Am J Roentgenol. 1 juin
Quincho-Lopez, Quincho-Lopez, Case Report: Pneumothorax and Pneumomediastinum as Uncommon Complications of COVID-19 Pneumonia-Literature Review, The American Journal of Tropical Medicine and Hygiene, doi:10.4269/ajtmh.20-0815
Quincho-Lopez, Quincho-Lopez, Hurtado-Medina, Case ; Shan, Guangming et al., Spontaneous pneumomediastinum, pneumothorax and subcutaneous emphysema in COVID-19: case report and literature review, Rev Inst Med Trop Sao Paulo, doi:10.1590/S1678-9946202062076
Rachoin, Weisberg, Renal replacement therapy in the ICU, Crit Care Med
Rad, Yarmohammadian, A study of relationship between managers' leadership style and employees' job satisfaction
Ranard, Engel, Kirtane, Masoumi, Stefanini et al., ST-elevation myocardial infarction in patients with COVID-19: clinical and angiographic outcomes, European Heart Journal-Case Reports, doi:10.1161/CIRCULATIONAHA.120.050809
Ranieri, A. Pesenti 18 ; D. Brodie, 19 ; A. Arcadipane 20 1 Anesthesia and intensive care unit
Ranieri, Rubenfeld, Thompson, Acute Respiratory Distress Syndrome: The Berlin Definition
Ranieri, Rubenfeld, Thompson, Ferguson, Caldwell, Acute respiratory distress syndrome: the Berlin Definition, JAMA, doi:10.1001/jama.2012.5669
Ranney, Griffeth, Jha, Critical Supply Shortages -The Need for Ventilators and Personal Protective Equipment during the Covid-19 Pandemic, NEJM
Raoof, Nava, Carpati, Hill, High-Flow, Noninvasive Ventilation and Awake (Nonintubation) Proning in Patients With Coronavirus Disease 2019 With Respiratory Failure, doi:10.1016/j.chest.2020.07.013
Rath, Petersen-Uribe, Avdiu, Witzel, Jaeger et al., Impaired cardiac function is associated with mortality in patients with acute COVID-19 infection, Clin Res Cardiol
Recovery Collaborative Group, Horby, Lim, Dexamethasone in Hospitalized Patients with Covid-19-Preliminary Report, N Engl J Med
Recovery Collaborative Group, Horby, Lim, Emberson, Mafham et al., None, N Engl J Med Online ahead of print
Remuzzi, Remuzzi, COVID-19 and Italy: what next?, Lancet, doi:10.1016/S0140-6736(20)30627-9
Results, Average applied PEEP resulted 11 ± 2.9 cmH2O for BMI < 30 kg/ m2, 16 ± 3.18 cmH2O for BMI > 30 kg/m2. No patient presented a BMI greater than 50 kg/m2. After low-PEEP strategy application, patients' P/F ratio presented daily improvement from admission during next 72 h
Results, of 144 patients, 80 received azithromycine (either before or during hospitalization) versus 64 who not received. Age and comorbidities didn't differ, female gender tended to be more present in azithromycin group
Rey, Valero, Pinedo, Merino, López-Sendón et al., COVID-19 and simultaneous thrombosis of two coronary arteries, Rev Esp Cardiol (Engl Ed), doi:10.1016/j.rec.2020.05.021
Reynolds, Meyyappan, Thakkar, Mitigation of Ventilator-Induced Diaphragm Atrophy by Transvenous Phrenic Nerve Stimulation, Am J Respir Crit Care Med
Rezoagli, Fumagalli, Bellani, Definition and epidemiology of acute respiratory distress syndrome, Ann Transl Med. julio de
Ribaric, Turel, Knafelj, Gorjup, Stanic et al., Prophylactic versus clinically-driven antibiotics in comatose survivors or out-of-hospital cardiac arrest-A randomised pilot study, Resuscitation
Ricard, Lisboa, Caution for chlorhexidine gluconate use for oral care: insufficient data, Intensive Care Med, doi:10.1007/s00134-018-5217-6
Richardson, Hirsch, Narasimhan, Crawford, Mcginn et al., Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area, Jama
Richardson, Hirsch, Narasimhan, Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area, JAMA
Richter, Bellani, Harris, Melo, Winkler et al., Effect of prone position on regional shunt, aeration, and perfusion in experimental acute lung injury, Am. J. Respir. Crit. Care Med
Rickard, Ibitoye, Deakin, The Clinical Frailty Scale predicts adverse outcome in older people admitted to a UK major trauma centre, Age and Ageing
Riera, Extracorporeal membrane oxygenation retrieval in coronavirus disease 2019: a case-series of 19 patients supported at a high-volume extracorporeal membrane oxygenation center, Crit Care Expl
Robba, Battaglini, Ball, Nicolo' Patroniti, Loconte et al., Patients with COVID-19 admitted to Intensive Care Units in Sri Lanka: Experience from a resource limited setting B. Imbulpitiya 1 ; SWGJW. Chinthaka 1 ; A. Galliyadda 2 ; CV, Respiratory Physiology & Neurobiology, doi:10.1016/j.resp.2020.103455
Roberge, Benson, Kim, Thermal burden of N95 filtering facepiece respirators, Ann Occup Hyg
Roberts, To PAPR or not to PAPR?, Can J Respir Ther
Roberts, Yates, Sandercock, Farrell, Wasserberg et al., Effect of intravenous corticosteroids on death within 14 days in 10,008 adults with clinically significant head injury (MRC CRASH trial): randomised placebo-controlled trial, Lancet, doi:10.1016/S0140-6736(04)17188-2
Robertson-Malt, Malt, Farquhar, Greer, Heparin versus normal saline for patency of arterial lines
Roca, Caralt, Messika, Samper, Sztrymf et al., An Index Combining Respiratory Rate and Oxygenation to Predict Outcome of Nasal High-Flow Therapy, American Journal of Respiratory and Critical Care Medicine
Rochwerg, Bram, Official ERS/ATS Clinical Practice Guidelines: Noninvasive Ventilation for Acute Respiratory Failure, European Respiratory Journal, doi:10.1183/13993003.02426-2016
Rochwerg, Brochard, Elliott, Hess, Hill et al., Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure, Eur Resp J
Rodriguez, Auditory-evoked potentials during coma: do they improve our prediction of awakening in comatose patients, J Crit Care
Rodríguez, Risk Factors for Noninvasive Ventilation Failure in Critically Ill Subjects with Confirmed Influenza Infection, Respiratory Care
Rogers, Chesney, Oliver, Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic, Lancet Psychiatry
Rola, Farkas, Spiegel, Kyle-Sidell, Weingart et al., Rethinking the early intubation paradigm of COVID-19: time to change gears?, Clin Exp Emerg Med, doi:10.15441/ceem.20.043
Rola, Farkas, Spiegel, Rethinking the early intubation paradigm of COVID-19: time to change gears?, Clin Exp Emerg Med
Rosa, Antonelli, Ronco, Hypothermia and kidney: a focus on ischaemia-reperfusion injury. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association-European Renal Association, doi:10.1093/ndt/gfw038
Rosano, Early Percutaneous Tracheostomy in Coronavirus Disease 2019: Association With Hospital Mortality and Factors Associated With Removal of Tracheostomy Tube at ICU Discharge. A Cohort Study on Reference(s)
Rosenberg, Press, Fishbein, External validation of the IMPROVE bleeding risk assessment model in medical patients, J Thromb Haemost
Rossetti, Clinical neurophysiology for neurogical prognostication of comatose patients after cardiac arrest, Clin Neurophysiol
Rothwell, Coull, Silver, Fairhead, Giles et al., Population-based study of event-rate, incidence, case fatality, and mortality for all acute vascular events in all arterial territories (Oxford Vascular Study), The Lancet
Rudd, Johnson, Agesa, Shackelford, Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study, Lancet
Rundgren, Ullén, Morgan, Glover, Cranshaw et al., Renal function after out-of-hospital cardiac arrest; the influence of temperature management and coronary angiography, a post hoc study of the target temperature management trial, Crit Care, doi:10.1186/s13054-019-2390-0
Sack, Kellum, Parikh, The Angiopoietin-Tie2 Pathway in Critical Illness, Crit Care Clin
Saito, Asai, Matsunaga, Hayakawa, Terada et al., First and second COVID-19 waves in Japan: A comparison of disease severity and characteristics, J Infect
Sakagianni, None
Salama, Han, Yau, Reiss, Kramer et al., Tocilizumab in Patients Hospitalized with Covid-19 Pneumonia. (EMPACTA trial), N Engl J Med, doi:10.1056/NEJMoa2030340
Salama-Younes, Montazeri, Ismaïl, Roncin, Factor structure and internal consistency of the 12-item General Health Questionnaire (GHQ-12) and the Subjective Vitality Scale (VS), and the relationship between them: a study from France, Health Qual Life Outcomes
Salluh, Wang, Schneider, Outcome of delirium in critically ill patients: Systematic review and meta-analysis, BMJ Br Med J
Sandroni, Prediction of poor neurological outcome in comatose survivors of cardiac arrest: a systematic review, Intensive Care Med
Sandroni, Prognostication after cardiac arrest, Crit Care
Sanfilippo, Murabito, Messina, Cerebral regional oxygen saturation during cardiopulmonary resuscitation and return of spontaneous circulation: A systematic review and meta-analysis, Resuscitation
Sanjeevani, Pruthi, Kalra, Goel, Kalra, Role of neutrophil gelatinase-associated lipocalin for early detection of acute kidney injury, International journal of critical illness and injury science, doi:10.4103/2229-5151.141420
Savasi, Clinical Findings and Disease Severity in Hospitalized Pregnant Women With Coronavirus Disease 2019 (COVID-19), Obstet Gynecol
Schaller, Postmortem Examination of Patients With COVID-19, JAMA
Schjørring, Klitgaard, Perner, Wetterslev, Lange et al., Lower or Higher Oxygenation Targets for Acute Hypoxemic Respiratory Failure, N Engl J Med
Schmidt, Bailey, Sheldrake, Hodgson, Aubron et al., Predicting Survival after Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Failure. The Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) Score, Am J Respir Crit Care Med
Schmidt, Hajage, Lebreton, Monsel, Voiriot et al., Groupe de recherche clinique en reanimation et soins intensifs du patiente en insuffisance Respiratorire aigue (GRC-RESPIRE)
Schmidt, Wenzel, Mahn, Improved lung recruitment and oxygenation during mandatory ventilation with a new expiratory ventilation assistance device: A controlled interventional trial in healthy pigs, Eur J Anaesthesiol
Schoults, None, JAMA Otolaryngol Head Neck Surg
Schriger, Baraff, Defining normal capillary refill: variation with age, sex, and temperature, Ann Emerg Med
Schuler, Rose, Targeted Maximum Likelihood Estimation for Causal Inference in Observational Studies, American Journal of Epidemiology, doi:10.1093/aje/kww165
Schumacher, Gray, Michel, Alcock, Brinker, Respiratory protection during simulated emergency pediatric life support: a randomized, controlled, crossover study, Prehosp Disaster Med
Schweizer, Godet, Petit, Adherence of French cardiologists to guidelines for non-cardiac surgery, Anaesth Crit Care Pain Med, doi:10.1016/j.accpm.2015.12.009
Scores, of patients died during resuscitation, 48.2% (n = 55) showed ROSC, but died during hospitalization, so that a total of 89 patients died in hospital. 21.9% (n = 25) could be discharged from hospital and one year after discharge 9% of patients (n = 10) were still alive. Significant differences in respect to SOFA Scores were observed only for patients, post CA, who died during stay in hospital, in contrast to those who were discharged alive (p < 0.003). The SAPS-II-Score pre ICU-CA was significantly lower for patients, who could be discharged from hospital, than for those, who died during hospitalization (pre (p < 0.006) and post ICU-CA (p < 0.001)). In addition, SAPS-II Scores post CA for patients still alive one year after CA were significantly lower
Sekhon, Gooderham, Toyota, Kherzi, Hu et al., Implementation of Neurocritical Care Is Associated With Improved Outcomes in Traumatic Brain Injury, The Canadian Journal of Neurological Sciences, doi:10.1017/cjn.2015.25
Semeraro, Greif, Böttiger, Burkart, Cimpoesu et al., European Resuscitation Council Guidelines 2021: Systems saving lives, Resuscitation, doi:10.1016/j.resuscitation.2021.02.008
Semeraro, None, Resuscitation
Seymour, Liu, Iwashyna, Brunkhorst, Rea et al., Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3), JAMA
Shams, Coronary thrombosis in a young male with COVID-19, IDCases, doi:10.1016/j.idcr.2020.e00923
Shi, Qin, Shen, Cai, Liu et al., Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, JAMA Cardiol, doi:10.1001/jamacardio.2020.0950
Shor, Halabe, Rishver, Severe hypophosphatemia in sepsis as a mortality predictor, Ann Clin Lab Sci
Siassakos, Fox, Crofts, Hunt, Winter et al., The management of a simulated emergency: better teamwork, better performance, Resuscitation
Siemieniuk, Drug treatments for covid-19: living systematic review and network meta-analysis, BMJ, doi:10.1136/bmj.m2980
Silva, Ono, Souza, Sleep and immunity in times of COVID-19, Rev Assoc Med Bras, doi:10.1590/1806-9282.66.S2.143
Sin, King, Ballard, Llewellyn, Laupland et al., Hypophosphatemia and Outcomes in ICU: A Systematic Review and Meta-Analysis, J Intensive Care Med. Published online August, doi:10.1177/0885066620940274
Singer, Deutschman, Seymour, Shankar-Hari, Annane et al., The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3), JAMA
Singer, Pichard, Waele, Practical guidance for the use of indirect calorimetry during COVID 19 pandemic, Clin Nutr Exp
Skoretz, Flowers, Martino, The incidence of dysphagia following endotracheal intubation: a systematic review, Chest, doi:10.1378/chest.09-1823
Smith, Devane, Nichol, Roche, Care bundles for improving outcomes in patients with COVID-19 or related conditions in intensive care-a rapid scoping review. Cochrane Database of Systematic Reviews, doi:10.1002/14651858.CD013819
Smith, Edwards, Siassakos, Effective team training to improve outcomes in maternal collapse and perimortem caesarean section, Resuscitation
Soar, Nolan, Böttiger, European Resuscitation Council Guidelines for Resuscitation 2015: Sect. 3. Adult advanced life support, Resuscitation
Solomon, Corwin, Barclay, Quddusi, Dannenberg, Effectiveness of rapid response teams on rates of in-hospital cardiopulmonary arrest and mortality: A systematic review and meta-analysis, J Hosp Med
Spiegel, Leproult, Cauter, Impact of sleep debt on metabolic and endocrine function, Occup. Med
Spinelli, Mauri, Beitler, Pesenti, Brodie, Respiratory drive in the acute respiratory distress syndrome: pathophysiology, monitoring, and therapeutic interventions, Intensive Care Medicine
St, Kalhari, None
Stagno, Gibson, Breitbart, The delirium subtypes: a review of prevalence, phenomenology, pathophysiology, and treatment response, Palliat. Support. Care
Starmer, Srivastava, Allen, Landrigan, Sectish et al., I-PASS, a Mnemonic to Standardize Verbal Handoffs, Pediatrics
Storm, Krannich, Schachtner, Engels, Schindler et al., Impact of acute kidney injury on neurological outcome and long-term survival after cardiac arrest-A 10 year observational follow up, Journal of critical care, doi:10.1016/j.jcrc.2018.07.023
Strathfield, NSW: Sleep Health Foundation; 2021. Workplace Scheduling Solutions 2021 [cited 2021
Suarez-Sipmann, Ferrando, Villar, PEEP titration guided by transpulmonary pressure: lessons from a negative trial, J Thorac Dis
Sulaiman, Juhani, Eljaaly, Alharbi, Shabasy et al., Clinical Features and Outcomes of Critically Ill Patients with Coronavirus Disease 2019 (COVID-19): A Multicenter Cohort Study, doi:10.1016/j.jacc.2020.05.001
Summerhill, El-Sameed, Glidden, Monitoring recovery from diaphragm paralysis with ultrasound, Chest
Supinski, Morris, Dhar, Callahan, Diaphragm Dysfunction in Critical Illness, Chest, doi:10.1016/j.chest.2017.08.1157
Suzuki, Egi, Schneider, Bellomo, Hart et al., Hypophosphatemia in critically ill patients, J Crit Care, doi:10.1016/j.jcrc.2012.10.011
Sweeney R Mac, Mcauley, Acute respiratory distress syndrome, Lancet
Taccone, Revisiting the loading dose of amikacin for patients with severe sepsis and septic shock, Critical Care
Tay, Khoo, Loh, Surgical considerations for tracheostomy during the COVID-19 pandemic, JAMA Otolaryngol. Head Neck Surg, doi:10.1001/jamaoto
Tedeschi, Rizzi, Biscaglia, Tumscitz, Acute myocardial infarction and large coronary thrombosis in a patient with COVID-19, Catheter Cardiovasc Interv, doi:10.1002/ccd.29179
Terzi, Acute respiratory distress syndrome and pneumothorax, J Thorac Dis
The, Group, Dexamethasone in Hospitalized Patients with Covid-19, N Engl J Med, doi:10.1056/NEJMoa2021436
Theodore W Marcy, None, P.t. Barotrauma: Detection, Recognition, and Management. Chest
Thille, Harrois, Schortgen, Brun-Buisson, Brochard, Outcomes of extubation failure in medical intensive care unit patients, Critical Care Medicine
Thompson, Chambers, Liu, Acute Respiratory Distress Syndrome, N Engl J Med. 10 de agosto de
Thompson, Wendell, Potter, Fehnel, Wilterdink et al., The use of transcranial Doppler ultrasound in confirming brain death in the setting of skull defects and extraventricular drains, Neurocrit Care, doi:10.1007/s12028-014-9979-6
Thongprayoon, Cheungpasitporn, Kashani, Serum creatinine level, a surrogate of muscle mass, predicts mortality in critically ill patients, Journal of thoracic disease, doi:10.21037/jtd.2016.03.62
Thrombomodulin, None
Thygesen, Alpert, Jaffe, Chaitman, Bax et al., Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018), J Am Coll Cardiol, doi:10.1016/j.jacc.2018.08.1038
Tipping, Bilish, Harrold, Holland, Chan et al., The impact of frailty in critically ill patients after trauma: A prospective observational study, Australian Critical Care
Tomazini, Maia, Cavalcanti, Berwanger, Rosa et al., Effect of Dexamethasone on Days Alive and Ventilator-Free in Patients With Moderate or Severe Acute Respiratory Distress Syndrome and COVID-19: The CoDEX Randomized Clinical Trial, JAMA
Torres, Niederman, Chastre, Ewig, Fernandez-Vandellos et al., International ERS/ESICM/ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia: Guidelines for the management of hospital-acquired pneumonia (HAP)/ventilator-associated pneumonia (VAP) of the, Eur Respir J, doi:10.1183/13993003.00582-2017
Torres, Niederman, Chastre, International ERS/ESICM/ ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia: Guidelines for the management of hospital-acquired pneumonia (HAP)/ventilatorassociated pneumonia (VAP) of the, European Society of Intensive Care Medicine (ESICM)
Trieu, Vasculotide, an Angiopoietin-1 Mimetic, Restores Microcirculatory Perfusion and Microvascular Leakage and Decreases Fluid Resuscitation Requirements in Hemorrhagic Shock, Anesthesiology, doi:10.1097/ALN.0000000000001907
Tsay, Pinkhas, Do, Lee, Guo et al., Worsening Renal Function in Cardiac Mechanical Support, Heart, Lung and Circulation
Turbil, Galerneau, Terzi, Schwebel, Argaud et al., Positiveend expiratory pressure titration and transpulmonary pressure: the EPVENT 2 trial, J Thorac Dis
Uab, Sabadell, Spain, Rehabilitation medicine
Ugalde, Medel, Nicolás, Romero, Cornejo, Transthoracic cardiac ultrasound in prone position: a technique variation description, Intensive Care Medicine
Van Leeuwen, In vitro endothelial hyperpermeability occurs early following traumatic hemorrhagic shock, Clin Hemorheol Microcirc, doi:10.3233/CH-190642
Van Mol, Developing and testing a nurse-led intervention to support bereavement in relatives in the intensive care (BRIC study): a protocol of a pre-post intervention study
Varga, Flammer, Steiger, Haberecker, Andermatt et al., Endothelial cell infection and endotheliitis in COVID-19, Lancet
Vega, Gordo, Tascón, Vélez, Pneumomediastinum et al., Spontaneous pneumomediastinum, pneumothorax and subcutaneous emphysema in COVID-19 pneumonia: a rare case and literature review, Clin Imaging, doi:10.12659/AJCR.925557
Vernon, Van Heerden 10 ; W. Szczeklik 11, J. Wollborn
Vieira, De Oliveira, Da, Mendonça, Should oral chlorhexidine remain in ventilator-associated pneumonia prevention bundles? Med Intensiva, doi:10.1016/j.medin.2020.09.009
Viejo, None, N. Arriero Fernández 1 ; B. Mariblanca-Nieves
Villar, Blanco, Añón, Santos-Bouza, Blanch et al., The ALIEN study: incidence and outcome of acute respiratory distress syndrome in the era of lung protective ventilation, Intensive Care Medicine
Villar, Zhang, Slutsky, Lung Repair and Regeneration in ARDS, Chest
Vincent, Moreno, Takala, Willatts, Mendonca et al., The SOFA (Sepsis -related Journal Pre-proof Journal Pre-proof Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis -Related Problems of the European Society of Intensive Care Medicine, Intensive Care Med, doi:10.1007/BF01709751
Vincent, Sakr, Singer, Prevalence and outcomes of infection among patients in intensive care units in 2017, JAMA
Vincent, The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine, Intensive Care Med
Vincent, The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine, Intensive Care Med
Vitale, Perazzo, Silingardi, Biffi, Banfi et al., Is disruption of sleep quality a consequence of severe Covid-19 infection? A case-series examination, Chronobiol Int, doi:10.1080/07420528.2020.1775241
Volpi, Ali, Pneumomediastinum in COVID-19 patients: a case series of a rare complication, European Journal of Cardio-Thoracic Surgery, doi:10.1093/ejcts/ezaa222
Wahlster, Sharma, Lewis, Patel, Hartog et al., The Coronavirus Disease 2019 Pandemic's Effect on Critical Care Resources and Health-Care Providers: A Global Survey, Chest, doi:10.1016/j.chest.2020.09.070
Wald, Casey-Gillman, Comer, Mansell, Teo et al., Animation-supported consent for urgent angiography and angioplasty: a service improvement initiative, Heart
Wali, Rizzo, Pneumomediastinum following intubation in COVID-19 patients: a case series. Anaesthesia, Peri-operative medicine, critical care and pain, doi:10.1111/anae.15113
Wang, Gao, Zheng, Jiang, COVID-19 with spontaneous pneumothorax, pneumomediastinum and subcutaneous emphysema, J Travel Med, doi:10.1093/jtm/taaa062
Wang, Hu, Hu, Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China, JAMA, doi:10.1001/jama.2020.1585
Wang, Hu, Hu, Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, JAMA
Wang, Jiang, Zhu, Wen, Xi, Fluid balance and mortality in critically ill patients with acute kidney injury: a multicenter prospective epidemiological study, Crit Care
Wang, Su, Zhang, Zheng, Spontaneous Pneumomediastinum: A Probable Unusual Complication of Coronavirus Disease
Wang, Zhang, Yu, Tao, Xie et al., Outcomes of Patients With Coronavirus Disease 2019 Receiving Organ Support Therapies: The International Viral Infection and Respiratory Illness Universal Study Registry, Intensive Care Med, doi:10.1097/CCM.0000000000004879
Webb, Clinical criteria for COVID-19-associated hyperinflammatory syndrome: a cohort study, Lancet Rheumatol
Weir, Steyerberg, Butcher, Lu, Lingsma et al., Does the extended Glasgow Outcome Scale add value to the conventional Glasgow Outcome Scale?, Journal of Neurotrauma, doi:10.1089/neu.2011.2137
Weiss, Cerda, Scott, Kaur, Sungurlu et al., Prone positioning for patients intubated for severe acute respiratory distress syndrome (ARDS) secondary to COVID-19: a retrospective observational cohort study, British Journal of Anaesthesia. 1 de enero de
Weiss, Cerda, Scott, Kaur, Sungurlu et al., Prone positioning for patients intubated for severe acute respiratory distress syndrome (ARDS) secondary to COVID-19: a retrospective observational cohort study, British journal of anaesthesia, doi:10.1016/j.bja.2020.09.042
Westafer, Soares We 3rd, Salvador, Medarametla, Schoenfeld, No evidence of increasing COVID-19 in health care workers after implementation of high flow nasal cannula: A safety evaluation, Am J Emerg Med, doi:10.1016/j.ajem.2020.09.086
Whittle, Molinger, Macleod, Haines, Wischmeyer, Persistent hypermetabolism and longitudinal energy expenditure in critically ill patients with COVID-19, Crit Care
Wichmann, Barbateskovic, Lindschou, Gluud, Perner et al., Loop diuretics in adult intensive care patients with fluid overload: A protocol for a systematic review of randomised clinical trials with meta-analysis and Trial Sequential Analysis, Acta Anaesthesiol Scand
Wihersaari, Tiainen, Skrifvars, Bendel, Kaukonen et al., Finnresusci study group. Usefulness of neuron specific enolase in prognostication after cardiac arrest: Impact of age and time to ROSC, Resuscitation
Wildenthal, Mierzwiak, Myers, Mitchell, Effects of acute lactic acidosis on left ventricular performance, Am J Physiol
Winck, Ambrosino, COVID-19 pandemic and non invasive respiratory management: Every Goliath needs a David. An evidence based evaluation of problems, Pulmonology, doi:10.1016/j.pulmoe.2020.04.013
Winters, Weaver, Pfoh, Yang, Pham et al., Rapid-response systems as a patient safety strategy: a systematic review, Ann Intern Med
Wise, 14 ; H. Zetterberg, 15 ; T. Cronberg 16 ; M. Moseby-Knappe
Woodfin, Voisin, Nourshargh, PECAM-1: A Multi-Functional Molecule in Inflammation and Vascular Biology, Arterioscler Thromb Vasc Biol
Workalert, None
Wu, Discovery of Long-Latency Somatosensory Evoked Potentials as a Marker of Cardiac Arrest Induced Brain Injury, IFMBE Proceedings
Wu, Lopez, None
Xiong, Redwood, Prendergast, Chen, Coronaviruses and the cardiovascular system: acute and long-term implications, Eur Heart J, doi:10.1093/eurheartj/ehaa231
Xirouchaki, Magkanas, Vaporidi, Kondili, Plataki et al., Lung ultrasound in critically ill patients: Comparison with bedside chest radiography, Intensive Care Med, doi:10.1007/s00134-011-2317-y
Xu, Yang, Huang, Zou, Zhou et al., A Novel Risk-Stratification Models of the High-Flow Nasal Cannula Therapy in COVID-19 Patients With Hypoxemic Respiratory Failure, Frontiers in Medicine
Yamamoto, Doi, Hayase, Pulse oximetry-based capillary refilling evaluation predicts postoperative outcomes in liver transplantation: a prospective observational cohort study, BMC Anesthesiol
Yang, Tian, Guo, Acute kidney injury and renal replacement therapy in COVID-19 patients: A systematic review and meta-analysis, Int Immunopharmacol, doi:10.1016/j.intimp.2020.107159
Yang, Yu, Xu, Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a singlecentered, retrospective, observational study, Lancet Respir Med
Yang, Yu, Xu, Shu, Xia et al., Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study, Lancet Respir Med, doi:10.1016/S2213-2600(20)30079-5
Yang, Yu, Xu, Shu, Xia et al., Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study, Lancet Respir Med, doi:10.1111/imj.14398
Yatim, Mercatello, Coronel, Bret, Colpart et al., 99mTc-HMPAO cerebral scintigraphy in the diagnosis of brain death
Yoon, Jeanselme, Dubrawski, Hravnak, Pinsky et al., Prediction of Hypotension Events with Physiologic Vital Sign Signatures in The Intensive Care Unit, Critical Care
Yu, Cassiere, Derosa, Bocchieri, Yar et al., Hypermetabolism and Coronavirus Disease, JPEN J Parenter Enteral Nutr
Zaim, Chong, Sankaranarayanan, Harky, COVID-19 and Multiorgan Response, Curr Probl Cardiol, doi:10.1016/j.cpcardiol.2020.100618
Zenati, Billiar, Townsend, Peitzman, Harbrecht, A brief episode of hypotension increases mortality in critically ill trauma patients, J Trauma
Zhao, Wu, Shiu-Xiang, Serum albumin is a predictor for duration of weaning in patients with traumatic brain injury, Int J. Clin Exp Med
Zhi, Xin, Ying, Guohong, Shuying, Obesity Paradox" in Acute Respiratory Distress Syndrome: Asystematic Review and Meta-Analysis, PLoS One
Zhou, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
Zhou, Lv, Wang, Yang, Liang et al., Early application of airway pressure release ventilation may reduce the duration of mechanical ventilation in acute respiratory distress syndrome. Intensive care medicine
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, The lancet
Zhu, A novel coronavirus from patients with pneumonia in China, N Engl J Med
Zhu, Zhang, Wang, A novel coronavirus from patients with pneumonia in China, N Engl J Med
Zile, Bennett, Sutton, Cho, Adamson et al., Transition from chronic compensated to acute decompensated heart failure. Pathophysiological insights obtained from continuous monitoring of intracardiac pressures, Circulation
Zuercher, Moret, Dziewas, Schefold, Dysphagia in the intensive care unit: epidemiology, mechanisms, and clinical management, Crit Care, doi:10.1186/s13054-019-2400-2
Zuercher, Moret, Schefold, Dysphagia in the intensive care unit in Switzerland (DICE)-results of a national survey on the current standard of care, Swiss Med Wkly, doi:10.4414/smw.2019.20111
Zuo, Huang, Ma, Xue, Zhang et al., Chinese Society of Anesthesiology Task Force on Airway Management, Airway Management Chinese Society of Anesthesiology Task Force on. Expert Recommendations for Tracheal Intubation in Critically ill Patients with Noval Coronavirus Disease, Chin Med Sci J, doi:10.24920/003724
Zuo, Huang, Ma, Xue, Zhang et al., Expert recommendations for tracheal intubation in critically iii patients with novel coronavirus disease, Chin Med Sci J
Zusman, Theilla, Cohen, Kagan, Bendavid et al., Resting energy expenditure, calorie and protein consumption in critically ill patients: a retrospective cohort study, Crit Care Lond Engl, doi:10.1186/s13054-016-1538-4
DOI record:
{
"DOI": "10.1186/s40635-021-00413-8",
"ISSN": [
"2197-425X"
],
"URL": "http://dx.doi.org/10.1186/s40635-021-00413-8",
"alternative-id": [
"413"
],
"article-number": "51",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 1,
"value": "29 September 2021"
}
],
"container-title": [
"Intensive Care Medicine Experimental"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2021,
10,
11
]
],
"date-time": "2021-10-11T11:03:05Z",
"timestamp": 1633950185000
},
"deposited": {
"date-parts": [
[
2021,
10,
11
]
],
"date-time": "2021-10-11T11:13:12Z",
"timestamp": 1633950792000
},
"indexed": {
"date-parts": [
[
2022,
1,
3
]
],
"date-time": "2022-01-03T18:26:47Z",
"timestamp": 1641234407038
},
"is-referenced-by-count": 3,
"issn-type": [
{
"type": "electronic",
"value": "2197-425X"
}
],
"issue": "S1",
"issued": {
"date-parts": [
[
2021,
9,
29
]
]
},
"journal-issue": {
"issue": "S1",
"published-print": {
"date-parts": [
[
2021,
10
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1186/s40635-021-00413-8.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1186",
"published": {
"date-parts": [
[
2021,
9,
29
]
]
},
"published-online": {
"date-parts": [
[
2021,
9,
29
]
]
},
"published-print": {
"date-parts": [
[
2021,
10
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference-count": 0,
"references-count": 0,
"relation": {},
"score": 1,
"short-container-title": [
"ICMx"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Critical Care and Intensive Care Medicine"
],
"subtitle": [],
"title": [
"ESICM LIVES 2021: Part 1"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "9"
}