Early Pandemic Associations of Latitude, Sunshine Duration, and Vitamin D Status with COVID-19 Incidence and Fatalities: A Global Analysis of 187 Countries
, R., PLOS Global Public Health, doi:10.1371/journal.pgph.0004074, Dec 2024 (preprint)
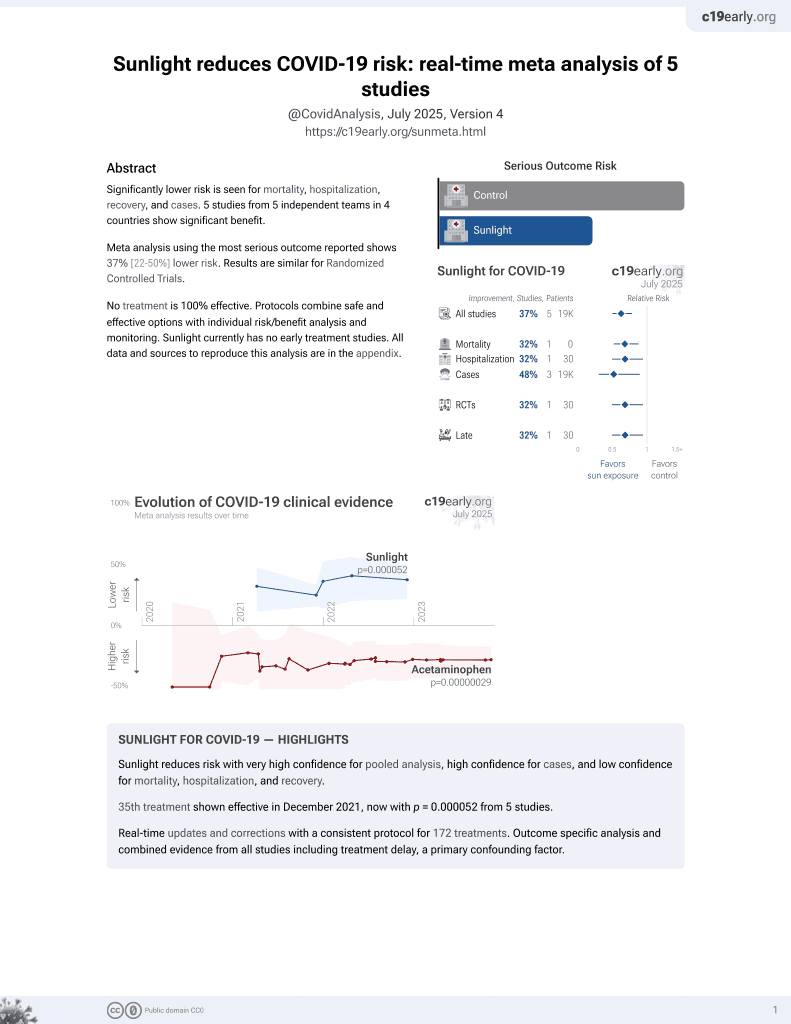
Sunlight for COVID-19
36th treatment shown to reduce risk in
December 2021, now with p = 0.000052 from 5 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
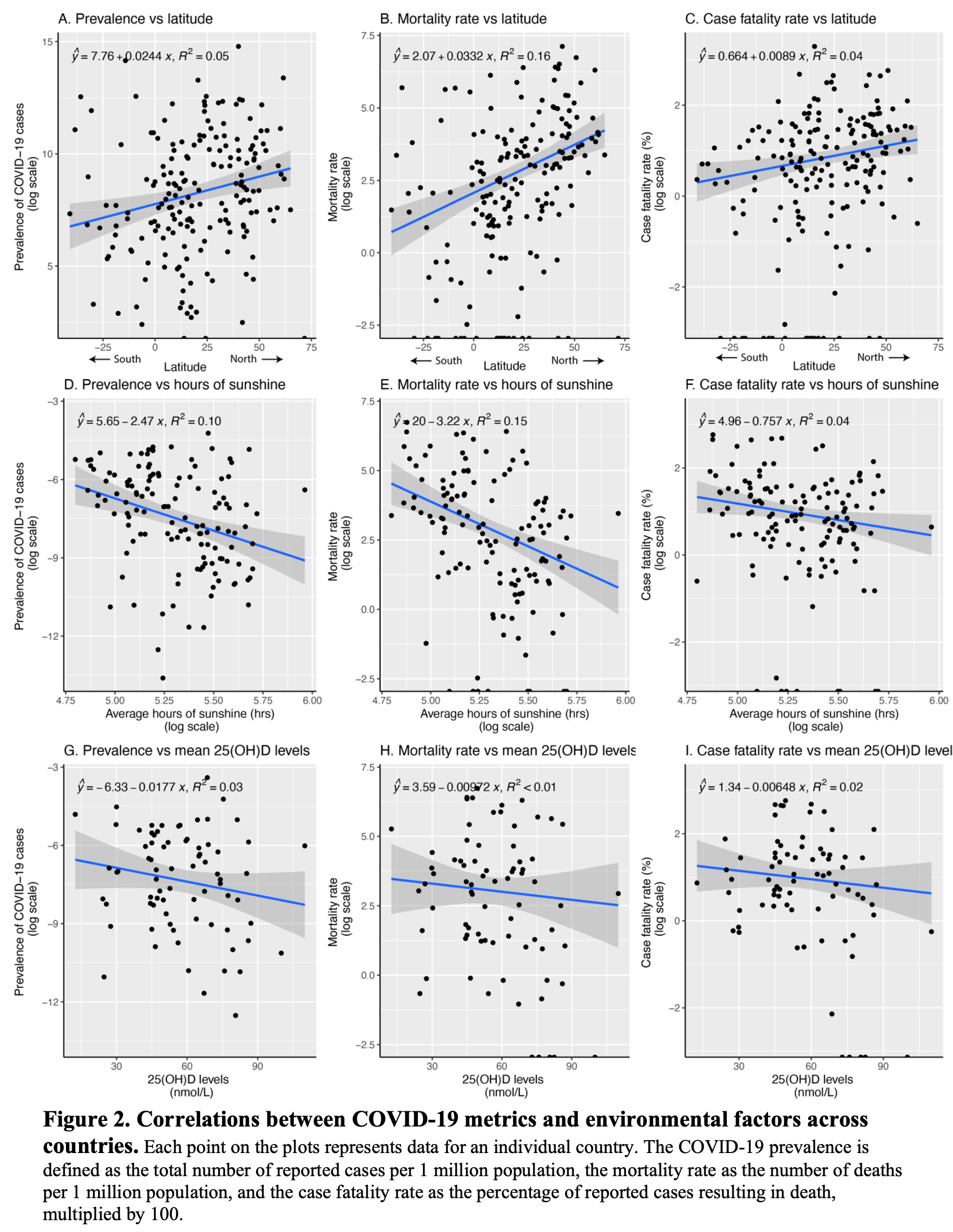
Analysis of 187 countries showing higher latitude and lower vitamin D levels associated with increased COVID-19 prevalence, mortality, and case fatality rates during the early months of the pandemic.
Study covers vitamin D and sunlight.
Mogire et al., 1 Dec 2024, retrospective, multiple countries, peer-reviewed, 1 author, study period January 2020 - June 2020.
Contact: reaganmoseti@gmail.com.
Early pandemic associations of latitude, sunshine duration, and vitamin D status with COVID-19 incidence and fatalities: A global analysis of 187 Countries
PLOS Global Public Health, doi:10.1371/journal.pgph.0004074
In the face of the COVID-19 pandemic, understanding the interplay between environmental factors and virus spread is crucial for global preparedness strategies. This study explores how geographic latitude, sunshine duration, and vitamin D status were associated with the incidence and fatality rates of COVID-19 across 187 countries during the crucial early months of the outbreak. Data on the total number of COVID-19 cases by country were obtained from the COVID-19 Data Repository by the Center for Systems Science and Engineering (CSSE) as of June 30, 2020. Univariate and multivariate regression analyses were conducted to determine the associations between COVID-19 cases and latitude, average hours of sunshine from January to June, and mean 25-hydroxyvitamin D (25(OH)D) levels. The average COVID-19 cumulative incidence and mortality per million population were 2,087 and 69, respectively, with a case fatality rate of 3.19%. COVID-19 case fatality rate was positively associated with latitude (β = 0.030; 95% CI: 0.008, 0.052) and negatively associated with hours of sunshine (β = -1.51; 95% CI: -4.44, 1.41) and 25(OH) D levels (β = -0.054; 95% CI: -0.089, -0.019) in adjusted linear regression analyses. Findings were similar for COVID-19 cumulative incidence and mortality rate. These findings indicate that higher latitude and lower 25(OH)D levels were associated with increased COVID-19 severity and mortality. While the data highlight potential links between vitamin D status and COVID-19 outcomes, causality cannot be inferred.
References
Asyary, Veruswati, Sunlight exposure increased Covid-19 recovery rates: A study in the central pandemic area of Indonesia, Sci Total Environ, doi:10.1016/j.scitotenv.2020.139016
Benedetti, Pachetti, Marini, Ippodrino, Gallo et al., Inverse correlation between average monthly high temperatures and COVID-19-related death rates in different geographical areas, J Transl Med, doi:10.1186/s12967-020-02418-5
Burki, Lifting of COVID-19 restrictions in the UK and the Delta variant, Lancet Respir Med, doi:10.1016/S2213-2600(21)00328-3
Byass, Eco-epidemiological assessment of the COVID-19 epidemic in China, January-February 2020, Glob Health Action, doi:10.1080/16549716.2020.1760490
Castillo, Costa, Barrios, Díaz, Miranda et al., Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, The Journal of Steroid Biochemistry and Molecular Biology
D'avolio, Avataneo, Manca, Cusato, Nicolò et al., 25-Hydroxyvitamin D Concentrations Are Lower in Patients with Positive PCR for SARS-CoV-2, Nutrients, doi:10.3390/nu12051359
Daneshkhah, Eshein, Subramanian, Roy, Backman, The role of vitamin D in suppressing cytokine storm in COVID-19 patients and associated mortality, MedRxiv
England, Disparities in the risk and outcomes of COVID-19
Fan, Zhao, Shi, Zhou, Bat Coronaviruses in China, Viruses, doi:10.3390/v11030210
Fauci, Lane, Redfield, Covid-19-navigating the uncharted, N Engl J Med
Gao, From "A"IV to "Z"IKV: Attacks from Emerging and Re-emerging Pathogens, Cell, doi:10.1016/j.cell.2018.02.025
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Hariyanto, Intan, Hananto, Harapan, Kurniawan, Vitamin D supplementation and Covid-19 outcomes: a systematic review, metaanalysis and meta-regression
Holick, Vitamin D deficiency, N Engl J Med, doi:10.1056/NEJMra070553
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin Exp Res, doi:10.1007/s40520-020-01570-8
Jolliffe, Holt, Greenig, Talaei, Perdek et al., Effect of a test-and-treat approach to vitamin D supplementation on risk of all cause acute respiratory tract infection and covid-19: phase 3 randomised controlled trial (CORONAVIT), BMJ
Jordan, Adab, Cheng, Covid-19: risk factors for severe disease and death, BMJ
Jääskeläinen, Itkonen, Lundqvist, Erkkola, Koskela et al., The positive impact of general vitamin D food fortification policy on vitamin D status in a representative adult Finnish population: evidence from an 11-y follow-up based on standardized 25-hydroxyvitamin D data, Am J Clin Nutr, doi:10.3945/ajcn.116.151415
Kirby, Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities, Lancet Respir Med, doi:10.1016/S2213-2600(20)30228-9
Kontis, Bennett, Rashid, Parks, Pearson-Stuttard et al., Magnitude, demographics and dynamics of the effect of the first wave of the COVID-19 pandemic on all-cause mortality in 21 industrialized countries, Nat Med, doi:10.1038/s41591-020-1112-0
Laird, Rhodes, Kenny, Vitamin D and Inflammation: Potential Implications for Severity of Covid-19, Ir Med J
Lawal, Africa's low COVID-19 mortality rate: A paradox?, Int J Infect Dis, doi:10.1016/j.ijid.2020.10.038
Lips, Cashman, Lamberg-Allardt, Bischoff-Ferrari, Obermayer-Pietsch et al., Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: a position statement of the European Calcified Tissue Society, Eur J Endocrinol, doi:10.1530/EJE-18-0736
Lowen, Mubareka, Steel, Palese, Influenza virus transmission is dependent on relative humidity and temperature, PLoS Pathog, doi:10.1371/journal.ppat.0030151
Mallapaty, Vaccines are curbing COVID: Data from Israel show drop in infections, Nature, doi:10.1038/d41586-021-00316-4
Martineau, Jolliffe, Hooper, Greenberg, Aloia et al., Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, BMJ
Meltzer, Best, Zhang, Vokes, Arora et al., Association of vitamin D deficiency and treatment with COVID-19 incidence, MedRxiv
Morens, Daszak, Taubenberger, Escaping Pandora's Box -Another Novel Coronavirus, N Engl J Med, doi:10.1056/NEJMp2002106
Munshi, Hussein, Toraih, Elshazli, Jardak et al., Vitamin D insufficiency as a potential culprit in critical COVID-19 patients, J Med Virol, doi:10.1002/jmv.26360
Murai, Fernandes, Sales, Pinto, Goessler et al., Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients With Moderate to Severe COVID-19: A Randomized Clinical Trial, JAMA, doi:10.1001/jama.2020.26848
Organization, WHO Coronavirus (COVID-19) Dashboard
Panarese, Shahini, Letter: Covid-19, and vitamin D, Aliment Pharmacol Ther, doi:10.1111/apt.15752
Rhodes, Subramanian, Laird, Kenny, Editorial: low population mortality from COVID-19 in countries south of latitude 35 degrees North supports vitamin D as a factor determining severity, Aliment Pharmacol Ther, doi:10.1111/apt.15777
Sajadi, Habibzadeh, Vintzileos, Shokouhi, Miralles-Wilhelm et al., Temperature, Humidity, and Latitude Analysis to Estimate Potential Spread and Seasonality of Coronavirus Disease 2019 (COVID-19), JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.11834
Sattar, Ho, Gill, Ghouri, Gray et al., BMI and future risk for COVID-19 infection and death across sex, age and ethnicity: Preliminary findings from UK biobank, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.06.060
Siuka, Pfeifer, Pinter, Vitamin D supplementation during the COVID-19 pandemic
Ssentongo, Ssentongo, Heilbrunn, Ba, Chinchilli, Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: A systematic review and meta-analysis, PLoS One, doi:10.1371/journal.pone.0238215
Whittemore, COVID-19 fatalities, latitude, sunlight, and vitamin D, American Journal of Infection Control
Woolhouse, Scott, Hudson, Howey, Chase-Topping, Human viruses: discovery and emergence, Philos Trans R Soc Lond B Biol Sci, doi:10.1098/rstb.2011.0354
Wösten-Van Asperen, Lutter, Specht, Moll, Van Woensel et al., Acute respiratory distress syndrome leads to reduced ratio of ACE/ACE2 activities and is prevented by angiotensin-(1-7) or an angiotensin II receptor antagonist, J Pathol, doi:10.1002/path.2987
Žmitek, Hribar, Lavriša, Hristov, Kušar et al., Socio-Demographic and Knowledge-Related Determinants of Vitamin D Supplementation in the Context of the COVID-19 Pandemic: Assessment of an Educational Intervention, Front Nutr, doi:10.3389/fnut.2021.648450
DOI record:
{
"DOI": "10.1371/journal.pgph.0004074",
"ISSN": [
"2767-3375"
],
"URL": "http://dx.doi.org/10.1371/journal.pgph.0004074",
"abstract": "<jats:p>In the face of the COVID-19 pandemic, understanding the interplay between environmental factors and virus spread is crucial for global preparedness strategies. This study explores how geographic latitude, sunshine duration, and vitamin D status were associated with the incidence and fatality rates of COVID-19 across 187 countries during the crucial early months of the outbreak. Data on the total number of COVID-19 cases by country were obtained from the COVID-19 Data Repository by the Center for Systems Science and Engineering (CSSE) as of June 30, 2020. Univariate and multivariate regression analyses were conducted to determine the associations between COVID-19 cases and latitude, average hours of sunshine from January to June, and mean 25-hydroxyvitamin D (25(OH)D) levels. The average COVID-19 cumulative incidence and mortality per million population were 2,087 and 69, respectively, with a case fatality rate of 3.19%. COVID-19 case fatality rate was positively associated with latitude (β = 0.030; 95% CI: 0.008, 0.052) and negatively associated with hours of sunshine (β = -1.51; 95% CI: -4.44, 1.41) and 25(OH)D levels (β = -0.054; 95% CI: -0.089, -0.019) in adjusted linear regression analyses. Findings were similar for COVID-19 cumulative incidence and mortality rate. These findings indicate that higher latitude and lower 25(OH)D levels were associated with increased COVID-19 severity and mortality. While the data highlight potential links between vitamin D status and COVID-19 outcomes, causality cannot be inferred.</jats:p>",
"author": [
{
"ORCID": "https://orcid.org/0000-0001-6454-1613",
"affiliation": [],
"authenticated-orcid": true,
"family": "Mogire",
"given": "Reagan M.",
"sequence": "first"
}
],
"container-title": "PLOS Global Public Health",
"container-title-short": "PLOS Glob Public Health",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.plosglobalpublichealth.org"
]
},
"created": {
"date-parts": [
[
2025,
7,
28
]
],
"date-time": "2025-07-28T17:42:18Z",
"timestamp": 1753724538000
},
"deposited": {
"date-parts": [
[
2025,
7,
28
]
],
"date-time": "2025-07-28T17:42:25Z",
"timestamp": 1753724545000
},
"editor": [
{
"affiliation": [],
"family": "Robinson",
"given": "Julia",
"sequence": "first"
}
],
"indexed": {
"date-parts": [
[
2025,
7,
30
]
],
"date-time": "2025-07-30T02:12:28Z",
"timestamp": 1753841548080,
"version": "3.41.2"
},
"is-referenced-by-count": 0,
"issue": "7",
"issued": {
"date-parts": [
[
2025,
7,
28
]
]
},
"journal-issue": {
"issue": "7",
"published-online": {
"date-parts": [
[
2025,
7,
28
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/publicdomain/zero/1.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
7,
28
]
],
"date-time": "2025-07-28T00:00:00Z",
"timestamp": 1753660800000
}
}
],
"link": [
{
"URL": "https://dx.plos.org/10.1371/journal.pgph.0004074",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "340",
"original-title": [],
"page": "e0004074",
"prefix": "10.1371",
"published": {
"date-parts": [
[
2025,
7,
28
]
]
},
"published-online": {
"date-parts": [
[
2025,
7,
28
]
]
},
"publisher": "Public Library of Science (PLoS)",
"reference": [
{
"author": "Organization WH",
"key": "pgph.0004074.ref001",
"year": "2024"
},
{
"DOI": "10.1056/NEJMe2002387",
"article-title": "Covid-19—navigating the uncharted",
"author": "AS Fauci",
"doi-asserted-by": "crossref",
"first-page": "1268",
"journal-title": "N Engl J Med",
"key": "pgph.0004074.ref002",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(21)00328-3",
"article-title": "Lifting of COVID-19 restrictions in the UK and the Delta variant",
"author": "TK Burki",
"doi-asserted-by": "crossref",
"issue": "8",
"journal-title": "Lancet Respir Med",
"key": "pgph.0004074.ref003",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1038/d41586-021-00316-4",
"article-title": "Vaccines are curbing COVID: Data from Israel show drop in infections",
"author": "S Mallapaty",
"doi-asserted-by": "crossref",
"first-page": "197",
"issue": "7845",
"journal-title": "Nature",
"key": "pgph.0004074.ref004",
"volume": "590",
"year": "2021"
},
{
"DOI": "10.1098/rstb.2011.0354",
"article-title": "Human viruses: discovery and emergence",
"author": "M Woolhouse",
"doi-asserted-by": "crossref",
"first-page": "2864",
"issue": "1604",
"journal-title": "Philos Trans R Soc Lond B Biol Sci",
"key": "pgph.0004074.ref005",
"volume": "367",
"year": "2012"
},
{
"article-title": "Covid-19: risk factors for severe disease and death",
"author": "RE Jordan",
"journal-title": "BMJ",
"key": "pgph.0004074.ref006",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0238215",
"article-title": "Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: A systematic review and meta-analysis",
"author": "P Ssentongo",
"doi-asserted-by": "crossref",
"issue": "8",
"journal-title": "PLoS One",
"key": "pgph.0004074.ref007",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.10.038",
"article-title": "Africa’s low COVID-19 mortality rate: A paradox?",
"author": "Y Lawal",
"doi-asserted-by": "crossref",
"first-page": "118",
"journal-title": "Int J Infect Dis",
"key": "pgph.0004074.ref008",
"volume": "102",
"year": "2021"
},
{
"DOI": "10.1016/S2213-2600(20)30228-9",
"article-title": "Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities",
"author": "T Kirby",
"doi-asserted-by": "crossref",
"first-page": "547",
"issue": "6",
"journal-title": "Lancet Respir Med",
"key": "pgph.0004074.ref009",
"volume": "8",
"year": "2020"
},
{
"author": "PH England",
"key": "pgph.0004074.ref010",
"volume-title": "Disparities in the risk and outcomes of COVID-19",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26360",
"article-title": "Vitamin D insufficiency as a potential culprit in critical COVID-19 patients",
"author": "R Munshi",
"doi-asserted-by": "crossref",
"first-page": "733",
"issue": "2",
"journal-title": "J Med Virol",
"key": "pgph.0004074.ref011",
"volume": "93",
"year": "2021"
},
{
"article-title": "Association of vitamin D deficiency and treatment with COVID-19 incidence",
"author": "DO Meltzer",
"journal-title": "MedRxiv",
"key": "pgph.0004074.ref012",
"volume": "2020",
"year": "2020"
},
{
"DOI": "10.3390/nu12040988",
"article-title": "Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths",
"author": "WB Grant",
"doi-asserted-by": "crossref",
"first-page": "988",
"issue": "4",
"journal-title": "Nutrients",
"key": "pgph.0004074.ref013",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.3390/nu12051359",
"article-title": "25-Hydroxyvitamin D Concentrations Are Lower in Patients with Positive PCR for SARS-CoV-2",
"author": "A D’Avolio",
"doi-asserted-by": "crossref",
"first-page": "1359",
"issue": "5",
"journal-title": "Nutrients",
"key": "pgph.0004074.ref014",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1056/NEJMra070553",
"article-title": "Vitamin D deficiency",
"author": "MF Holick",
"doi-asserted-by": "crossref",
"first-page": "266",
"issue": "3",
"journal-title": "N Engl J Med",
"key": "pgph.0004074.ref015",
"volume": "357",
"year": "2007"
},
{
"article-title": "Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data",
"author": "AR Martineau",
"journal-title": "BMJ",
"key": "pgph.0004074.ref016",
"volume": "356",
"year": "2017"
},
{
"article-title": "The role of vitamin D in suppressing cytokine storm in COVID-19 patients and associated mortality",
"author": "A Daneshkhah",
"journal-title": "MedRxiv",
"key": "pgph.0004074.ref017",
"year": "2020"
},
{
"DOI": "10.1016/j.mayocp.2020.05.036",
"author": "D Siuka",
"doi-asserted-by": "crossref",
"key": "pgph.0004074.ref018",
"volume-title": "Vitamin D supplementation during the COVID-19 pandemic",
"year": "2020"
},
{
"DOI": "10.1111/apt.15777",
"article-title": "Editorial: low population mortality from COVID-19 in countries south of latitude 35 degrees North supports vitamin D as a factor determining severity",
"author": "JM Rhodes",
"doi-asserted-by": "crossref",
"first-page": "1434",
"issue": "12",
"journal-title": "Aliment Pharmacol Ther",
"key": "pgph.0004074.ref019",
"volume": "51",
"year": "2020"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"article-title": "The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality",
"author": "PC Ilie",
"doi-asserted-by": "crossref",
"first-page": "1195",
"issue": "7",
"journal-title": "Aging Clin Exp Res",
"key": "pgph.0004074.ref020",
"volume": "32",
"year": "2020"
},
{
"article-title": "Vitamin D and Inflammation: Potential Implications for Severity of Covid-19",
"author": "E Laird",
"first-page": "81",
"issue": "5",
"journal-title": "Ir Med J",
"key": "pgph.0004074.ref021",
"volume": "113",
"year": "2020"
},
{
"DOI": "10.1016/j.ajic.2020.06.193",
"article-title": "COVID-19 fatalities, latitude, sunlight, and vitamin D",
"author": "PB Whittemore",
"doi-asserted-by": "crossref",
"first-page": "1042",
"issue": "9",
"journal-title": "American Journal of Infection Control",
"key": "pgph.0004074.ref022",
"volume": "48",
"year": "2020"
},
{
"DOI": "10.1056/NEJMp2002106",
"article-title": "Escaping Pandora’s Box - Another Novel Coronavirus",
"author": "DM Morens",
"doi-asserted-by": "crossref",
"first-page": "1293",
"issue": "14",
"journal-title": "N Engl J Med",
"key": "pgph.0004074.ref023",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2018.02.025",
"article-title": "From “A”IV to “Z”IKV: Attacks from Emerging and Re-emerging Pathogens",
"author": "GF Gao",
"doi-asserted-by": "crossref",
"first-page": "1157",
"issue": "6",
"journal-title": "Cell",
"key": "pgph.0004074.ref024",
"volume": "172",
"year": "2018"
},
{
"author": "United Nations DoEaSA, Population Division",
"key": "pgph.0004074.ref025",
"volume-title": "World Population Prospects 2019. Department of Economic and Social Affairs PD",
"year": "2019"
},
{
"author": "World Meteorological Organization",
"key": "pgph.0004074.ref026",
"volume-title": "World Weather Information ServiceReport No"
},
{
"DOI": "10.1111/apt.15752",
"article-title": "Letter: Covid-19, and vitamin D",
"author": "A Panarese",
"doi-asserted-by": "crossref",
"first-page": "993",
"issue": "10",
"journal-title": "Aliment Pharmacol Ther",
"key": "pgph.0004074.ref027",
"volume": "51",
"year": "2020"
},
{
"DOI": "10.1001/jamanetworkopen.2020.11834",
"article-title": "Temperature, Humidity, and Latitude Analysis to Estimate Potential Spread and Seasonality of Coronavirus Disease 2019 (COVID-19)",
"author": "MM Sajadi",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "JAMA Netw Open",
"key": "pgph.0004074.ref028",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1186/s12967-020-02418-5",
"article-title": "Inverse correlation between average monthly high temperatures and COVID-19-related death rates in different geographical areas",
"author": "F Benedetti",
"doi-asserted-by": "crossref",
"first-page": "251",
"issue": "1",
"journal-title": "J Transl Med",
"key": "pgph.0004074.ref029",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.3390/v11030210",
"article-title": "Bat Coronaviruses in China",
"author": "Y Fan",
"doi-asserted-by": "crossref",
"first-page": "210",
"issue": "3",
"journal-title": "Viruses",
"key": "pgph.0004074.ref030",
"volume": "11",
"year": "2019"
},
{
"DOI": "10.1371/journal.ppat.0030151",
"article-title": "Influenza virus transmission is dependent on relative humidity and temperature",
"author": "AC Lowen",
"doi-asserted-by": "crossref",
"first-page": "1470",
"issue": "10",
"journal-title": "PLoS Pathog",
"key": "pgph.0004074.ref031",
"volume": "3",
"year": "2007"
},
{
"DOI": "10.1080/16549716.2020.1760490",
"article-title": "Eco-epidemiological assessment of the COVID-19 epidemic in China, January-February 2020",
"author": "P Byass",
"doi-asserted-by": "crossref",
"first-page": "1760490",
"issue": "1",
"journal-title": "Glob Health Action",
"key": "pgph.0004074.ref032",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1016/j.scitotenv.2020.139016",
"article-title": "Sunlight exposure increased Covid-19 recovery rates: A study in the central pandemic area of Indonesia",
"author": "A Asyary",
"doi-asserted-by": "crossref",
"first-page": "139016",
"journal-title": "Sci Total Environ",
"key": "pgph.0004074.ref033",
"volume": "729",
"year": "2020"
},
{
"DOI": "10.1002/path.2987",
"article-title": "Acute respiratory distress syndrome leads to reduced ratio of ACE/ACE2 activities and is prevented by angiotensin-(1-7) or an angiotensin II receptor antagonist",
"author": "RM Wösten-van Asperen",
"doi-asserted-by": "crossref",
"first-page": "618",
"issue": "4",
"journal-title": "J Pathol",
"key": "pgph.0004074.ref034",
"volume": "225",
"year": "2011"
},
{
"DOI": "10.1016/j.dsx.2020.06.060",
"article-title": "BMI and future risk for COVID-19 infection and death across sex, age and ethnicity: Preliminary findings from UK biobank",
"author": "N Sattar",
"doi-asserted-by": "crossref",
"first-page": "1149",
"issue": "5",
"journal-title": "Diabetes Metab Syndr",
"key": "pgph.0004074.ref035",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1530/EJE-18-0736",
"article-title": "Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: a position statement of the European Calcified Tissue Society",
"author": "P Lips",
"doi-asserted-by": "crossref",
"issue": "4",
"journal-title": "Eur J Endocrinol",
"key": "pgph.0004074.ref036",
"volume": "180",
"year": "2019"
},
{
"DOI": "10.3945/ajcn.116.151415",
"article-title": "The positive impact of general vitamin D food fortification policy on vitamin D status in a representative adult Finnish population: evidence from an 11-y follow-up based on standardized 25-hydroxyvitamin D data",
"author": "T Jääskeläinen",
"doi-asserted-by": "crossref",
"first-page": "1512",
"issue": "6",
"journal-title": "Am J Clin Nutr",
"key": "pgph.0004074.ref037",
"volume": "105",
"year": "2017"
},
{
"DOI": "10.1038/s41591-020-1112-0",
"article-title": "Magnitude, demographics and dynamics of the effect of the first wave of the COVID-19 pandemic on all-cause mortality in 21 industrialized countries",
"author": "V Kontis",
"doi-asserted-by": "crossref",
"first-page": "1919",
"issue": "12",
"journal-title": "Nat Med",
"key": "pgph.0004074.ref038",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.3389/fnut.2021.648450",
"article-title": "Socio-Demographic and Knowledge-Related Determinants of Vitamin D Supplementation in the Context of the COVID-19 Pandemic: Assessment of an Educational Intervention",
"author": "K Žmitek",
"doi-asserted-by": "crossref",
"first-page": "648450",
"journal-title": "Front Nutr",
"key": "pgph.0004074.ref039",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.26848",
"article-title": "Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients With Moderate to Severe COVID-19: A Randomized Clinical Trial",
"author": "IH Murai",
"doi-asserted-by": "crossref",
"first-page": "1053",
"issue": "11",
"journal-title": "JAMA",
"key": "pgph.0004074.ref040",
"volume": "325",
"year": "2021"
},
{
"article-title": "Effect of a test-and-treat approach to vitamin D supplementation on risk of all cause acute respiratory tract infection and covid-19: phase 3 randomised controlled trial (CORONAVIT)",
"author": "DA Jolliffe",
"first-page": "378",
"journal-title": "BMJ",
"key": "pgph.0004074.ref041",
"year": "2022"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"article-title": "Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study",
"author": "ME Castillo",
"doi-asserted-by": "crossref",
"first-page": "105751",
"journal-title": "The Journal of Steroid Biochemistry and Molecular Biology",
"key": "pgph.0004074.ref042",
"volume": "203",
"year": "2020"
},
{
"article-title": "Vitamin D supplementation and Covid‐19 outcomes: a systematic review, meta‐analysis and meta‐regression",
"author": "TI Hariyanto",
"journal-title": "Wiley Online Library",
"key": "pgph.0004074.ref043",
"year": "2022"
}
],
"reference-count": 43,
"references-count": 43,
"relation": {},
"resource": {
"primary": {
"URL": "https://dx.plos.org/10.1371/journal.pgph.0004074"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Early pandemic associations of latitude, sunshine duration, and vitamin D status with COVID-19 incidence and fatalities: A global analysis of 187 Countries",
"type": "journal-article",
"update-policy": "https://doi.org/10.1371/journal.pgph.corrections_policy",
"volume": "5"
}
mogire