Association of glycemic control with Long COVID in patients with type 2 diabetes: findings from the National COVID Cohort Collaborative (N3C)
et al., BMJ Open Diabetes Research & Care, doi:10.1136/bmjdrc-2024-004536, Feb 2025
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
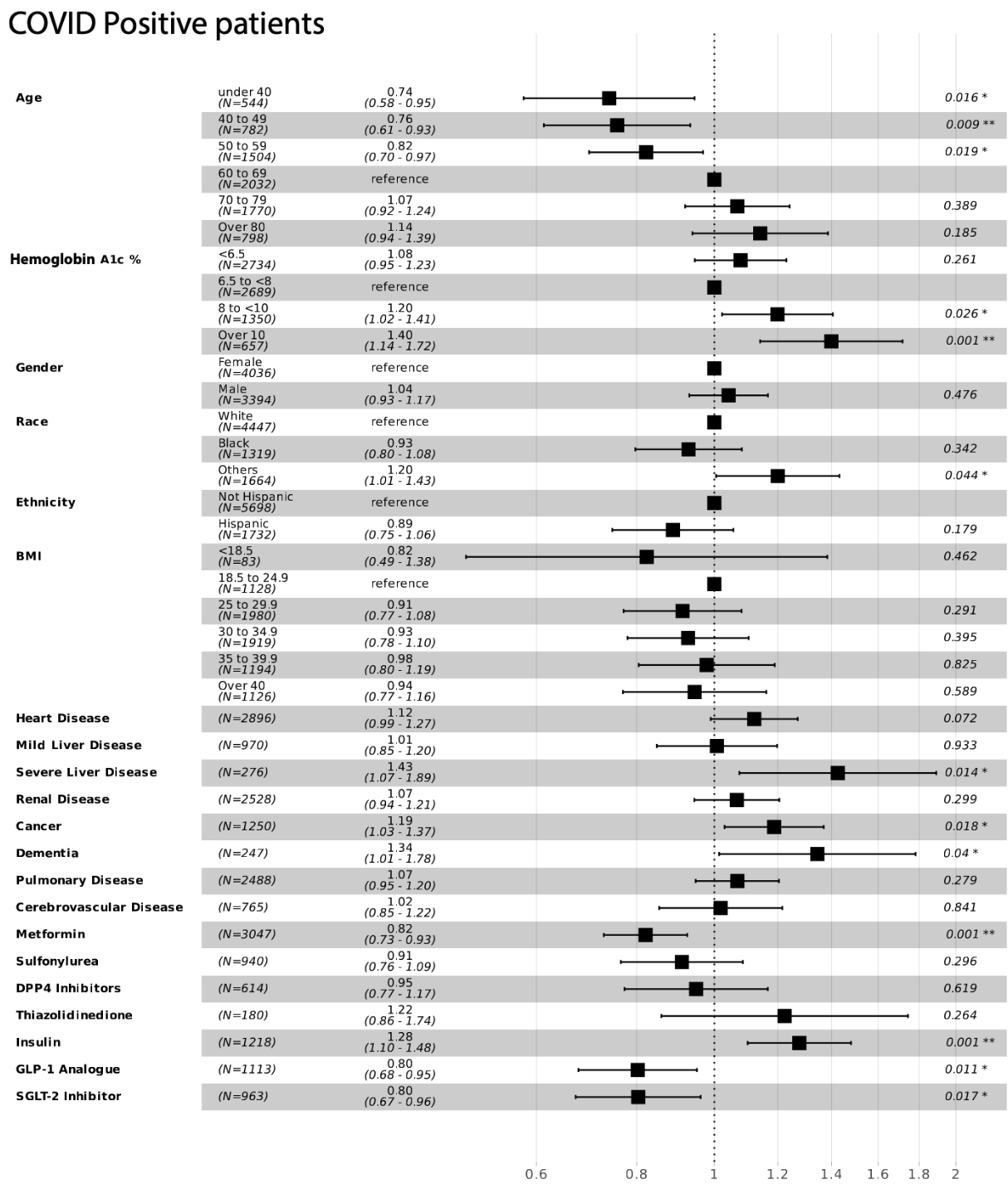
Retrospective 7,430 COVID-positive patients with type 2 diabetes showing lower risk of long COVID or death with metformin use, and higher risk with insulin use.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
long COVID or death, 18.0% lower, OR 0.82, p = 0.001, treatment 3,047, control 4,383, adjusted per study, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Soff et al., 4 Feb 2025, retrospective, USA, peer-reviewed, mean age 62.0, 11 authors, study period 1 January, 2021 - 30 June, 2022.
Association of glycemic control with Long COVID in patients with type 2 diabetes: findings from the National COVID Cohort Collaborative (N3C)
BMJ Open Diabetes Research & Care, doi:10.1136/bmjdrc-2024-004536
Introduction Elevated glycosylated hemoglobin (HbA1c) in individuals with type 2 diabetes is associated with increased risk of hospitalization and death after acute COVID-19, however the effect of HbA1c on Long COVID is unclear. Objective Evaluate the association of glycemic control with the development of Long COVID in patients with type 2 diabetes (T2D).
Research design and methods We conducted a retrospective cohort study using electronic health record data from the National COVID Cohort Collaborative. Our cohort included individuals with T2D from eight sites with longitudinal natural language processing (NLP) data. The primary outcome was death or new-onset recurrent Long COVID symptoms within 30-180 days after COVID-19. Symptoms were identified as keywords from clinical notes using NLP in respiratory, brain fog, fatigue, loss of smell/taste, cough, cardiovascular and musculoskeletal symptom categories. Logistic regression was used to evaluate the risk of Long COVID by HbA1c range, adjusting for demographics, body mass index, comorbidities, and diabetes medication. A COVID-negative group was used as a control. Results Among 7430 COVID-positive patients, 1491 (20.1%) developed symptomatic Long COVID, and 380 (5.1%) died. The primary outcome of death or Long COVID was increased in patients with HbA1c 8% to <10% (OR 1.20, 95% CI 1.02 to 1.41) and ≥10% (OR 1.40, 95% CI 1.14 to 1.72) compared with those with HbA1c 6.5% to <8%. This association was not seen in the COVID-negative group. Higher HbA1c levels were associated with increased risk of Long COVID symptoms, especially respiratory and brain fog. There was no association between HbA1c levels and risk of death within 30-180 days following COVID-19. NLP identified more patients with Long COVID symptoms compared with diagnosis codes. Conclusion Poor glycemic control (HbA1c≥8%) in people with T2D was associated with higher risk of Long COVID symptoms 30-180 days following COVID-19. Notably, this risk increased as HbA1c levels rose. However, this association was not observed in patients with T2D without a history of COVID-19. An NLP-based definition of Long COVID identified more patients than diagnosis codes and should be considered in future studies. ⇒ Clinicians should be aware of the increased risk of Long COVID in patients with poor glycemic control, especially respiratory and brain fog symptoms. Additionally, this study highlights that only textual data from clinical notes contained sufficient information to capture Long COVID in these patients, indicating the potential insensitivity of diagnosis codes in identifying Long COVID.
Contributors SS, RW, and RM conceived the study. SS and YJY performed the analysis. JEBR and RW provided clinical expertise and reviewed/edited the manuscript. RM, MAH, TS, ZB-D, JDH and DB provided statistical or analytical expertise and reviewed/edited the manuscript. CB provided expertise on diabetes and obesity. SS drafted the manuscript and is the guarantor of this work, and as such had full access to all the data in the study and takes full responsibility for the integrity of the data and the accuracy of the data analysis. Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors. Disclaimer The N3C Publication Committee confirmed that this manuscript (MSID:1915.021) is in accordance with N3C data use and attribution policies; however, this content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the N3C program. Competing interests TS receives funding and support from the Center for Pharmacoepidemiology (current members: GlaxoSmithKline, UCB BioSciences, Takeda, AbbVie, Boehringer Ingelheim, Astellas, and Sarepta) and owns stock in Novartis, Roche, and Novo Nordisk. JEBR has affiliations with or receives funding from Springer Nature Switzerland-Exercise Book, Medtronic Diabetes, and AstraZeneca.
Patient consent for publication Not applicable. Ethics approval N3C Attribution. The analyses..
References
Arnold, Wang, The HbA1c and all-cause mortality relationship in patients with type 2 diabetes is J-shaped: a meta-analysis of observational studies, Rev Diabet Stud, doi:10.1900/RDS.2014.11.138
Astin, Banerjee, Baker, Long COVID: mechanisms, risk factors and recovery, Exp Physiol, doi:10.1113/EP090802
Bennett, Moffitt, Hajagos, Clinical Characterization and Prediction of Clinical Severity of SARS-CoV-2 Infection Among US Adults Using Data From the US National COVID Cohort Collaborative, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.16901
Bode, Garrett, Messler, Glycemic Characteristics and Clinical Outcomes of COVID-19 Patients Hospitalized in the United States, J Diabetes Sci Technol, doi:10.1177/1932296820924469
Bramante, Buse, Liebovitz, Outpatient treatment of COVID-19 and incidence of post-COVID-19 condition over 10
Butler, Chiuzan, Ahn, Before and after COVID-19: Changes in symptoms and diagnoses in 13,033 adults, PLoS One, doi:10.1371/journal.pone.0286371
Chen, Chen, Gong, Clinical Characteristics and Outcomes of Type 2 Diabetes Patients Infected with COVID-19: A Retrospective Study, Engineering, doi:10.1016/j.eng.2020.05.017
Currie, Peters, Tynan, Survival as a function of HbA1c in people with type 2 diabetes: a retrospective cohort study, The Lancet, doi:10.1016/S0140-6736(09)61969-3
Fernández-De-Las-Peñas, Guijarro, Torres-Macho, Diabetes and the Risk of Long-term Post-COVID Symptoms, Diabetes, doi:10.2337/db21-0329
Haendel, Chute, Bennett, The National COVID Cohort Collaborative (N3C): Rationale, design, infrastructure, and deployment, J Am Med Inform Assoc, doi:10.1093/jamia/ocaa196
Hainer, Aldhoon-Hainerová, Obesity paradox does exist, BMJ Open Diabetes Research & Care, doi:10.2337/dcS13-2023
Heald, Jenkins, Williams, Mortality in People with Type 2 Diabetes Following SARS-CoV-2 Infection: A Population Level Analysis of Potential Risk Factors, Diabetes Ther, doi:10.1007/s13300-022-01259-3
Heald, Williams, Jenkins, The prevalence of long COVID in people with diabetes mellitus-evidence from a UK cohort, EClinicalMedicine, doi:10.1016/j.eclinm.2024.102607
Healey, Sheikh, Daines, Symptoms and signs of long COVID: A rapid review and meta-analysis, J Glob Health, doi:10.7189/jogh.12.05014
Horberg, Watson, Bhatia, Post-acute sequelae of SARS-CoV-2 with clinical condition definitions and comparison in a matched cohort, Nat Commun, doi:10.1038/s41467-022-33573-6
Johnson, Signor, Lappe, A comparison of natural language processing to ICD-10 codes for identification and characterization of pulmonary embolism, Thromb Res, doi:10.1016/j.thromres.2021.04.020
Kreutzenberg, De, Long COVID-19 and diabetes mellitus: a short review, Metab Target Organ Damage, doi:10.20517/mtod.2022.30
Latouche, Allignol, Beyersmann, A competing risks analysis should report results on all cause-specific hazards and cumulative incidence functions, J Clin Epidemiol, doi:10.1016/j.jclinepi.2012.09.017
Months, COVID-OUT): a multicentre, randomised, quadruple-blind, parallel-group, phase 3 trial, Lancet Infect Dis, doi:10.1016/S1473-3099(23)00299-2
Nathan, The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus, N Engl J Med, doi:10.1056/NEJM199309303291401
Olawore, Turner, Evans, Risk of Post-Acute Sequelae of SARS-CoV-2 Infection (PASC) Among Patients with Type 2 Diabetes Mellitus on Anti-Hyperglycemic Medications, Clin Epidemiol, doi:10.2147/CLEP.S458901
Pfaff, Girvin, Bennett, Identifying who has long COVID in the USA: a machine learning approach using N3C data, Lancet Digit Health, doi:10.1016/S2589-7500(22)00048-6
Pfaff, Madlock-Brown, Baratta, Coding long COVID: characterizing a new disease through an ICD-10 lens, BMC Med, doi:10.1186/s12916-023-02737-6
Qaseem, Wilt, Kansagara, Hemoglobin A1c Targets for Glycemic Control With Pharmacologic Therapy for Nonpregnant Adults With Type 2 Diabetes Mellitus: A Guidance Statement Update From the American College of Physicians, BMJ Open Diab Res Care, doi:10.7326/M17-0939
Rosen, Viral Variants, Vaccinations, and Long Covid -New Insights, N Engl J Med, doi:10.1056/NEJMe2407575
Schuster, Hoogendijk, Kok, Ignoring competing events in the analysis of survival data may lead to biased results: a nonmathematical illustration of competing risk analysis, J Clin Epidemiol, doi:10.1016/j.jclinepi.2020.03.004
Schöning, Liakoni, Drewe, Automatic identification of risk factors for sars-cov-2 positivity and severe clinical outcomes of covid-19 using data mining and natural language processing
Scirica, Lincoff, Lingvay, The Effect of Semaglutide on Mortality and COVID-19-Related Deaths: An Analysis From the SELECT Trial, J Am Coll Cardiol, doi:10.1016/j.jacc.2024.08.007
Sisó-Almirall, Brito-Zerón, Ferrín, Long Covid-19: Proposed Primary Care Clinical Guidelines for Diagnosis and Disease Management, Int J Environ Res Public Health, doi:10.5281/zenodo.10231330
Stratton, Adler, Neil, Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study, BMJ, doi:10.1136/bmj.321.7258.405
Thaweethai, Jolley, Karlson, Development of a Definition of Postacute Sequelae of SARS-CoV-2 Infection, JAMA, doi:10.1001/jama.2023.8823
Wander, Baraff, Fox, Rates of ICD-10 Code U09.9 Documentation and Clinical Characteristics of VA Patients With Post-COVID-19 Condition, JAMA Netw Open, doi:10.1001/jamanetworkopen.2023.46783
Wang, Foer, Macphaul, PASCLex: A comprehensive post-acute sequelae of COVID-19 (PASC) symptom lexicon derived from electronic health record clinical notes, J Biomed Inform, doi:10.1016/j.jbi.2021.103951
Wang, Yi, Wang, Effect of hyperglycemia on the immune function of COVID-19 patients with type 2 diabetes mellitus: a retrospective study, PeerJ, doi:10.7717/peerj.14570
Wong, Hall, Vaddavalli, Glycemic Control and Clinical Outcomes in U.S. Patients With COVID-19: Data From the National COVID Cohort Collaborative (N3C) Database, Diabetes Care, doi:10.2337/dc21-2186
Zhang, Honerlaw, Maripuri, Characterizing the use of the icd-10 code for long covid in 3 us healthcare systems
Zhang, Honerlaw, Maripuri, Potential pitfalls in the use of real-world data for studying long COVID, Nat Med, doi:10.1038/s41591-023-02274-y
Zhu, She, Cheng, Association of Blood Glucose Control and Outcomes in Patients with COVID-19 and Pre-existing Type 2 Diabetes, Cell Metab, doi:10.1016/j.cmet.2020.04.021
DOI record:
{
"DOI": "10.1136/bmjdrc-2024-004536",
"ISSN": [
"2052-4897"
],
"URL": "http://dx.doi.org/10.1136/bmjdrc-2024-004536",
"abstract": "<jats:sec><jats:title>Introduction</jats:title><jats:p>Elevated glycosylated hemoglobin (HbA1c) in individuals with type 2 diabetes is associated with increased risk of hospitalization and death after acute COVID-19, however the effect of HbA1c on Long COVID is unclear.</jats:p></jats:sec><jats:sec><jats:title>Objective</jats:title><jats:p>Evaluate the association of glycemic control with the development of Long COVID in patients with type 2 diabetes (T2D).</jats:p></jats:sec><jats:sec><jats:title>Research design and methods</jats:title><jats:p>We conducted a retrospective cohort study using electronic health record data from the National COVID Cohort Collaborative. Our cohort included individuals with T2D from eight sites with longitudinal natural language processing (NLP) data. The primary outcome was death or new-onset recurrent Long COVID symptoms within 30–180 days after COVID-19. Symptoms were identified as keywords from clinical notes using NLP in respiratory, brain fog, fatigue, loss of smell/taste, cough, cardiovascular and musculoskeletal symptom categories. Logistic regression was used to evaluate the risk of Long COVID by HbA1c range, adjusting for demographics, body mass index, comorbidities, and diabetes medication. A COVID-negative group was used as a control.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Among 7430 COVID-positive patients, 1491 (20.1%) developed symptomatic Long COVID, and 380 (5.1%) died. The primary outcome of death or Long COVID was increased in patients with HbA1c 8% to <10% (OR 1.20, 95% CI 1.02 to 1.41) and ≥10% (OR 1.40, 95% CI 1.14 to 1.72) compared with those with HbA1c 6.5% to <8%. This association was not seen in the COVID-negative group. Higher HbA1c levels were associated with increased risk of Long COVID symptoms, especially respiratory and brain fog. There was no association between HbA1c levels and risk of death within 30–180 days following COVID-19. NLP identified more patients with Long COVID symptoms compared with diagnosis codes.</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>Poor glycemic control (HbA1c≥8%) in people with T2D was associated with higher risk of Long COVID symptoms 30–180 days following COVID-19. Notably, this risk increased as HbA1c levels rose. However, this association was not observed in patients with T2D without a history of COVID-19. An NLP-based definition of Long COVID identified more patients than diagnosis codes and should be considered in future studies.</jats:p></jats:sec>",
"accepted": {
"date-parts": [
[
2024,
12,
26
]
]
},
"alternative-id": [
"10.1136/bmjdrc-2024-004536"
],
"author": [
{
"ORCID": "https://orcid.org/0000-0001-5851-6075",
"affiliation": [],
"authenticated-orcid": false,
"family": "Soff",
"given": "Samuel",
"sequence": "first"
},
{
"ORCID": "https://orcid.org/0000-0003-2144-8480",
"affiliation": [],
"authenticated-orcid": false,
"family": "Yoo",
"given": "Yun Jae",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0001-5858-2080",
"affiliation": [],
"authenticated-orcid": false,
"family": "Bramante",
"given": "Carolyn",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0001-8620-1003",
"affiliation": [],
"authenticated-orcid": false,
"family": "Reusch",
"given": "Jane E B",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0003-0670-4845",
"affiliation": [],
"authenticated-orcid": false,
"family": "Huling",
"given": "Jared Davis",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0002-6263-440X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hall",
"given": "Margaret A",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0001-8095-547X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Brannock",
"given": "Daniel",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0002-9204-7177",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sturmer",
"given": "Til",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0001-6419-0008",
"affiliation": [],
"authenticated-orcid": false,
"family": "Butzin-Dozier",
"given": "Zachary",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0003-3108-7324",
"affiliation": [],
"authenticated-orcid": false,
"family": "Wong",
"given": "Rachel",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0003-2723-5902",
"affiliation": [],
"authenticated-orcid": false,
"family": "Moffitt",
"given": "Richard",
"sequence": "additional"
}
],
"container-title": "BMJ Open Diabetes Research & Care",
"container-title-short": "BMJ Open Diab Res Care",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2025,
2,
4
]
],
"date-time": "2025-02-04T17:32:29Z",
"timestamp": 1738690349000
},
"deposited": {
"date-parts": [
[
2025,
2,
4
]
],
"date-time": "2025-02-04T17:32:39Z",
"timestamp": 1738690359000
},
"indexed": {
"date-parts": [
[
2025,
2,
5
]
],
"date-time": "2025-02-05T05:26:14Z",
"timestamp": 1738733174235,
"version": "3.37.0"
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2025,
2
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2025,
2,
4
]
]
},
"published-print": {
"date-parts": [
[
2025,
2
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 3,
"start": {
"date-parts": [
[
2025,
2,
4
]
],
"date-time": "2025-02-04T00:00:00Z",
"timestamp": 1738627200000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjdrc-2024-004536",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "e004536",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2025,
2
]
]
},
"published-online": {
"date-parts": [
[
2025,
2,
4
]
]
},
"published-print": {
"date-parts": [
[
2025,
2
]
]
},
"publisher": "BMJ",
"reference": [
{
"key": "2025020409301403000_13.1.e004536.1",
"unstructured": "WHO COVID-19 Dashboard . COVID-19 cases. 2024. Available: https://data.who.int/dashboards/covid19/cases"
},
{
"DOI": "10.1113/EP090802",
"doi-asserted-by": "publisher",
"key": "2025020409301403000_13.1.e004536.2"
},
{
"DOI": "10.1001/jama.2023.8823",
"doi-asserted-by": "publisher",
"key": "2025020409301403000_13.1.e004536.3"
},
{
"DOI": "10.1101/2023.02.12.23285701",
"doi-asserted-by": "crossref",
"key": "2025020409301403000_13.1.e004536.4",
"unstructured": "Zhang HG , Honerlaw JP , Maripuri M , et al . Characterizing the use of the icd-10 code for long covid in 3 us healthcare systems. Health Informatics [Preprint] 2023. doi:10.1101/2023.02.12.23285701"
},
{
"DOI": "10.1038/s41467-022-33573-6",
"article-title": "Post-acute sequelae of SARS-CoV-2 with clinical condition definitions and comparison in a matched cohort",
"author": "Horberg",
"doi-asserted-by": "crossref",
"journal-title": "Nat Commun",
"key": "2025020409301403000_13.1.e004536.5",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/j.jbi.2021.103951",
"article-title": "PASCLex: A comprehensive post-acute sequelae of COVID-19 (PASC) symptom lexicon derived from electronic health record clinical notes",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "103951",
"journal-title": "J Biomed Inform",
"key": "2025020409301403000_13.1.e004536.6",
"volume": "125",
"year": "2022"
},
{
"DOI": "10.1016/j.cmet.2020.04.021",
"doi-asserted-by": "publisher",
"key": "2025020409301403000_13.1.e004536.7"
},
{
"DOI": "10.1177/1932296820924469",
"article-title": "Glycemic Characteristics and Clinical Outcomes of COVID-19 Patients Hospitalized in the United States",
"author": "Bode",
"doi-asserted-by": "crossref",
"first-page": "813",
"journal-title": "J Diabetes Sci Technol",
"key": "2025020409301403000_13.1.e004536.8",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1007/s13300-022-01259-3",
"doi-asserted-by": "publisher",
"key": "2025020409301403000_13.1.e004536.9"
},
{
"article-title": "Clinical Characteristics and Outcomes of Type 2 Diabetes Patients Infected with COVID-19: A Retrospective Study",
"author": "Chen",
"first-page": "1170",
"journal-title": "Engineering (Beijing)",
"key": "2025020409301403000_13.1.e004536.10",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.7717/peerj.14570",
"article-title": "Effect of hyperglycemia on the immune function of COVID-19 patients with type 2 diabetes mellitus: a retrospective study",
"author": "Wang",
"doi-asserted-by": "crossref",
"journal-title": "PeerJ",
"key": "2025020409301403000_13.1.e004536.11",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.2337/dc21-2186",
"article-title": "Glycemic Control and Clinical Outcomes in U.S. Patients With COVID-19: Data From the National COVID Cohort Collaborative (N3C) Database",
"author": "Wong",
"doi-asserted-by": "crossref",
"first-page": "1099",
"journal-title": "Diabetes Care",
"key": "2025020409301403000_13.1.e004536.12",
"volume": "45",
"year": "2022"
},
{
"DOI": "10.1900/RDS.2014.11.138",
"doi-asserted-by": "publisher",
"key": "2025020409301403000_13.1.e004536.13"
},
{
"DOI": "10.1136/bmj.321.7258.405",
"doi-asserted-by": "publisher",
"key": "2025020409301403000_13.1.e004536.14"
},
{
"DOI": "10.1016/S2589-7500(22)00048-6",
"article-title": "Identifying who has long COVID in the USA: a machine learning approach using N3C data",
"author": "Pfaff",
"doi-asserted-by": "crossref",
"first-page": "e532",
"journal-title": "Lancet Digit Health",
"key": "2025020409301403000_13.1.e004536.15",
"volume": "4",
"year": "2022"
},
{
"DOI": "10.1016/j.eclinm.2024.102607",
"article-title": "The prevalence of long COVID in people with diabetes mellitus-evidence from a UK cohort",
"author": "Heald",
"doi-asserted-by": "crossref",
"journal-title": "EClinicalMedicine",
"key": "2025020409301403000_13.1.e004536.16",
"volume": "71",
"year": "2024"
},
{
"DOI": "10.1001/jamanetworkopen.2023.46783",
"article-title": "Rates of ICD-10 Code U09.9 Documentation and Clinical Characteristics of VA Patients With Post-COVID-19 Condition",
"author": "Wander",
"doi-asserted-by": "crossref",
"journal-title": "JAMA Netw Open",
"key": "2025020409301403000_13.1.e004536.17",
"volume": "6",
"year": "2023"
},
{
"DOI": "10.1186/s12916-023-02737-6",
"article-title": "Coding long COVID: characterizing a new disease through an ICD-10 lens",
"author": "Pfaff",
"doi-asserted-by": "crossref",
"journal-title": "BMC Med",
"key": "2025020409301403000_13.1.e004536.18",
"volume": "21",
"year": "2023"
},
{
"DOI": "10.1038/s41591-023-02274-y",
"article-title": "Potential pitfalls in the use of real-world data for studying long COVID",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "1040",
"journal-title": "Nat Med",
"key": "2025020409301403000_13.1.e004536.19",
"volume": "29",
"year": "2023"
},
{
"DOI": "10.1016/j.thromres.2021.04.020",
"article-title": "A comparison of natural language processing to ICD-10 codes for identification and characterization of pulmonary embolism",
"author": "Johnson",
"doi-asserted-by": "crossref",
"first-page": "190",
"journal-title": "Thromb Res",
"key": "2025020409301403000_13.1.e004536.20",
"volume": "203",
"year": "2021"
},
{
"key": "2025020409301403000_13.1.e004536.21",
"unstructured": "Yuanda Zhu Georgia Institute of Technology, Aishwarya Mahale Georgia Institute of Technology, Kourtney Peters Emory University . Using natural language processing on free-text clinical notes to identify patients with long-term covid effects. Available: https://dl.acm.org/doi/10.1145/3535508.3545555 [Accessed 26 Mar 2024]."
},
{
"DOI": "10.1101/2021.03.25.21254314",
"doi-asserted-by": "crossref",
"key": "2025020409301403000_13.1.e004536.22",
"unstructured": "Schöning V , Liakoni E , Drewe J , et al . Automatic identification of risk factors for sars-cov-2 positivity and severe clinical outcomes of covid-19 using data mining and natural language processing. Health Informatics [Preprint] 2021. doi:10.1101/2021.03.25.21254314"
},
{
"DOI": "10.1001/jamanetworkopen.2021.16901",
"article-title": "Clinical Characterization and Prediction of Clinical Severity of SARS-CoV-2 Infection Among US Adults Using Data From the US National COVID Cohort Collaborative",
"author": "Bennett",
"doi-asserted-by": "crossref",
"journal-title": "JAMA Netw Open",
"key": "2025020409301403000_13.1.e004536.23",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1093/jamia/ocaa196",
"article-title": "The National COVID Cohort Collaborative (N3C): Rationale, design, infrastructure, and deployment",
"author": "Haendel",
"doi-asserted-by": "crossref",
"first-page": "427",
"journal-title": "J Am Med Inform Assoc",
"key": "2025020409301403000_13.1.e004536.24",
"volume": "28",
"year": "2021"
},
{
"key": "2025020409301403000_13.1.e004536.25",
"unstructured": "github . N3C nlp documentation. January 2022 Available: https://github.com/OHNLP/N3C-NLP-Documentation/wiki"
},
{
"DOI": "10.3390/ijerph18084350",
"article-title": "Long Covid-19: Proposed Primary Care Clinical Guidelines for Diagnosis and Disease Management",
"author": "Sisó-Almirall",
"doi-asserted-by": "crossref",
"journal-title": "Int J Environ Res Public Health",
"key": "2025020409301403000_13.1.e004536.26",
"volume": "18",
"year": "2021"
},
{
"key": "2025020409301403000_13.1.e004536.27",
"unstructured": "N3C concept set - 21890932 (SARS-COV-2 qual results-negative). 2023. Available: http://dx.doi.org/10.5281/zenodo.10231330"
},
{
"DOI": "10.1371/journal.pone.0286371",
"article-title": "Before and after COVID-19: Changes in symptoms and diagnoses in 13,033 adults",
"author": "Butler",
"doi-asserted-by": "crossref",
"journal-title": "PLoS One",
"key": "2025020409301403000_13.1.e004536.28",
"volume": "19",
"year": "2024"
},
{
"DOI": "10.7189/jogh.12.05014",
"article-title": "Symptoms and signs of long COVID: A rapid review and meta-analysis",
"author": "Healey",
"doi-asserted-by": "crossref",
"journal-title": "J Glob Health",
"key": "2025020409301403000_13.1.e004536.29",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1016/j.jclinepi.2020.03.004",
"doi-asserted-by": "publisher",
"key": "2025020409301403000_13.1.e004536.30"
},
{
"DOI": "10.1016/j.jclinepi.2012.09.017",
"doi-asserted-by": "publisher",
"key": "2025020409301403000_13.1.e004536.31"
},
{
"key": "2025020409301403000_13.1.e004536.32",
"unstructured": "N3C concept set - 708775231 (Long-COVID (PASC)). 2023. Available: http://dx.doi.org/10.5281/zenodo.10231302"
},
{
"DOI": "10.2337/db21-0329",
"doi-asserted-by": "publisher",
"key": "2025020409301403000_13.1.e004536.33"
},
{
"DOI": "10.20517/mtod.2022.30",
"article-title": "Long COVID-19 and diabetes mellitus: a short review",
"author": "Kreutzenberg",
"doi-asserted-by": "crossref",
"first-page": "4",
"journal-title": "Metab Target Organ Damage",
"key": "2025020409301403000_13.1.e004536.34",
"volume": "3",
"year": "2023"
},
{
"DOI": "10.1016/S0140-6736(09)61969-3",
"article-title": "Survival as a function of HbA1c in people with type 2 diabetes: a retrospective cohort study",
"author": "Currie",
"doi-asserted-by": "crossref",
"first-page": "481",
"journal-title": "The Lancet",
"key": "2025020409301403000_13.1.e004536.35",
"volume": "375",
"year": "2010"
},
{
"DOI": "10.1056/NEJM199309303291401",
"doi-asserted-by": "publisher",
"key": "2025020409301403000_13.1.e004536.36"
},
{
"DOI": "10.7326/M17-0939",
"article-title": "Hemoglobin A1c Targets for Glycemic Control With Pharmacologic Therapy for Nonpregnant Adults With Type 2 Diabetes Mellitus: A Guidance Statement Update From the American College of Physicians",
"author": "Qaseem",
"doi-asserted-by": "crossref",
"first-page": "569",
"journal-title": "Ann Intern Med",
"key": "2025020409301403000_13.1.e004536.37",
"volume": "168",
"year": "2018"
},
{
"DOI": "10.2337/dc22-S013",
"doi-asserted-by": "publisher",
"key": "2025020409301403000_13.1.e004536.38"
},
{
"DOI": "10.1056/NEJMe2407575",
"article-title": "Viral Variants, Vaccinations, and Long Covid - New Insights",
"author": "Rosen",
"doi-asserted-by": "crossref",
"first-page": "561",
"journal-title": "N Engl J Med",
"key": "2025020409301403000_13.1.e004536.39",
"volume": "391",
"year": "2024"
},
{
"DOI": "10.1016/j.jacc.2024.08.007",
"article-title": "The Effect of Semaglutide on Mortality and COVID-19-Related Deaths: An Analysis From the SELECT Trial",
"author": "Scirica",
"doi-asserted-by": "crossref",
"first-page": "1632",
"journal-title": "J Am Coll Cardiol",
"key": "2025020409301403000_13.1.e004536.40",
"volume": "84",
"year": "2024"
},
{
"DOI": "10.1016/S1473-3099(23)00299-2",
"doi-asserted-by": "publisher",
"key": "2025020409301403000_13.1.e004536.41"
},
{
"DOI": "10.2147/CLEP.S458901",
"article-title": "Risk of Post-Acute Sequelae of SARS-CoV-2 Infection (PASC) Among Patients with Type 2 Diabetes Mellitus on Anti-Hyperglycemic Medications",
"author": "Olawore",
"doi-asserted-by": "crossref",
"first-page": "379",
"journal-title": "Clin Epidemiol",
"key": "2025020409301403000_13.1.e004536.42",
"volume": "16",
"year": "2024"
},
{
"DOI": "10.2337/dcS13-2023",
"article-title": "Obesity paradox does exist",
"author": "Hainer",
"doi-asserted-by": "crossref",
"first-page": "S276",
"journal-title": "Diabetes Care",
"key": "2025020409301403000_13.1.e004536.43",
"volume": "36 Suppl 2",
"year": "2013"
}
],
"reference-count": 43,
"references-count": 43,
"relation": {},
"resource": {
"primary": {
"URL": "https://drc.bmj.com/lookup/doi/10.1136/bmjdrc-2024-004536"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Association of glycemic control with Long COVID in patients with type 2 diabetes: findings from the National COVID Cohort Collaborative (N3C)",
"type": "journal-article",
"update-policy": "https://doi.org/10.1136/crossmarkpolicy",
"volume": "13"
}
