Lifestyle and Comorbidity-Related Risk Factors of Severe and Critical COVID-19 Infection: A Comparative Study Among Survived COVID-19 Patients in Bangladesh
et al., Infection and Drug Resistance, doi:10.2147/IDR.S331470, Sep 2021
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 1,500 COVID+ patients in Bangladesh, showing lower risk of severe cases with regular exercise in unadjusted results.
This study is excluded in the after exclusion results of meta-analysis:
unadjusted results with no group details.
Study covers sleep and exercise.
|
risk of severe case, 19.0% lower, RR 0.81, p = 0.04, high activity levels 86 of 258 (33.3%), low activity levels 224 of 544 (41.2%), NNT 13, exercise >30 minutes.
|
|
risk of severe case, 0.9% higher, RR 1.01, p = 0.91, high activity levels 290 of 698 (41.5%), low activity levels 224 of 544 (41.2%), exercise <30 minutes.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Mohsin et al., 30 Sep 2021, retrospective, Bangladesh, peer-reviewed, survey, 10 authors, study period November 2020 - April 2021.
Lifestyle and Comorbidity-Related Risk Factors of Severe and Critical COVID-19 Infection: A Comparative Study Among Survived COVID-19 Patients in Bangladesh
Infection and Drug Resistance, doi:10.2147/idr.s331470
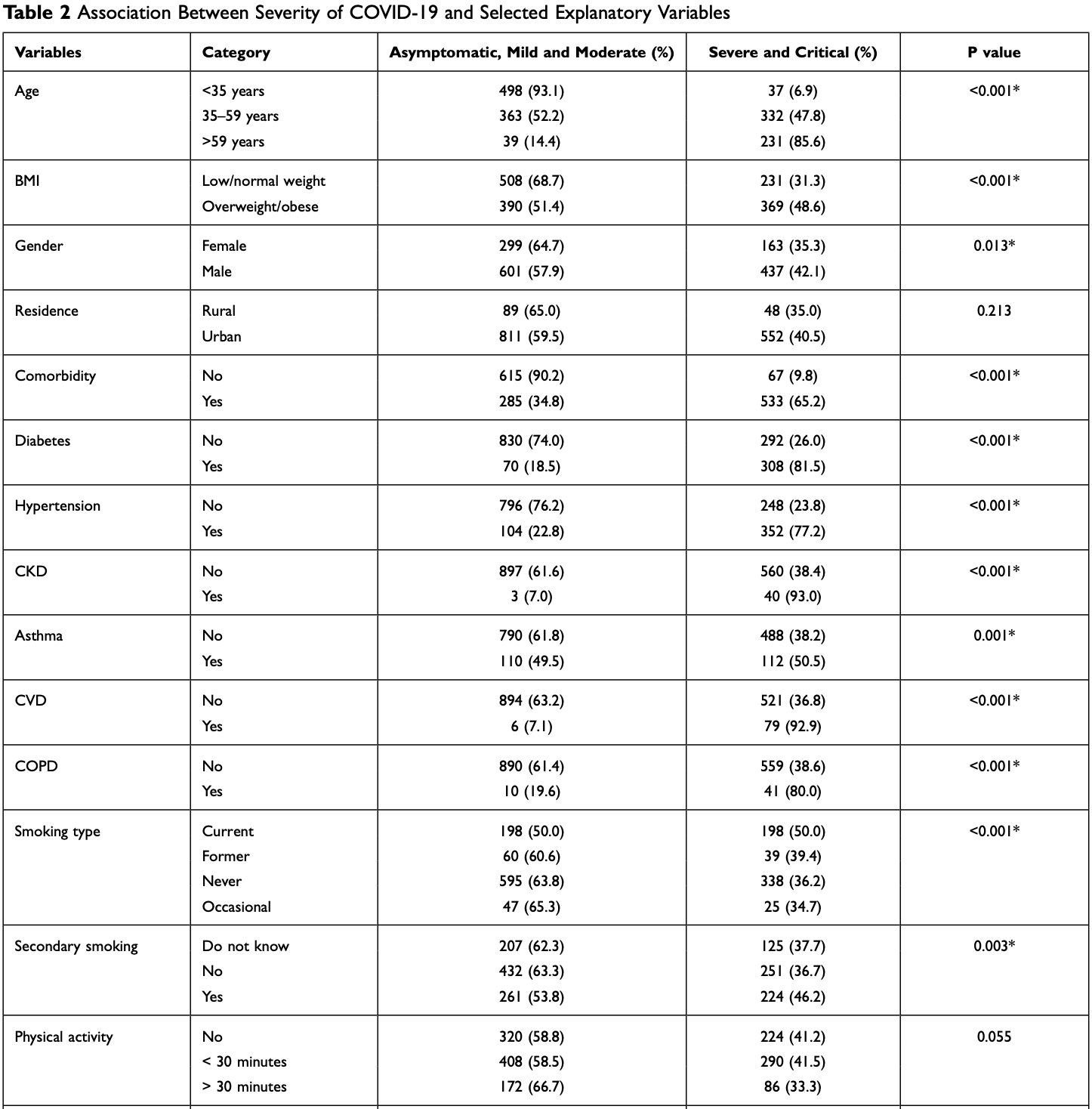
Background: Severe COVID-19 infections have already taken more than 4 million lives worldwide. Factors, such as socio-demographics, comorbidities, lifestyles, environment, and so on, have been widely discussed to be associated with increased severity in many countries. The study aimed to determine the risk factors of severe-critical COVID-19 in Bangladesh. Methods: This was a comparative cross-sectional study among various types of COVID-19 patients (both hospitalized and non-hospitalized) confirmed by reverse transcription polymerase chain reaction (RT-PCR). We have selected 1500 COVID-19 positive patients using a convenient sampling technique and analyzed lifestyle and comorbidity-related data using IBM SPSS-23 statistical package software. Chi-square test and multinomial logistic regression were used to determine risk factors of life-threatening COVID-19 infection.
Results: The mean age of the study participants was 43.23 (±15.48) years. The study identified several lifestyle-related factors and common commodities as risk factors for severe-critical COVID-19. The patient's age was one of the most important predictors, as people >59 years were at higher risk (AOR=18.223). Among other lifestyle factors, active smoking (AOR=1.482), exposure to secondary smoking (AOR=1.728), sleep disturbance (AOR=2.208) and attachment with SLT/alcohol/substance abuse (AOR=1.804) were identified as significant predictors for severe-critical COVID-19. Patients those were overweight/ obese (AOR=2.105), diabetic (AOR=4.286), hypertensive (AOR=3.363), CKD patients (AOR=8.317), asthma patients (AOR=2.152), CVD patients (AOR=7.747) were also at higher risk of severe-critical COVID-19 infection.
Conclusion: This study has identified several vital lifestyles and comorbidity-related risk factors of severe-critical COVID-19. People who have these comorbidities should be under high protection, and risky lifestyles of the general population should modify through the proper educational campaign.
Disclosure The authors report no conflicts of interest in this work.
Infection and Drug Resistance
Dovepress
References
Berlin, Thomas, Faou, Cornuz, COVID 19 and smoking, Nicotine Tob Res, doi:10.1093/ntr/ntaa059
Boehmer, Devies, Caruso, Changing age distribution of the COVID 19 pandemic, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm6939e1
Burrell, Howard, Murphy, Epidemiology of viral infections, Fenner Whites Med Virol, doi:10.1016/B978-0-12-375156-0.00013-8
Cascella, Rajnik, Cuomo, Dulebohn, Napoli, Features, evaluation and treatment Coronavirus (COVID 19)
Cen, Chen, Shen, Risk factors for disease progression in patients with mild to moderate coronavirus disease 2019-a multicentre observational study, Clin Microbiol Infect, doi:10.1016/j.cmi.2020.05.041
Cortis, On determining the age distribution of COVID 19 pandemic, Front Public Health
Demeulemeester, De Punder, Van Heijningen, Van Doesburg, Obesity as a risk factor for severe COVID 19 and complications: a review, Cells, doi:10.3390/cells10040933
Fischer, Minnwegen, Kaneider, Kraemer, Khan, Prevalence and determinants of secondhand smoke exposure among women in Bangladesh, 2011, Nicotine Tob Res, doi:10.1093/ntr/ntu129
Gao, Zheng, Wang, Obesity is a risk factor for greater COVID 19 severity, Diabetes Care, doi:10.2337/dc20-0682
Ghebreyesus, WHO director-general's opening remarks at the media briefing on COVID 19-11
Hamer, Kivimäki, Gale, Batty, Lifestyle risk factors, inflammatory mechanisms, and COVID 19 hospitalization: a community-based cohort study of 387,109 adults in UK, Brain Behav Immun, doi:10.1016/j.bbi.2020.05.059
Harlem, Descriptive analysis of social determinant factors in urban communities affected by COVID 19, J Public Health
Ho, Petermann-Rocha, Gray, Is older age associated with COVID 19 mortality in the absence of other risk factors? General population cohort study of 470,034 participants, PLoS One, doi:10.1371/journal.pone.0241824
Igić, Smoking and COVID 19, Vojnosanit Pregl, doi:10.2298/VSP2005461I
Kim, Hegde, Lafiura, COVID-19 illness in relation to sleep and burnout, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2021-000228
Li, Schoufour, Wang, Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: prospective cohort study, BMJ
Mohsin, Tonmon, Nahrin, Association between smoking and COVID 19 severity: evidence from Bangladesh, J Multidiscip Healthc, doi:10.2147/JMDH.S317603
Nargis, Thompson, Fong, Prevalence and patterns of tobacco use in Bangladesh from 2009 to 2012: evidence from International Tobacco Control (ITC) study, PLoS One, doi:10.1371/journal.pone.0141135
Newman, Enright, Manolio, Haponik, Wahl, Sleep disturbance, psychosocial correlates, and cardiovascular disease in 5201 older adults: the Cardiovascular Health Study, J Am Geriatr Soc, doi:10.1111/j.1532-5415.1997.tb00970.x
Nishiga, Wang, Han, Lewis, Wu, COVID 19 and cardiovascular disease: from basic mechanisms to clinical perspectives, Nat Rev Cardiol, doi:10.1038/s41569-020-0413-9
Nyberg, Singh-Manoux, Pentti, Association of healthy lifestyle with years lived without major chronic diseases, JAMA Intern Med, doi:10.1001/jamainternmed.2020.0618
Ortiz, Cozzolino, Duivenvoorden, Chronic kidney disease is a key risk factor for severe COVID 19: a call to action by the ERA-EDTA, Nephrol Dial Transplant, doi:10.1093/ndt/gfaa314
Pötschke-Langer, Schotte, Szilagyi, The WHO framework convention on tobacco control, Prog Respir Res
Sanyaolu, Okorie, Marinkovic, Comorbidity and its impact on patients with COVID 19, SN Compr Clin Med, doi:10.1007/s42399-020-00363-4
Schlesinger, Neuenschwander, Ballon, Nöthlings, Barbaresko, Adherence to healthy lifestyles and incidence of diabetes and mortality among individuals with diabetes: a systematic review and meta-analysis of prospective studies, J Epidemiol Community Health, doi:10.1136/jech-2019-213415
Simonnet, Chetboun, Poissy, High prevalence of obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation, Obesity, doi:10.1002/oby.22831
Simons, Shahab, Brown, Perski, The association of smoking status with SARS-CoV-2 infection, hospitalisation and mortality from COVID 19: a living rapid evidence review (version 6), Qeios
Vahidy, Pan, Ahnstedt, Sex differences in susceptibility, severity, and outcomes of coronavirus disease 2019: crosssectional analysis from a diverse US metropolitan area, PLoS One, doi:10.1371/journal.pone.0245556
Williamson, Walker, Bhaskaran, Factors associated with COVID 19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Wu, Zhang, Sun, Influence of diabetes mellitus on the severity and fatality of SARS-CoV-2 (COVID 19) infection, Diabetes Obes Metab, doi:10.1111/dom.14105
Zhang, Dong, Cao, Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China, Allergy Eur J Allergy Clin Immunol, doi:10.1111/all.14238
Zhao, Meng, Kumar, The impact of COPD and smoking history on the severity of COVID 19: a systemic review and metaanalysis, J Med Virol, doi:10.1002/jmv.25889
Zhou, Yang, Chi, Comorbidities and the risk of severe or fatal outcomes associated with coronavirus disease 2019: a systematic review and meta-analysis, Int J Infect Dis, doi:10.1016/j.ijid.2020.07.029
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID 19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
DOI record:
{
"DOI": "10.2147/idr.s331470",
"ISSN": [
"1178-6973"
],
"URL": "http://dx.doi.org/10.2147/IDR.S331470",
"author": [
{
"ORCID": "http://orcid.org/0000-0003-3432-4559",
"affiliation": [],
"authenticated-orcid": true,
"family": "Mohsin",
"given": "Faroque Md",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-3264-9237",
"affiliation": [],
"authenticated-orcid": true,
"family": "Nahrin",
"given": "Ridwana",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4579-679X",
"affiliation": [],
"authenticated-orcid": true,
"family": "Tonmon",
"given": "Tajrin Tahrin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nesa",
"given": "Maherun",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0585-8658",
"affiliation": [],
"authenticated-orcid": true,
"family": "Tithy",
"given": "Sharmin Ahmed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Saha",
"given": "Shuvajit",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mannan",
"given": "Mahmudul",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2218-8433",
"affiliation": [],
"authenticated-orcid": true,
"family": "Shahjalal",
"given": "Md",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Faruque",
"given": "Mohammad Omar",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1443-6257",
"affiliation": [],
"authenticated-orcid": true,
"family": "Hawlader",
"given": "Mohammad Delwer Hossain",
"sequence": "additional"
}
],
"container-title": "Infection and Drug Resistance",
"container-title-short": "IDR",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
9,
29
]
],
"date-time": "2021-09-29T11:09:20Z",
"timestamp": 1632913760000
},
"deposited": {
"date-parts": [
[
2021,
9,
29
]
],
"date-time": "2021-09-29T11:10:00Z",
"timestamp": 1632913800000
},
"indexed": {
"date-parts": [
[
2022,
4,
1
]
],
"date-time": "2022-04-01T05:35:30Z",
"timestamp": 1648791330769
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2021,
9
]
]
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/3.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
9,
1
]
],
"date-time": "2021-09-01T00:00:00Z",
"timestamp": 1630454400000
}
}
],
"link": [
{
"URL": "https://www.dovepress.com/getfile.php?fileID=74171",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.dovepress.com/getfile.php?fileID=74171",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "301",
"original-title": [],
"page": "4057-4066",
"prefix": "10.2147",
"published": {
"date-parts": [
[
2021,
9
]
]
},
"published-online": {
"date-parts": [
[
2021,
9
]
]
},
"publisher": "Informa UK Limited",
"reference": [
{
"DOI": "10.1016/B978-0-12-375156-0.00013-8",
"author": "Burrell",
"doi-asserted-by": "publisher",
"first-page": "185",
"journal-title": "Fenner Whites Med Virol",
"key": "ref1",
"year": "2017"
},
{
"key": "ref2",
"unstructured": "Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, evaluation and treatment Coronavirus (COVID 19). StatPearls [Internet]; 2020. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32150360. Accessed September 23, 2021."
},
{
"key": "ref3",
"unstructured": "Ghebreyesus TA. WHO director-general’s opening remarks at the media briefing on COVID 19-11 March 2020 [Internet]. WHO Director General’s speeches; 2020:4. Available from: https://www.who.int/director-general/speeches/who-director-general-s-opening-remarks-at-the-media-briefing-on-COVID19—11-march-2020%0Ahttps://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-cov. Accessed September 23, 2021."
},
{
"key": "ref4",
"unstructured": "Johns Hopkins Coronavirus Resource Center. No title [Internet]; 2021 [cited July 13, 2021]. Available from: https://coronavirus.jhu.edu/map.html. Accessed September 23, 2021."
},
{
"key": "ref5",
"unstructured": "World Health Organization. Tracking SARS-CoV-2 variants [Internet]. Available from: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/. Accessed September 23, 2021."
},
{
"DOI": "10.1038/s41586-020-2521-4",
"author": "Williamson",
"doi-asserted-by": "publisher",
"first-page": "430",
"journal-title": "Nature",
"key": "ref6",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1002/oby.22831",
"author": "Simonnet",
"doi-asserted-by": "publisher",
"first-page": "1195",
"journal-title": "Obesity",
"key": "ref7",
"volume": "28",
"year": "2020"
},
{
"key": "ref8",
"unstructured": "Centre for Disease Control and Prevention (CDC). COVID 19 [Internet]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/index.html. Accessed September 23, 2021."
},
{
"DOI": "10.1136/jech-2019-213415",
"author": "Schlesinger",
"doi-asserted-by": "publisher",
"first-page": "481",
"journal-title": "J Epidemiol Community Health",
"key": "ref9",
"volume": "74",
"year": "2020"
},
{
"DOI": "10.1001/jamainternmed.2020.0618",
"author": "Nyberg",
"doi-asserted-by": "publisher",
"first-page": "760",
"journal-title": "JAMA Intern Med",
"key": "ref10",
"volume": "180",
"year": "2020"
},
{
"DOI": "10.1136/bmj.l6669",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "l6669",
"journal-title": "BMJ",
"key": "ref11",
"volume": "368",
"year": "2020"
},
{
"author": "Simons",
"first-page": "1319",
"journal-title": "Qeios",
"key": "ref12",
"volume": "116",
"year": "2020"
},
{
"key": "ref13",
"unstructured": "World no tobacco day. Med Today. 2002;3:7. WHO: https://www.who.int/campaigns/world-no-tobacco-day"
},
{
"key": "ref14",
"unstructured": "World Health Organization. WHO Statement: Tobacco Use and COVID 19. WHO; May, 2020:19–20."
},
{
"key": "ref15",
"unstructured": "Centre for Disease Control and Prevention (CDC). People at Increased Risk of COVID 19; 2020:2019–2021."
},
{
"DOI": "10.2298/VSP2005461I",
"author": "Igić",
"doi-asserted-by": "publisher",
"first-page": "461",
"journal-title": "Vojnosanit Pregl",
"key": "ref16",
"volume": "77",
"year": "2020"
},
{
"author": "Pötschke-Langer",
"first-page": "149",
"journal-title": "Prog Respir Res",
"key": "ref17",
"volume": "42",
"year": "2015"
},
{
"DOI": "10.1136/bmjnph-2021-000228",
"author": "Kim",
"doi-asserted-by": "publisher",
"first-page": "132",
"journal-title": "BMJ Nutr Prev Health",
"key": "ref18",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1016/j.bbi.2020.05.059",
"author": "Hamer",
"doi-asserted-by": "publisher",
"first-page": "184",
"journal-title": "Brain Behav Immun",
"key": "ref19",
"volume": "87",
"year": "2020"
},
{
"key": "ref20",
"unstructured": "International Centre for Diarrhoeal Disease Research Bangladesh. Non-communicable diseases. https://www.icddrb.org/research/research-themes/non-communicable-diseases"
},
{
"DOI": "10.1371/journal.pone.0141135",
"author": "Nargis",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "PLoS One",
"key": "ref21",
"volume": "10",
"year": "2015"
},
{
"DOI": "10.1093/ntr/ntu129",
"author": "Fischer",
"doi-asserted-by": "publisher",
"first-page": "58",
"journal-title": "Nicotine Tob Res",
"key": "ref22",
"volume": "17",
"year": "2015"
},
{
"key": "ref23",
"unstructured": "Coronavirus disease (COVID-2019) Bangladesh situation reports. https://www.who.int/bangladesh/emergencies/coronavirus-disease-(covid-19)-update/coronavirus-disease-(covid-2019)-bangladesh-situation-reports"
},
{
"key": "ref24",
"unstructured": "Bangladesh Society of Medicine. 2019-nCOV (SARS-COV-2) Infection Prevention Control (IPC) and Management in Healthcare Facilities; 2020."
},
{
"DOI": "10.1371/journal.pone.0241824",
"author": "Ho",
"doi-asserted-by": "publisher",
"first-page": "e0241824",
"journal-title": "PLoS One",
"key": "ref25",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.15585/mmwr.mm6939e1",
"author": "Boehmer",
"doi-asserted-by": "publisher",
"first-page": "1404",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "ref26",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.3389/fpubh.2020.00202",
"author": "Cortis",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Front Public Health",
"key": "ref27",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1093/pubmed/fdaa078",
"author": "Harlem",
"doi-asserted-by": "crossref",
"first-page": "466",
"journal-title": "J Public Health",
"key": "ref28",
"volume": "42",
"year": "2020"
},
{
"DOI": "10.3390/cells10040933",
"author": "Demeulemeester",
"doi-asserted-by": "publisher",
"journal-title": "Cells",
"key": "ref29",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.2337/dc20-0682",
"author": "Gao",
"doi-asserted-by": "publisher",
"first-page": "E72",
"journal-title": "Diabetes Care",
"key": "ref30",
"volume": "43",
"year": "2020"
},
{
"key": "ref31",
"unstructured": "World Health Organization. Update: 31 July 2020. WHO; July, 2020:1–203."
},
{
"DOI": "10.1093/ntr/ntaa059",
"author": "Berlin",
"doi-asserted-by": "publisher",
"first-page": "1650",
"journal-title": "Nicotine Tob Res",
"key": "ref32",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1007/s42399-020-00363-4",
"author": "Sanyaolu",
"doi-asserted-by": "publisher",
"first-page": "1069",
"journal-title": "SN Compr Clin Med",
"key": "ref33",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.07.029",
"author": "Zhou",
"doi-asserted-by": "publisher",
"first-page": "47",
"journal-title": "Int J Infect Dis",
"key": "ref34",
"volume": "99",
"year": "2020"
},
{
"DOI": "10.1111/dom.14105",
"author": "Wu",
"doi-asserted-by": "publisher",
"first-page": "1907",
"journal-title": "Diabetes Obes Metab",
"key": "ref35",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1038/s41569-020-0413-9",
"author": "Nishiga",
"doi-asserted-by": "publisher",
"first-page": "543",
"journal-title": "Nat Rev Cardiol",
"key": "ref36",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1093/ndt/gfaa314",
"author": "Ortiz",
"doi-asserted-by": "publisher",
"first-page": "87",
"journal-title": "Nephrol Dial Transplant",
"key": "ref37",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.2147/JMDH.S317603",
"author": "Mohsin",
"doi-asserted-by": "publisher",
"first-page": "1923",
"journal-title": "J Multidiscip Healthc",
"key": "ref38",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1111/all.14238",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "1730",
"journal-title": "Allergy Eur J Allergy Clin Immunol",
"key": "ref39",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"author": "Zhou",
"doi-asserted-by": "publisher",
"first-page": "1054",
"journal-title": "Lancet",
"key": "ref40",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/j.cmi.2020.05.041",
"author": "Cen",
"doi-asserted-by": "publisher",
"first-page": "1242",
"journal-title": "Clin Microbiol Infect",
"key": "ref41",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1002/jmv.25889",
"author": "Zhao",
"doi-asserted-by": "publisher",
"first-page": "1915",
"journal-title": "J Med Virol",
"key": "ref42",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.1111/j.1532-5415.1997.tb00970.x",
"author": "Newman",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Am Geriatr Soc",
"key": "ref43",
"volume": "45",
"year": "1997"
},
{
"DOI": "10.1371/journal.pone.0245556",
"author": "Vahidy",
"doi-asserted-by": "publisher",
"first-page": "e0245556",
"journal-title": "PLoS One",
"key": "ref44",
"volume": "16",
"year": "2021"
}
],
"reference-count": 44,
"references-count": 44,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.dovepress.com/lifestyle-and-comorbidity-related-risk-factors-of-severe-and-critical--peer-reviewed-fulltext-article-IDR"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Pharmacology (medical)",
"Infectious Diseases",
"Pharmacology"
],
"subtitle": [],
"title": "Lifestyle and Comorbidity-Related Risk Factors of Severe and Critical COVID-19 Infection: A Comparative Study Among Survived COVID-19 Patients in Bangladesh",
"type": "journal-article",
"volume": "Volume 14"
}
mohsin
