Modifiable lifestyle factors and severe COVID-19 risk: a Mendelian randomisation study
et al., BMC Medical Genomics, doi:10.1186/s12920-021-00887-1, Feb 2021
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Mendelian randomization study showing lower risk of severe COVID-19 with physical activity.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
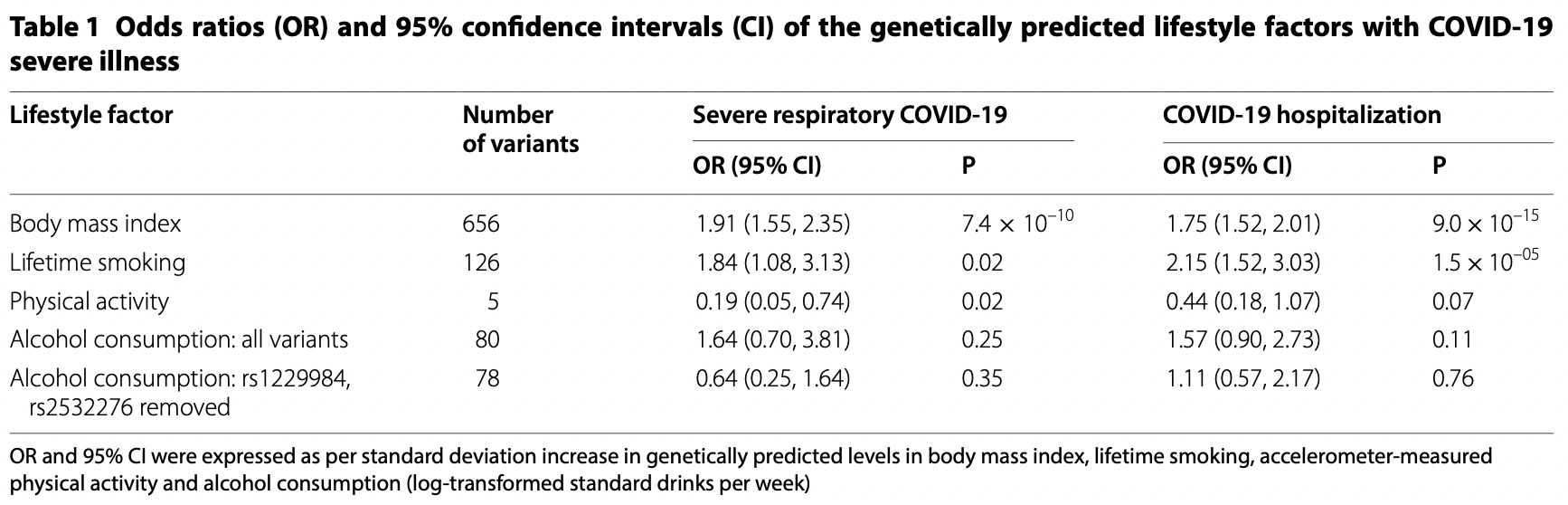
risk of severe case, 81.0% lower, OR 0.19, p = 0.02, RR approximated with OR.
|
|
risk of hospitalization, 56.0% lower, OR 0.44, p = 0.07, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Li et al., 3 Feb 2021, retrospective, United Kingdom, peer-reviewed, 2 authors, per SD increase.
Contact: shuai.li@unimelb.edu.au (corresponding author).
Modifiable lifestyle factors and severe COVID-19 risk: a Mendelian randomisation study
BMC Medical Genomics, doi:10.1186/s12920-021-00887-1
Background: Lifestyle factors including obesity and smoking are suggested to be correlated with increased risk of COVID-19 severe illness or related death. However, whether these relationships are causal is not well known; neither for the relationships between COVID-19 severe illness and other common lifestyle factors, such as physical activity and alcohol consumption. Methods: Genome-wide significant genetic variants associated with body mass index (BMI), lifetime smoking, physical activity and alcohol consumption identified by large-scale genome-wide association studies (GWAS) of up to 941,280 individuals were selected as instrumental variables. Summary statistics of the genetic variants on severe illness of COVID-19 were obtained from GWAS analyses of up to 6492 cases and 1,012,809 controls. Two-sample Mendelian randomisation analyses were conducted. Results: Both per-standard deviation (SD) increase in genetically predicted BMI and lifetime smoking were associated with about two-fold increased risks of severe respiratory COVID-19 and COVID-19 hospitalization (all P < 0.05). Per-SD increase in genetically predicted physical activity was associated with decreased risks of severe respiratory COVID-19 (odds ratio [OR] = 0.19; 95% confidence interval [CI], 0.05, 0.74; P = 0.02), but not with COVID-19 hospitalization (OR = 0.44; 95% CI 0.18, 1.07; P = 0.07). No evidence of association was found for genetically predicted alcohol consumption. Similar results were found across robust Mendelian randomisation methods.
Conclusions: Evidence is found that BMI and smoking causally increase and physical activity might causally decrease the risk of COVID-19 severe illness. This study highlights the importance of maintaining a healthy lifestyle in protecting from COVID-19 severe illness and its public health value in fighting against COVID-19 pandemic.
Supplementary Information The online version contains supplementary material available at https ://doi. org/10.1186/s1292 0-021-00887 -1. Additional file 1: Supplementary Tables 1-4 . Summary statistics for genetic instrumental variables of the four lifestyle factors. Additional file 2: Supplementary Table 5 . Parameter values used in statistical power analysis. Additional file 3: Supplementary Table 6 . Sample sizes of participating studies in the COVID-19 Host Genetic Initiative GWAS Release 4 in September 2020. Additional file 4: Supplementary Fig. 1 . Leave-one-out analysis results for body mass index and severe respiratory COVID-19. Additional file 5: Supplementary Fig. 2 . Leave-one-out analysis results for body mass index and COVID-19 hospitalization. Additional file 6: Supplementary Fig. 3 . Leave-one-out analysis results for lifetime smoking and severe respiratory COVID-19. Additional file 7: Supplementary Fig. 4 . Leave-one-out analysis results for lifetime smoking and COVID-19 hospitalization. Additional file 8: Supplementary Fig. 5 . Leave-one-out analysis results for physical activity and severe respiratory COVID-19. Additional file 9: Supplementary Fig. 6 . Leave-one-out analysis results for physical activity and COVID-19 hospitalization. Additional file 10: Supplementary Fig. 7 . Leave-one-out analysis results for alcohol consumption and severe respiratory COVID-19 using all genetic variants. Additional file 11: Supplementary Fig. 8 . Leave-one-out..
References
Bowden, Smith, Burgess, Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression, Int J Epidemiol
Bowden, Smith, Haycock, Burgess, Consistent estimation in mendelian randomization with some invalid instruments using a weighted median estimator, Genet Epidemiol
Burgess, Butterworth, Thompson, Mendelian randomization analysis with multiple genetic variants using summarized data, Genet Epidemiol
Burgess, Davies, Thompson, Bias due to participant overlap in two-sample Mendelian randomization, Genet Epidemiol
Burgess, Sample size and power calculations in Mendelian randomization with a single instrumental variable and a binary outcome, Int J Epidemiol
Docherty, Harrison, Green, Hardwick, Pius et al., clinical characterisation protocol
Doherty, Smith-Byrne, Ferreira, Holmes, Holmes et al., GWAS identifies 14 loci for device-measured physical activity and sleep duration, Nat Commun
Ellinghaus, Degenhardt, Bujanda, Buti, Albillos et al., Genomewide association study of severe covid-19 with respiratory failure, N Engl J Med
García, Immune response, inflammation, and the clinical spectrum of COVID-19, Front Immunol
Guan, Ni, Hu, Liang, Ou et al., Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med
Hartwig, Smith, Bowden, Robust inference in summary data Mendelian randomization via the zero modal pleiotropy assumption, Int J Epidemiol
Hemani, Zheng, Elsworth, Wade, Haberland et al., The MR-Base platform supports systematic causal inference across the human phenome, Elife
Leong, Cole, Brenner, Meigs, Florez et al., Cardiometabolic risk factors for COVID-19 susceptibility and severity: a mendelian randomization analysis, medRxiv
Liu, Jiang, Wedow, Li, Brazel et al., Association studies of up to 12 million individuals yield new insights into the genetic etiology of tobacco and alcohol use, Nat Genet
Pierce, Burgess, Efficient design for Mendelian randomization studies: subsample and 2-sample instrumental variable estimators, Am J Epidemiol
Ponsford, Gkatzionis, Walker, Grant, Wootton et al., Cardiometabolic traits, sepsis and severe COVID-19: a mendelian randomization investigation
Rocha, Libby, Obesity, inflammation, and atherosclerosis, Nat Rev Cardiol
Rossato, Russo, Mazzocut, Vincenzo, Fioretto et al., Current smoking is not associated with COVID-19, Eur Respir J
Simonnet, Chetboun, Poissy, Raverdy, Noulette et al., High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation, Obesity (Silver Spring)
Simons, Shahab, Brown, Perski, evidence review with Bayesian meta-analyses (version 7)
Smith, Ebrahim, Mendelian randomization': can genetic epidemiology contribute to understanding environmental determinants of disease?, Int J Epidemiol
Tilg, Moschen, Adipocytokines: mediators linking adipose tissue, inflammation and immunity, Nat Rev Immunol
Williamson, Walker, Bhaskaran, Bacon, Bates et al., Factors associated with COVID-19-related death using OpenSAFELY, Nature
Wootton, Richmond, Stuijfzand, Lawn, Sallis et al., Evidence for causal effects of lifetime smoking on risk for depression and schizophrenia: a Mendelian randomisation study, Psychol Med
Yengo, Sidorenko, Kemper, Zheng, Wood et al., Meta-analysis of genome-wide association studies for height and body mass index in ∼700000 individuals of European ancestry, Hum Mol Genet
Ying, Fu, Lee, Olefsky, The role of macrophages in obesityassociated islet inflammation and β-cell abnormalities, Nat Rev Endocrinol
Zhang, Li, Sun, He, Xu et al., Physical activity, BMI and COVID-19: an observational and Mendelian randomisation study, medRxiv
DOI record:
{
"DOI": "10.1186/s12920-021-00887-1",
"ISSN": [
"1755-8794"
],
"URL": "http://dx.doi.org/10.1186/s12920-021-00887-1",
"abstract": "<jats:title>Abstract</jats:title><jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>Lifestyle factors including obesity and smoking are suggested to be correlated with increased risk of COVID-19 severe illness or related death. However, whether these relationships are causal is not well known; neither for the relationships between COVID-19 severe illness and other common lifestyle factors, such as physical activity and alcohol consumption.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>Genome-wide significant genetic variants associated with body mass index (BMI), lifetime smoking, physical activity and alcohol consumption identified by large-scale genome-wide association studies (GWAS) of up to 941,280 individuals were selected as instrumental variables. Summary statistics of the genetic variants on severe illness of COVID-19 were obtained from GWAS analyses of up to 6492 cases and 1,012,809 controls. Two-sample Mendelian randomisation analyses were conducted.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>Both per-standard deviation (SD) increase in genetically predicted BMI and lifetime smoking were associated with about two-fold increased risks of severe respiratory COVID-19 and COVID-19 hospitalization (all P < 0.05). Per-SD increase in genetically predicted physical activity was associated with decreased risks of severe respiratory COVID-19 (odds ratio [OR] = 0.19; 95% confidence interval [CI], 0.05, 0.74; P = 0.02), but not with COVID-19 hospitalization (OR = 0.44; 95% CI 0.18, 1.07; P = 0.07). No evidence of association was found for genetically predicted alcohol consumption. Similar results were found across robust Mendelian randomisation methods.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Conclusions</jats:title>\n <jats:p>Evidence is found that BMI and smoking causally increase and physical activity might causally decrease the risk of COVID-19 severe illness. This study highlights the importance of maintaining a healthy lifestyle in protecting from COVID-19 severe illness and its public health value in fighting against COVID-19 pandemic.</jats:p>\n </jats:sec>",
"alternative-id": [
"887"
],
"article-number": "38",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "12 November 2020"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "27 January 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "3 February 2021"
},
{
"group": {
"label": "Ethics approval and consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1,
"value": "Not applicable, as this study used publicly available genome-wide association study summary statistics. No human participants were contacted or involved. No administrative permissions were required to access the summary statistics."
},
{
"group": {
"label": "Consent for publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "Not applicable."
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "The authors declare that they have no competing interests."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-8696-8594",
"affiliation": [],
"authenticated-orcid": false,
"family": "Li",
"given": "Shuai",
"sequence": "first"
},
{
"affiliation": [],
"family": "Hua",
"given": "Xinyang",
"sequence": "additional"
}
],
"container-title": "BMC Medical Genomics",
"container-title-short": "BMC Med Genomics",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2021,
2,
3
]
],
"date-time": "2021-02-03T12:06:26Z",
"timestamp": 1612353986000
},
"deposited": {
"date-parts": [
[
2021,
2,
3
]
],
"date-time": "2021-02-03T12:10:49Z",
"timestamp": 1612354249000
},
"funder": [
{
"DOI": "10.13039/100008018",
"award": [
"ECRF19020"
],
"doi-asserted-by": "publisher",
"name": "Victorian Cancer Agency"
}
],
"indexed": {
"date-parts": [
[
2022,
8,
23
]
],
"date-time": "2022-08-23T00:29:17Z",
"timestamp": 1661214557558
},
"is-referenced-by-count": 18,
"issue": "1",
"issued": {
"date-parts": [
[
2021,
2,
3
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2021,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
2,
3
]
],
"date-time": "2021-02-03T00:00:00Z",
"timestamp": 1612310400000
}
},
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
2,
3
]
],
"date-time": "2021-02-03T00:00:00Z",
"timestamp": 1612310400000
}
}
],
"link": [
{
"URL": "http://link.springer.com/content/pdf/10.1186/s12920-021-00887-1.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://link.springer.com/article/10.1186/s12920-021-00887-1/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://link.springer.com/content/pdf/10.1186/s12920-021-00887-1.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1186",
"published": {
"date-parts": [
[
2021,
2,
3
]
]
},
"published-online": {
"date-parts": [
[
2021,
2,
3
]
]
},
"published-print": {
"date-parts": [
[
2021,
12
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1101/2020.04.23.20076042",
"doi-asserted-by": "crossref",
"key": "887_CR1",
"unstructured": "Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, Holden KA, Read JM, Dondelinger F, Carson G, et al. Features of 16,749 hospitalised UK patients with COVID-19 using the ISARIC WHO clinical characterisation protocol. medRxiv 2020:2020.2004.2023.20076042."
},
{
"DOI": "10.1038/s41586-020-2521-4",
"author": "EJ Williamson",
"doi-asserted-by": "publisher",
"first-page": "430",
"issue": "7821",
"journal-title": "Nature",
"key": "887_CR2",
"unstructured": "Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, Curtis HJ, Mehrkar A, Evans D, Inglesby P, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–6.",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1002/oby.22831",
"author": "A Simonnet",
"doi-asserted-by": "publisher",
"first-page": "1195",
"issue": "7",
"journal-title": "Obesity (Silver Spring)",
"key": "887_CR3",
"unstructured": "Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, Duhamel A, Labreuche J, Mathieu D, Pattou F, Jourdain M. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity (Silver Spring). 2020;28(7):1195–9.",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2002032",
"author": "WJ Guan",
"doi-asserted-by": "publisher",
"first-page": "1708",
"issue": "18",
"journal-title": "N Engl J Med",
"key": "887_CR4",
"unstructured": "Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20.",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.32388/UJR2AW.8",
"doi-asserted-by": "crossref",
"key": "887_CR5",
"unstructured": "Simons D, Shahab L, Brown J, Perski O. The association of smoking status with SARS-CoV-2 infection, hospitalisation and mortality from COVID-19: a living rapid evidence review with Bayesian meta-analyses (version 7). Addiction. 2020."
},
{
"DOI": "10.1183/13993003.01290-2020",
"doi-asserted-by": "crossref",
"key": "887_CR6",
"unstructured": "Rossato M, Russo L, Mazzocut S, Di Vincenzo A, Fioretto P, Vettor R. Current smoking is not associated with COVID-19. Eur Respir J. 2020;55(6)."
},
{
"key": "887_CR7",
"unstructured": "Coronavirus Disease 2019 (COVID-19)—People with certain medical conditions. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html."
},
{
"DOI": "10.1101/2020.08.01.20166405",
"doi-asserted-by": "crossref",
"key": "887_CR8",
"unstructured": "Zhang X, Li X, Sun Z, He Y, Xu W, Campbell H, Dunlop MG, Timofeeva M, Theodoratou E. Physical activity, BMI and COVID-19: an observational and Mendelian randomisation study. medRxiv 2020:2020.2008.2001.20166405."
},
{
"DOI": "10.1093/ije/dyg070",
"author": "GD Smith",
"doi-asserted-by": "publisher",
"first-page": "1",
"issue": "1",
"journal-title": "Int J Epidemiol",
"key": "887_CR9",
"unstructured": "Smith GD, Ebrahim S. ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol. 2003;32(1):1–22.",
"volume": "32",
"year": "2003"
},
{
"DOI": "10.1101/2020.06.18.20134676",
"doi-asserted-by": "crossref",
"key": "887_CR10",
"unstructured": "Ponsford MJ, Gkatzionis A, Walker VM, Grant AJ, Wootton RE, Moore LSP, Fatumo S, Mason AM, Zuber V, Willer C, et al. Cardiometabolic traits, sepsis and severe COVID-19: a mendelian randomization investigation. Circulation. 2020."
},
{
"DOI": "10.1101/2020.08.26.20182709",
"doi-asserted-by": "crossref",
"key": "887_CR11",
"unstructured": "Leong A, Cole J, Brenner LN, Meigs JB, Florez JC, Mercader JM. Cardiometabolic risk factors for COVID-19 susceptibility and severity: a mendelian randomization analysis. medRxiv. 2020:2020.2008.2026.20182709."
},
{
"DOI": "10.1093/aje/kwt084",
"author": "BL Pierce",
"doi-asserted-by": "publisher",
"first-page": "1177",
"issue": "7",
"journal-title": "Am J Epidemiol",
"key": "887_CR12",
"unstructured": "Pierce BL, Burgess S. Efficient design for Mendelian randomization studies: subsample and 2-sample instrumental variable estimators. Am J Epidemiol. 2013;178(7):1177–84.",
"volume": "178",
"year": "2013"
},
{
"DOI": "10.1038/s41431-020-0636-6",
"doi-asserted-by": "crossref",
"key": "887_CR13",
"unstructured": "The COVID-19 Host Genetics Initiative, a global initiative to elucidate the role of host genetic factors in susceptibility and severity of the SARS-CoV-2 virus pandemic. Eur J Hum Genet. 2020;28(6):715–718."
},
{
"DOI": "10.1093/hmg/ddy271",
"author": "L Yengo",
"doi-asserted-by": "publisher",
"first-page": "3641",
"issue": "20",
"journal-title": "Hum Mol Genet",
"key": "887_CR14",
"unstructured": "Yengo L, Sidorenko J, Kemper KE, Zheng Z, Wood AR, Weedon MN, Frayling TM, Hirschhorn J, Yang J, Visscher PM. Meta-analysis of genome-wide association studies for height and body mass index in ∼700000 individuals of European ancestry. Hum Mol Genet. 2018;27(20):3641–9.",
"volume": "27",
"year": "2018"
},
{
"DOI": "10.1101/381301",
"doi-asserted-by": "crossref",
"key": "887_CR15",
"unstructured": "Wootton RE, Richmond RC, Stuijfzand BG, Lawn RB, Sallis HM, Taylor GMJ, Hemani G, Jones HJ, Zammit S, Davey Smith G, et al. Evidence for causal effects of lifetime smoking on risk for depression and schizophrenia: a Mendelian randomisation study. Psychol Med;2019:1–9."
},
{
"DOI": "10.1038/s41467-018-07743-4",
"author": "A Doherty",
"doi-asserted-by": "publisher",
"first-page": "5257",
"issue": "1",
"journal-title": "Nat Commun",
"key": "887_CR16",
"unstructured": "Doherty A, Smith-Byrne K, Ferreira T, Holmes MV, Holmes C, Pulit SL, Lindgren CM. GWAS identifies 14 loci for device-measured physical activity and sleep duration. Nat Commun. 2018;9(1):5257.",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1038/s41588-018-0307-5",
"author": "M Liu",
"doi-asserted-by": "publisher",
"first-page": "237",
"issue": "2",
"journal-title": "Nat Genet",
"key": "887_CR17",
"unstructured": "Liu M, Jiang Y, Wedow R, Li Y, Brazel DM, Chen F, Datta G, Davila-Velderrain J, McGuire D, Tian C, et al. Association studies of up to 12 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat Genet. 2019;51(2):237–44.",
"volume": "51",
"year": "2019"
},
{
"DOI": "10.1093/ije/dyu005",
"author": "S Burgess",
"doi-asserted-by": "publisher",
"first-page": "922",
"issue": "3",
"journal-title": "Int J Epidemiol",
"key": "887_CR18",
"unstructured": "Burgess S. Sample size and power calculations in Mendelian randomization with a single instrumental variable and a binary outcome. Int J Epidemiol. 2014;43(3):922–9.",
"volume": "43",
"year": "2014"
},
{
"DOI": "10.1002/gepi.21758",
"author": "S Burgess",
"doi-asserted-by": "publisher",
"first-page": "658",
"issue": "7",
"journal-title": "Genet Epidemiol",
"key": "887_CR19",
"unstructured": "Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol. 2013;37(7):658–65.",
"volume": "37",
"year": "2013"
},
{
"DOI": "10.1093/ije/dyv080",
"author": "J Bowden",
"doi-asserted-by": "publisher",
"first-page": "512",
"issue": "2",
"journal-title": "Int J Epidemiol",
"key": "887_CR20",
"unstructured": "Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44(2):512–25.",
"volume": "44",
"year": "2015"
},
{
"DOI": "10.1002/gepi.21965",
"author": "J Bowden",
"doi-asserted-by": "publisher",
"first-page": "304",
"issue": "4",
"journal-title": "Genet Epidemiol",
"key": "887_CR21",
"unstructured": "Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 2016;40(4):304–14.",
"volume": "40",
"year": "2016"
},
{
"DOI": "10.1093/ije/dyx102",
"author": "FP Hartwig",
"doi-asserted-by": "publisher",
"first-page": "1985",
"issue": "6",
"journal-title": "Int J Epidemiol",
"key": "887_CR22",
"unstructured": "Hartwig FP, Davey Smith G, Bowden J. Robust inference in summary data Mendelian randomization via the zero modal pleiotropy assumption. Int J Epidemiol. 2017;46(6):1985–98.",
"volume": "46",
"year": "2017"
},
{
"DOI": "10.7554/eLife.34408",
"doi-asserted-by": "crossref",
"key": "887_CR23",
"unstructured": "Hemani G, Zheng J, Elsworth B, Wade KH, Haberland V, Baird D, Laurin C, Burgess S, Bowden J, Langdon R, et al. The MR-Base platform supports systematic causal inference across the human phenome. Elife. 2018, 7."
},
{
"key": "887_CR24",
"unstructured": "Ellinghaus D, Degenhardt F, Bujanda L, Buti M, Albillos A, Invernizzi P, Fernández J, Prati D, Baselli G, Asselta R, et al. Genomewide association study of severe covid-19 with respiratory failure. N Engl J Med. 2020."
},
{
"DOI": "10.1038/nri1937",
"author": "H Tilg",
"doi-asserted-by": "publisher",
"first-page": "772",
"issue": "10",
"journal-title": "Nat Rev Immunol",
"key": "887_CR25",
"unstructured": "Tilg H, Moschen AR. Adipocytokines: mediators linking adipose tissue, inflammation and immunity. Nat Rev Immunol. 2006;6(10):772–83.",
"volume": "6",
"year": "2006"
},
{
"DOI": "10.1038/nrcardio.2009.55",
"author": "VZ Rocha",
"doi-asserted-by": "publisher",
"first-page": "399",
"issue": "6",
"journal-title": "Nat Rev Cardiol",
"key": "887_CR26",
"unstructured": "Rocha VZ, Libby P. Obesity, inflammation, and atherosclerosis. Nat Rev Cardiol. 2009;6(6):399–409.",
"volume": "6",
"year": "2009"
},
{
"DOI": "10.1038/s41574-019-0286-3",
"author": "W Ying",
"doi-asserted-by": "publisher",
"first-page": "81",
"issue": "2",
"journal-title": "Nat Rev Endocrinol",
"key": "887_CR27",
"unstructured": "Ying W, Fu W, Lee YS, Olefsky JM. The role of macrophages in obesity-associated islet inflammation and β-cell abnormalities. Nat Rev Endocrinol. 2020;16(2):81–90.",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2020.01441",
"author": "LF García",
"doi-asserted-by": "publisher",
"first-page": "1441",
"journal-title": "Front Immunol",
"key": "887_CR28",
"unstructured": "García LF. Immune response, inflammation, and the clinical spectrum of COVID-19. Front Immunol. 2020;11:1441.",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1002/gepi.21998",
"author": "S Burgess",
"doi-asserted-by": "publisher",
"first-page": "597",
"issue": "7",
"journal-title": "Genet Epidemiol",
"key": "887_CR29",
"unstructured": "Burgess S, Davies NM, Thompson SG. Bias due to participant overlap in two-sample Mendelian randomization. Genet Epidemiol. 2016;40(7):597–608.",
"volume": "40",
"year": "2016"
}
],
"reference-count": 29,
"references-count": 29,
"relation": {
"has-review": [
{
"asserted-by": "object",
"id": "10.3410/f.739501721.793583095",
"id-type": "doi"
}
]
},
"resource": {
"primary": {
"URL": "https://bmcmedgenomics.biomedcentral.com/articles/10.1186/s12920-021-00887-1"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Genetics (clinical)",
"Genetics"
],
"subtitle": [],
"title": "Modifiable lifestyle factors and severe COVID-19 risk: a Mendelian randomisation study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "14"
}
