Cannabis Use and COVID-19 Hospitalization Outcomes. A Retrospective Study
et al., SSRN Electronic Journal, doi:10.2139/ssrn.4336513, Jan 2023
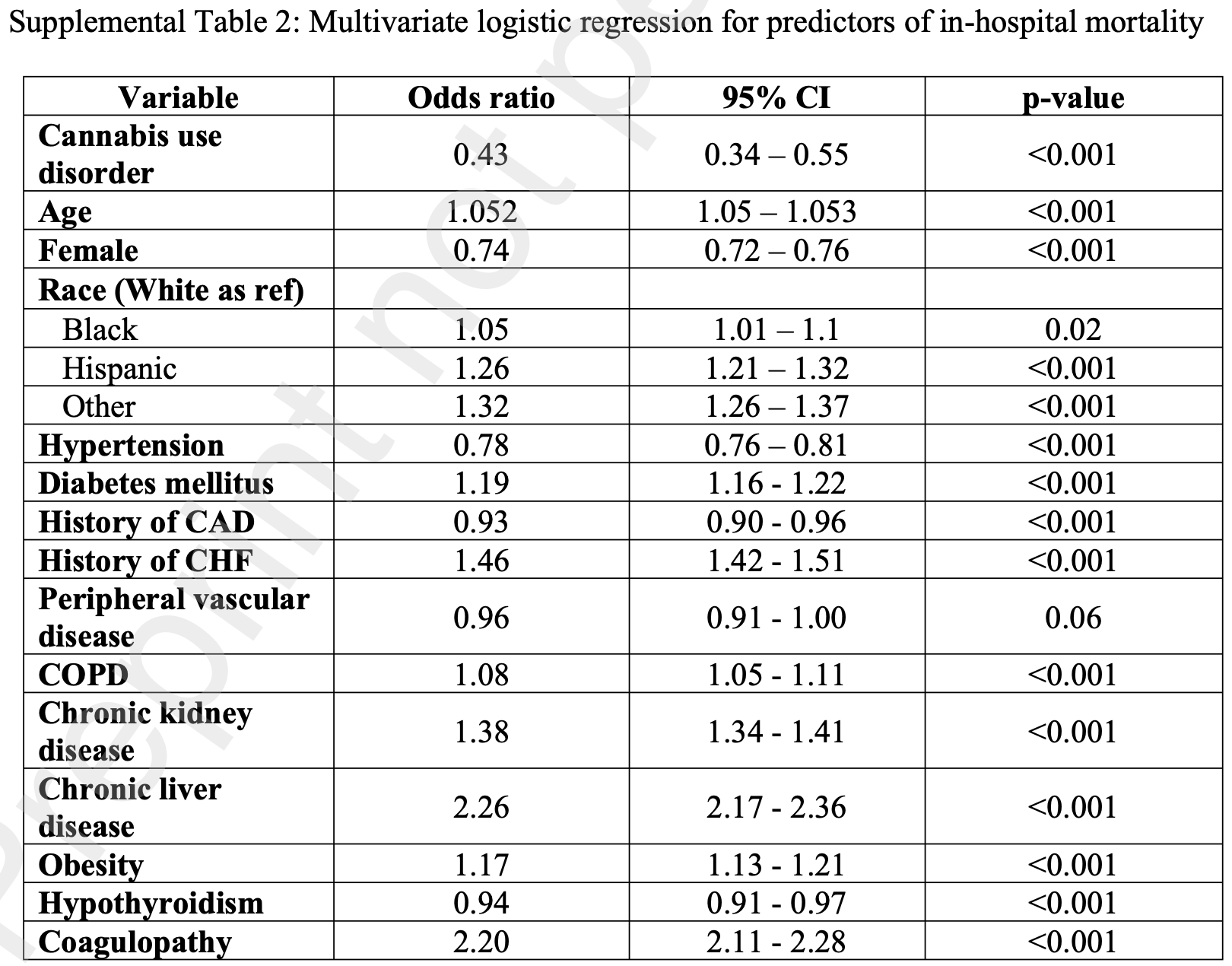
Retrospective 1,657,800 COVID-19 hospitalizations in the USA including 13,095 patients with cannabis use disorder, showing lower risk of mortality with cannabis use disorder. The text and Table S2 have conflicting results for mortality: 0.45 [0.36-0.57] versus 0.43 [0.34-0.55].
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 55.6% lower, RR 0.44, p < 0.001, treatment 380 of 13,095 (2.9%), control 1,430 of 26,190 (5.5%), NNT 39, odds ratio converted to relative risk.
|
|
risk of mechanical ventilation, 24.6% lower, RR 0.75, p < 0.001, treatment 925 of 13,095 (7.1%), control 2,455 of 26,190 (9.4%), NNT 43.
|
|
hospitalization time, 5.9% higher, relative time 1.06, p < 0.001, treatment mean 7.2 (±12.78) n=13,095, control mean 6.8 (±10.42) n=26,190.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Mannumbeth Renjithlal et al., 28 Jan 2023, retrospective, propensity score matching, USA, preprint, 7 authors, study period 1 January, 2020 - 31 December, 2020.
Contact: mrlalsarath@gmail.com.
Background In vitro studies have shown cannabinoids blocking SARS-CoV-2 cellular entry and affecting replication. There is a paucity of data assessing the effect of cannabis on patients hospitalized with COVID in the USA. The aim of our study was to assess mortality and complication rates in patients hospitalized with COVID stratified by cannabis use.
Methods We used the National Inpatient Sample, the largest all-payer inpatient database with 95% of US hospitalizations from 49 states, to identify all COVID hospitalizations from January 01, 2020, to December 31, 2020. We included all adult patients without missing mortality and gender information. The whole cohort was stratified by cannabis use into two groups (cannabis use disorder (CUD) vs. no CUD). We performed propensity score matching based on multiple patient and hospital characteristics to assess the outcome difference.
Results A total of 1,657,800 hospitalizations were included. Of these, 13,095 (0.79%) were cannabis users and were likely to be male (65.6%) and Black (35%) compared to non-cannabis users. After propensity score matching, the CUD group had lower mortality (2.9% compared to 5.5%, OR 0.43 [CI 0.34 -0.55] p <0.001). They also had lower rates of non-invasive (2.9% vs. 3.9 p <0.014), invasive mechanical ventilation (9.4% vs. 7.1%, p<0.001) and ECMO use (0.1 vs. 0.3 p <0.014). They also had a lower rate of septic shock (3.1% vs. 4% p<0.03) and lesser GI bleeding (3.3% vs. 2.3% p<0.005) compared to no CUD. The cost of hospitalization in the CUD group was significantly lower. There was no significant difference between the other complications assessed.
Conclusion We found lower mortality rates, lesser need for mechanical ventilation, and reduced hospitalization expenses among cannabis users hospitalized with
Vasopressor use (%) 195 (1.
References
-Anil, Shalev, Vinayaka, Nadarajan, Namdar et al., Cannabis compounds exhibit anti-inflammatory activity in vitro in COVID-19-related inflammation in lung epithelial cells and pro-inflammatory activity in macrophages, Sci Rep, doi:10.1038/s41598-021-81049-2
-Austin, An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies, Multivariate Behav Res
-Austin, Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies, Pharm Stat
-Borgonhi, Volpatto, Ornell, Rabelo-Da-Ponte, Kessler, Multiple clinical risks for cannabis users during the COVID-19 pandemic, Addict Sci Clin Pract, doi:10.1186/s13722-021-00214-0
-Dravet, Bureau, Oguni, Fukuyama, Cokar, Severe myoclonic epilepsy in infancy: Dravet syndrome, Adv Neurol
-Ghasemiesfe, Ravi, Vali, Korenstein, Arjomandi et al., Marijuana Use, Respiratory Symptoms, and Pulmonary Function: A Systematic Review and Metaanalysis, Ann Intern Med, doi:10.7326/M18-0522
-Golub, Reddy, Cannabidiol Therapy for Refractory Epilepsy and Seizure Disorders, Adv Exp Med Biol, doi:10.1007/978-3-030-57369-0_7
-Hoffmann, Kleine-Weber, Schroeder, Krüger, Herrler et al., SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor, Cell, doi:10.1016/j.cell.2020.02.052
-Hojyo, Uchida, Tanaka, Hasebe, Tanaka et al., How COVID-19 induces cytokine storm with high mortality, Inflamm Regen, doi:10.1186/s41232-020-00146-3
-Kendall, Yudowski, Cannabinoid Receptors in the Central Nervous System: Their Signaling and Roles in Disease, Front Cell Neurosci, doi:10.3389/fncel.2016.00294
-Nguyen, Yang, Nicolaescu, Best, Gula et al., Cannabidiol inhibits SARS-CoV-2 replication through induction of the host ER stress and innate immune responses, Sci Adv
-Paland, Pechkovsky, Aswad, Hamza, Popov et al., The Immunopathology of COVID-19 and the Cannabis Paradigm, Front Immunol, doi:10.3389/fimmu.2021.631233
-Peng, An, Ni, Huang, Luo, A narrative review of molecular mechanism and therapeutic effect of cannabidiol (CBD), Basic & Clinical Pharmacology & Toxicology, doi:10.1111/bcpt.13710
-Raj, Park, Cho, Choi, Kim et al., Assessment of antiviral potencies of cannabinoids against SARS-CoV-2 using computational and in vitro approaches, Int J Biol Macromol, doi:10.1016/j.ijbiomac.2020.12.020
-Rom, Slava, Persidsky, Cannabinoid receptor 2: potential role in immunomodulation and neuroinflammation, Journal of Neuroimmune Pharmacology
-Saadatian-Elahi, Amour, Elias, Henaff, Dananché et al., Tobacco smoking and severity of COVID-19: Experience from a hospital-based prospective cohort study in Lyon, France, J Med Virol, doi:10.1002/jmv.27233
-Sekar, Pack, Epidiolex as adjunct therapy for treatment of refractory epilepsy: a comprehensive review with a focus on adverse effects, doi:10.12688/f1000research.16515.1
-Sholler, Huestis, Amendolara, Vandrey, Cooper, Therapeutic potential and safety considerations for the clinical use of synthetic cannabinoids, Pharmacol Biochem Behav, doi:10.1016/j.pbb.2020.173059
-Van Breemen, Muchiri, Bates, Weinstein, Leier et al., Cannabinoids Block Cellular Entry of SARS-CoV-2 and the Emerging Variants, J Nat Prod, doi:10.1021/acs.jnatprod.1c00946
-Von Wrede, Helmstaedter, Surges, Cannabidiol in the Treatment of Epilepsy, Clin Drug Investig, doi:10.1007/s40261-021-01003-y
-Zuardi, Waldo, Antipsychotic effect of cannabidiol, The Journal of clinical psychiatry
Crippa, Pacheco, Zuardi, Guimarães, Campos et al., Cannabidiol for COVID-19 Patients with Mild to Moderate Symptoms (CANDIDATE Study): A Randomized, Double-Blind, Placebo-Controlled Clinical Trial, Cannabis Cannabinoid Res, doi:10.1089/can.2021.0093
Jha, Sharma, Hashiesh, Arunachalam, Meeran et al., β-Caryophyllene, A Natural Dietary CB2 Receptor Selective Cannabinoid can be a Candidate to Target the Trinity of Infection, Immunity, and Inflammation in COVID-19, Front Pharmacol, doi:10.3389/fphar.2021.590201
Malinowska, Baranowska-Kuczko, Kicman, Schlicker, Opportunities, Challenges and Pitfalls of Using Cannabidiol as an Adjuvant Drug in COVID-19, Int J Mol Sci, doi:10.3390/ijms22041986
Mcallister, Murase, Christian, Lau, Zielinski et al., Pathways mediating the effects of cannabidiol on the reduction of breast cancer cell proliferation, invasion, and metastasis, Breast Cancer Res Treat, doi:10.1007/s10549-010-1177-4
Ramer, Merkord, Rohde, Hinz, Cannabidiol inhibits cancer cell invasion via upregulation of tissue inhibitor of matrix metalloproteinases-1, Biochem Pharmacol, doi:10.1016/j.bcp.2009.11.007
Roehler, Hoots, Holland, Baldwin, Vivolo-Kantor, Trends and characteristics of cannabis-associated emergency department visits in the United States, 2006-2018, Drug Alcohol Depend, doi:10.1016/j.drugalcdep.2022.109288
Shover, Yan, Jackson, Buhr, Fulcher et al., Cannabis consumption is associated with lower COVID-19 severity among hospitalized patients: a retrospective cohort analysis, Journal of Cannabis Research
Stulberg, Haut, Practical Guide to Surgical Data Sets: Healthcare Cost and Utilization Project National Inpatient Sample (NIS), JAMA Surgery, doi:10.1001/jamasurg.2018.0542
Vilela, Lima, Kunsch, Pinto, De Miranda et al., Anticonvulsant effect of cannabidiol in the pentylenetetrazole model: Pharmacological mechanisms, electroencephalographic profile, and brain cytokine levels, Epilepsy Behav, doi:10.1016/j.yebeh.2017.07.014
DOI record:
{
"DOI": "10.2139/ssrn.4336513",
"ISSN": [
"1556-5068"
],
"URL": "http://dx.doi.org/10.2139/ssrn.4336513",
"author": [
{
"affiliation": [],
"family": "Mannumbeth Renjithlal",
"given": "Sarath Lal",
"sequence": "first"
},
{
"affiliation": [],
"family": "Eid",
"given": "Mohamed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Azhar",
"given": "Abdullah Zoheb",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mannumbeth Renjith",
"given": "Keerthi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "El-Daher",
"given": "Nayef",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alweis",
"given": "Richard",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mohammed",
"given": "Moghniuddin",
"sequence": "additional"
}
],
"container-title": "SSRN Electronic Journal",
"container-title-short": "SSRN Journal",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
1,
31
]
],
"date-time": "2023-01-31T13:57:58Z",
"timestamp": 1675173478000
},
"deposited": {
"date-parts": [
[
2023,
1,
31
]
],
"date-time": "2023-01-31T13:57:59Z",
"timestamp": 1675173479000
},
"indexed": {
"date-parts": [
[
2023,
1,
31
]
],
"date-time": "2023-01-31T14:14:51Z",
"timestamp": 1675174491361
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023
]
]
},
"language": "en",
"member": "78",
"original-title": [],
"prefix": "10.2139",
"published": {
"date-parts": [
[
2023
]
]
},
"published-online": {
"date-parts": [
[
2023
]
]
},
"publisher": "Elsevier BV",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.ssrn.com/abstract=4336513"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Earth and Planetary Sciences",
"General Environmental Science"
],
"subtitle": [],
"title": "Cannabis Use and COVID-19 Hospitalization Outcomes. A Retrospective Study",
"type": "journal-article"
}