Inflammatory-Metal Profile as a Hallmark for COVID-19 Severity During Pregnancy
et al., Frontiers in Cell and Developmental Biology, doi:10.3389/fcell.2022.935363, Aug 2022
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000019 from 42 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
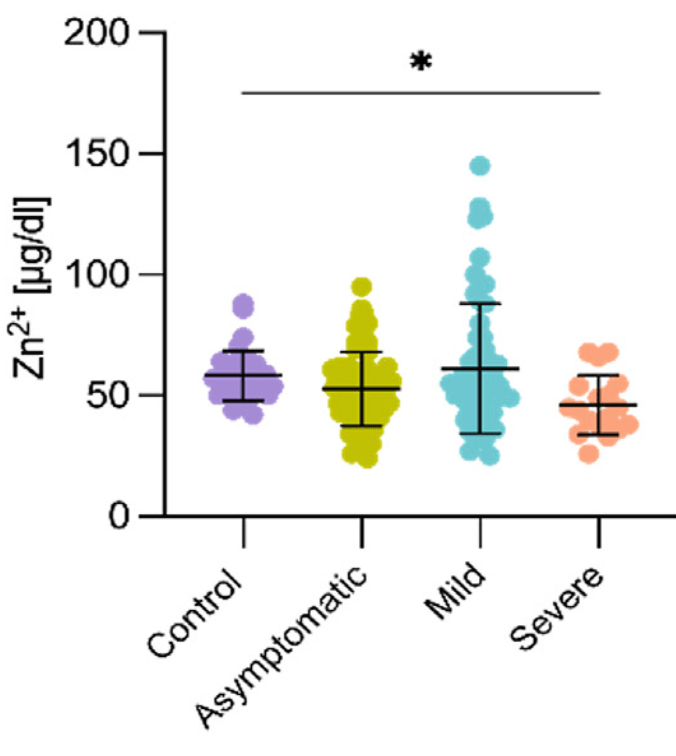
Prospective study of 163 COVID+ and 34 COVID- pregnant women in Mexico, showing significantly lower zinc levels in patients with severe COVID-19.
Vásquez-Procopio et al., 9 Aug 2022, prospective, Mexico, peer-reviewed, 15 authors, study period July 2020 - March 2021.
Contact: gpestrad@gmail.com.
Inflammatory-Metal Profile as a Hallmark for COVID-19 Severity During Pregnancy
Frontiers in Cell and Developmental Biology, doi:10.3389/fcell.2022.935363
Pregnancy makes women more susceptible to infectious agents; however, available data on the effect of SARS-CoV-2 on pregnant women are limited. To date, inflammatory responses and changes in serum metal concentration have been reported in COVID-19 patients, but few associations between metal ions and cytokines have been described. The aim of this study was to evaluate correlations between inflammatory markers and serum metal ions in third-trimester pregnant women with varying COVID-19 disease severity. Patients with severe symptoms had increased concentrations of serum magnesium, copper, and calcium ions and decreased concentrations of iron, zinc, and sodium ions. Potassium ions were unaffected. Pro-inflammatory cytokines IL-6, TNF-α, IL-8, IL-1α, anti-inflammatory cytokine IL-4, and the IP-10 chemokine were induced in the severe presentation of COVID-19 during pregnancy. Robust negative correlations between iron/magnesium and zinc/IL-6, and a positive correlation between copper/IP-10 were observed in pregnant women with the severe form of the disease. Thus, coordinated alterations of serum metal ions and inflammatory markerssuggestive of underlying pathophysiological interactions-occur during SARS-CoV-2 infection in pregnancy.
ETHICS STATEMENT The studies involving human participants were reviewed and approved by the study was IRB of the National Institute of Perinatology, (Registration number 2020-1-32), and Hospital General de México Dr. Eduardo Liceaga (DI/20/112/03/33). The patients/participants provided their written informed consent to participate in this study.
AUTHOR CONTRIBUTIONS JV-P, FM, and GE-G designed the research. JV-P, AE-N, and MT-D conducted the measurements. JV-P, PM-R, JT-T, SE,
SUPPLEMENTARY MATERIAL The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcell.2022.935363/ full#supplementary-material Conflict of Interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. Publisher's Note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abrao Trad, Ibirogba, Elrefaei, Narang, Tonni et al., Complications and Outcomes of SARS-CoV-2 in Pregnancy: where and what Is the Evidence?, Hypertens. Pregnancy, doi:10.1080/10641955.2020.1769645
Adhikari, Moreno, Zofkie, Macdonald, Mcintire et al., Pregnancy Outcomes Among Women with and without Severe Acute Respiratory Syndrome Coronavirus 2 Infection, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2020.29256
Anderson, Shah, Iron Homeostasis in the Liver, Compr. Physiol, doi:10.1002/cphy.c120016
Anuk, Polat, Akdas, Erol, Tanacan et al., The Relation Between Trace Element Status (Zinc, Copper, Magnesium) and Clinical Outcomes in COVID-19 Infection During Pregnancy, Biol. Trace Elem. Res, doi:10.1007/s12011-020-02496-y
Azem, Daou, Bassil, Anvari, Taliercio et al., Serum Magnesium, Mortality and Disease Progression in Chronic Kidney Disease, BMC Nephrol, doi:10.1186/s12882-020-1713-3
Becker, Skaar, Metal Limitation and Toxicity at the Interface between Host and Pathogen, FEMS Microbiol. Rev, doi:10.1111/1574-6976.12087
Ben Moftah, Eswayah, Intricate Relationship between SARS-CoV-2-Induced Shedding and Cytokine Storm Generation: A Signaling Inflammatory Pathway Augmenting COVID-19, Health Sci. Rev, doi:10.1016/j.hsr.2021.100011
Cappellini, Comin-Colet, De Francisco, Dignass, Doehner et al., Iron Deficiency across Chronic Inflammatory Conditions: International Expert Opinion on Definition, Diagnosis, and Management, Am. J. Hematol, doi:10.1002/ajh.24820
Cardona-Pérez, Villegas-Mota, Helguera-Repetto, Acevedo-Gallegos, Rodríguez-Bosch et al., Prevalence, Clinical Features, and Outcomes of SARS-CoV-2 Infection in Pregnant Women with or without Mild/moderate Symptoms: Results from Universal Screening in a Tertiary Care Center in Mexico City, Mexico, PLoS One, doi:10.1371/journal.pone.0249584
Castro-Leyva, Espejel-Nuñez, Barroso, Zaga-Clavellina, Flores-Pliego et al., Preserved Ex Vivo Inflammatory Status in Decidual Cells from Women with Preterm Labor and Subclinical Intrauterine Infection, PLoS One, doi:10.1371/journal.pone.0043605
Chasapis, Interactions between Metal Binding Viral Proteins and Human Targets as Revealed by Network-Based Bioinformatics, J. Inorg. Biochem, doi:10.1016/j.jinorgbio.2018.06.012
Chen, Jiang, Shi, Peng, Fan et al., The Molecular Mechanisms of Copper Metabolism and its Roles in Human Diseases, Pflugers Arch. -Eur. J. Physiol, doi:10.1007/s00424-020-02412-2
Chen, Liao, Ai, Yang, Bai et al., Immune Response to COVID-19 During Pregnancy, Front. Immunol, doi:10.3389/fimmu.2021.675476
Chen, Wu, Guo, Cao, Huang et al., Clinical and Immunological Features of Severe and Moderate Coronavirus Disease 2019, J. Clin. Invest, doi:10.1172/jci137244
Chen, Zhang, Zhang, Ai, Yang et al., Differential Immune Responses in Pregnant Patients Recovered from COVID-19, Sig Transduct. Target Ther, doi:10.1038/s41392-021-00703-3
Chen, Zhou, Dong, Qu, Gong et al., Epidemiological and Clinical Characteristics of 99 Cases of 2019 Novel Coronavirus Pneumonia in Wuhan, China: a Descriptive Study, Lancet, doi:10.1016/s0140-6736(20)30211-7
Copyright, Vásquez-Procopio, Espejel-Nuñez, Torres-Torres, Martinez-Portilla et al., This is an open-access article distributed under the terms of the Creative Commons Attribution License
Cornish, Filipovic, Åsenius, Williams, Mcdonnell, Innate Immune Responses to Acute Viral Infection During Pregnancy, Front. Immunol, doi:10.3389/fimmu.2020.572567
De, De Araújo Andrade, Understanding the Relationship between Viral Infections and Trace Elements from a Metallomics Perspective: Implications for COVID-19, Metallomics, doi:10.1039/d0mt00220h
Dharmalingam, Birdi, Tomo, Sreenivasulu, Charan et al., Trace Elements as Immunoregulators in SARS-CoV-2 and Other Viral Infections, Ind. J. Clin. Biochem, doi:10.1007/s12291-021-00961-6
Fisher, Nemeth, Iron Homeostasis during Pregnancy, Am. J. Clin. Nutr, doi:10.3945/ajcn.117.155812
Flores-Quijano, Vega-Sánchez, Tolentino-Dolores, López-Alarcón, Flores-Urrutia et al., Obesity Is Associated with Changes in Iron Nutrition Status and its Homeostatic Regulation in Pregnancy, Nutrients, doi:10.3390/nu11030693
Fooladi, Matin, Mahmoodpoor, Copper as a Potential Adjunct Therapy for Critically Ill COVID-19 Patients, Clin. Nutr. ESPEN, doi:10.1016/j.clnesp.2020.09.022
Foster, Samman, Zinc and Regulation of Inflammatory Cytokines: Implications for Cardiometabolic Disease, Nutrients, doi:10.3390/nu4070676
Frontera, Valdes, Huang, Lewis, Lord et al., Prevalence and Impact of Hyponatremia in Patients with Coronavirus Disease 2019 in New York City, Crit. Care Med, doi:10.1097/ccm.0000000000004605
Frost, Tan, Abbas, Wideman, Bonadonna et al., Hepcidin-Mediated Hypoferremia Disrupts Immune Responses to Vaccination and Infection, Med, doi:10.1016/j.medj.2020.10.004
Gambling, Mcardle, Iron, Copper and Fetal Development, Proc. Nutr. Soc, doi:10.1079/pns2004385
Gandhi, Lynch, Del Rio, Mild or Moderate Covid-19, N. Engl. J. Med, doi:10.1056/nejmcp2009249
Garay, Schuth, Barbanente, Tejeda-Guzmán, Vitone et al., Tryptophan Regulates Drosophila Zinc Stores, Proc. Natl. Acad. Sci. U. S. A, doi:10.1073/pnas.2117807119
Garcia-Flores, Romero, Xu, Theis, Arenas-Hernandez et al., Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 -COVID-NET, 14, MMWR Morb. Mortal. Wkly. Rep, doi:10.15585/mmwr.mm6915e3
Girelli, Marchi, Busti, Vianello, Iron Metabolism in Infections: Focus on COVID-19, Seminars Hematol, doi:10.1053/j.seminhematol.2021.07.001
Goldstein, Gallagher, Beck, Kumar, Gernand, Maternal-Fetal Inflammation in the Placenta and the Developmental Origins of Health and Disease, Front. Immunol, doi:10.3389/fimmu.2020.531543
Gonçalves, Gonçalves, Guarnieri, Risegato, Guimarães et al., Association Between Low Zinc Levels and Severity of Acute Respiratory Distress Syndrome by New Coronavirus SARS-CoV-2, Nutr. Clin. Pract, doi:10.1002/ncp.10612
Goulle, Saussereau, Mahieu, Bouige, Groenwont et al., Application of Inductively Coupled Plasma Mass Spectrometry Multielement Analysis in Fingernail and Toenail as a Biomarker of Metal Exposure, J. Anal. Toxicol, doi:10.1093/jat/33.2.92
Grzeszczak, Kwiatkowski, Kosik-Bogacka, The Role of Fe, Zn, and Cu in Pregnancy, Biomolecules, doi:10.3390/biom10081176
Guan, -J, Liang, Zhao, Liang et al., Comorbidity and its Impact on 1590 Patients with COVID-19 in China: a Nationwide Analysis, Eur. Respir. J, doi:10.1183/13993003.00547-2020
Hackler, Heller, Sun, Schwarzer, Diegmann et al., Relation of Serum Copper Status to Survival in COVID-19, Nutrients, doi:10.3390/nu13061898
Hafizi, Mardani, Borhani, Ahmadi, Nasri et al., Association of helicobacter Pylori Infection with Serum Magnesium in Kidney Transplant Patients, J. Ren. Inj. Prev, doi:10.12861/jrip.2014.29
Hippchen, Altamura, Muckenthaler, Hypoferremia Is Associated with Increased Hospitalization and Oxygen Demand in COVID-19 Patients, Hemasphere, doi:10.1097/hs9.0000000000000492
Hirano, Murakami, Fukada, Nishida, Yamasaki et al., Roles of Zinc and Zinc Signaling in Immunity: Zinc as an Intracellular Signaling Molecule, Adv. Immunol, doi:10.1016/s0065-2776(08)00003-5
Hosier, Farhadian, Morotti, Deshmukh, Lu-Culligan et al., SARS-CoV-2 Infection of the Placenta, J. Clin. Invest, doi:10.1172/jci139569
Howe, Ling, Elangovan, Vasoo, Abdad et al., Plasma IP-10 Could Identify Early Lung Disease in Severe COVID-19 Patients, Ann. Acad. Med. Singap, doi:10.47102/annals-acadmedsg.2021154
Hu, Chen, Wu, He, Ye, Declined Serum High Density Lipoprotein Cholesterol Is Associated with the Severity of COVID-19 Infection, Clin. Chim. Acta, doi:10.1016/j.cca.2020.07.015
Hu, Guo, Zhou, Shi, Characteristics of SARS-CoV-2 and COVID-19, Nat. Rev. Microbiol, doi:10.1038/s41579-020-00459-7
Hussein Were, Njue, Murungi, Wanjau, Use of Human Nails as Bio-Indicators of Heavy Metals Environmental Exposure Among School Age Children in Kenya, Sci. Total Environ, doi:10.1016/j.scitotenv.2007.12.035
Jung, Kim, Choi, The Relationship between Zinc Status and Inflammatory Marker Levels in Rural Korean Adults Aged 40 and Older, PLoS One, doi:10.1371/journal.pone.0130016
Kassu, Yabutani, Mahmud, Mohammad, Nguyen et al., Alterations in Serum Levels of Trace Elements in Tuberculosis and HIV Infections, Eur. J. Clin. Nutr, doi:10.1038/sj.ejcn.1602352
Khoury, Bernstein, Debolt, Stone, Sutton et al., Characteristics and Outcomes of 241 Births to Women with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection at Five New York City Medical Centers, Obstet. Gynecol, doi:10.1097/aog.0000000000004025
Kilbride, Baker, Parapia, Khoury, Shuqaidef et al., Anaemia during Pregnancy as a Risk Factor for Iron-Deficiency Anaemia in Infancy: a Case-Control Study in Jordan, Int. J. Epidemiol, doi:10.1093/ije/28.3.461
Killerby, Link-Gelles, Haight, Schrodt, England et al., Characteristics Associated with Hospitalization Among Patients with COVID-19 -Metropolitan Atlanta, Georgia, MMWR Morb. Mortal. Wkly. Rep, doi:10.15585/mmwr.mm6925e1
Knight, Bunch, Vousden, Morris, Simpson et al., Characteristics and Outcomes of Pregnant Women Admitted to Hospital with Confirmed SARS-CoV-2 Infection in UK: National Population Based Cohort Study, Bmj, doi:10.1136/bmj.m2107
Kucirka, Norton, Sheffield, Severity of COVID-19 in Pregnancy: A Review of Current Evidence, Am. J. Reprod. Immunol, doi:10.1111/aji.13332
Laine, Tuomainen, Salonen, Virtanen, Serum Copper-To-Zinc-Ratio and Risk of Incident Infection in Men: the Kuopio Ischaemic Heart Disease Risk Factor Study, Eur. J. Epidemiol, doi:10.1007/s10654-020-00644-1
Lal, Kumar, Ranjan, Rabidas, Verma et al., Comparative Analysis of Serum Zinc, Copper, Magnesium, Calcium and Iron Level in Acute and Chronic Patients of Visceral Leishmaniasis, J. Trace Elem. Med. Biol, doi:10.1016/j.jtemb.2012.09.007
Lippi, South, Henry, Electrolyte Imbalances in Patients with Severe Coronavirus Disease 2019 (COVID-19), Ann. Clin. Biochem, doi:10.1177/0004563220922255
Liu, Guo, Hibbert, Jain, Singh et al., CXCL10/IP-10 in Infectious Diseases Pathogenesis and Potential Therapeutic Implications, Cytokine Growth Factor Rev, doi:10.1016/j.cytogfr.2011.06.001
Long, Tang, Shi, Li, Deng et al., Clinical and Immunological Assessment of Asymptomatic SARS-CoV-2
Lukác, Massányi, Effects of Trace Elements on the Immune System, Epidemiol. Mikrobiol. Imunol
Luo, Yao, Xia, Cheng, Chen, Characteristics and Pregnancy Outcomes of Asymptomatic and Symptomatic Women with COVID-19: Lessons from Hospitals in Wuhan, J. Infect. Dev. Ctries, doi:10.3855/jidc.14010
Lötscher, Martí I Líndez, Kirchhammer, Cribioli, Giordano Attianese et al., Magnesium Sensing via LFA-1 Regulates CD8+ T Cell Effector Function, Cell, doi:10.1016/j.cell.2021.12.039
Ma, Tu, Gu, Xu, Hou et al., The Predictive Value of Myoglobin for COVID-19-Related Adverse Outcomes: A Systematic Review and Meta-Analysis, Front. Cardiovasc. Med, doi:10.3389/fcvm.2021.757799
Malavolta, Giacconi, Piacenza, Santarelli, Cipriano et al., Plasma Copper/zinc Ratio: an Inflammatory/nutritional Biomarker as Predictor of All-Cause Mortality in Elderly Population, Biogerontology, doi:10.1007/s10522-009-9251-1
Mandel, Harari, Gurevich, Achiron, Cytokine Prediction of Mortality in COVID19 Patients, Cytokine, doi:10.1016/j.cyto.2020.155190
Mardi, Meidaninikjeh, Nikfarjam, Majidi Zolbanin, Jafari, Interleukin-1 in COVID-19 Infection: Immunopathogenesis and Possible Therapeutic Perspective, Viral Immunol, doi:10.1089/vim.2021.0071
Maru, Patil, Carroll-Bennett, Baum, Bohn-Hemmerdinger et al., Universal Screening for SARS-CoV-2 Infection Among Pregnant Women at Elmhurst Hospital Center, Queens, New York, PLoS One, doi:10.1371/journal.pone.0238409
Marzi, Vigano, Trabattoni, Villa, Salvaggio et al., Characterization of Type 1 and Type 2 Cytokine Production Profile in Physiologic and Pathologic Human Pregnancy, Clin. Exp. Immunol, doi:10.1046/j.1365-2249.1996.d01-809.x
Mehra, Juneja, Fingernails as Biological Indices of Metal Exposure, J. Biosci, doi:10.1007/bf02703706
Mirbeyk, Saghazadeh, Rezaei, A Systematic Review of Pregnant Women with COVID-19 and Their Neonates, Arch. Gynecol. Obstet, doi:10.1007/s00404-021-06049-z
Nai, Lorè, Pagani, De Lorenzo, Di Modica et al., Hepcidin Levels Predict Covid-19 Severity and Mortality in a Cohort of Hospitalized Italian Patients, Am. J. Hematol, doi:10.1002/ajh.26027
Nemeth, Valore, Territo, Schiller, Lichtenstein et al., Hepcidin, a Putative Mediator of Anemia of Inflammation, Is a Type II Acute-phase Protein, Blood, doi:10.1182/blood-2002-10-3235
Patteril, Davey-Quinn, Gedney, Murdoch, Bellamy, Functional Iron Deficiency, Infection and Systemic Inflammatory Response Syndrome in Critical Illness, Anaesth. Intensive Care, doi:10.1177/0310057X0102900504
Pedersen, Ho, SARS-CoV-2: a Storm Is Raging, J. Clin. Invest, doi:10.1172/JCI137647
Ratnaningsih, Sukirto, Wahyuningsih, Soluble Transferrin Receptor (sTfR) Identifies Iron Deficiency Anemia (IDA) in Pulmonary Tuberculosis Patients, Acta Med. Indones
Read, Obeid, Ahlenstiel, Ahlenstiel, The Role of Zinc in Antiviral Immunity, Adv. Nutr, doi:10.1093/advances/nmz013
Resnick, Altura, Gupta, Laragh, Alderman et al., Intracellular and Extracellular Magnesium Depletion in Type 2 (Non-insulin-dependent) Diabetes Mellitus, Diabetologia, doi:10.1007/BF00401149
Roeser, Lee, Nacht, Cartwright, The Role of Ceruloplasmin in Iron Metabolism, J. Clin. Invest, doi:10.1172/JCI106460
Salem, Katranji, Bakdash, COVID-19 Infection in Pregnant Women: Review of Maternal and Fetal Outcomes, Int. J. Gynecol. Obstet, doi:10.1002/ijgo.13533
Sangaré, Van Eijk, Ter Kuile, Walson, Stergachis, The Association between Malaria and Iron Status or Supplementation in Pregnancy: a Systematic Review and Meta-Analysis, PLoS One, doi:10.1371/journal.pone.0087743
Sanyaolu, Okorie, Marinkovic, Patidar, Younis et al., Comorbidity and its Impact on Patients with COVID-19, SN Compr. Clin. Med, doi:10.1007/s42399-020-00363-4
Schwartz, Morotti, Placental Pathology of COVID-19 with and without Fetal and Neonatal Infection: Trophoblast Necrosis and Chronic Histiocytic Intervillositis as Risk Factors for Transplacental Transmission of SARS-CoV-2, Viruses, doi:10.3390/v12111308
Sevilla-Montoya, Hidalgo-Bravo, Estrada-Gutiérrez, Villavicencio-Carrisoza, Leon-Juarez et al., Evidence of Possible SARS-CoV -2 Vertical Transmission According to World Health Organization Criteria in Asymptomatic Pregnant Women, Ultrasound Obstet Gyne, doi:10.1002/uog.24787
Skalny, Timashev, Aschner, Aaseth, Chernova et al., Serum Zinc, Copper, and Other Biometals Are Associated with COVID-19 Severity Markers, Metabolites, doi:10.3390/metabo11040244
Sonnweber, Boehm, Sahanic, Pizzini, Aichner et al., Persisting Alterations of Iron Homeostasis in COVID-19 Are Associated with Non-resolving Lung Pathologies and Poor Patients' Performance: a Prospective Observational Cohort Study, Respir. Res, doi:10.1186/s12931-020-01546-2
Taheri, Bahrami, Habibi, Nouri, A Review on the Serum Electrolytes and Trace Elements Role in the Pathophysiology of COVID-19, Biol. Trace Elem. Res, doi:10.1007/s12011-020-02377-4
Tanacan, Yazihan, Erol, Anuk, Yucel Yetiskin et al., The Impact of COVID-19 Infection on the Cytokine Profile of Pregnant Women: A Prospective Case-Control Study, Cytokine, doi:10.1016/j.cyto.2021.155431
Tejeda-Guzmán, Rosas-Arellano, Kroll, Webb, Barajas-Aceves et al., Biogenesis of Zinc Storage Granules in Drosophila melanogaster, J. Exp. Biol, doi:10.1242/jeb.168419
Terrin, Berni Canani, Di Chiara, Pietravalle, Aleandri et al., Zinc in Early Life: A Key Element in the Fetus and Preterm Neonate, Nutrients, doi:10.3390/nu7125542
Tung-Chen, Algora-Martín, Rodríguez-Roca, Díaz De Santiago, COVID-19 Multisystemic Inflammatory Syndrome in Adults: a Not to Be Missed Diagnosis, BMJ Case Rep, doi:10.1136/bcr-2021-241696
Ueda, Takasawa, Impact of Inflammation on Ferritin, Hepcidin and the Management of Iron Deficiency Anemia in Chronic Kidney Disease, Nutrients, doi:10.3390/nu10091173
Valdespino-Vázquez, Helguera-Repetto, León-Juárez, Villavicencio-Carrisoza, Flores-Pliego et al., Fetal and Placental Infection with SARS-CoV-2 in Early Pregnancy, J. Med. Virology, doi:10.1002/jmv.26965
Van Kempen, Deixler, SARS-CoV-2: Influence of Phosphate and Magnesium, Moderated by Vitamin D, on Energy (ATP) Metabolism and on Severity of COVID-19, Am. J. Physiology-Endocrinology Metabolism, doi:10.1152/ajpendo.00474.2020
Van Weyenbergh, Santana, D'oliveira, Jr, Santos et al., Zinc/copper Imbalance Reflects Immune Dysfunction in Human Leishmaniasis: an Ex Vivo and In Vitro Study, BMC Infect. Dis, doi:10.1186/1471-2334-4-50
Vasilyev, Interactions of Caeruloplasmin with Other Proteins Participating in Inflammation, Biochem. Soc. Trans, doi:10.1042/BST0380947
Vivanti, Vauloup-Fellous, Prevot, Zupan, Suffee et al., Transplacental Transmission of SARS-CoV-2 Infection, Nat. Commun, doi:10.1038/s41467-020-17436-6
Vogel-González, Talló-Parra, Herrera-Fernández, Pérez-Vilaró, Chillón et al., Low Zinc Levels at Admission Associates with Poor Clinical Outcomes in SARS-CoV-2 Infection, Nutrients, doi:10.3390/nu13020562
Vukelic, Kapamadzija, Petrovic, Grujic, Novakov-Mikic et al., Variations of Serum Copper Values in Pregnancy, Srp. Arh. Celok. Lek, doi:10.2298/sarh1202042v
Vásquez-Procopio, Osorio, Cortés-Martínez, Hernández-Hernández, Medina-Contreras et al., Intestinal Response to Dietary Manganese Depletion in Drosophila, Metallomics, doi:10.1039/c9mt00218a
Wei, Zeng, Su, Wan, Yu et al., Hypolipidemia Is Associated with the Severity of COVID-19, J. Clin. Lipidol, doi:10.1016/j.jacl.2020.04.008
Weiss, Carver, Role of Divalent Metals in Infectious Disease Susceptibility and Outcome, Clin. Microbiol. Infect, doi:10.1016/j.cmi.2017.01.018
Wessels, Fischer, Rink, Dietary and Physiological Effects of Zinc on the Immune System, Annu. Rev. Nutr, doi:10.1146/annurev-nutr-122019-120635
Wessels, Rolles, Slusarenko, Rink, Zinc Deficiency as a Possible Risk Factor for Increased Susceptibility and Severe Progression of Corona Virus Disease 19, Br. J. Nutr, doi:10.1017/S0007114521000738
Wong, Magnusson, Sharpton, Ho, Effects of Zinc Status on Age-Related T Cell Dysfunction and Chronic Inflammation, Biometals, doi:10.1007/s10534-020-00279-5
Yang, Ma, Wu, Han, Zheng et al., Low Serum Calcium and Phosphorus and Their Clinical Performance in Detecting COVID-19 Patients, J. Med. Virol, doi:10.1002/jmv.26515
Yang, Shen, Li, Yuan, Wei et al., Plasma IP-10 and MCP-3 Levels Are Highly Associated with Disease Severity and Predict the Progression of COVID-19, J. Allergy Clin. Immunol, doi:10.1016/j.jaci.2020.04.027
Yasui, Yasui, Suzuki, Saitou, Yamamoto et al., Analysis of the Predictive Factors for a Critical Illness of COVID-19 during Treatment Relationship between Serum Zinc Level and Critical Illness of COVID-19, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.09.008
Zhang, He, Zeng, Peng, Roles of Interferons in Pregnant Women with Dengue Infection: Protective or Dangerous Factors, Can. J. Infect. Dis. Med. Microbiol, doi:10.1155/2017/1671607
Zhao, Huang, Dai, Feng, Liu et al., Serum Iron Level as a Potential Predictor of Coronavirus Disease 2019 Severity and Mortality: A Retrospective Study, Open Forum Infect. Dis, doi:10.1093/ofid/ofaa250
Zhou, Chen, Ji, He, Xue, Increased Serum Levels of Hepcidin and Ferritin Are Associated with Severity of COVID-19, Med. Sci. Monit, doi:10.12659/MSM.926178
Zinellu, Paliogiannis, Fois, Solidoro, Carru et al., Cholesterol and Triglyceride Concentrations, COVID-19 Severity, and Mortality: A Systematic Review and Meta-Analysis with Meta-Regression, Front. Public Health, doi:10.3389/fpubh.2021.705916
DOI record:
{
"DOI": "10.3389/fcell.2022.935363",
"ISSN": [
"2296-634X"
],
"URL": "http://dx.doi.org/10.3389/fcell.2022.935363",
"abstract": "<jats:p>Pregnancy makes women more susceptible to infectious agents; however, available data on the effect of SARS-CoV-2 on pregnant women are limited. To date, inflammatory responses and changes in serum metal concentration have been reported in COVID-19 patients, but few associations between metal ions and cytokines have been described. The aim of this study was to evaluate correlations between inflammatory markers and serum metal ions in third-trimester pregnant women with varying COVID-19 disease severity. Patients with severe symptoms had increased concentrations of serum magnesium, copper, and calcium ions and decreased concentrations of iron, zinc, and sodium ions. Potassium ions were unaffected. Pro-inflammatory cytokines IL-6, TNF-α, IL-8, IL-1α, anti-inflammatory cytokine IL-4, and the IP-10 chemokine were induced in the severe presentation of COVID-19 during pregnancy. Robust negative correlations between iron/magnesium and zinc/IL-6, and a positive correlation between copper/IP-10 were observed in pregnant women with the severe form of the disease. Thus, coordinated alterations of serum metal ions and inflammatory markers – suggestive of underlying pathophysiological interactions—occur during SARS-CoV-2 infection in pregnancy.</jats:p>",
"alternative-id": [
"10.3389/fcell.2022.935363"
],
"author": [
{
"affiliation": [],
"family": "Vásquez-Procopio",
"given": "Johana",
"sequence": "first"
},
{
"affiliation": [],
"family": "Espejel-Nuñez",
"given": "Aurora",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Torres-Torres",
"given": "Johnatan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Martinez-Portilla",
"given": "Raigam Jafet",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Espino Y. Sosa",
"given": "Salvador",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mateu-Rogell",
"given": "Paloma",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ortega-Castillo",
"given": "Veronica",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tolentino-Dolores",
"given": "Maricruz",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Perichart-Perera",
"given": "Otilia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Franco-Gallardo",
"given": "José Osman",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Carranco-Martínez",
"given": "José Alberto",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Prieto-Rodríguez",
"given": "Scarleth",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Guzmán-Huerta",
"given": "Mario",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Missirlis",
"given": "Fanis",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Estrada-Gutierrez",
"given": "Guadalupe",
"sequence": "additional"
}
],
"container-title": "Frontiers in Cell and Developmental Biology",
"container-title-short": "Front. Cell Dev. Biol.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2022,
8,
9
]
],
"date-time": "2022-08-09T06:52:16Z",
"timestamp": 1660027936000
},
"deposited": {
"date-parts": [
[
2022,
8,
9
]
],
"date-time": "2022-08-09T06:52:25Z",
"timestamp": 1660027945000
},
"indexed": {
"date-parts": [
[
2022,
8,
10
]
],
"date-time": "2022-08-10T04:09:52Z",
"timestamp": 1660104592496
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
8,
9
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
8,
9
]
],
"date-time": "2022-08-09T00:00:00Z",
"timestamp": 1660003200000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fcell.2022.935363/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2022,
8,
9
]
]
},
"published-online": {
"date-parts": [
[
2022,
8,
9
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1001/jamanetworkopen.2020.29256",
"article-title": "Pregnancy Outcomes Among Women with and without Severe Acute Respiratory Syndrome Coronavirus 2 Infection",
"author": "Adhikari",
"doi-asserted-by": "publisher",
"first-page": "e2029256",
"journal-title": "JAMA Netw. Open",
"key": "B1",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1002/cphy.c120016",
"article-title": "Iron Homeostasis in the Liver",
"author": "Anderson",
"doi-asserted-by": "publisher",
"first-page": "315",
"journal-title": "Compr. Physiol.",
"key": "B2",
"volume": "3",
"year": "2013"
},
{
"DOI": "10.1007/s12011-020-02496-y",
"article-title": "The Relation Between Trace Element Status (Zinc, Copper, Magnesium) and Clinical Outcomes in COVID-19 Infection During Pregnancy",
"author": "Anuk",
"doi-asserted-by": "publisher",
"first-page": "3608",
"journal-title": "Biol. Trace Elem. Res.",
"key": "B3",
"volume": "199",
"year": "2021"
},
{
"DOI": "10.1186/s12882-020-1713-3",
"article-title": "Serum Magnesium, Mortality and Disease Progression in Chronic Kidney Disease",
"author": "Azem",
"doi-asserted-by": "publisher",
"first-page": "49",
"journal-title": "BMC Nephrol.",
"key": "B4",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1111/1574-6976.12087",
"article-title": "Metal Limitation and Toxicity at the Interface between Host and Pathogen",
"author": "Becker",
"doi-asserted-by": "publisher",
"first-page": "1235",
"journal-title": "FEMS Microbiol. Rev.",
"key": "B5",
"volume": "38",
"year": "2014"
},
{
"DOI": "10.1016/j.hsr.2021.100011",
"article-title": "Intricate Relationship between SARS-CoV-2-Induced Shedding and Cytokine Storm Generation: A Signaling Inflammatory Pathway Augmenting COVID-19",
"author": "Ben Moftah",
"doi-asserted-by": "publisher",
"first-page": "100011",
"journal-title": "Health Sci. Rev.",
"key": "B6",
"volume": "2",
"year": "2022"
},
{
"DOI": "10.1002/ajh.24820",
"article-title": "Iron Deficiency across Chronic Inflammatory Conditions: International Expert Opinion on Definition, Diagnosis, and Management",
"author": "Cappellini",
"doi-asserted-by": "publisher",
"first-page": "1068",
"journal-title": "Am. J. Hematol.",
"key": "B7",
"volume": "92",
"year": "2017"
},
{
"DOI": "10.1371/journal.pone.0249584",
"article-title": "Prevalence, Clinical Features, and Outcomes of SARS-CoV-2 Infection in Pregnant Women with or without Mild/moderate Symptoms: Results from Universal Screening in a Tertiary Care Center in Mexico City, Mexico",
"author": "Cardona-Pérez",
"doi-asserted-by": "publisher",
"first-page": "e0249584",
"journal-title": "PLoS One",
"key": "B8",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0043605",
"article-title": "Preserved Ex Vivo Inflammatory Status in Decidual Cells from Women with Preterm Labor and Subclinical Intrauterine Infection",
"author": "Castro-Leyva",
"doi-asserted-by": "publisher",
"first-page": "e43605",
"journal-title": "PLoS One",
"key": "B9",
"volume": "7",
"year": "2012"
},
{
"DOI": "10.1016/j.jinorgbio.2018.06.012",
"article-title": "Interactions between Metal Binding Viral Proteins and Human Targets as Revealed by Network-Based Bioinformatics",
"author": "Chasapis",
"doi-asserted-by": "publisher",
"first-page": "157",
"journal-title": "J. Inorg. Biochem.",
"key": "B10",
"volume": "186",
"year": "2018"
},
{
"DOI": "10.3389/fimmu.2021.675476",
"article-title": "Immune Response to COVID-19 During Pregnancy",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "675476",
"journal-title": "Front. Immunol.",
"key": "B11",
"volume": "12",
"year": ""
},
{
"DOI": "10.1172/jci137244",
"article-title": "Clinical and Immunological Features of Severe and Moderate Coronavirus Disease 2019",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "2620",
"journal-title": "J. Clin. Invest",
"key": "B12",
"volume": "130",
"year": ""
},
{
"DOI": "10.1038/s41392-021-00703-3",
"article-title": "Differential Immune Responses in Pregnant Patients Recovered from COVID-19",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "289",
"journal-title": "Sig Transduct. Target Ther.",
"key": "B13",
"volume": "6",
"year": ""
},
{
"DOI": "10.1007/s00424-020-02412-2",
"article-title": "The Molecular Mechanisms of Copper Metabolism and its Roles in Human Diseases",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "1415",
"journal-title": "Pflugers Arch. - Eur. J. Physiol.",
"key": "B14",
"volume": "472",
"year": ""
},
{
"DOI": "10.1016/s0140-6736(20)30211-7",
"article-title": "Epidemiological and Clinical Characteristics of 99 Cases of 2019 Novel Coronavirus Pneumonia in Wuhan, China: a Descriptive Study",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "507",
"journal-title": "Lancet",
"key": "B15",
"volume": "395",
"year": ""
},
{
"DOI": "10.3389/fimmu.2020.572567",
"article-title": "Innate Immune Responses to Acute Viral Infection During Pregnancy",
"author": "Cornish",
"doi-asserted-by": "publisher",
"first-page": "572567",
"journal-title": "Front. Immunol.",
"key": "B16",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1039/d0mt00220h",
"article-title": "Understanding the Relationship between Viral Infections and Trace Elements from a Metallomics Perspective: Implications for COVID-19",
"author": "De Jesus",
"doi-asserted-by": "publisher",
"first-page": "1912",
"journal-title": "Metallomics",
"key": "B17",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1007/s12291-021-00961-6",
"article-title": "Trace Elements as Immunoregulators in SARS-CoV-2 and Other Viral Infections",
"author": "Dharmalingam",
"doi-asserted-by": "publisher",
"first-page": "416",
"journal-title": "Ind. J. Clin. Biochem.",
"key": "B18",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.3945/ajcn.117.155812",
"article-title": "Iron Homeostasis during Pregnancy",
"author": "Fisher",
"doi-asserted-by": "publisher",
"first-page": "1567s",
"journal-title": "Am. J. Clin. Nutr.",
"key": "B19",
"volume": "106",
"year": "2017"
},
{
"DOI": "10.3390/nu11030693",
"article-title": "Obesity Is Associated with Changes in Iron Nutrition Status and its Homeostatic Regulation in Pregnancy",
"author": "Flores-Quijano",
"doi-asserted-by": "publisher",
"first-page": "693",
"journal-title": "Nutrients",
"key": "B20",
"volume": "11",
"year": "2019"
},
{
"DOI": "10.1016/j.clnesp.2020.09.022",
"article-title": "Copper as a Potential Adjunct Therapy for Critically Ill COVID-19 Patients",
"author": "Fooladi",
"doi-asserted-by": "publisher",
"first-page": "90",
"journal-title": "Clin. Nutr. ESPEN",
"key": "B21",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.3390/nu4070676",
"article-title": "Zinc and Regulation of Inflammatory Cytokines: Implications for Cardiometabolic Disease",
"author": "Foster",
"doi-asserted-by": "publisher",
"first-page": "676",
"journal-title": "Nutrients",
"key": "B22",
"volume": "4",
"year": "2012"
},
{
"DOI": "10.1097/ccm.0000000000004605",
"article-title": "Prevalence and Impact of Hyponatremia in Patients with Coronavirus Disease 2019 in New York City",
"author": "Frontera",
"doi-asserted-by": "publisher",
"first-page": "e1211",
"journal-title": "Crit. Care Med.",
"key": "B23",
"volume": "48",
"year": "2020"
},
{
"DOI": "10.1016/j.medj.2020.10.004",
"article-title": "Hepcidin-Mediated Hypoferremia Disrupts Immune Responses to Vaccination and Infection",
"author": "Frost",
"doi-asserted-by": "publisher",
"first-page": "164",
"journal-title": "Med",
"key": "B24",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1079/pns2004385",
"article-title": "Iron, Copper and Fetal Development",
"author": "Gambling",
"doi-asserted-by": "publisher",
"first-page": "553",
"journal-title": "Proc. Nutr. Soc.",
"key": "B25",
"volume": "63",
"year": "2004"
},
{
"DOI": "10.1056/nejmcp2009249",
"article-title": "Mild or Moderate Covid-19",
"author": "Gandhi",
"doi-asserted-by": "publisher",
"first-page": "1757",
"journal-title": "N. Engl. J. Med.",
"key": "B26",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1073/pnas.2117807119",
"article-title": "Tryptophan Regulates Drosophila Zinc Stores",
"author": "Garay",
"doi-asserted-by": "publisher",
"first-page": "e2117807119",
"journal-title": "Proc. Natl. Acad. Sci. U. S. A.",
"key": "B27",
"volume": "119",
"year": "2022"
},
{
"DOI": "10.1038/s41467-021-27745-z",
"article-title": "Maternal-fetal Immune Responses in Pregnant Women Infected with SARS-CoV-2",
"author": "Garcia-Flores",
"doi-asserted-by": "publisher",
"first-page": "320",
"journal-title": "Nat. Commun.",
"key": "B28",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.15585/mmwr.mm6915e3",
"article-title": "Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 - COVID-NET, 14 States, March 1-30, 2020",
"author": "Garg",
"doi-asserted-by": "publisher",
"first-page": "458",
"journal-title": "MMWR Morb. Mortal. Wkly. Rep.",
"key": "B29",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1053/j.seminhematol.2021.07.001",
"article-title": "Iron Metabolism in Infections: Focus on COVID-19",
"author": "Girelli",
"doi-asserted-by": "publisher",
"first-page": "182",
"journal-title": "Seminars Hematol.",
"key": "B30",
"volume": "58",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2020.531543",
"article-title": "Maternal-Fetal Inflammation in the Placenta and the Developmental Origins of Health and Disease",
"author": "Goldstein",
"doi-asserted-by": "publisher",
"first-page": "531543",
"journal-title": "Front. Immunol.",
"key": "B31",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1002/ncp.10612",
"article-title": "Association Between Low Zinc Levels and Severity of Acute Respiratory Distress Syndrome by New Coronavirus SARS‐CoV‐2",
"author": "Gonçalves",
"doi-asserted-by": "publisher",
"first-page": "186",
"journal-title": "Nutr. Clin. Pract.",
"key": "B32",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.1093/jat/33.2.92",
"article-title": "Application of Inductively Coupled Plasma Mass Spectrometry Multielement Analysis in Fingernail and Toenail as a Biomarker of Metal Exposure",
"author": "Goulle",
"doi-asserted-by": "publisher",
"first-page": "92",
"journal-title": "J. Anal. Toxicol.",
"key": "B33",
"volume": "33",
"year": "2009"
},
{
"DOI": "10.3390/biom10081176",
"article-title": "The Role of Fe, Zn, and Cu in Pregnancy",
"author": "Grzeszczak",
"doi-asserted-by": "publisher",
"first-page": "1176",
"journal-title": "Biomolecules",
"key": "B34",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1183/13993003.00547-2020",
"article-title": "Comorbidity and its Impact on 1590 Patients with COVID-19 in China: a Nationwide Analysis",
"author": "Guan",
"doi-asserted-by": "publisher",
"first-page": "2000547",
"journal-title": "Eur. Respir. J.",
"key": "B35",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.3390/nu13061898",
"article-title": "Relation of Serum Copper Status to Survival in COVID-19",
"author": "Hackler",
"doi-asserted-by": "publisher",
"first-page": "1898",
"journal-title": "Nutrients",
"key": "B36",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.12861/jrip.2014.29",
"article-title": "Association of helicobacter Pylori Infection with Serum Magnesium in Kidney Transplant Patients",
"author": "Hafizi",
"doi-asserted-by": "publisher",
"first-page": "101",
"journal-title": "J. Ren. Inj. Prev.",
"key": "B37",
"volume": "3",
"year": "2014"
},
{
"DOI": "10.1097/hs9.0000000000000492",
"article-title": "Hypoferremia Is Associated with Increased Hospitalization and Oxygen Demand in COVID-19 Patients",
"author": "Hippchen",
"doi-asserted-by": "publisher",
"first-page": "e492",
"journal-title": "Hemasphere",
"key": "B38",
"volume": "4",
"year": "2020"
},
{
"DOI": "10.1016/s0065-2776(08)00003-5",
"article-title": "Roles of Zinc and Zinc Signaling in Immunity: Zinc as an Intracellular Signaling Molecule",
"author": "Hirano",
"doi-asserted-by": "publisher",
"first-page": "149",
"journal-title": "Adv. Immunol.",
"key": "B39",
"volume": "97",
"year": "2008"
},
{
"DOI": "10.1172/jci139569",
"article-title": "SARS-CoV-2 Infection of the Placenta",
"author": "Hosier",
"doi-asserted-by": "publisher",
"first-page": "4947",
"journal-title": "J. Clin. Invest",
"key": "B40",
"volume": "130",
"year": "2020"
},
{
"DOI": "10.47102/annals-acadmedsg.2021154",
"article-title": "Plasma IP-10 Could Identify Early Lung Disease in Severe COVID-19 Patients",
"author": "Howe",
"doi-asserted-by": "publisher",
"first-page": "856",
"journal-title": "Ann. Acad. Med. Singap",
"key": "B41",
"volume": "50",
"year": "2021"
},
{
"DOI": "10.1038/s41579-020-00459-7",
"article-title": "Characteristics of SARS-CoV-2 and COVID-19",
"author": "Hu",
"doi-asserted-by": "publisher",
"first-page": "141",
"journal-title": "Nat. Rev. Microbiol.",
"key": "B42",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1016/j.cca.2020.07.015",
"article-title": "Declined Serum High Density Lipoprotein Cholesterol Is Associated with the Severity of COVID-19 Infection",
"author": "Hu",
"doi-asserted-by": "publisher",
"first-page": "105",
"journal-title": "Clin. Chim. Acta",
"key": "B43",
"volume": "510",
"year": "2020"
},
{
"DOI": "10.1016/j.scitotenv.2007.12.035",
"article-title": "Use of Human Nails as Bio-Indicators of Heavy Metals Environmental Exposure Among School Age Children in Kenya",
"author": "Hussein Were",
"doi-asserted-by": "publisher",
"first-page": "376",
"journal-title": "Sci. Total Environ.",
"key": "B44",
"volume": "393",
"year": "2008"
},
{
"DOI": "10.1371/journal.pone.0130016",
"article-title": "The Relationship between Zinc Status and Inflammatory Marker Levels in Rural Korean Adults Aged 40 and Older",
"author": "Jung",
"doi-asserted-by": "publisher",
"first-page": "e0130016",
"journal-title": "PLoS One",
"key": "B45",
"volume": "10",
"year": "2015"
},
{
"DOI": "10.1038/sj.ejcn.1602352",
"article-title": "Alterations in Serum Levels of Trace Elements in Tuberculosis and HIV Infections",
"author": "Kassu",
"doi-asserted-by": "publisher",
"first-page": "580",
"journal-title": "Eur. J. Clin. Nutr.",
"key": "B46",
"volume": "60",
"year": "2006"
},
{
"DOI": "10.1097/aog.0000000000004025",
"article-title": "Characteristics and Outcomes of 241 Births to Women with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection at Five New York City Medical Centers",
"author": "Khoury",
"doi-asserted-by": "publisher",
"first-page": "273",
"journal-title": "Obstet. Gynecol.",
"key": "B47",
"volume": "136",
"year": "2020"
},
{
"DOI": "10.1093/ije/28.3.461",
"article-title": "Anaemia during Pregnancy as a Risk Factor for Iron-Deficiency Anaemia in Infancy: a Case-Control Study in Jordan",
"author": "Kilbride",
"doi-asserted-by": "publisher",
"first-page": "461",
"journal-title": "Int. J. Epidemiol.",
"key": "B48",
"volume": "28",
"year": "1999"
},
{
"DOI": "10.15585/mmwr.mm6925e1",
"article-title": "Characteristics Associated with Hospitalization Among Patients with COVID-19 - Metropolitan Atlanta, Georgia, March-April 2020",
"author": "Killerby",
"doi-asserted-by": "publisher",
"first-page": "790",
"journal-title": "MMWR Morb. Mortal. Wkly. Rep.",
"key": "B49",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m2107",
"article-title": "Characteristics and Outcomes of Pregnant Women Admitted to Hospital with Confirmed SARS-CoV-2 Infection in UK: National Population Based Cohort Study",
"author": "Knight",
"doi-asserted-by": "publisher",
"first-page": "m2107",
"journal-title": "Bmj",
"key": "B50",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1111/aji.13332",
"article-title": "Severity of COVID-19 in Pregnancy: A Review of Current Evidence",
"author": "Kucirka",
"doi-asserted-by": "publisher",
"first-page": "e13332",
"journal-title": "Am. J. Reprod. Immunol.",
"key": "B51",
"volume": "84",
"year": "2020"
},
{
"DOI": "10.1007/s10654-020-00644-1",
"article-title": "Serum Copper-To-Zinc-Ratio and Risk of Incident Infection in Men: the Kuopio Ischaemic Heart Disease Risk Factor Study",
"author": "Laine",
"doi-asserted-by": "publisher",
"first-page": "1149",
"journal-title": "Eur. J. Epidemiol.",
"key": "B52",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1016/j.jtemb.2012.09.007",
"article-title": "Comparative Analysis of Serum Zinc, Copper, Magnesium, Calcium and Iron Level in Acute and Chronic Patients of Visceral Leishmaniasis",
"author": "Lal",
"doi-asserted-by": "publisher",
"first-page": "98",
"journal-title": "J. Trace Elem. Med. Biol.",
"key": "B53",
"volume": "27",
"year": "2013"
},
{
"DOI": "10.1177/0004563220922255",
"article-title": "Electrolyte Imbalances in Patients with Severe Coronavirus Disease 2019 (COVID-19)",
"author": "Lippi",
"doi-asserted-by": "publisher",
"first-page": "262",
"journal-title": "Ann. Clin. Biochem.",
"key": "B54",
"volume": "57",
"year": "2020"
},
{
"DOI": "10.1016/j.cytogfr.2011.06.001",
"article-title": "CXCL10/IP-10 in Infectious Diseases Pathogenesis and Potential Therapeutic Implications",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "121",
"journal-title": "Cytokine Growth Factor Rev.",
"key": "B55",
"volume": "22",
"year": "2011"
},
{
"DOI": "10.1038/s41591-020-0965-6",
"article-title": "Clinical and Immunological Assessment of Asymptomatic SARS-CoV-2 Infections",
"author": "Long",
"doi-asserted-by": "publisher",
"first-page": "1200",
"journal-title": "Nat. Med.",
"key": "B56",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2021.12.039",
"article-title": "Magnesium Sensing via LFA-1 Regulates CD8+ T Cell Effector Function",
"author": "Lötscher",
"doi-asserted-by": "publisher",
"first-page": "585",
"journal-title": "Cell",
"key": "B57",
"volume": "185",
"year": "2022"
},
{
"article-title": "Effects of Trace Elements on the Immune System",
"author": "Lukác",
"first-page": "3",
"journal-title": "Epidemiol. Mikrobiol. Imunol.",
"key": "B58",
"volume": "56",
"year": "2007"
},
{
"DOI": "10.3855/jidc.14010",
"article-title": "Characteristics and Pregnancy Outcomes of Asymptomatic and Symptomatic Women with COVID-19: Lessons from Hospitals in Wuhan",
"author": "Luo",
"doi-asserted-by": "publisher",
"first-page": "463",
"journal-title": "J. Infect. Dev. Ctries.",
"key": "B59",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.3389/fcvm.2021.757799",
"article-title": "The Predictive Value of Myoglobin for COVID-19-Related Adverse Outcomes: A Systematic Review and Meta-Analysis",
"author": "Ma",
"doi-asserted-by": "publisher",
"first-page": "757799",
"journal-title": "Front. Cardiovasc. Med.",
"key": "B60",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1007/s10522-009-9251-1",
"article-title": "Plasma Copper/zinc Ratio: an Inflammatory/nutritional Biomarker as Predictor of All-Cause Mortality in Elderly Population",
"author": "Malavolta",
"doi-asserted-by": "publisher",
"first-page": "309",
"journal-title": "Biogerontology",
"key": "B61",
"volume": "11",
"year": "2010"
},
{
"DOI": "10.1016/j.cyto.2020.155190",
"article-title": "Cytokine Prediction of Mortality in COVID19 Patients",
"author": "Mandel",
"doi-asserted-by": "publisher",
"first-page": "155190",
"journal-title": "Cytokine",
"key": "B62",
"volume": "134",
"year": "2020"
},
{
"DOI": "10.1089/vim.2021.0071",
"article-title": "Interleukin-1 in COVID-19 Infection: Immunopathogenesis and Possible Therapeutic Perspective",
"author": "Mardi",
"doi-asserted-by": "publisher",
"first-page": "679",
"journal-title": "Viral Immunol.",
"key": "B63",
"volume": "34",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0238409",
"article-title": "Universal Screening for SARS-CoV-2 Infection Among Pregnant Women at Elmhurst Hospital Center, Queens, New York",
"author": "Maru",
"doi-asserted-by": "publisher",
"first-page": "e0238409",
"journal-title": "PLoS One",
"key": "B64",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1046/j.1365-2249.1996.d01-809.x",
"article-title": "Characterization of Type 1 and Type 2 Cytokine Production Profile in Physiologic and Pathologic Human Pregnancy",
"author": "Marzi",
"doi-asserted-by": "publisher",
"first-page": "127",
"journal-title": "Clin. Exp. Immunol.",
"key": "B65",
"volume": "106",
"year": "1996"
},
{
"DOI": "10.1007/bf02703706",
"article-title": "Fingernails as Biological Indices of Metal Exposure",
"author": "Mehra",
"doi-asserted-by": "publisher",
"first-page": "253",
"journal-title": "J. Biosci.",
"key": "B66",
"volume": "30",
"year": "2005"
},
{
"DOI": "10.1007/s00404-021-06049-z",
"article-title": "A Systematic Review of Pregnant Women with COVID-19 and Their Neonates",
"author": "Mirbeyk",
"doi-asserted-by": "publisher",
"first-page": "5",
"journal-title": "Arch. Gynecol. Obstet.",
"key": "B67",
"volume": "304",
"year": "2021"
},
{
"DOI": "10.1002/ajh.26027",
"article-title": "Hepcidin Levels Predict Covid-19 Severity and Mortality in a Cohort of Hospitalized Italian Patients",
"author": "Nai",
"doi-asserted-by": "publisher",
"first-page": "E32",
"journal-title": "Am. J. Hematol.",
"key": "B68",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1182/blood-2002-10-3235",
"article-title": "Hepcidin, a Putative Mediator of Anemia of Inflammation, Is a Type II Acute-phase Protein",
"author": "Nemeth",
"doi-asserted-by": "publisher",
"first-page": "2461",
"journal-title": "Blood",
"key": "B69",
"volume": "101",
"year": "2003"
},
{
"DOI": "10.1177/0310057X0102900504",
"article-title": "Functional Iron Deficiency, Infection and Systemic Inflammatory Response Syndrome in Critical Illness",
"author": "Patteril",
"doi-asserted-by": "publisher",
"first-page": "473",
"journal-title": "Anaesth. Intensive Care",
"key": "B70",
"volume": "29",
"year": "2001"
},
{
"DOI": "10.1172/JCI137647",
"article-title": "SARS-CoV-2: a Storm Is Raging",
"author": "Pedersen",
"doi-asserted-by": "publisher",
"first-page": "2202",
"journal-title": "J. Clin. Invest",
"key": "B71",
"volume": "130",
"year": "2020"
},
{
"article-title": "Soluble Transferrin Receptor (sTfR) Identifies Iron Deficiency Anemia (IDA) in Pulmonary Tuberculosis Patients",
"author": "Ratnaningsih",
"first-page": "334",
"journal-title": "Acta Med. Indones.",
"key": "B72",
"volume": "52",
"year": "2020"
},
{
"DOI": "10.1093/advances/nmz013",
"article-title": "The Role of Zinc in Antiviral Immunity",
"author": "Read",
"doi-asserted-by": "publisher",
"first-page": "696",
"journal-title": "Adv. Nutr.",
"key": "B73",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1007/BF00401149",
"article-title": "Intracellular and Extracellular Magnesium Depletion in Type 2 (Non-insulin-dependent) Diabetes Mellitus",
"author": "Resnick",
"doi-asserted-by": "publisher",
"first-page": "767",
"journal-title": "Diabetologia",
"key": "B74",
"volume": "36",
"year": "1993"
},
{
"DOI": "10.1172/JCI106460",
"article-title": "The Role of Ceruloplasmin in Iron Metabolism",
"author": "Roeser",
"doi-asserted-by": "publisher",
"first-page": "2408",
"journal-title": "J. Clin. Invest.",
"key": "B75",
"volume": "49",
"year": "1970"
},
{
"DOI": "10.1002/ijgo.13533",
"article-title": "COVID‐19 Infection in Pregnant Women: Review of Maternal and Fetal Outcomes",
"author": "Salem",
"doi-asserted-by": "publisher",
"first-page": "291",
"journal-title": "Int. J. Gynecol. Obstet.",
"key": "B76",
"volume": "152",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0087743",
"article-title": "The Association between Malaria and Iron Status or Supplementation in Pregnancy: a Systematic Review and Meta-Analysis",
"author": "Sangaré",
"doi-asserted-by": "publisher",
"first-page": "e87743",
"journal-title": "PLoS One",
"key": "B77",
"volume": "9",
"year": "2014"
},
{
"DOI": "10.1007/s42399-020-00363-4",
"article-title": "Comorbidity and its Impact on Patients with COVID-19",
"author": "Sanyaolu",
"doi-asserted-by": "publisher",
"first-page": "1069",
"journal-title": "SN Compr. Clin. Med.",
"key": "B78",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.3390/v12111308",
"article-title": "Placental Pathology of COVID-19 with and without Fetal and Neonatal Infection: Trophoblast Necrosis and Chronic Histiocytic Intervillositis as Risk Factors for Transplacental Transmission of SARS-CoV-2",
"author": "Schwartz",
"doi-asserted-by": "publisher",
"first-page": "1308",
"journal-title": "Viruses",
"key": "B79",
"volume": "12",
"year": "2020"
},
{
"article-title": "Informe Semanal de Notificación Inmediata de Muerte Materna",
"first-page": "30",
"key": "B80",
"year": "2021"
},
{
"DOI": "10.1002/uog.24787",
"article-title": "Evidence of Possible SARS‐CoV ‐2 Vertical Transmission According to World Health Organization Criteria in Asymptomatic Pregnant Women",
"author": "Sevilla‐Montoya",
"doi-asserted-by": "publisher",
"first-page": "900",
"journal-title": "Ultrasound Obstet Gyne",
"key": "B81",
"volume": "58",
"year": "2021"
},
{
"DOI": "10.3390/metabo11040244",
"article-title": "Serum Zinc, Copper, and Other Biometals Are Associated with COVID-19 Severity Markers",
"author": "Skalny",
"doi-asserted-by": "publisher",
"first-page": "244",
"journal-title": "Metabolites",
"key": "B82",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1186/s12931-020-01546-2",
"article-title": "Persisting Alterations of Iron Homeostasis in COVID-19 Are Associated with Non-resolving Lung Pathologies and Poor Patients' Performance: a Prospective Observational Cohort Study",
"author": "Sonnweber",
"doi-asserted-by": "publisher",
"first-page": "276",
"journal-title": "Respir. Res.",
"key": "B83",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1007/s12011-020-02377-4",
"article-title": "A Review on the Serum Electrolytes and Trace Elements Role in the Pathophysiology of COVID-19",
"author": "Taheri",
"doi-asserted-by": "publisher",
"first-page": "2475",
"journal-title": "Biol. Trace Elem. Res.",
"key": "B84",
"volume": "199",
"year": "2021"
},
{
"DOI": "10.1016/j.cyto.2021.155431",
"article-title": "The Impact of COVID-19 Infection on the Cytokine Profile of Pregnant Women: A Prospective Case-Control Study",
"author": "Tanacan",
"doi-asserted-by": "publisher",
"first-page": "155431",
"journal-title": "Cytokine",
"key": "B85",
"volume": "140",
"year": "2021"
},
{
"DOI": "10.1242/jeb.168419",
"article-title": "Biogenesis of Zinc Storage Granules in Drosophila melanogaster",
"author": "Tejeda-Guzmán",
"doi-asserted-by": "publisher",
"first-page": "jeb168419",
"journal-title": "J. Exp. Biol.",
"key": "B86",
"volume": "221",
"year": "2018"
},
{
"DOI": "10.1080/10641955.2020.1769645",
"article-title": "Complications and Outcomes of SARS-CoV-2 in Pregnancy: where and what Is the Evidence?",
"author": "Teles Abrao Trad",
"doi-asserted-by": "publisher",
"first-page": "361",
"journal-title": "Hypertens. Pregnancy",
"key": "B87",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.3390/nu7125542",
"article-title": "Zinc in Early Life: A Key Element in the Fetus and Preterm Neonate",
"author": "Terrin",
"doi-asserted-by": "publisher",
"first-page": "10427",
"journal-title": "Nutrients",
"key": "B88",
"volume": "7",
"year": "2015"
},
{
"DOI": "10.1136/bcr-2021-241696",
"article-title": "COVID-19 Multisystemic Inflammatory Syndrome in Adults: a Not to Be Missed Diagnosis",
"author": "Tung-Chen",
"doi-asserted-by": "publisher",
"first-page": "e241696",
"journal-title": "BMJ Case Rep.",
"key": "B89",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.3390/nu10091173",
"article-title": "Impact of Inflammation on Ferritin, Hepcidin and the Management of Iron Deficiency Anemia in Chronic Kidney Disease",
"author": "Ueda",
"doi-asserted-by": "publisher",
"first-page": "1173",
"journal-title": "Nutrients",
"key": "B90",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.1002/jmv.26965",
"article-title": "Fetal and Placental Infection with SARS‐CoV‐2 in Early Pregnancy",
"author": "Valdespino‐Vázquez",
"doi-asserted-by": "publisher",
"first-page": "4480",
"journal-title": "J. Med. Virology",
"key": "B91",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1152/ajpendo.00474.2020",
"article-title": "SARS-CoV-2: Influence of Phosphate and Magnesium, Moderated by Vitamin D, on Energy (ATP) Metabolism and on Severity of COVID-19",
"author": "Van Kempen",
"doi-asserted-by": "publisher",
"first-page": "E2",
"journal-title": "Am. J. Physiology-Endocrinology Metabolism",
"key": "B92",
"volume": "320",
"year": "2021"
},
{
"DOI": "10.1186/1471-2334-4-50",
"article-title": "Zinc/copper Imbalance Reflects Immune Dysfunction in Human Leishmaniasis: an Ex Vivo and In Vitro Study",
"author": "Van Weyenbergh",
"doi-asserted-by": "publisher",
"first-page": "50",
"journal-title": "BMC Infect. Dis.",
"key": "B93",
"volume": "4",
"year": "2004"
},
{
"DOI": "10.1042/BST0380947",
"article-title": "Interactions of Caeruloplasmin with Other Proteins Participating in Inflammation",
"author": "Vasilyev",
"doi-asserted-by": "publisher",
"first-page": "947",
"journal-title": "Biochem. Soc. Trans.",
"key": "B94",
"volume": "38",
"year": "2010"
},
{
"DOI": "10.1039/c9mt00218a",
"article-title": "Intestinal Response to Dietary Manganese Depletion in Drosophila",
"author": "Vásquez-Procopio",
"doi-asserted-by": "publisher",
"first-page": "218",
"journal-title": "Metallomics",
"key": "B95",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1038/s41467-020-17436-6",
"article-title": "Transplacental Transmission of SARS-CoV-2 Infection",
"author": "Vivanti",
"doi-asserted-by": "publisher",
"first-page": "3572",
"journal-title": "Nat. Commun.",
"key": "B96",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.3390/nu13020562",
"article-title": "Low Zinc Levels at Admission Associates with Poor Clinical Outcomes in SARS-CoV-2 Infection",
"author": "Vogel-González",
"doi-asserted-by": "publisher",
"first-page": "562",
"journal-title": "Nutrients",
"key": "B97",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.2298/sarh1202042v",
"article-title": "Variations of Serum Copper Values in Pregnancy",
"author": "Vukelic",
"doi-asserted-by": "publisher",
"first-page": "42",
"journal-title": "Srp. Arh. Celok. Lek.",
"key": "B98",
"volume": "140",
"year": "2012"
},
{
"DOI": "10.1016/j.jacl.2020.04.008",
"article-title": "Hypolipidemia Is Associated with the Severity of COVID-19",
"author": "Wei",
"doi-asserted-by": "publisher",
"first-page": "297",
"journal-title": "J. Clin. Lipidol.",
"key": "B99",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.cmi.2017.01.018",
"article-title": "Role of Divalent Metals in Infectious Disease Susceptibility and Outcome",
"author": "Weiss",
"doi-asserted-by": "publisher",
"first-page": "16",
"journal-title": "Clin. Microbiol. Infect.",
"key": "B100",
"volume": "24",
"year": "2018"
},
{
"DOI": "10.1146/annurev-nutr-122019-120635",
"article-title": "Dietary and Physiological Effects of Zinc on the Immune System",
"author": "Wessels",
"doi-asserted-by": "publisher",
"first-page": "133",
"journal-title": "Annu. Rev. Nutr.",
"key": "B101",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.1017/S0007114521000738",
"article-title": "Zinc Deficiency as a Possible Risk Factor for Increased Susceptibility and Severe Progression of Corona Virus Disease 19",
"author": "Wessels",
"doi-asserted-by": "publisher",
"first-page": "214",
"journal-title": "Br. J. Nutr.",
"key": "B102",
"volume": "127",
"year": "2022"
},
{
"DOI": "10.1007/s10534-020-00279-5",
"article-title": "Effects of Zinc Status on Age-Related T Cell Dysfunction and Chronic Inflammation",
"author": "Wong",
"doi-asserted-by": "publisher",
"first-page": "291",
"journal-title": "Biometals",
"key": "B103",
"volume": "34",
"year": "2021"
},
{
"DOI": "10.1002/jmv.26515",
"article-title": "Low Serum Calcium and Phosphorus and Their Clinical Performance in Detecting COVID‐19 Patients",
"author": "Yang",
"doi-asserted-by": "publisher",
"first-page": "1639",
"journal-title": "J. Med. Virol.",
"key": "B104",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1016/j.jaci.2020.04.027",
"article-title": "Plasma IP-10 and MCP-3 Levels Are Highly Associated with Disease Severity and Predict the Progression of COVID-19",
"author": "Yang",
"doi-asserted-by": "publisher",
"first-page": "119",
"journal-title": "J. Allergy Clin. Immunol.",
"key": "B105",
"volume": "146",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.09.008",
"article-title": "Analysis of the Predictive Factors for a Critical Illness of COVID-19 during Treatment Relationship between Serum Zinc Level and Critical Illness of COVID-19",
"author": "Yasui",
"doi-asserted-by": "publisher",
"first-page": "230",
"journal-title": "Int. J. Infect. Dis.",
"key": "B106",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.1155/2017/1671607",
"article-title": "Roles of Interferons in Pregnant Women with Dengue Infection: Protective or Dangerous Factors",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Can. J. Infect. Dis. Med. Microbiol.",
"key": "B107",
"volume": "2017",
"year": "2017"
},
{
"DOI": "10.1093/ofid/ofaa250",
"article-title": "Serum Iron Level as a Potential Predictor of Coronavirus Disease 2019 Severity and Mortality: A Retrospective Study",
"author": "Zhao",
"doi-asserted-by": "publisher",
"first-page": "ofaa250",
"journal-title": "Open Forum Infect. Dis.",
"key": "B108",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.12659/MSM.926178",
"article-title": "Increased Serum Levels of Hepcidin and Ferritin Are Associated with Severity of COVID-19",
"author": "Zhou",
"doi-asserted-by": "publisher",
"first-page": "e926178",
"journal-title": "Med. Sci. Monit.",
"key": "B109",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.3389/fpubh.2021.705916",
"article-title": "Cholesterol and Triglyceride Concentrations, COVID-19 Severity, and Mortality: A Systematic Review and Meta-Analysis with Meta-Regression",
"author": "Zinellu",
"doi-asserted-by": "publisher",
"first-page": "705916",
"journal-title": "Front. Public Health",
"key": "B110",
"volume": "9",
"year": "2021"
}
],
"reference-count": 110,
"references-count": 110,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fcell.2022.935363/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Cell Biology",
"Developmental Biology"
],
"subtitle": [],
"title": "Inflammatory-Metal Profile as a Hallmark for COVID-19 Severity During Pregnancy",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "10"
}
