COVID-19 outcomes in patients taking cardioprotective medications
et al., PLOS ONE, doi:10.1371/journal.pone.0275787, Oct 2022
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 13,585 COVID+ patients in the USA, showing lower mortality with metformin use, but no significant difference for ventilation, ICU admission, and hospitalization.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
Study covers aspirin and metformin.
|
risk of death, 41.1% lower, OR 0.59, p = 0.003, treatment 2,684, control 2,684, propensity score matching, RR approximated with OR.
|
|
risk of mechanical ventilation, 15.7% higher, OR 1.16, p = 0.49, treatment 2,684, control 2,684, propensity score matching, RR approximated with OR.
|
|
risk of ICU admission, 2.8% lower, OR 0.97, p = 0.85, treatment 2,684, control 2,684, propensity score matching, RR approximated with OR.
|
|
risk of hospitalization, 3.9% higher, OR 1.04, p = 0.72, treatment 2,684, control 2,684, propensity score matching, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Morrison et al., 10 Oct 2022, retrospective, USA, peer-reviewed, mean age 62.5, 3 authors, study period March 2020 - March 2021.
Contact: aturchin@bwh.harvard.edu, irb@partners.org.
COVID-19 outcomes in patients taking cardioprotective medications
PLOS ONE, doi:10.1371/journal.pone.0275787
Introduction The coronavirus disease 2019 (COVID-19) caused a worldwide pandemic and has led to over five million deaths. Many cardiovascular risk factors (e.g. obesity or diabetes) are associated with an increased risk of adverse outcomes in COVID-19. On the other hand, it has been suggested that medications used to treat cardiometabolic conditions may have protective effects for patients with COVID-19.
Objectives To determine whether patients taking four classes of cardioprotective medications-aspirin, metformin, renin angiotensin aldosterone system inhibitors (RAASi) and statins-have a lower risk of adverse outcomes of COVID-19.
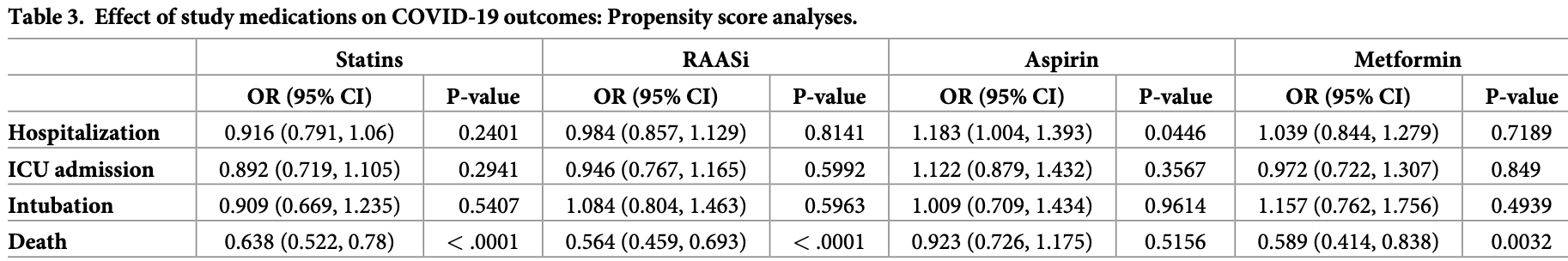
Methods We conducted a retrospective cohort study of primary care patients at a large integrated healthcare delivery system who had a positive COVID-19 test between March 2020 and March 2021. We compared outcomes of patients who were taking one of the study medications at the time of the COVID-19 test to patients who took a medication from the same class in the past (to minimize bias by indication). The following outcomes were compared: a) hospitalization; b) ICU admission; c) intubation; and d) death. Multivariable analysis was used to adjust for patient demographics and comorbidities.
Results Among 13,585 study patients, 1,970 (14.5%) were hospitalized; 763 (5.6%) were admitted to an ICU; 373 (2.8%) were intubated and 720 (5.3%) died. In bivariate analyses, patients taking metformin, RAASi and statins had lower risk of hospitalization, ICU admission and death. However, in multivariable analysis, only the lower risk of death remained statistically significant. Patients taking aspirin had a significantly higher risk of hospitalization in both bivariate and multivariable analyses.
Author Contributions Conceptualization: Alexander Turchin.
References
Alamdari, Afaghi, Rahimi, Tarki, Tavana et al., Mortality risk factors among hospitalized COVID-19 patients in a major referral center in Iran. The Tohoku journal of experimental medicine, doi:10.1620/tjem.252.73
Austin, An introduction to propensity score methods for reducing the effects of confounding in observational studies, Multivariate behavioral research, doi:10.1080/00273171.2011.568786
Bramante, Ingraham, Murray, Marmor, Hovertsen et al., Observational Study of Metformin and Risk of Mortality in Patients Hospitalized with Covid-19, medRxiv, doi:10.1101/2020.06.19.20135095
Cariou, Goronflot, Rimbert, Boullu, May et al., Routine use of statins and increased COVID-19 related mortality in inpatients with type 2 diabetes: Results from the CORONADO study, Diabetes & Metabolism, doi:10.1016/j.diabet.2020.10.001
Chen, Yang, Cheng, Chen, Peng et al., Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication, Diabetes Care, doi:10.2337/dc20-0660
Chow, Khanna, Kethireddy, Yamane, Levine et al., Aspirin Use Is Associated With Decreased Mechanical Ventilation, Intensive Care Unit Admission, and In-Hospital Mortality in Hospitalized Patients With Coronavirus Disease 2019, Anesth Analg, doi:10.1213/ANE.0000000000005292
Crouse, Grimes, Li, Might, Ovalle et al., Metformin Use Is Associated With Reduced Mortality in a Diverse Population With COVID-19 and Diabetes, Front Endocrinol, doi:10.3389/fendo.2020.600439
Delgado, Baweja, Crews, Eneanya, Gadegbeku et al., A Unifying Approach for GFR Estimation: Recommendations of the NKF-ASN Task Force on Reassessing the Inclusion of Race in Diagnosing Kidney Disease, Am J Kidney Dis, doi:10.1053/j.ajkd.2021.08.003
Do, Kim, Park, Cho, Kang, Is there an association between metformin use and clinical outcomes in diabetes patients with COVID-19? Diabetes & metabolism, doi:10.1016/j.diabet.2020.10.006
Driver, Bamitale, Kazi, Olla, Nyane et al., Cardioprotective Effects of Metformin, J Cardiovasc Pharmacol, doi:10.1097/FJC.0000000000000599
Felice, Nardin, Tanna, Grossi, Bernardi et al., Use of RAAS Inhibitors and Risk of Clinical Deterioration in COVID-19: Results From an Italian Cohort of 133 Hypertensives, Am J Hypertens, doi:10.1093/ajh/hpaa096
Frohlich, Jeschke, Eichler, Thiele, Alhariri et al., Impact of oral anticoagulation on clinical outcomes of COVID-19: a nationwide cohort study of hospitalized patients in Germany, Clin Res Cardiol, doi:10.1007/s00392-020-01783-x
Gu, Xie, Li, Zhang, Lai et al., Angiotensin-converting enzyme 2 inhibits lung injury induced by respiratory syncytial virus, Sci Rep, doi:10.1038/srep19840
Gupta, Madhavan, Poterucha, Defilippis, Hennessey et al., Association between antecedent statin use and decreased mortality in hospitalized patients with COVID-19, Nat Commun, doi:10.1038/s41467-021-21553-1
Gurbel, Bliden, Schror, Can an Old Ally Defeat a New Enemy?, Circulation, doi:10.1161/CIRCULATIONAHA.120.047830
Hergens, Bell, Haglund, Sundstrom, Lampa et al., Risk factors for COVID-19-related death, hospitalization and intensive care: a population-wide study of all inhabitants in Stockholm, Eur J Epidemiol, doi:10.1007/s10654-021-00840-7
Holman, Knighton, Kar, 'keefe, Curley et al., Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587%2820%2930271-0
Inciardi, Solomon, Ridker, Metra, Coronavirus 2019 Disease (COVID-19), Systemic Inflammation, and Cardiovascular Disease, J Am Heart Assoc, doi:10.1161/JAHA.120.017756
Keene, The log transformation is special, Stat Med, doi:10.1002/sim.4780140810
Khunti, Knighton, Zaccardi, Bakhai, Barron et al., Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England, doi:10.1016/S2213-8587%2821%2900050-4
Kuba, Imai, Rao, Gao, Guo et al., A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury, Nat Med, doi:10.1038/nm1267
Kuno, So, Iwagami, Takahashi, Egorova, The association of statins use with survival of patients with COVID-19, Journal of cardiology, doi:10.1016/j.jjcc.2021.12.012
Li, Ashcroft, Chung, Dighero, Dozier et al., Risk factors for poor outcomes in hospitalised COVID-19 patients: A systematic review and meta-analysis, doi:10.7189/jogh.11.10001
Mitacchione, Schiavone, Curnis, Arca, Antinori et al., Impact of prior statin use on clinical outcomes in COVID-19 patients: data from tertiary referral hospitals during COVID-19 pandemic in Italy, Journal of clinical lipidology, doi:10.1016/j.jacl.2020.12.008
Moccia, Gerbino, Lionetti, Miragoli, Munaron et al., COVID-19-associated cardiovascular morbidity in older adults: a position paper from the Italian Society of Cardiovascular Researches, Geroscience, doi:10.1007/s11357-020-00198-w
Nguyen, Ho, Nguyen, Ho, Li et al., Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: A meta-analysis, Metabolism, doi:10.1016/j.metabol.2022.155196
Reynolds, Adhikari, Pulgarin, Troxel, Iturrate et al., Renin-Angiotensin-Aldosterone System Inhibitors and Risk of Covid-19, N Engl J Med, doi:10.1056/NEJMoa2008975
Saeed, Castagna, Agalliu, Xue, Patel et al., Statin Use and In-Hospital Mortality in Patients With Diabetes Mellitus and COVID-19, Journal of the American Heart Association, doi:10.1161/JAHA.120.018475
Seiglie, Platt, Cromer, Bunda, Foulkes et al., Diabetes as a Risk Factor for Poor Early Outcomes in Patients Hospitalized With COVID-19, Diabetes Care, doi:10.2337/dc20-1506
Spiegeleer, Bronselaer, Teo, Byttebier, Tre et al., The effects of ARBs, ACEis, and statins on clinical outcomes of COVID-19 infection among nursing home residents, Journal of the American Medical Directors Association, doi:10.1016/j.jamda.2020.06.018
Vaduganathan, Vardeny, Michel, Mcmurray, Pfeffer et al., Renin-Angiotensin-Aldosterone System Inhibitors in Patients with Covid-19, N Engl J Med, doi:10.1056/NEJMsr2005760
Valero, Civit, Dupont, Selnihhin, Reinert et al., A serum-stable RNA aptamer specific for SARS-CoV-2 neutralizes viral entry, Proc Natl Acad Sci U S A, doi:10.1073/pnas.2112942118
Villa, Brunialti, Dellavedova, Meda, Rebecchi et al., DNA aptamers masking angiotensin converting enzyme 2 as an innovative way to treat SARS-CoV-2 pandemic, Pharmacol Res, doi:10.1016/j.phrs.2021.105982
Wang, Van Oekelen, Mouhieddine, Valle, Richter et al., A tertiary center experience of multiple myeloma patients with COVID-19: lessons learned and the path forward, J Hematol Oncol, doi:10.1186/s13045-020-00934-x
Yin, Wang, Song, Li, Miao, Effects of Renin-Angiotensin System Inhibitors on Mortality and Disease Severity of COVID-19 Patients: A Meta-analysis of Randomized Controlled Trials, Am J Hypertens, doi:10.1093/ajh/hpac001
Zhang, Qin, Cheng, Shen, Zhao et al., In-hospital use of statins is associated with a reduced risk of mortality among individuals with COVID-19, Cell metabolism, doi:10.1016/j.cmet.2020.06.015
Zhang, Zhu, Cai, Lei, Qin et al., Association of inpatient use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19, Circulation research, doi:10.1161/CIRCRESAHA.120.317134
Zibaeenezhad, Lu, Zahra, Mahboobeh, Lionetti, Angiotensin-converting enzyme 2: a double-edged sword in COVID-19 patients with an increased risk of heart failure, Heart Fail Rev, doi:10.1007/s10741-020-10016-2
Zou, Yan, Shu, Gao, Sun et al., Angiotensin-converting enzyme 2 protects from lethal avian influenza A H5N1 infections, Nat Commun, doi:10.1038/ncomms4594
DOI record:
{
"DOI": "10.1371/journal.pone.0275787",
"ISSN": [
"1932-6203"
],
"URL": "http://dx.doi.org/10.1371/journal.pone.0275787",
"abstract": "<jats:sec id=\"sec001\">\n<jats:title>Introduction</jats:title>\n<jats:p>The coronavirus disease 2019 (COVID-19) caused a worldwide pandemic and has led to over five million deaths. Many cardiovascular risk factors (e.g. obesity or diabetes) are associated with an increased risk of adverse outcomes in COVID-19. On the other hand, it has been suggested that medications used to treat cardiometabolic conditions may have protective effects for patients with COVID-19.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec002\">\n<jats:title>Objectives</jats:title>\n<jats:p>To determine whether patients taking four classes of cardioprotective medications—aspirin, metformin, renin angiotensin aldosterone system inhibitors (RAASi) and statins–have a lower risk of adverse outcomes of COVID-19.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec003\">\n<jats:title>Methods</jats:title>\n<jats:p>We conducted a retrospective cohort study of primary care patients at a large integrated healthcare delivery system who had a positive COVID-19 test between March 2020 and March 2021. We compared outcomes of patients who were taking one of the study medications at the time of the COVID-19 test to patients who took a medication from the same class in the past (to minimize bias by indication). The following outcomes were compared: a) hospitalization; b) ICU admission; c) intubation; and d) death. Multivariable analysis was used to adjust for patient demographics and comorbidities.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec004\">\n<jats:title>Results</jats:title>\n<jats:p>Among 13,585 study patients, 1,970 (14.5%) were hospitalized; 763 (5.6%) were admitted to an ICU; 373 (2.8%) were intubated and 720 (5.3%) died. In bivariate analyses, patients taking metformin, RAASi and statins had lower risk of hospitalization, ICU admission and death. However, in multivariable analysis, only the lower risk of death remained statistically significant. Patients taking aspirin had a significantly higher risk of hospitalization in both bivariate and multivariable analyses.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec005\">\n<jats:title>Conclusions</jats:title>\n<jats:p>Cardioprotective medications were not associated with a consistent benefit in COVID-19. As vaccination and effective treatments are not yet universally accessible worldwide, research should continue to determine whether affordable and widely available medications could be utilized to decrease the risks of this disease.</jats:p>\n</jats:sec>",
"author": [
{
"affiliation": [],
"family": "Morrison",
"given": "Fritha J.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Su",
"given": "Maxwell",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8609-564X",
"affiliation": [],
"authenticated-orcid": true,
"family": "Turchin",
"given": "Alexander",
"sequence": "additional"
}
],
"container-title": "PLOS ONE",
"container-title-short": "PLoS ONE",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.plosone.org"
]
},
"created": {
"date-parts": [
[
2022,
10,
10
]
],
"date-time": "2022-10-10T17:34:01Z",
"timestamp": 1665423241000
},
"deposited": {
"date-parts": [
[
2022,
10,
10
]
],
"date-time": "2022-10-10T17:34:53Z",
"timestamp": 1665423293000
},
"editor": [
{
"affiliation": [],
"family": "Mogi",
"given": "Masaki",
"sequence": "first"
}
],
"funder": [
{
"DOI": "10.13039/100006093",
"award": [
"ME-2019C1-15328"
],
"doi-asserted-by": "publisher",
"name": "Patient-Centered Outcomes Research Institute"
}
],
"indexed": {
"date-parts": [
[
2022,
10,
10
]
],
"date-time": "2022-10-10T18:17:33Z",
"timestamp": 1665425853406
},
"is-referenced-by-count": 0,
"issue": "10",
"issued": {
"date-parts": [
[
2022,
10,
10
]
]
},
"journal-issue": {
"issue": "10",
"published-online": {
"date-parts": [
[
2022,
10,
10
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
10,
10
]
],
"date-time": "2022-10-10T00:00:00Z",
"timestamp": 1665360000000
}
}
],
"link": [
{
"URL": "https://dx.plos.org/10.1371/journal.pone.0275787",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "340",
"original-title": [],
"page": "e0275787",
"prefix": "10.1371",
"published": {
"date-parts": [
[
2022,
10,
10
]
]
},
"published-online": {
"date-parts": [
[
2022,
10,
10
]
]
},
"publisher": "Public Library of Science (PLoS)",
"reference": [
{
"key": "pone.0275787.ref001",
"unstructured": "Medicine JHUo. Coronavirus Resource Center 2022 [cited 2022 2/16/2022]. https://coronavirus.jhu.edu/."
},
{
"DOI": "10.1161/JAHA.120.017756",
"article-title": "Coronavirus 2019 Disease (COVID-19), Systemic Inflammation, and Cardiovascular Disease",
"author": "RM Inciardi",
"doi-asserted-by": "crossref",
"first-page": "e017756",
"issue": "16",
"journal-title": "J Am Heart Assoc",
"key": "pone.0275787.ref002",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.7189/jogh.11.10001",
"article-title": "Risk factors for poor outcomes in hospitalised COVID-19 patients: A systematic review and meta-analysis",
"author": "Y Li",
"doi-asserted-by": "crossref",
"first-page": "10001",
"journal-title": "J Glob Health",
"key": "pone.0275787.ref003",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.3389/fendo.2020.600439",
"article-title": "Metformin Use Is Associated With Reduced Mortality in a Diverse Population With COVID-19 and Diabetes",
"author": "AB Crouse",
"doi-asserted-by": "crossref",
"first-page": "600439",
"journal-title": "Front Endocrinol (Lausanne)",
"key": "pone.0275787.ref004",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.2337/dc20-1506",
"article-title": "Diabetes as a Risk Factor for Poor Early Outcomes in Patients Hospitalized With COVID-19",
"author": "J Seiglie",
"doi-asserted-by": "crossref",
"first-page": "2938",
"issue": "12",
"journal-title": "Diabetes Care",
"key": "pone.0275787.ref005",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1007/s10654-021-00840-7",
"article-title": "Risk factors for COVID-19-related death, hospitalization and intensive care: a population-wide study of all inhabitants in Stockholm",
"author": "MP Hergens",
"doi-asserted-by": "crossref",
"first-page": "157",
"issue": "2",
"journal-title": "Eur J Epidemiol",
"key": "pone.0275787.ref006",
"volume": "37",
"year": "2022"
},
{
"DOI": "10.1007/s11357-020-00198-w",
"article-title": "COVID-19-associated cardiovascular morbidity in older adults: a position paper from the Italian Society of Cardiovascular Researches",
"author": "F Moccia",
"doi-asserted-by": "crossref",
"first-page": "1021",
"issue": "4",
"journal-title": "Geroscience",
"key": "pone.0275787.ref007",
"volume": "42",
"year": "2020"
},
{
"DOI": "10.1038/s41467-021-21553-1",
"article-title": "Association between antecedent statin use and decreased mortality in hospitalized patients with COVID-19",
"author": "A Gupta",
"doi-asserted-by": "crossref",
"first-page": "1325",
"issue": "1",
"journal-title": "Nat Commun",
"key": "pone.0275787.ref008",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1038/nm1267",
"article-title": "A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury",
"author": "K Kuba",
"doi-asserted-by": "crossref",
"first-page": "875",
"issue": "8",
"journal-title": "Nat Med",
"key": "pone.0275787.ref009",
"volume": "11",
"year": "2005"
},
{
"DOI": "10.1038/ncomms4594",
"article-title": "Angiotensin-converting enzyme 2 protects from lethal avian influenza A H5N1 infections",
"author": "Z Zou",
"doi-asserted-by": "crossref",
"first-page": "3594",
"journal-title": "Nat Commun",
"key": "pone.0275787.ref010",
"volume": "5",
"year": "2014"
},
{
"DOI": "10.1038/srep19840",
"article-title": "Angiotensin-converting enzyme 2 inhibits lung injury induced by respiratory syncytial virus",
"author": "H Gu",
"doi-asserted-by": "crossref",
"first-page": "19840",
"journal-title": "Sci Rep",
"key": "pone.0275787.ref011",
"volume": "6",
"year": "2016"
},
{
"DOI": "10.1007/s10741-020-10016-2",
"article-title": "Angiotensin-converting enzyme 2: a double-edged sword in COVID-19 patients with an increased risk of heart failure",
"author": "I Razeghian-Jahromi",
"doi-asserted-by": "crossref",
"first-page": "371",
"issue": "2",
"journal-title": "Heart Fail Rev",
"key": "pone.0275787.ref012",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1097/FJC.0000000000000599",
"article-title": "Cardioprotective Effects of Metformin",
"author": "C Driver",
"doi-asserted-by": "crossref",
"first-page": "121",
"issue": "2",
"journal-title": "J Cardiovasc Pharmacol",
"key": "pone.0275787.ref013",
"volume": "72",
"year": "2018"
},
{
"article-title": "Observational Study of Metformin and Risk of Mortality in Patients Hospitalized with Covid-19",
"author": "CT Bramante",
"journal-title": "medRxiv",
"key": "pone.0275787.ref014",
"year": "2020"
},
{
"author": "PA Gurbel",
"first-page": "315",
"issue": "4",
"journal-title": "Can an Old Ally Defeat a New Enemy? Circulation",
"key": "pone.0275787.ref015",
"volume": "142",
"year": "2020"
},
{
"article-title": "A Unifying Approach for GFR Estimation: Recommendations of the NKF-ASN Task Force on Reassessing the Inclusion of Race in Diagnosing Kidney Disease",
"author": "C Delgado",
"journal-title": "Am J Kidney Dis",
"key": "pone.0275787.ref016",
"year": "2021"
},
{
"DOI": "10.1002/sim.4780140810",
"article-title": "The log transformation is special",
"author": "ON Keene",
"doi-asserted-by": "crossref",
"first-page": "811",
"issue": "8",
"journal-title": "Stat Med",
"key": "pone.0275787.ref017",
"volume": "14",
"year": "1995"
},
{
"DOI": "10.1080/00273171.2011.568786",
"article-title": "An introduction to propensity score methods for reducing the effects of confounding in observational studies",
"author": "PC Austin",
"doi-asserted-by": "crossref",
"first-page": "399",
"issue": "3",
"journal-title": "Multivariate behavioral research",
"key": "pone.0275787.ref018",
"volume": "46",
"year": "2011"
},
{
"DOI": "10.1186/s13045-020-00934-x",
"article-title": "A tertiary center experience of multiple myeloma patients with COVID-19: lessons learned and the path forward",
"author": "B Wang",
"doi-asserted-by": "crossref",
"first-page": "94",
"issue": "1",
"journal-title": "J Hematol Oncol",
"key": "pone.0275787.ref019",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.2337/dc20-0660",
"article-title": "Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication",
"author": "Y Chen",
"doi-asserted-by": "crossref",
"first-page": "1399",
"issue": "7",
"journal-title": "Diabetes Care",
"key": "pone.0275787.ref020",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(21)00050-4",
"article-title": "Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England",
"author": "K Khunti",
"doi-asserted-by": "crossref",
"first-page": "293",
"issue": "5",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "pone.0275787.ref021",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1161/CIRCRESAHA.120.317134",
"article-title": "Association of inpatient use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19",
"author": "P Zhang",
"doi-asserted-by": "crossref",
"first-page": "1671",
"issue": "12",
"journal-title": "Circulation research",
"key": "pone.0275787.ref022",
"volume": "126",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.06.015",
"article-title": "In-hospital use of statins is associated with a reduced risk of mortality among individuals with COVID-19",
"author": "X-J Zhang",
"doi-asserted-by": "crossref",
"first-page": "176",
"issue": "2",
"journal-title": "Cell metabolism",
"key": "pone.0275787.ref023",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1620/tjem.252.73",
"article-title": "Mortality risk factors among hospitalized COVID-19 patients in a major referral center in Iran",
"author": "NM Alamdari",
"doi-asserted-by": "crossref",
"first-page": "73",
"issue": "1",
"journal-title": "The Tohoku journal of experimental medicine",
"key": "pone.0275787.ref024",
"volume": "252",
"year": "2020"
},
{
"DOI": "10.1016/j.jamda.2020.06.018",
"article-title": "The effects of ARBs, ACEis, and statins on clinical outcomes of COVID-19 infection among nursing home residents",
"author": "A De Spiegeleer",
"doi-asserted-by": "crossref",
"first-page": "909",
"issue": "7",
"journal-title": "Journal of the American Medical Directors Association",
"key": "pone.0275787.ref025",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"article-title": "Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study",
"author": "N Holman",
"doi-asserted-by": "crossref",
"first-page": "823",
"issue": "10",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "pone.0275787.ref026",
"volume": "8",
"year": "2020"
},
{
"article-title": "The association of statins use with survival of patients with COVID-19",
"author": "T Kuno",
"journal-title": "Journal of cardiology",
"key": "pone.0275787.ref027",
"year": "2021"
},
{
"DOI": "10.1161/JAHA.120.018475",
"article-title": "Statin Use and In‐Hospital Mortality in Patients With Diabetes Mellitus and COVID‐19",
"author": "O Saeed",
"doi-asserted-by": "crossref",
"first-page": "e018475",
"issue": "24",
"journal-title": "Journal of the American Heart Association",
"key": "pone.0275787.ref028",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1016/j.diabet.2020.10.001",
"article-title": "Routine use of statins and increased COVID-19 related mortality in inpatients with type 2 diabetes: Results from the CORONADO study",
"author": "B Cariou",
"doi-asserted-by": "crossref",
"first-page": "101202",
"issue": "2",
"journal-title": "Diabetes & Metabolism",
"key": "pone.0275787.ref029",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.1016/j.jacl.2020.12.008",
"article-title": "Impact of prior statin use on clinical outcomes in COVID-19 patients: data from tertiary referral hospitals during COVID-19 pandemic in Italy",
"author": "G Mitacchione",
"doi-asserted-by": "crossref",
"first-page": "68",
"issue": "1",
"journal-title": "Journal of clinical lipidology",
"key": "pone.0275787.ref030",
"volume": "15",
"year": "2021"
},
{
"article-title": "Use of RAAS Inhibitors and Risk of Clinical Deterioration in COVID-19: Results From an Italian Cohort of 133 Hypertensives",
"author": "C Felice",
"first-page": "944",
"issue": "10",
"journal-title": "Am J Hypertens",
"key": "pone.0275787.ref031",
"volume": "33",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2008975",
"article-title": "Renin-Angiotensin-Aldosterone System Inhibitors and Risk of Covid-19",
"author": "HR Reynolds",
"doi-asserted-by": "crossref",
"first-page": "2441",
"issue": "25",
"journal-title": "N Engl J Med",
"key": "pone.0275787.ref032",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1093/ajh/hpac001",
"article-title": "Effects of Renin-Angiotensin System Inhibitors on Mortality and Disease Severity of COVID-19 Patients: A Meta-analysis of Randomized Controlled Trials",
"author": "J Yin",
"doi-asserted-by": "crossref",
"first-page": "462",
"issue": "5",
"journal-title": "Am J Hypertens",
"key": "pone.0275787.ref033",
"volume": "35",
"year": "2022"
},
{
"DOI": "10.1213/ANE.0000000000005292",
"article-title": "Aspirin Use Is Associated With Decreased Mechanical Ventilation, Intensive Care Unit Admission, and In-Hospital Mortality in Hospitalized Patients With Coronavirus Disease 2019",
"author": "JH Chow",
"doi-asserted-by": "crossref",
"first-page": "930",
"issue": "4",
"journal-title": "Anesth Analg",
"key": "pone.0275787.ref034",
"volume": "132",
"year": "2021"
},
{
"DOI": "10.1016/j.metabol.2022.155196",
"article-title": "Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: A meta-analysis",
"author": "NN Nguyen",
"doi-asserted-by": "crossref",
"first-page": "155196",
"journal-title": "Metabolism",
"key": "pone.0275787.ref035",
"volume": "131",
"year": "2022"
},
{
"DOI": "10.1016/j.diabet.2020.10.006",
"article-title": "Is there an association between metformin use and clinical outcomes in diabetes patients with COVID-19?",
"author": "JY Do",
"doi-asserted-by": "crossref",
"first-page": "101208",
"issue": "4",
"journal-title": "Diabetes & metabolism",
"key": "pone.0275787.ref036",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.1056/NEJMsr2005760",
"article-title": "Renin-Angiotensin-Aldosterone System Inhibitors in Patients with Covid-19",
"author": "M Vaduganathan",
"doi-asserted-by": "crossref",
"first-page": "1653",
"issue": "17",
"journal-title": "N Engl J Med",
"key": "pone.0275787.ref037",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/j.phrs.2021.105982",
"article-title": "DNA aptamers masking angiotensin converting enzyme 2 as an innovative way to treat SARS-CoV-2 pandemic",
"author": "A Villa",
"doi-asserted-by": "crossref",
"first-page": "105982",
"journal-title": "Pharmacol Res",
"key": "pone.0275787.ref038",
"volume": "175",
"year": "2022"
},
{
"DOI": "10.1073/pnas.2112942118",
"article-title": "A serum-stable RNA aptamer specific for SARS-CoV-2 neutralizes viral entry",
"author": "J Valero",
"doi-asserted-by": "crossref",
"issue": "50",
"journal-title": "Proc Natl Acad Sci U S A",
"key": "pone.0275787.ref039",
"volume": "118",
"year": "2021"
},
{
"DOI": "10.1007/s00392-020-01783-x",
"article-title": "Impact of oral anticoagulation on clinical outcomes of COVID-19: a nationwide cohort study of hospitalized patients in Germany",
"author": "GM Frohlich",
"doi-asserted-by": "crossref",
"first-page": "1041",
"issue": "7",
"journal-title": "Clin Res Cardiol",
"key": "pone.0275787.ref040",
"volume": "110",
"year": "2021"
}
],
"reference-count": 40,
"references-count": 40,
"relation": {},
"resource": {
"primary": {
"URL": "https://dx.plos.org/10.1371/journal.pone.0275787"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "COVID-19 outcomes in patients taking cardioprotective medications",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1371/journal.pone.corrections_policy",
"volume": "17"
}
