Incidence and Risk of Post-COVID-19 Thromboembolic Disease and the Impact of Aspirin Prescription; Nationwide Observational Cohort at the US Department of Veteran Affairs.
et al., medRxiv, doi:10.1101/2024.04.10.24305647, Apr 2024
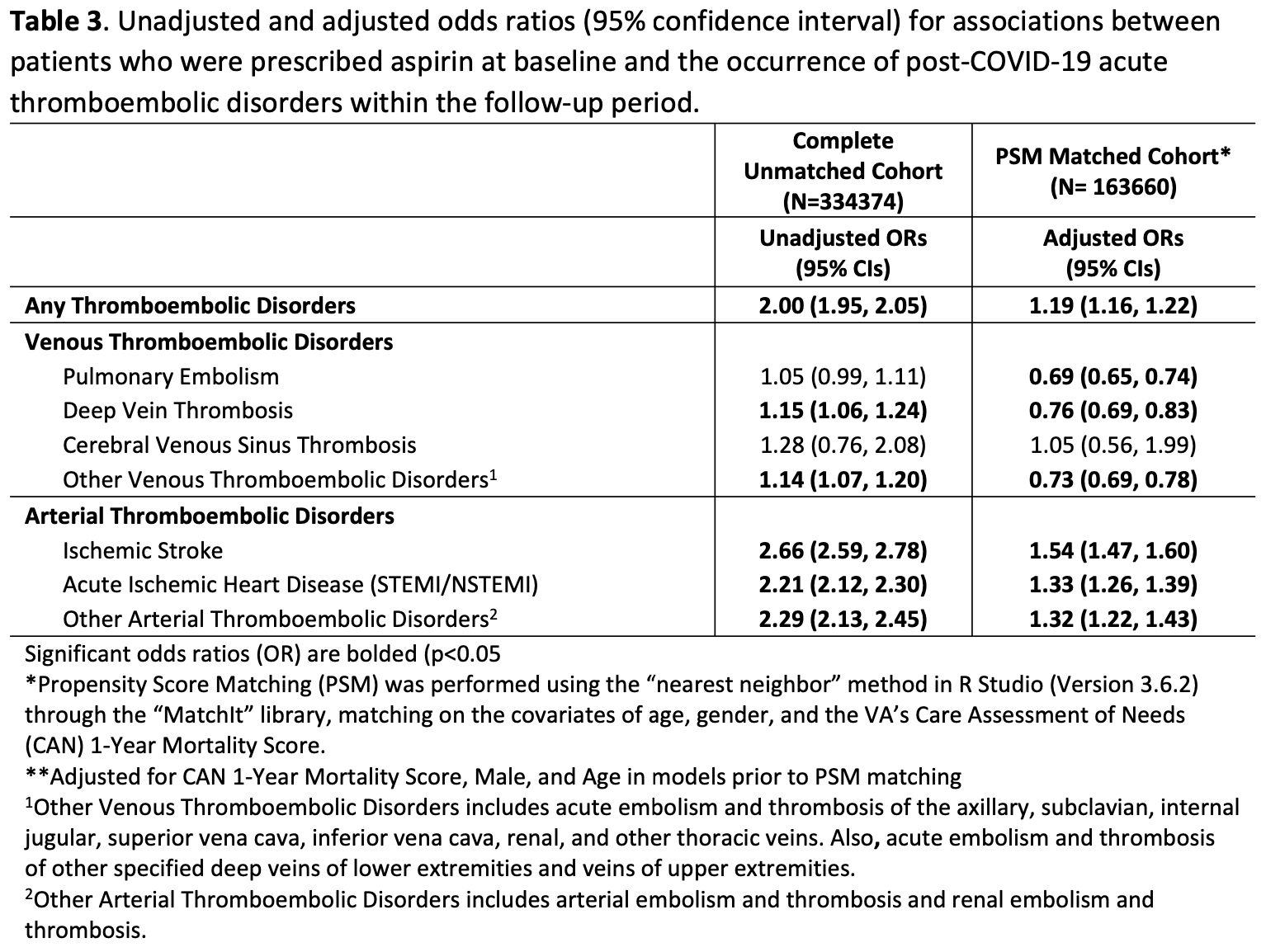
PSM retrospective 334,374 COVID-19 patients showing decreased risk of venous thromboembolism, including pulmonary embolism and deep vein thrombosis, but increased risk of arterial thromboembolic disorders, including ischemic stroke and acute ischemic heart disease, with aspirin use prior to COVID-19 diagnosis. The increased risk of arterial disease may be associated with preexisting cardiovascular disease for which aspirin was already prescribed. All cause mortality was lower in the aspirin group, however authors do not discuss this result.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 45.8% lower, RR 0.54, p = 0.001, treatment 7,531 of 81,830 (9.2%), control 13,890 of 81,830 (17.0%), NNT 13, propensity score matching, day 365.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ware et al., 12 Apr 2024, retrospective, propensity score matching, USA, preprint, 7 authors, study period 2 March, 2020 - 13 June, 2022.
Contact: anna.ware@va.gov.
Incidence and Risk of Post-COVID-19 Thromboembolic Disease and the Impact of Aspirin Prescription; Nationwide Observational Cohort at the US Department of Veteran Affairs.
doi:10.1101/2024.04.10.24305647
Introduction: COVID-19 triggers prothrombotic and proinflammatory changes, with thrombotic disease prevalent in up to 30% SARS-CoV-2 infected patients. Early work suggests that aspirin could prevent COVID-19 related thromboembolic disorders in some studies but not others. This study leverages data from the largest integrated healthcare system in the United States to better understand this association. Our objective was to evaluate the incidence and risk of COVID-19 associated acute thromboembolic disorders and the potential impact of aspirin.
Methods: This retrospective, observational study utilized national electronic health record data from the Veterans Health Administration. 334,374 Veterans who tested positive for COVID-19 from March 2, 2020, to June 13, 2022, were included, 81,830 of whom had preexisting aspirin prescription prior to their COVID-19 diagnosis. Patients with and without aspirin prescriptions were matched and the odds of post-COVID acute thromboembolic disorders were assessed. Results: 10.1% of Veterans had a documented thromboembolic disorder within 12 months following their COVID-19 diagnosis. Those with specific comorbidities were at greatest risk. Preexisting aspirin prescription was associated with a significant decrease risk of post-COVID-19 thromboembolic disorders, including pulmonary embolism (OR [95% CI]: 0.69 [0.65, 0.74]) and deep vein thrombosis (OR [95% CI]: 0.76 [0.69, 0.83], but an increased risk of acute arterial diseases, including ischemic stroke (OR [95% CI]: 1.54 [1.46, 1.60]) and acute ischemic heart disease (1.33 [1.26, 1.39]). Conclusions: Findings demonstrated that preexisting aspirin prescription prior to COVID-19 diagnosis was associated with significantly decreased risk of venous thromboembolism and pulmonary embolism but increased risk of acute arterial disease. The risk of arterial disease may be associated with increased COVID-19 prothrombotic effects superimposed on preexisting chronic cardiovascular disease for which aspirin was already prescribed. Prospective clinical trials may help to further assess the efficacy of aspirin use prior to COVID-19 diagnosis for the prevention of post-COVID-19 thromboembolic disorders.
References
Abdi, Lamardi, Shirjan, Mohammadi, Abadi et al., The Effect of Aspirin on the Prevention of Pro-thrombotic States in Hospitalized COVID-19 Patients: Systematic Review, Cardiovasc Hematol Agents Med Chem, doi:10.2174/1871525720666220401102728
Albandar, Markert, Agrawal, The relationship between aspirin use and mortality in colorectal cancer, Journal of Gastrointestinal Oncology
Barnes, Burnett, Allen, Ansell, Blumenstein et al., Thromboembolic prevention and anticoagulant therapy during the COVID-19 pandemic: updated clinical guidance from the anticoagulation forum, J Thromb Thrombolysis, doi:10.1007/s11239-022-02643-3
Bhatt, Jr, The Future of Aspirin Therapy in Cardiovascular Disease, The American Journal of Cardiology
Chuang, Tsai, Liu, Wu, Liu, COVID-19 in Veterans: A Narrative Review, Risk Manag Healthc Policy, doi:10.2147/RMHP.S354814
Cui, Chen, Li, Liu, Wang, Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia, J Thromb Haemost, doi:10.1111/jth.14830
Cushman, Epidemiology and risk factors for venous thrombosis, Semin Hematol, doi:10.1053/j.seminhematol.2007.02.004
Dev, Gonzalez, Coffing, Slaven, Dev et al., Validating administratively derived frailty scores for use in Veterans Health Administration emergency departments, Acad Emerg Med, doi:10.1111/acem.14705
Finh, Box, Care Assessment Need (CAN) Score and the Patient Care Assessment System (PCAS): Tools for Care Management
Greifer, MatchIt: Getting started
Harthi, Aljuhani, Korayem, Altebainawi, Alenezi et al., Evaluation of Low-Dose Aspirin use among Critically Ill Patients with COVID-19: A Multicenter Propensity Score Matched Study, J Intensive Care Med, doi:10.1177/08850666221093229
Klok, Kruip, Van Der Meer, Arbous, Gommers et al., Incidence of thrombotic complications in critically ill ICU patients with COVID-19, Thromb Res, doi:10.1016/j.thromres.2020.04.013
Lodigiani, Iapichino, Carenzo, Cecconi, Ferrazzi et al., Humanitas COVID-19 Task Force. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy, Thromb Res, doi:10.1016/j.thromres.2020.04.024
Ma, Su, Sun, Does aspirin have an effect on risk of death in patients with COVID-19? A metaanalysis, Eur J Clin Pharmacol, doi:10.1007/s00228-022-03356-5
Meizlish, Goshua, Liu, Fine, Amin et al., Intermediate-dose anticoagulation, aspirin, and in-hospital mortality in COVID-19: A propensity score-matched analysis, Am J Hematol, doi:10.1002/ajh.26102
Middeldorp, Coppens, Van Haaps, Tf, Incidence of venous thromboembolism in hospitalized patients with COVID-19, J Thromb Haemost, doi:10.1111/jth.14888
Ochani, Asad, Yasmin, Shaikh, Khalid et al., COVID-19 pandemic: from origins to outcomes. A comprehensive review of viral pathogenesis, clinical manifestations, diagnostic evaluation, and management, Infez Med
Osborne, Veigulis, Arreola, Mahajan, Röösli et al., Association of mortality and aspirin prescription for COVID-19 patients at the Veterans Health Administration, PLoS One, doi:10.1371/journal.pone.0246825
Osborne, Veigulis, Arreola, Röösli, Curtin, Automated EHR score to predict COVID-19 outcomes at US Department of Veterans Affairs, Plos One
Piazza, Campia, Hurwitz, Registry of Arterial and Venous Thromboembolic Complications in Patients With COVID-19, J Am Coll Cardiol, doi:.org/10.1016/j.jacc.2020.08.070
Raman, Bluemke, Lüscher, Neubauer, Long COVID: post-acute sequelae of COVID-19 with a cardiovascular focus, Eur Heart J, doi:10.1093/eurheartj/ehac031
Restrepo, Marin-Corral, Rodriguez, Restrepo, Cavallazzi, Cardiovascular Complications in Coronavirus Disease 2019-Pathogenesis and Management, Semin Respir Crit Care Med, doi:10.1055/s-0042-1760096
Violi, Cammisotto, Pignatelli, Thrombosis in Covid-19 and non-Covid-19 pneumonia: role of platelets, Platelets, doi:10.1080/09537104.2021.1936478
Violi, Cammisotto, Pignatelli, Thrombosis in Covid-19 and non-Covid-19 pneumonia: role of platelets, Platelets, doi:10.1080/09537104.2021.1936478
Wang, Dhanireddy, Prince, Larsen, Schimpf et al., Main results report, prepared for Strategic Analysis Service
Wichmann, Sperhake, Lütgehetmann, Steurer, Edler, Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study, Ann Intern Med, doi:10.7326/M20-2003
Wu, Zuo, Yang, Luo, Jiang et al., Venous Thromboembolic Events in Patients with COVID-19: A Systematic Review and Meta-Analysis, Age Ageing, doi:10.1093/ageing/afaa259
Xie, Xu, Bowe, Long-term cardiovascular outcomes of COVID-19, Nat Med, doi:10.1038/s41591-022-01689-3
Zareef, Diab, Saleh, Makarem, Younis et al., Aspirin in COVID-19: Pros and Cons, Front Pharmacol, doi:10.3389/fphar.2022.849628
DOI record:
{
"DOI": "10.1101/2024.04.10.24305647",
"URL": "http://dx.doi.org/10.1101/2024.04.10.24305647",
"abstract": "<jats:p>Introduction: COVID-19 triggers prothrombotic and proinflammatory changes, with thrombotic disease prevalent in up to 30% SARS-CoV-2 infected patients. Early work suggests that aspirin could prevent COVID-19 related thromboembolic disorders in some studies but not others. This study leverages data from the largest integrated healthcare system in the United States to better understand this association. Our objective was to evaluate the incidence and risk of COVID-19 associated acute thromboembolic disorders and the potential impact of aspirin. Methods: This retrospective, observational study utilized national electronic health record data from the Veterans Health Administration. 334,374 Veterans who tested positive for COVID-19 from March 2, 2020, to June 13, 2022, were included, 81,830 of whom had preexisting aspirin prescription prior to their COVID-19 diagnosis. Patients with and without aspirin prescriptions were matched and the odds of post-COVID acute thromboembolic disorders were assessed. Results: 10.1% of Veterans had a documented thromboembolic disorder within 12 months following their COVID-19 diagnosis. Those with specific comorbidities were at greatest risk. Preexisting aspirin prescription was associated with a significant decrease risk of post-COVID-19 thromboembolic disorders, including pulmonary embolism (OR [95% CI]: 0.69 [0.65, 0.74]) and deep vein thrombosis (OR [95% CI]: 0.76 [0.69, 0.83], but an increased risk of acute arterial diseases, including ischemic stroke (OR [95% CI]: 1.54 [1.46, 1.60]) and acute ischemic heart disease (1.33 [1.26, 1.39]). Conclusions: Findings demonstrated that preexisting aspirin prescription prior to COVID-19 diagnosis was associated with significantly decreased risk of venous thromboembolism and pulmonary embolism but increased risk of acute arterial disease. The risk of arterial disease may be associated with increased COVID-19 prothrombotic effects superimposed on preexisting chronic cardiovascular disease for which aspirin was already prescribed. Prospective clinical trials may help to further assess the efficacy of aspirin use prior to COVID-19 diagnosis for the prevention of post-COVID-19 thromboembolic disorders.</jats:p>",
"accepted": {
"date-parts": [
[
2024,
4,
12
]
]
},
"author": [
{
"ORCID": "http://orcid.org/0000-0003-3333-7833",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ware",
"given": "Anna",
"sequence": "first"
},
{
"affiliation": [],
"family": "Veigulis",
"given": "Zachary P",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hoover",
"given": "Peter J",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Blumke",
"given": "Terri",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ioannou",
"given": "George N",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3695-192X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Boyko",
"given": "Edward J",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Osborne",
"given": "Thomas",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
4,
13
]
],
"date-time": "2024-04-13T03:50:10Z",
"timestamp": 1712980210000
},
"deposited": {
"date-parts": [
[
2024,
4,
13
]
],
"date-time": "2024-04-13T03:50:10Z",
"timestamp": 1712980210000
},
"group-title": "Infectious Diseases (except HIV/AIDS)",
"indexed": {
"date-parts": [
[
2024,
4,
13
]
],
"date-time": "2024-04-13T04:10:35Z",
"timestamp": 1712981435147
},
"institution": [
{
"name": "medRxiv"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
4,
12
]
]
},
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2024.04.10.24305647",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2024,
4,
12
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2024,
4,
12
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "http://medrxiv.org/lookup/doi/10.1101/2024.04.10.24305647"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "Incidence and Risk of Post-COVID-19 Thromboembolic Disease and the Impact of Aspirin Prescription; Nationwide Observational Cohort at the US Department of Veteran Affairs.",
"type": "posted-content"
}