Lifestyle, course of COVID-19, and risk of Long-COVID in non-hospitalized patients
et al., Frontiers in Medicine, doi:10.3389/fmed.2022.1036556, Oct 2022
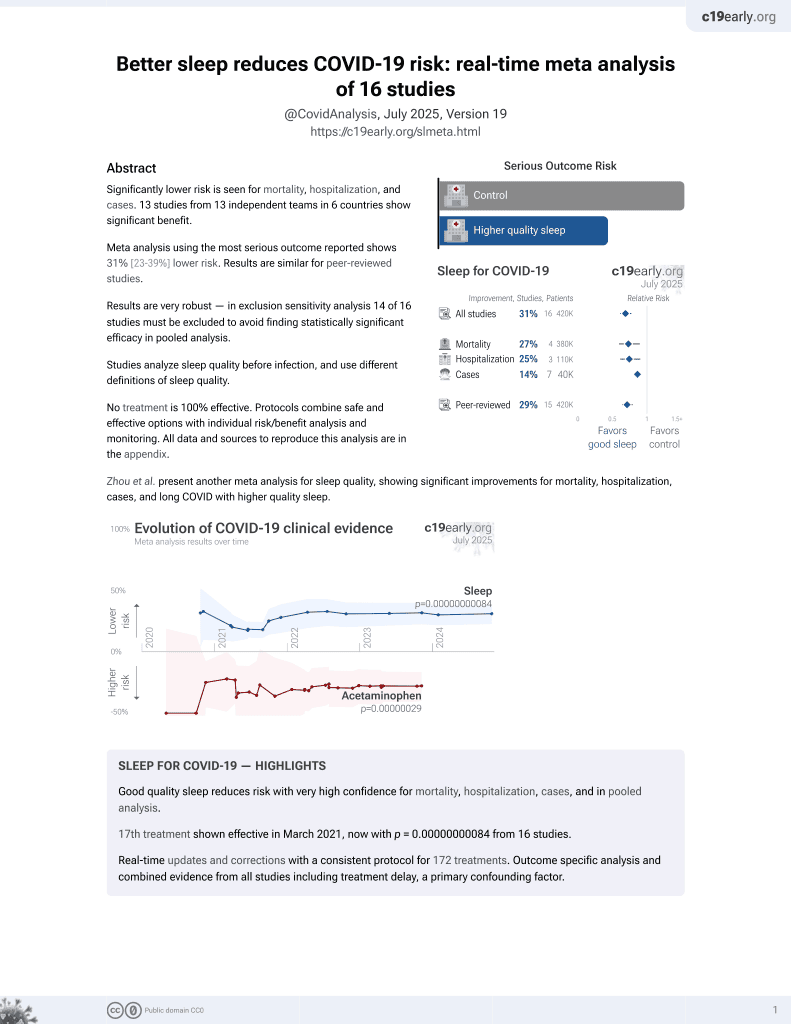
Sleep for COVID-19
18th treatment shown to reduce risk in
March 2021, now with p = 0.00000000084 from 16 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 1,847 COVID+ patients in Poland, showing lower moderate/severe cases with improved sleep, without statistical significance. Hospitalized patients were excluded.
Study covers exercise and sleep.
|
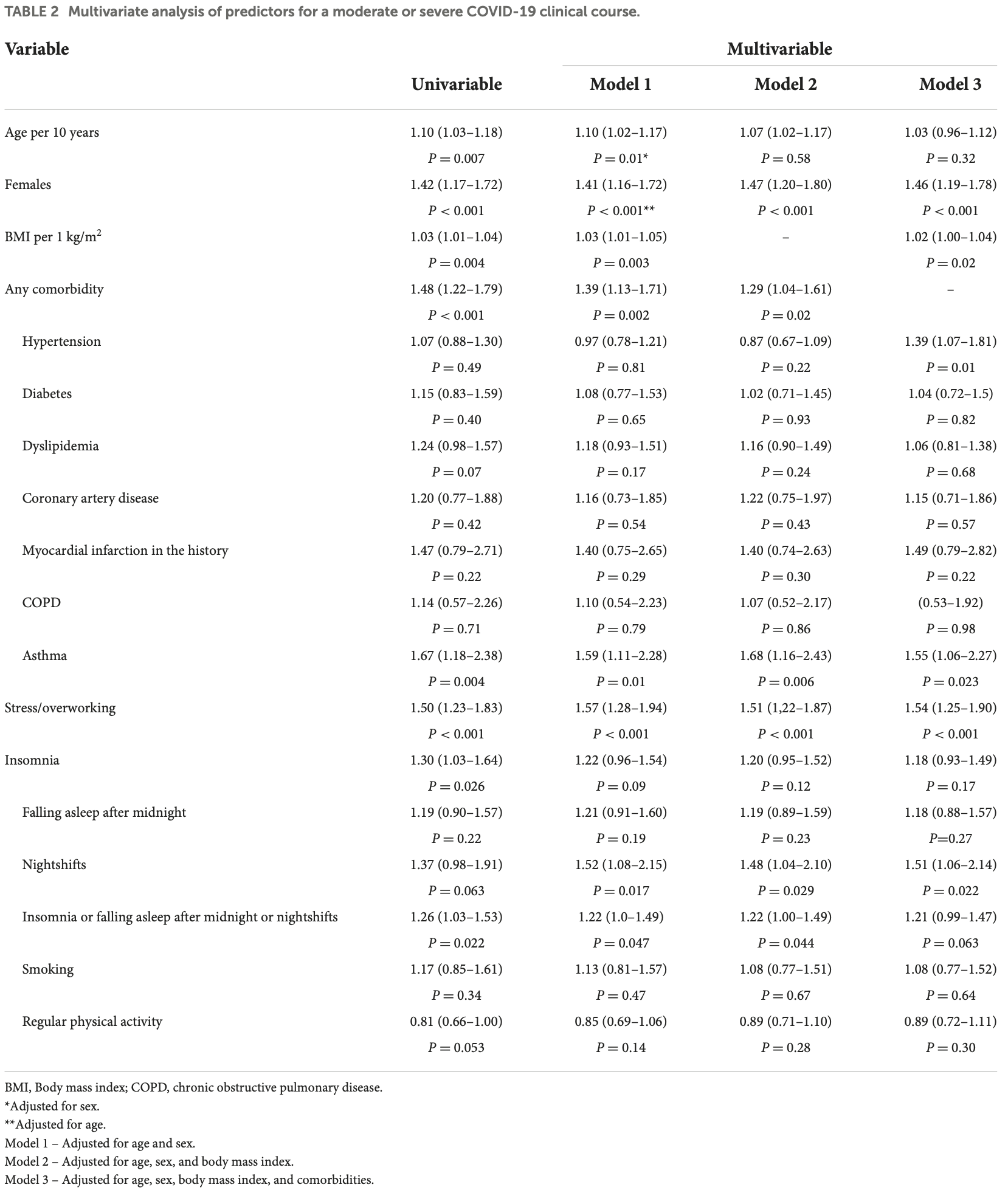
risk of moderate/severe case, 17.4% lower, OR 0.83, p = 0.06, improved sleep 1,225, worse sleep 622, adjusted per study, inverted to make OR<1 favor improved sleep, higher quality sleep vs. insomnia or falling asleep after midnight or nightshifts, multivariable, model 3, RR approximated with OR.
|
|
risk of long COVID, 7.4% lower, OR 0.93, p = 0.51, improved sleep 1,015, worse sleep 502, adjusted per study, inverted to make OR<1 favor improved sleep, higher quality sleep vs. insomnia or falling asleep after midnight or nightshifts, multivariable, model 3, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Pływaczewska-Jakubowska et al., 24 Oct 2022, retrospective, Poland, peer-reviewed, median age 51.0, 5 authors, study period May 2020 - January 2022.
Contact: joanna.kapusta@umed.lodz.pl, ma.babicki@gmail.com.
Lifestyle, course of COVID-, and risk of Long-COVID in non-hospitalized patients
Introduction: The coronavirus disease (COVID) pandemic remains a great challenge for the healthcare system. The widely reported prolonged signs and symptoms resulting from severe acute respiratory syndrome coronavirus (SARS-CoV-) infection (Long-COVID) require medical care. The aim of the study was to assess factors, including lifestyle variables, related to the course of COVID-infection and to assess their impact on prolonged symptoms in non-hospitalized patients with COVID-. Methods: A total of , ( men and , women) non-hospitalized participants of the STOP-COVID registry of the PoLoCOV-Study who, following the COVID-, underwent check-up examinations at the cardiology outpatient clinic were included in the analysis. Results: The study participants (median age [ -] years) were evaluated at . ( . -. ) weeks following the diagnosis of COVID-. Female sex (odds ratio [OR] . [ % CI . -. ]), body mass index (BMI; per kg/m : . [ . -. ]), hypertension ( . [ . -. ]), asthma ( . [ . -. ]), stress or overworking ( . [ . -. ]), and nightshift work ( . [ . -. ]) were independently related to the severity of symptoms during acute phase of the COVID-infection. The Long-COVID syndrome was independently related to the female sex ( . [ . -. ]), history of myocardial infarction ( . [ . -. ]), asthma ( . [ . -. ]), and severe course of the acute phase of the COVID-infection ( . [ . -. ]).
Conclusion: Female sex, BMI, asthma, hypertension, nightshifts, and stress or overworking are significantly related to the severity of the acute phase of the COVID-infection, while female sex, asthma, history of myocardial infarction, and the severity of symptoms in the acute phase of COVID-are the predictors of Long-COVID in non-hospitalized patients. We did not find an independent relation between Long-COVID and the studied lifestyle factors.
we have also observed an association between higher values of BMI and a symptomatic course of COVID-19. Furthermore, it seems that obesity-related chronic inflammations and processes of immunometabolism not only promote a severe clinical course of acute SARS-CoV-2 infection but also contribute to a Long-COVID-19 syndrome (38) . However, we did not confirm this in
Ethics statement The studies involving human participants were reviewed and approved by Bioethics Committee of Lodz Regional Medical Chamber-No. 0115/2021. The patients/participants provided their written informed consent to participate in this study.
Author contributions Conceptualization: MC and MP-J. Data curation and methodology: MC, MP-J, and PJ. Formal analysis: MB and JK. Investigation, visualization, and writing-review and editing: MC, MP-J, MB, JK, and PJ. Project administration: MC. Supervision and validation: MC and PJ. All authors have read and agreed to the published version of the manuscript.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer,..
References
Augustin, Schommers, Stecher, Dewald, Gieselmann et al., Post-COVID syndrome in non-hospitalised patients with COVID-19: a longitudinal prospective cohort study, Lancet Reg Health Eur, doi:10.1016/j.lanepe.2021.100122
Cai, Chen, Wang, Luo, Liu et al., Obesity and COVID-19 severity in a designated hospital in Shenzhen, China, Diabetes Care, doi:10.2337/dc20-0576
Carvalho-Schneider, Laurent, Lemaignen, Beaufils, Bourbao-Tournois et al., Follow-up of adults with noncritical COVID-19 two months after symptom onset, Clin Microbiol Infect, doi:10.1016/j.cmi.2020.09.052
Chiappetta, Sharma, Bottino, Stier, COVID-19 and the role of chronic inflammation in patients with obesity, Int J Obes (Lond), doi:10.1038/s41366-020-0597-4
Chl, Association of timing and balance of physical activity and rest/sleep with risk of COVID-19: a UK biobank study, BMC Med Genomics, doi:10.1186/s12920-021-00887-1
Colpani, Baena, Jaspers, Van Dijk, Farajzadegan et al., Lifestyle factors, cardiovascular disease and all-cause mortality in middleaged and elderly women: a systematic review and meta-analysis, Eur J Epidemiol, doi:10.1007/s10654-018-0374-z
Conti, Younes, Coronavirus COV-19/SARS-CoV-2 affects women less than men: clinical response to viral infection, J Biol Regul Homeost Agents, doi:10.23812/Editorial-Conti-3
Evans, Mcauley, Harrison, Shikotra, Singapuri et al., COVID Collaborative Group. Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): a UK multicentre, prospective cohort study, Lancet Respir Med, doi:10.1016/S2213-2600(21)00383-0
Fernández-De-Las-Peñas, Palacios-Ceña, Gómez-Mayordomo, Florencio, Cuadrado et al., Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: a systematic review and meta-analysis, Eur J Intern Med, doi:10.1016/j.ejim.2021.06.009
Gargiullo, Morbid obesity as a risk factor for hospitalization and death due to 2009 pandemic influenza A(H1N1) disease, PLoS ONE, doi:10.1128/mBio.03341-19
Garrigues, Janvier, Kherabi, Bot, Hamon et al., Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19, J Infect, doi:10.1016/j.jinf.2020.08.029
Gomez, Du-Fay-De-Lavallaz, Fugar, Sarau, Simmons et al., Considering how biological sex impacts immune responses and COVID-19 outcomes, J Womens Health (Larchmt), doi:10.1038/s41577-020-0348-8
Goërtz, Van Herck, Delbressine, Vaes, Meys et al., Persistent symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome?, ERJ Open Res, doi:10.1183/23120541.00542-2020
Halasz, Leoni, Villani, Nolli, Villani, Obesity, overweight and survival in critically ill patients with SARS-CoV-2 pneumonia: is there an obesity paradox? Preliminary results from Italy, Eur J Prev Cardiol, doi:10.1177/2047487320939675
Halpin, Mcivor, Whyatt, Adams, Harvey et al., Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation, J Med Virol, doi:10.1002/jmv.26368
Hamer, Kivimäki, Gale, Batty, Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: a community-based cohort study of 387,109 adults in UK, Brain Behav Immun, doi:10.1016/j.bbi.2020.05.059
Ho, Sepand, Bigdelou, Shekarian, Esfandyarpour et al., The immune response to COVID-19: does sex matter?, Immunology, doi:10.1111/imm.13487
Khatib, Ananthegowda, Elshafei, El-Zeer, Abdaljawad et al., Predictors of mortality and morbidity in critically ill COVID-19 patients: an experience from a low mortality country, Health Sci Rep, doi:10.1002/hsr2.542
Loosen, Jensen, Tanislav, Luedde, Roderburg et al., Obesity and lipid me-tabolism disorders determine the risk for development of long COVID syndrome: a cross-sectional study from 50,402 COVID-19 patients, Infection, doi:10.1007/s15010-022-01784-0
Lovre, Bateman, Sherman, Fonseca, Lefante et al., Acute estradiol and progesterone therapy in hospitalised adults to reduce COVID-19 severity: a randomised control trial, BMJ Open, doi:10.1136/bmjopen-2021-053684
Malik, Patel, Pinto, Jaiswal, Tirupathi et al., Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)-A systematic review and meta-analysis, J Med Virol, doi:10.1002/jmv.27309
Nair, Soliman, Masalamani, Sanctis, Nashwan et al., Clinical outcome of eosinophilia in patients with COVID-19: a controlled study, Acta Biomed
Nieman, Soroush, Naghipour, Heidarpour, Abdollahzad et al., Coronavirus disease-2019: A tocsin to our aging, unfit, corpulent, and immunodeficient society, J Sport Health Sci, doi:10.15280/jlm.2022.12.1.56
Nieman, Wentz, Segerstrom, Miller, Vai et al., Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis, J Sport Health Sci, doi:10.1016/S2215-0366(21)00232-7
Nyberg, Singh-Manoux, Pentti, Madsen, Sabia et al., Adherence to healthy lifestyles and incidence of diabetes and mortality among individuals with diabetes: a systematic review and meta-analysis of prospective studies, J Epidemiol Community Health, doi:10.1136/jech-2019-213415
Pan, Liu, Wang, Guo, Hao et al., Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China, JAMA, doi:10.1001/jama.2020.6130
Peters, Mcgrath, Hawkins, Hastie, Levy et al., Blood Institute Severe Asthma Research Program. Plasma interleukin-6 concentrations, metabolic dysfunction, and asthma severity: a cross-sectional analysis of two cohorts, Lancet Respir Med, doi:10.1016/S2213-2600(16)30048-0
Phung, Wang, Rutherford, Huang, Chu, Body mass index and risk of pneumonia: a systematic review and meta-analysis, Obes Rev, doi:10.1111/obr.12055
Pradhan, Olsson, Sex differences in severity and mortality from COVID-19: are males more vulnerable?, Biol Sex Differ, doi:10.1186/s13293-020-00330-7
Rowlands, Kloecker, Chudasama, Davies, Dawkins, None
Salari, Hosseinian-Far, Jalali, Vaisi-Raygani, Rasoulpoor et al., Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and metaanalysis, Clin Microbiol Infect, doi:10.1016/j.cmi.2021.11.002
Sha, Qie, Yao, Sun, Wang et al., Sex differences on clinical characteristics, severity, and mortality in adult patients with COVID-19: a multicentre retrospective study, Front. Med, doi:10.3389/fmed.2021.607059
Stefan, Schick, Hu ; Morgan, Bramley, Fowlkes et al., Causes, characteristics, and consequences of metabolically unhealthy normal weight in humans, Cell Metab, doi:10.1016/j.cmet.2017.07.008
Sudre, Murray, Varsavsky, Graham, Penfold et al., Post-COVID syndrome symptoms, functional disability, and clinical severity phenotypes in hospitalized and nonhospitalized individuals: a cross-sectional evaluation from a community COVID rehabilitation service, J Med Virol, doi:10.1002/jmv.27456
Visseren, Mach, Smulders, Carballo, Koskinas et al., ESC Scientific Document Group 2021. ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC), Rev Esp Cardiol (Engl Ed), doi:10.1016/j.rec.2022.04.003
Wang, Deng, Ou, Liang, Wang et al., Clinical symptoms, comorbidities and complications in severe and non-severe patients with COVID-19: A systematic review and meta-analysis without cases duplication, Postgrad Med, doi:10.1016/j.jinf.2021.01.004
Yang, Hu, Zhu, Petrilli, Jones et al., Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study, J Med Virol, doi:10.1136/bmj.m1966
Yang, Yu, Xu, Shu, Xia et al., Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study, Lancet Respir Med, doi:10.1016/S2213-2600(20)30079-5
Yang, Zheng, Gou, Pu, Chen et al., Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis, Int J Infect Dis, doi:10.1016/S0140-6736(20)30558-4
DOI record:
{
"DOI": "10.3389/fmed.2022.1036556",
"ISSN": [
"2296-858X"
],
"URL": "http://dx.doi.org/10.3389/fmed.2022.1036556",
"abstract": "<jats:sec><jats:title>Introduction</jats:title><jats:p>The coronavirus disease (COVID) 2019 pandemic remains a great challenge for the healthcare system. The widely reported prolonged signs and symptoms resulting from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (Long-COVID) require medical care. The aim of the study was to assess factors, including lifestyle variables, related to the course of COVID-19 infection and to assess their impact on prolonged symptoms in non-hospitalized patients with COVID-19.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>A total of 1,847 (637 men and 1,210 women) non-hospitalized participants of the STOP-COVID registry of the PoLoCOV-Study who, following the COVID-19, underwent check-up examinations at the cardiology outpatient clinic were included in the analysis.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>The study participants (median age 51 [41–62] years) were evaluated at 13.4 (8.4–23.6) weeks following the diagnosis of COVID-19. Female sex (odds ratio [OR] 1.46 [95% CI 1.19–1.78]), body mass index (BMI; per 1 kg/m<jats:sup>2</jats:sup>: 1.02 [1.00–1.04]), hypertension (1.39 [1.07–1.81]), asthma (1.55 [1.06–2.27]), stress or overworking (1.54 [1.25–1.90]), and nightshift work (1.51 [1.06–2.14]) were independently related to the severity of symptoms during acute phase of the COVID-19 infection. The Long-COVID syndrome was independently related to the female sex (1.42 [1.13–1.79]), history of myocardial infarction (2.57 [1.04–6.32]), asthma (1.56 [1.01–2.41]), and severe course of the acute phase of the COVID-19 infection (2.27 [1.82–2.83]).</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>Female sex, BMI, asthma, hypertension, nightshifts, and stress or overworking are significantly related to the severity of the acute phase of the COVID-19 infection, while female sex, asthma, history of myocardial infarction, and the severity of symptoms in the acute phase of COVID-19 are the predictors of Long-COVID in non-hospitalized patients. We did not find an independent relation between Long-COVID and the studied lifestyle factors.</jats:p></jats:sec>",
"alternative-id": [
"10.3389/fmed.2022.1036556"
],
"author": [
{
"affiliation": [],
"family": "Pływaczewska-Jakubowska",
"given": "Magdalena",
"sequence": "first"
},
{
"affiliation": [],
"family": "Chudzik",
"given": "Michał",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Babicki",
"given": "Mateusz",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kapusta",
"given": "Joanna",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jankowski",
"given": "Piotr",
"sequence": "additional"
}
],
"container-title": "Frontiers in Medicine",
"container-title-short": "Front. Med.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2022,
10,
24
]
],
"date-time": "2022-10-24T04:52:35Z",
"timestamp": 1666587155000
},
"deposited": {
"date-parts": [
[
2022,
10,
24
]
],
"date-time": "2022-10-24T04:52:41Z",
"timestamp": 1666587161000
},
"indexed": {
"date-parts": [
[
2022,
10,
25
]
],
"date-time": "2022-10-25T05:08:47Z",
"timestamp": 1666674527064
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
10,
24
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
10,
24
]
],
"date-time": "2022-10-24T00:00:00Z",
"timestamp": 1666569600000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2022.1036556/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2022,
10,
24
]
]
},
"published-online": {
"date-parts": [
[
2022,
10,
24
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"key": "B1",
"unstructured": "2022"
},
{
"DOI": "10.1016/j.ejim.2021.06.009",
"article-title": "Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: a systematic review and meta-analysis",
"author": "Fernández-de-Las-Peñas",
"doi-asserted-by": "publisher",
"journal-title": "Eur J Intern Med",
"key": "B2",
"year": "2021"
},
{
"DOI": "10.1183/23120541.00542-2020",
"article-title": "Persistent symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome?",
"author": "Goërtz",
"doi-asserted-by": "publisher",
"first-page": "00542",
"journal-title": "ERJ Open Res.",
"key": "B3",
"volume": "6",
"year": "2020"
},
{
"key": "B4",
"unstructured": ""
},
{
"DOI": "10.1016/j.cmi.2020.09.052",
"article-title": "Follow-up of adults with noncritical COVID-19 two months after symptom onset",
"author": "Carvalho-Schneider",
"doi-asserted-by": "publisher",
"first-page": "258",
"journal-title": "Clin Microbiol Infect.",
"key": "B5",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1016/j.jinf.2020.08.029",
"article-title": "Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19",
"author": "Garrigues",
"doi-asserted-by": "publisher",
"first-page": "e4",
"journal-title": "J Infect.",
"key": "B6",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.6130",
"article-title": "Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China",
"author": "Pan",
"doi-asserted-by": "publisher",
"first-page": "1915",
"journal-title": "JAMA.",
"key": "B7",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.3389/fmed.2021.607059",
"article-title": "Sex differences on clinical characteristics, severity, and mortality in adult patients with COVID-19: a multicentre retrospective study",
"author": "Sha",
"doi-asserted-by": "publisher",
"first-page": "607059",
"journal-title": "Front. Med.",
"key": "B8",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2020.03.017",
"article-title": "Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis",
"author": "Yang",
"doi-asserted-by": "publisher",
"first-page": "91",
"journal-title": "Int J Infect Dis.",
"key": "B9",
"volume": "94",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30558-4",
"article-title": "Comorbidities and multi-organ injuries in the treatment of COVID-19",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "e52",
"journal-title": "Lancet.",
"key": "B10",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/j.mayocp.2020.10.032",
"article-title": "Association of timing and balance of physical activity and rest/sleep with risk of COVID-19: a UK biobank study",
"author": "Rowlands",
"doi-asserted-by": "publisher",
"first-page": "156",
"journal-title": "Mayo Clin Proc.",
"key": "B11",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1186/s12920-021-00887-1",
"article-title": "Modifiable lifestyle factors and severe COVID-19 risk: a Mendelian randomisation study",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "38",
"journal-title": "BMC Med Genomics",
"key": "B12",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1038/s41591-021-01292-y",
"article-title": "Attributes and predictors of long COVID",
"author": "Sudre",
"doi-asserted-by": "publisher",
"first-page": "626",
"journal-title": "Nat Med.",
"key": "B13",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1002/jmv.27456",
"article-title": "Post-COVID syndrome symptoms, functional disability, and clinical severity phenotypes in hospitalized and nonhospitalized individuals: a cross-sectional evaluation from a community COVID rehabilitation service",
"author": "Sivan",
"doi-asserted-by": "publisher",
"first-page": "1419",
"journal-title": "J Med Virol.",
"key": "B14",
"volume": "94",
"year": "2022"
},
{
"DOI": "10.1016/S2213-2600(21)00383-0",
"article-title": "PHOSP-COVID Collaborative Group. Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): a UK multicentre, prospective cohort study",
"author": "Evans",
"doi-asserted-by": "publisher",
"first-page": "1275",
"journal-title": "Lancet Respir Med.",
"key": "B15",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.lanepe.2021.100122",
"article-title": "Post-COVID syndrome in non-hospitalised patients with COVID-19: a longitudinal prospective cohort study",
"author": "Augustin",
"doi-asserted-by": "publisher",
"first-page": "100122",
"journal-title": "Lancet Reg Health Eur.",
"key": "B16",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1002/jmv.27309",
"article-title": "Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)-A systematic review and meta-analysis",
"author": "Malik",
"doi-asserted-by": "publisher",
"first-page": "253",
"journal-title": "J Med Virol.",
"key": "B17",
"volume": "94",
"year": "2022"
},
{
"DOI": "10.1177/1557988320954021",
"article-title": "Men and COVID-19: a pathophysiologic review",
"author": "Lipsky",
"doi-asserted-by": "publisher",
"first-page": "1557988320954021",
"journal-title": "Am J Mens Health.",
"key": "B18",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1161/circ.142.suppl_3.17393",
"article-title": "Sex differences in COVID-19 hospitalization and mortality",
"author": "Gomez",
"doi-asserted-by": "publisher",
"first-page": "646",
"journal-title": "J Womens Health (Larchmt).",
"key": "B19",
"volume": "30",
"year": "2021"
},
{
"DOI": "10.1038/s41577-020-0348-8",
"article-title": "Considering how biological sex impacts immune responses and COVID-19 outcomes",
"author": "Scully",
"doi-asserted-by": "publisher",
"first-page": "442",
"journal-title": "Nat Rev Immunol.",
"key": "B20",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1186/s13293-020-00330-7",
"article-title": "Sex differences in severity and mortality from COVID-19: are males more vulnerable?",
"author": "Pradhan",
"doi-asserted-by": "publisher",
"first-page": "53",
"journal-title": "Biol Sex Differ.",
"key": "B21",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1111/imm.13487",
"article-title": "The immune response to COVID-19: does sex matter?",
"author": "Ho",
"doi-asserted-by": "publisher",
"first-page": "429",
"journal-title": "Immunology",
"key": "B22",
"volume": "166",
"year": "2022"
},
{
"DOI": "10.23812/Editorial-Conti-3",
"article-title": "Coronavirus COV-19/SARS-CoV-2 affects women less than men: clinical response to viral infection",
"author": "Conti",
"doi-asserted-by": "publisher",
"first-page": "339",
"journal-title": "J Biol Regul Homeost Agents",
"key": "B23",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.1136/bmjopen-2021-053684",
"article-title": "Acute estradiol and progesterone therapy in hospitalised adults to reduce COVID-19 severity: a randomised control trial",
"author": "Lovre",
"doi-asserted-by": "publisher",
"first-page": "e053684",
"journal-title": "BMJ Open.",
"key": "B24",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1186/s12992-020-00589-w",
"article-title": "Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis",
"author": "Salari",
"doi-asserted-by": "publisher",
"first-page": "57",
"journal-title": "Glob Health.",
"key": "B25",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.1016/j.cmi.2021.11.002",
"article-title": "Female gender is associated with long COVID syndrome: a prospective cohort study",
"author": "Bai",
"doi-asserted-by": "publisher",
"first-page": "611",
"journal-title": "Clin Microbiol Infect",
"key": "B26",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1016/j.rec.2022.04.003",
"article-title": "ESC Scientific Document Group 2021. ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC)",
"author": "Visseren",
"doi-asserted-by": "publisher",
"first-page": "429",
"journal-title": "Rev Esp Cardiol (Engl Ed).",
"key": "B27",
"volume": "75",
"year": "2022"
},
{
"DOI": "10.1016/j.cmet.2017.07.008",
"article-title": "Causes, characteristics, and consequences of metabolically unhealthy normal weight in humans",
"author": "Stefan",
"doi-asserted-by": "publisher",
"first-page": "292",
"journal-title": "Cell Metab",
"key": "B28",
"volume": "26",
"year": "2017"
},
{
"DOI": "10.1371/journal.pone.0009694",
"article-title": "Morbid obesity as a risk factor for hospitalization and death due to 2009 pandemic influenza A(H1N1) disease",
"author": "Morgan",
"doi-asserted-by": "publisher",
"first-page": "e9694",
"journal-title": "PLoS ONE.",
"key": "B29",
"volume": "5",
"year": "2010"
},
{
"DOI": "10.1128/mBio.03341-19",
"article-title": "Obesity-related microenvironment promotes emergence of virulent influenza virus strains",
"author": "Honce",
"doi-asserted-by": "publisher",
"first-page": "e03341",
"journal-title": "mBio",
"key": "B30",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1111/obr.12055",
"article-title": "Body mass index and risk of pneumonia: a systematic review and meta-analysis",
"author": "Phung",
"doi-asserted-by": "publisher",
"first-page": "839",
"journal-title": "Obes Rev.",
"key": "B31",
"volume": "14",
"year": "2013"
},
{
"DOI": "10.1002/jmv.26237",
"article-title": "Obesity aggravates COVID-19: a systematic review and meta-analysis",
"author": "Yang",
"doi-asserted-by": "publisher",
"first-page": "257",
"journal-title": "J Med Virol.",
"key": "B32",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1136/bmj.m1966",
"article-title": "Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study",
"author": "Petrilli C",
"doi-asserted-by": "publisher",
"journal-title": "BMJ",
"key": "B33",
"year": "2020"
},
{
"DOI": "10.2337/dc20-0576",
"article-title": "Obesity and COVID-19 severity in a designated hospital in Shenzhen, China",
"author": "Cai",
"doi-asserted-by": "publisher",
"first-page": "1392",
"journal-title": "Diabetes Care.",
"key": "B34",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1038/s41366-020-0597-4",
"article-title": "COVID-19 and the role of chronic inflammation in patients with obesity",
"author": "Chiappetta",
"doi-asserted-by": "publisher",
"first-page": "1790",
"journal-title": "Int J Obes (Lond).",
"key": "B35",
"volume": "44",
"year": "2020"
},
{
"DOI": "10.1177/2047487320939675",
"article-title": "Obesity, overweight and survival in critically ill patients with SARS-CoV-2 pneumonia: is there an obesity paradox? Preliminary results from Italy",
"author": "Halasz",
"doi-asserted-by": "publisher",
"first-page": "2047487320939675",
"journal-title": "Eur J Prev Cardiol.",
"key": "B36",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1007/s15010-022-01784-0",
"article-title": "Obesity and lipid me-tabolism disorders determine the risk for development of long COVID syndrome: a cross-sectional study from 50,402 COVID-19 patients",
"author": "Loosen",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Infection.",
"key": "B37",
"volume": "30",
"year": "2022"
},
{
"DOI": "10.1016/S2213-2600(16)30048-0",
"article-title": "Blood Institute Severe Asthma Research Program. Plasma interleukin-6 concentrations, metabolic dysfunction, and asthma severity: a cross-sectional analysis of two cohorts",
"author": "Peters",
"doi-asserted-by": "publisher",
"first-page": "574",
"journal-title": "Lancet Respir Med.",
"key": "B38",
"volume": "4",
"year": "2016"
},
{
"DOI": "10.1016/S2213-2600(20)30079-5",
"article-title": "Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study",
"author": "Yang",
"doi-asserted-by": "publisher",
"first-page": "475",
"journal-title": "Lancet Respir Med.",
"key": "B39",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1097/MD.0000000000023327",
"article-title": "Clinical symptoms, comorbidities and complications in severe and non-severe patients with COVID-19: A systematic review and meta-analysis without cases duplication",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "e23327",
"journal-title": "Medicine (Baltimore).",
"key": "B40",
"volume": "99",
"year": "2020"
},
{
"DOI": "10.1080/00325481.2020.1786964",
"article-title": "COVID-19 and comorbidities: a systematic review and meta-analysis",
"author": "Gold",
"doi-asserted-by": "publisher",
"first-page": "749",
"journal-title": "Postgrad Med.",
"key": "B41",
"volume": "132",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2021.01.004",
"article-title": "COVID19-ALC research group. Post-acute COVID-19 syndrome Incidence and risk factors: a Mediterranean cohort study",
"author": "Moreno-Pérez",
"doi-asserted-by": "publisher",
"first-page": "378",
"journal-title": "J Infect.",
"key": "B42",
"volume": "82",
"year": "2021"
},
{
"DOI": "10.1002/jmv.26368",
"article-title": "Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation",
"author": "Halpin",
"doi-asserted-by": "publisher",
"first-page": "1013",
"journal-title": "J Med Virol.",
"key": "B43",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1007/s10654-018-0374-z",
"article-title": "Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and meta-analysis",
"author": "Colpani",
"doi-asserted-by": "publisher",
"first-page": "831",
"journal-title": "Eur J Epidemiol.",
"key": "B44",
"volume": "33",
"year": "2018"
},
{
"DOI": "10.1001/jamainternmed.2020.0618",
"article-title": "Association of healthy lifestyle with years lived without major chronic diseases",
"author": "Nyberg",
"doi-asserted-by": "publisher",
"first-page": "760",
"journal-title": "JAMA Intern Med",
"key": "B45",
"volume": "180",
"year": "2020"
},
{
"DOI": "10.1136/jech-2019-213415",
"article-title": "Adherence to healthy lifestyles and incidence of diabetes and mortality among individuals with diabetes: a systematic review and meta-analysis of prospective studies",
"author": "Schlesinger",
"doi-asserted-by": "publisher",
"first-page": "481",
"journal-title": "J Epidemiol Community Health.",
"key": "B46",
"volume": "74",
"year": "2020"
},
{
"DOI": "10.1016/j.bbi.2020.05.059",
"article-title": "Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: a community-based cohort study of 387,109 adults in UK",
"author": "Hamer",
"doi-asserted-by": "publisher",
"first-page": "184",
"journal-title": "Brain Behav Immun.",
"key": "B47",
"volume": "87",
"year": "2020"
},
{
"DOI": "10.1016/j.jshs.2020.05.001",
"article-title": "Coronavirus disease-2019: A tocsin to our aging, unfit, corpulent, and immunodeficient society",
"author": "Nieman",
"doi-asserted-by": "publisher",
"first-page": "293",
"journal-title": "J Sport Health Sci.",
"key": "B48",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.15280/jlm.2022.12.1.56",
"article-title": "Examining lifestyle components in hospitalized COVID-19 patients, Iran 2021",
"author": "Soroush",
"doi-asserted-by": "publisher",
"first-page": "56",
"journal-title": "J Lifestyle Med.",
"key": "B49",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1016/j.jshs.2018.09.009",
"article-title": "The compelling link between physical activity and the body's defense system",
"author": "Nieman",
"doi-asserted-by": "publisher",
"first-page": "201",
"journal-title": "J Sport Health Sci.",
"key": "B50",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.1037/0033-2909.130.4.601",
"article-title": "Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry",
"author": "Segerstrom",
"doi-asserted-by": "publisher",
"first-page": "601",
"journal-title": "Psychol Bull.",
"key": "B51",
"volume": "130",
"year": "2004"
},
{
"DOI": "10.1016/S2215-0366(21)00232-7",
"article-title": "Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis",
"author": "Vai",
"doi-asserted-by": "publisher",
"first-page": "797",
"journal-title": "Lancet Psychiatry.",
"key": "B52",
"volume": "8",
"year": "2021"
},
{
"article-title": "Clinical outcome of eosinophilia in patients with COVID-19: a controlled study",
"author": "Nair",
"first-page": "e2020165",
"journal-title": "Acta Biomed.",
"key": "B53",
"volume": "91",
"year": "2020"
},
{
"DOI": "10.1002/hsr2.542",
"article-title": "Predictors of mortality and morbidity in critically ill COVID-19 patients: an experience from a low mortality country",
"author": "Khatib",
"doi-asserted-by": "publisher",
"first-page": "e542",
"journal-title": "Health Sci Rep.",
"key": "B54",
"volume": "5",
"year": "2022"
}
],
"reference-count": 54,
"references-count": 54,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2022.1036556/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Lifestyle, course of COVID-19, and risk of Long-COVID in non-hospitalized patients",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "9"
}
plywaczewska