Hepatic and gastrointestinal disturbances in Egyptian patients infected with coronavirus disease 2019: A multicentre cohort study
et al., World Journal of Gastroenterology, doi:10.3748/wjg.v27.i40.6951, Oct 2021
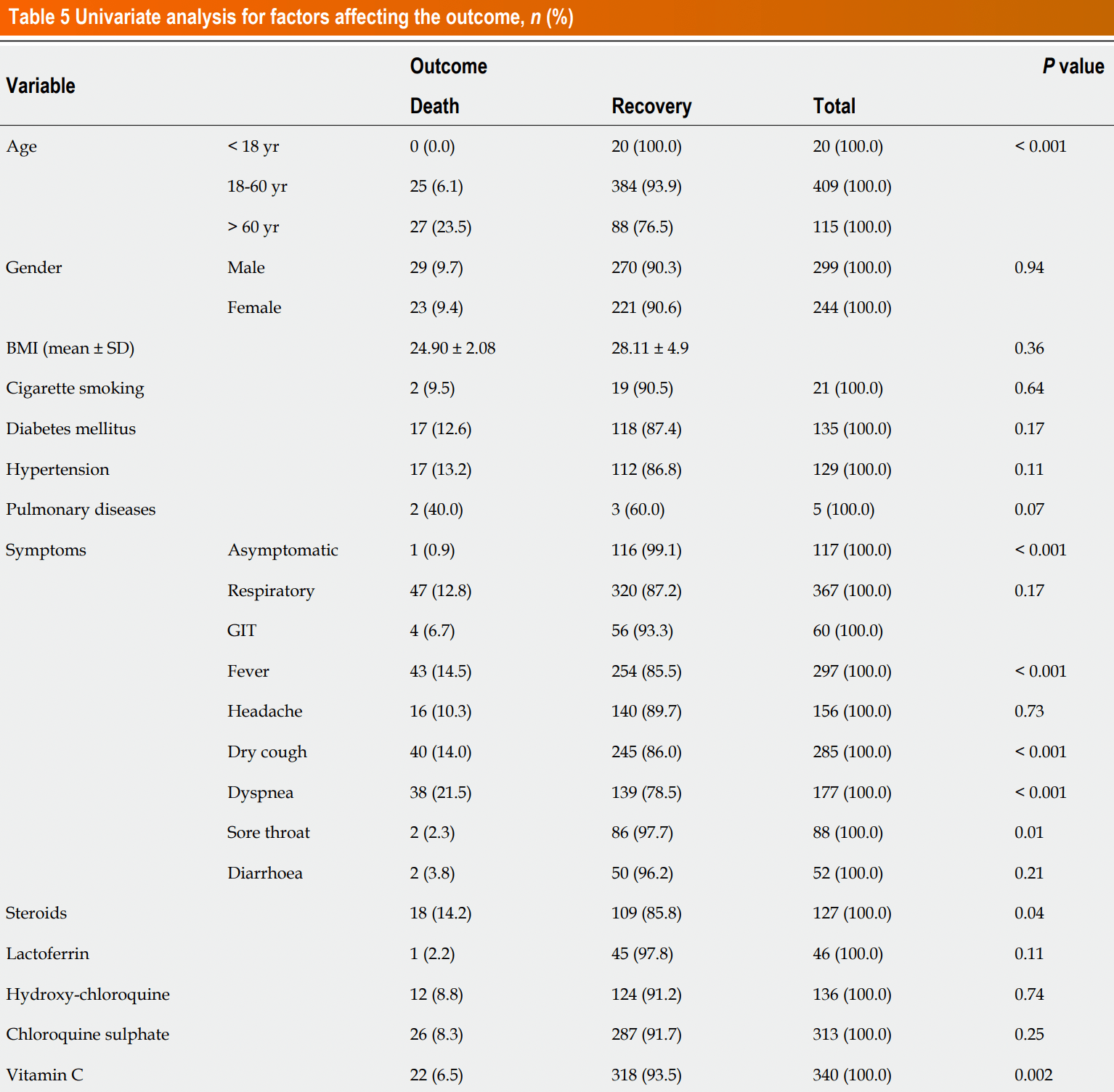
Retrospective 547 hospitalized COVID+ patients in Egypt, showing lower mortality with lactoferrin treatment (without statistical significance).
This study is excluded in the after exclusion results of meta-analysis:
confounding by indication, unadjusted results and treatment used selectively per official protocol; unadjusted results with no group details.
|
risk of death, 79.1% lower, RR 0.21, p = 0.11, treatment 1 of 46 (2.2%), control 52 of 501 (10.4%), NNT 12, unadjusted.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Shousha et al., 28 Oct 2021, retrospective, Egypt, peer-reviewed, 18 authors, study period 15 April, 2020 - 29 July, 2020.
Hepatic and gastrointestinal disturbances in Egyptian patients infected with coronavirus disease 2019: A multicentre cohort study
World Journal of Gastroenterology, doi:10.3748/wjg.v27.i40.6951
Informed consent statement: All study subjects gave written informed consent before study inclusion.
Author contributions: Shousha HI October 28, 2021 Volume 27 Issue 40
Research motivation Comprehensive researches on hepatic and GI derangements in patients with COVID-19 are still lacking, and they are needed for better understanding of the underlying factors, clinical presentations, and disease outcome
Research objectives We aimed to study the prevalence and severity of liver and GI derangements in Egyptian patients with COVID-19 infection and their relation to disease outcomes.
Research methods This multicentre cohort study was conducted on 547 COVID-19 cases from four quarantine hospitals during the period from April 15, 2020 to July 29, 2020. Clinical, laboratory features, fibrosis-4 (FIB-4) index, COVID-19 severity, and outcomes were recorded. Follow-ups were conducted until discharge or death.
Research results Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were elevated in 26% and 32% of patients while elevations above 3 fold were recorded in 4.91% and 3.73% patients, respectively. Male gender, smoking, hypertension, chronic hepatitis C, and lung involvement were associated with elevated AST or ALT. FIB-4 was significantly higher in patients admitted to the intensive care unit (ICU), those with more severe COVID-19, and non-survivors. The independent variables affecting outcome were supplementary vitamin C intake, lung consolidation, ICU admission, and FIB-4 score > 3.25. GI symptoms were present in 60 (13.98%) patients. They were..
References
Abdalazeem, None
Ahmed Y Abdelaziz, None
Asem, None
Aziz, None
Burton, Fort, Seoane, Hospitalization and Mortality among Black Patients and White Patients with Covid-19, N Engl J Med, doi:10.1056/NEJMsa2011686
Chan, Biostatistics 103: qualitative data -tests of independence, Singapore Med J
Chan, Biostatistics 202: logistic regression analysis, Singapore Med J
Ehab, Mostafa, None
Elgarem, None
Elsayed, None
Feng, Zheng, Yan, Rios, Targher et al., COVID-19 and Liver Dysfunction: Current Insights and Emergent Therapeutic Strategies, J Clin Transl Hepatol, doi:10.14218/JCTH.2020.00018
Fouad, None
Frater, Zini, Onofrio, Rogers, Chan, Biostatistics 102: quantitative data--parametric & non-parametric tests, doi:10.1111/ijlh.13229
Ghoda, Ghoda, Liver Injury in COVID-19 Infection: A Systematic Review, Cureus, doi:10.7759/cureus.9487
Hassany, None
Ibrahem, None
Jothimani, Venugopal, Abedin, Kaliamoorthy, Rela, COVID-19 and the liver, J Hepatol, doi:10.1016/j.jhep.2020.06.006
Kassas, None
Kulkarni, Kumar, Tevethia, Premkumar, Arab et al., Systematic review with meta-analysis: liver manifestations and outcomes in COVID-19, Aliment Pharmacol Ther, doi:10.1111/apt.15916
Kumar, Harne, Mukherjee, Gupta, Masood et al., Transaminitis is an indicator of mortality in patients with COVID-19: A retrospective cohort study, World J Hepatol, doi:10.4254/wjh.v12.i9.619
Li, Regan, Fajnzylber, Coxen, Corry et al., Liver Fibrosis Index FIB-4 Is Associated With Mortality in COVID-19, Hepatol Commun, doi:10.1002/hep4.1650
Liu, Yang, Wang, Zheng, Tang, Liver injury could be associated with severe disease in COVID-19 patients: a meta-analysis, Eur J Gastroenterol Hepatol, doi:10.1097/MEG.0000000000001953
Luo, Zhang, Xu, Don't Overlook Digestive Symptoms in Patients With 2019 Novel Coronavirus Disease (COVID-19), Clin Gastroenterol Hepatol, doi:10.1016/j.cgh.2020.03.043
Maher, None
Mohammed A Medhat, None
Musa, Hepatic and gastrointestinal involvement in coronavirus disease 2019 (COVID-19): What do we know till now?, Arab J Gastroenterol, doi:10.1016/j.ajg.2020.03.002
Nobel, Phipps, Zucker, Lebwohl, Wang et al., Gastrointestinal Symptoms and Coronavirus Disease 2019: A Case-Control Study From the United States, Gastroenterology, doi:10.1053/j.gastro.2020.04.017
Omran, None
Parasa, Desai, Chandrasekar, Patel, Kennedy et al., Prevalence of Gastrointestinal Symptoms and Fecal Viral Shedding in Patients With Coronavirus Disease 2019: A Systematic Review and Meta-analysis, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.11335
Phipps, Barraza, Lasota, Sobieszczyk, Pereira et al., Acute Liver Injury in COVID-19: Prevalence and Association with Clinical Outcomes in a Large U.S. Cohort, Hepatology, doi:10.1002/hep.31404
Ponziani, Zompo, Nesci, Santopaolo, Ianiro et al., Gemelli against COVID-19" group. Liver involvement is not associated with mortality: results from a large cohort of SARS-CoV-2-positive patients, Aliment Pharmacol Ther, doi:10.1111/apt.15996
Rateba, None
Redd, Zhou, Hathorn, Mccarty, Bazarbashi et al., Prevalence and Characteristics of Gastrointestinal Symptoms in Patients With Severe Acute Respiratory Syndrome Coronavirus 2 Infection in the United States: A Multicenter Cohort Study, Gastroenterology, doi:10.1053/j.gastro.2020.04.045
Rentsch, Kidwai-Khan, Tate, Park, King et al., Covid-19
Sterling, Lissen, Clumeck, Sola, Correa et al., Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection, Hepatology, doi:10.1002/hep.21178
Sterling, Oakes, Gal, Stevens, Dewit et al., The Fibrosis-4 Index Is Associated With Need for Mechanical Ventilation and 30-Day Mortality in Patients Admitted With Coronavirus Disease 2019, J Infect Dis, doi:10.1093/infdis/jiaa550
Villapol, Gastrointestinal symptoms associated with COVID-19: impact on the gut microbiome, Transl Res, doi:10.1016/j.trsl.2020.08.004
Wan, Wang, Su, Zhang, Jin et al., Digestive symptoms and liver injury in patients with coronavirus disease 2019 (COVID-19): A systematic review with meta-analysis, JGH Open, doi:10.1002/jgh3.12428
Wang, Qiu, Liu, Wang, Zhao, The liver injury and gastrointestinal symptoms in patients with Coronavirus Disease 19: A systematic review and meta-analysis, Clin Res Hepatol Gastroenterol, doi:10.1016/j.clinre.2020.04.012
Wijarnpreecha, Ungprasert, Panjawatanan, Harnois, Zaver et al., COVID-19 and liver injury: a meta-analysis, Eur J Gastroenterol Hepatol, doi:10.1097/MEG.0000000000001817
Wu, Li, Guo, Yoshida, Mendez-Sanchez et al., Incidence, risk factors, and prognosis of abnormal liver biochemical tests in COVID-19 patients: a systematic review and meta-analysis, Hepatol Int, doi:10.1007/s12072-020-10074-6
Wu, Yang, A meta-analysis of the impact of COVID-19 on liver dysfunction, Eur J Med Res, doi:10.1186/s40001-020-00454-x
Xing, Dong, Ren, Chen, Zeng et al., Liver Chemistries in Patients with COVID-19 Who Discharged alive or Died: A Meta-analysis, Hepatol Commun, doi:10.1002/hep4.1585
Youssef, Hussein, Attia, Elshazli, Zora et al., COVID-19 and liver dysfunction: A systematic review and meta-analysis of retrospective studies, J Med Virol, doi:10.1002/jmv.26055
Zhong, Xu, Yang, Shen, Wang et al., COVID-19-associated gastrointestinal and liver injury: clinical features and potential mechanisms, Signal Transduct Target Ther, doi:10.1038/s41392-020-00373-7
Zhou, Zhao, Shu, Han, Chen et al., Effect of Gastrointestinal Symptoms in Patients With COVID-19, Gastroenterology, doi:10.1053/j.gastro.2020.03.020
DOI record:
{
"DOI": "10.3748/wjg.v27.i40.6951",
"ISSN": [
"1007-9327"
],
"URL": "http://dx.doi.org/10.3748/wjg.v27.i40.6951",
"author": [
{
"affiliation": [],
"family": "Shousha",
"given": "Hend Ibrahim",
"sequence": "first"
},
{
"affiliation": [],
"family": "Afify",
"given": "Shimaa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Maher",
"given": "Rabab",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Asem",
"given": "Noha",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fouad",
"given": "Eman",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mostafa",
"given": "Ehab F",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Medhat",
"given": "Mohammed A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abdalazeem",
"given": "Amr",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Elmorsy",
"given": "Hazem",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Aziz",
"given": "Miriam M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mohammed",
"given": "Rateba S",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ibrahem",
"given": "Mohamed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Elgarem",
"given": "Hassan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Omran",
"given": "Dalia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hassany",
"given": "Mohamed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Elsayed",
"given": "Bassem",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abdelaziz",
"given": "Ahmed Y",
"sequence": "additional"
},
{
"affiliation": [],
"family": "El Kassas",
"given": "Mohamed",
"sequence": "additional"
}
],
"container-title": [
"World Journal of Gastroenterology"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
10,
27
]
],
"date-time": "2021-10-27T06:41:45Z",
"timestamp": 1635316905000
},
"deposited": {
"date-parts": [
[
2021,
10,
27
]
],
"date-time": "2021-10-27T06:43:23Z",
"timestamp": 1635317003000
},
"indexed": {
"date-parts": [
[
2021,
12,
16
]
],
"date-time": "2021-12-16T10:28:34Z",
"timestamp": 1639650514460
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "print",
"value": "1007-9327"
}
],
"issue": "40",
"issued": {
"date-parts": [
[
2021,
10,
28
]
]
},
"journal-issue": {
"issue": "40"
},
"link": [
{
"URL": "https://www.wjgnet.com/1007-9327/full/v27/i40/6951.htm",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "2060",
"original-title": [],
"page": "6951-6966",
"prefix": "10.3748",
"published": {
"date-parts": [
[
2021,
10,
28
]
]
},
"published-print": {
"date-parts": [
[
2021,
10,
28
]
]
},
"publisher": "Baishideng Publishing Group Inc.",
"reference": [
{
"DOI": "10.1016/j.ajg.2020.03.002",
"doi-asserted-by": "publisher",
"key": "B1"
},
{
"DOI": "10.1002/jmv.26055",
"doi-asserted-by": "publisher",
"key": "B2"
},
{
"DOI": "10.14218/JCTH.2020.00018",
"doi-asserted-by": "publisher",
"key": "B3"
},
{
"DOI": "10.1002/hep.31404",
"doi-asserted-by": "publisher",
"key": "B4"
},
{
"DOI": "10.7759/cureus.9487",
"doi-asserted-by": "publisher",
"key": "B5"
},
{
"DOI": "10.1016/j.jhep.2020.06.006",
"doi-asserted-by": "publisher",
"key": "B6"
},
{
"DOI": "10.4254/wjh.v12.i9.619",
"doi-asserted-by": "publisher",
"key": "B7"
},
{
"DOI": "10.1038/s41392-020-00373-7",
"doi-asserted-by": "publisher",
"key": "B8"
},
{
"DOI": "10.1136/gutjnl-2020-320953",
"doi-asserted-by": "publisher",
"key": "B9"
},
{
"DOI": "10.1016/j.trsl.2020.08.004",
"doi-asserted-by": "publisher",
"key": "B10"
},
{
"DOI": "10.1002/hep.21178",
"doi-asserted-by": "publisher",
"key": "B11"
},
{
"DOI": "10.1111/ijlh.13229",
"doi-asserted-by": "publisher",
"key": "B12"
},
{
"key": "B13",
"unstructured": "Ministry of Health and Population, Egypt Management protocol for COVID-19 Patients. [cited 30 May 2020]. Available from: https://www.elwatannews.com/data/iframe/pdf/17175200761591035127.pdf"
},
{
"key": "B14",
"unstructured": "Chan YH. Biostatistics 102: quantitative data--parametric & non-parametric tests. Singapore Med J 2003; 44: 391-396"
},
{
"key": "B15",
"unstructured": "Chan YH. Biostatistics 103: qualitative data - tests of independence. Singapore Med J 2003; 44: 498-503"
},
{
"key": "B16",
"unstructured": "Chan YH. Biostatistics 202: logistic regression analysis. Singapore Med J 2004; 45: 149-153"
},
{
"DOI": "10.1097/MEG.0000000000001817",
"doi-asserted-by": "publisher",
"key": "B17"
},
{
"DOI": "10.1186/s40001-020-00454-x",
"doi-asserted-by": "publisher",
"key": "B18"
},
{
"DOI": "10.1002/hep4.1585",
"doi-asserted-by": "publisher",
"key": "B19"
},
{
"DOI": "10.1007/s12072-020-10074-6",
"doi-asserted-by": "publisher",
"key": "B20"
},
{
"DOI": "10.1097/MEG.0000000000001953",
"doi-asserted-by": "publisher",
"key": "B21"
},
{
"DOI": "10.1111/apt.15916",
"doi-asserted-by": "publisher",
"key": "B22"
},
{
"DOI": "10.1111/apt.15996",
"doi-asserted-by": "publisher",
"key": "B23"
},
{
"DOI": "10.1093/infdis/jiaa550",
"doi-asserted-by": "publisher",
"key": "B24"
},
{
"DOI": "10.1002/hep4.1650",
"doi-asserted-by": "publisher",
"key": "B25"
},
{
"DOI": "10.1101/2020.04.09.20059964",
"doi-asserted-by": "publisher",
"key": "B26"
},
{
"DOI": "10.1056/NEJMsa2011686",
"doi-asserted-by": "publisher",
"key": "B27"
},
{
"DOI": "10.1016/j.clinre.2020.04.012",
"doi-asserted-by": "publisher",
"key": "B28"
},
{
"DOI": "10.1016/j.cgh.2020.03.043",
"doi-asserted-by": "publisher",
"key": "B29"
},
{
"DOI": "10.1002/jgh3.12428",
"doi-asserted-by": "publisher",
"key": "B30"
},
{
"DOI": "10.1001/jamanetworkopen.2020.11335",
"doi-asserted-by": "publisher",
"key": "B31"
},
{
"DOI": "10.1053/j.gastro.2020.04.045",
"doi-asserted-by": "publisher",
"key": "B32"
},
{
"DOI": "10.1053/j.gastro.2020.04.017",
"doi-asserted-by": "publisher",
"key": "B33"
},
{
"DOI": "10.1053/j.gastro.2020.03.020",
"doi-asserted-by": "publisher",
"key": "B34"
}
],
"reference-count": 34,
"references-count": 34,
"relation": {},
"score": 1,
"short-container-title": [
"WJG"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Gastroenterology",
"General Medicine"
],
"subtitle": [],
"title": [
"Hepatic and gastrointestinal disturbances in Egyptian patients infected with coronavirus disease 2019: A multicentre cohort study"
],
"type": "journal-article",
"volume": "27"
}
shousha