Risk of severe case in COVID-19 patients and Azvudine: A Retrospective cohort study after exit from ‘zero-COVID’ policy
et al., Research Square, doi:10.21203/rs.3.rs-3707560/v1, NCT06006611, Jan 2024
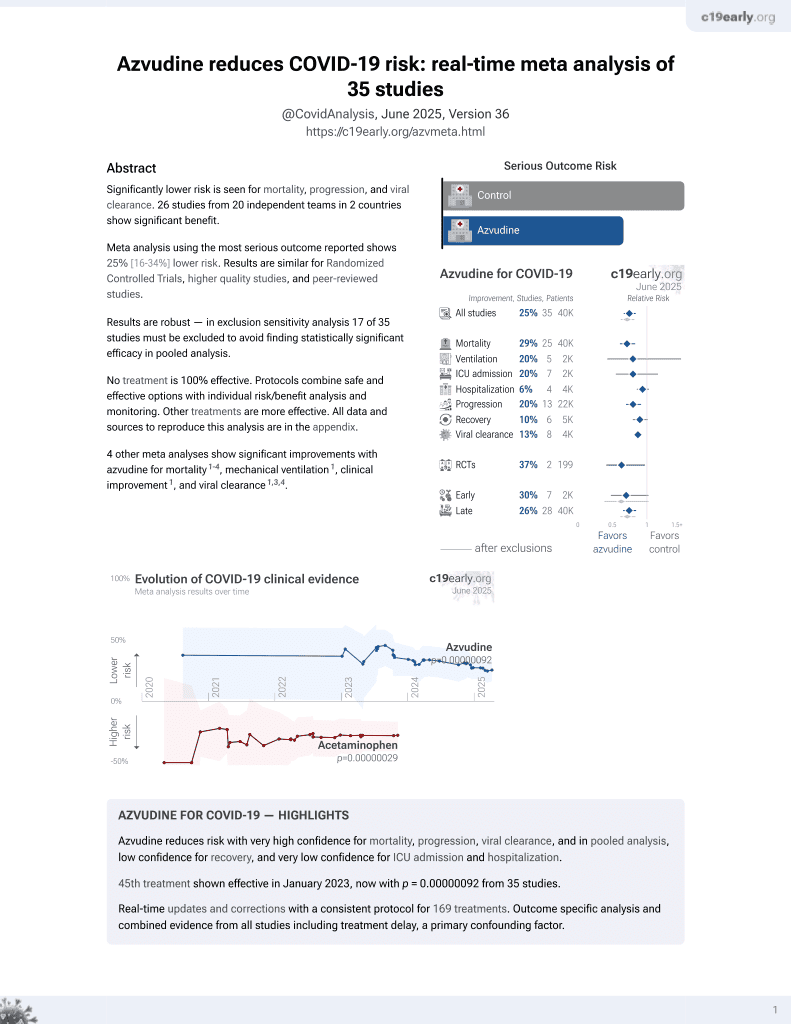
Azvudine for COVID-19
48th treatment shown to reduce risk in
January 2023, now with p = 0.000000017 from 39 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 4,201 hospitalized COVID-19 patients in China, showing lower mortality with azvudine.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments3.
|
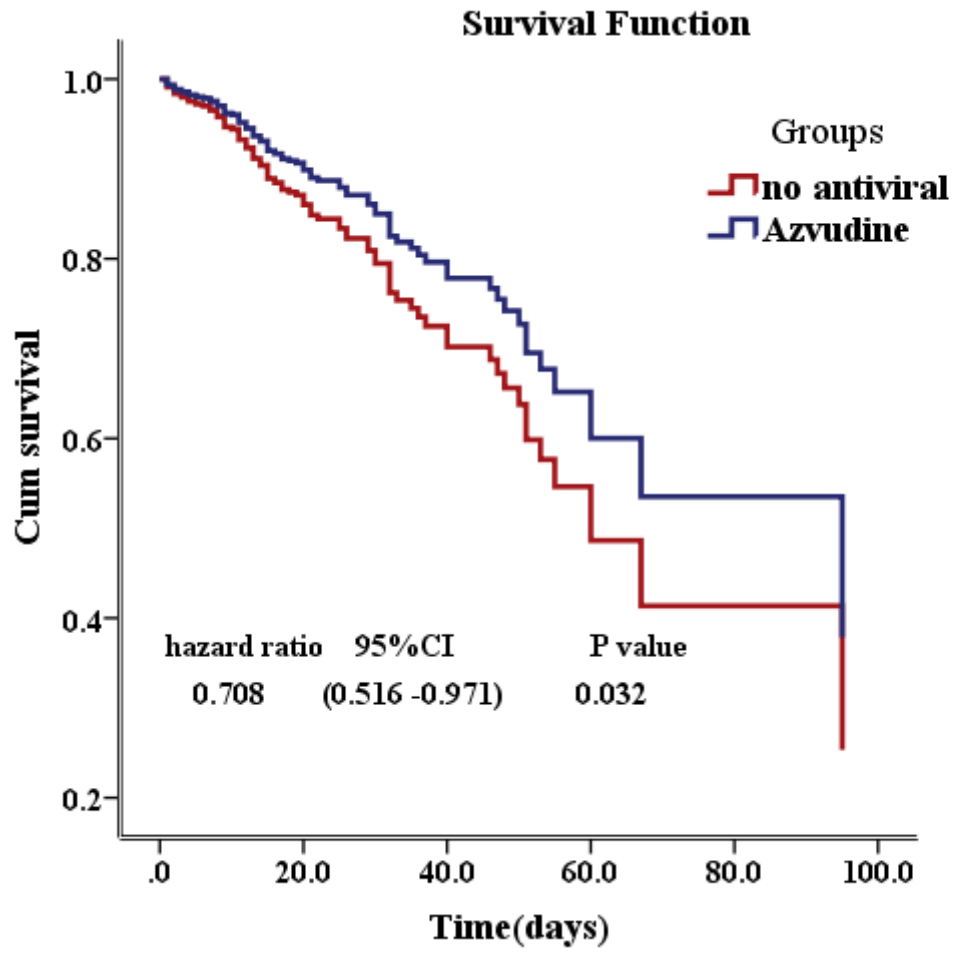
risk of death, 29.2% lower, HR 0.71, p = 0.03, treatment 1,103, control 1,103, propensity score matching, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Xiong et al., Real-world data of Azvudine-induced hepatotoxicity among hospitalized COVID-19 patients in China: a retrospective case-control study, Frontiers in Pharmacology, doi:10.3389/fphar.2025.1558054.
Li et al., 5 Jan 2024, retrospective, China, preprint, 7 authors, study period 1 November, 2022 - 31 May, 2023, trial NCT06006611 (history).
Contact: 850144863@qq.com, 156318962@qq.com, 254241317@qq.com, 20160611@qq.com, ling2005.hi@163.com, iznaug@163.com, bz232@163.com.
Risk of severe case in COVID-19 patients and Azvudine: A Retrospective cohort study after exit from 'zero-COVID' policy
Background: COVID-19 leaded to significant morbidity and mortality. To investigate contributing factors to severity and examine whether Azvudine can reduce mortality, we conducted a single-center, retrospective cohort study. Method: 4201 COVID-19 patients discharged from our hospital were enrolled. Logistic regression analysis and ROC curve were used to investigate the role of comorbidities, laboratory parameters and clinical manifestation on progression of COVID-19. Propensity-score models conditional on baseline characteristics and Univariate Cox regression model were used to examine whether Azvudine can reduce the mortality of COVID-19. Result: Age, male sex, cerebrovascular disease, chronic kidney disease, liver disease, tumor and chronic lung disease were associated with elevated risk of mortality and chronic kidney disease contributed the most risk. Uric acid showed a U-shape risk of severity. Both hyperuricemia and hypouricemia increased the risk of severity. D-dimer,NT-BNP, LDH and FT3 were the most sensitive and specific markers for the prediction of mortality. Poor appetite, consciousness deterioration, polypnea and persistent high fever were associated with elevated risk of severity. Compared with no antiviral group, Azvudine can reduce the COVID-19 mortality (hazard ratio 0.708(95% confidence interval 0.516 to 0.971), P=0.032. There was no significant difference in mortality reduction between Molnupiravir and Azvudine(P=0.486). Conclusions: Among COVID-19 patients, age, male sex and comorbidities can affect progression of COVID-19. D-dimer , NT-BNP, LDH, FT3, UA, poor appetite, consciousness deterioration, polypnea and persistent high fever can help doctors predict severe illness. Azvudine is neck and neck with Molnupiravir in the mortality reduction among COIVD-19.
Authors' contributions All authors participated in the design of the study. Zhuang Bian performed the statistical analysis. Lishan Li was the major contributor in writing the manuscript. All authors read and approved the final manuscript. Ethical approval and consent to participate The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Ethics Committee of the Fifth Affiliated Hospital of Sun Yat-sen University ([2023] K171-1). Informed consent waiver with Institutional Ethics Committee of the Fifth Affiliated Hospital of Sun Yat-sen University.
Consent to publication
Not applicable
Competing interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Supplementary Files
References
Baldelli, Nicastri, Petrosillo, Marchioni, Gubbiotti et al., Thyroid dysfunction in COVID-19 patients, Journal of Endocrinological Investigation
Boonpiyathad, Szener, Satitsuksanoa, Akdis, Immunologic mechanisms in asthma, Seminars in immunology
Dufour, Werion, Belkhir, Wisniewska, Yildiz, Serum uric acid, disease severity and outcomes in COVID-19, Critical Care
Dugerdil, Semenzato, Weill, Zureik, Flahault, Severe SARS-CoV-2 infection as a marker of undiagnosed cancer: a population-based study, Sci Rep
Felsenstein, Herbert, Mcnamara, Hedrich, COVID-19: Immunology and treatment options, Clinical Immunology
Gianfrancesco, Hyrich, Aladely, Carmona, Danila et al., Characteristics associated with hospitalisation for COVID-19 in people with rheumatic disease: data from the COVID-19 Global Rheumatology Alliance physician-reported registry, Annals of the Rheumatic Diseases
Group, Aspirin in patients admitted to hospital with COVID-19 (RECOVERY) : a randomised, controlled, open-label, platform trial
Hou, Zhao, Martin, Kallianpur, Cheng, New insights into genetic susceptibility of COVID-19: an ACE2 and TMPRSS2 polymorphism analysis, BMC Medicine
Lee, Chang-Hwanjang, Jinlee, Chang-Hoon, Renin-angiotensin system blocker and outcomes of COVID-19: a systematic review and meta-analysis, Thorax: The Journal of the British Thoracic Society
Macchia, La, Sorsa, Urbani, Moretti et al., Eosinophils as potential biomarkers in respiratory viral infections, Front Immunol
Pawlos, Niedzielski, Gorzelak-Pabiś, Broncel, Woźniak, COVID-19: direct and indirect mechanisms of statins, International Journal of Molecular Sciences
Savarino, Trani, Donatelli, Cauda, Cassone, New insights into the antiviral effects of chloroquine, Retour au numé
Schlter, Dürholz, Bucci, Burmester, Schett, Does methotrexate influence COVID-19 infection? Case series and mechanistic data, Arthritis Research & Therapy
Singh, Singh, Singh, Misra, Molnupiravir in COVID-19: A systematic review of literature, Diabetes & Metabolic Syndrome: Clinical Research & Reviews
Uk, COVID-19: consider cytokine storm syndromes and immunosuppression, The Lancet
Wakabayashi, Pawankar, Narazaki, Ueda, Itabashi, Coronavirus disease 2019 and asthma, allergic rhinitis: molecular mechanisms and host-environmental interactions, Current Opinion in Allergy and Clinical Immunology
Xu, Li, Guo, Ikezoe, Dalman, Angiotensin-converting enzyme 2, coronavirus disease 2019 and abdominal aortic aneurysms, Journal of Vascular Surgery
Xue, Sun, Cai, Zeng, Huo, Effects of ACEI and ARB on COVID-19 patients: A meta-analysis, Journal of Renin-Angiotensin-Aldosterone System
Yanai, Adachi, Hakoshima, Katsuyama, Molecular Biological and Clinical Understanding of the Pathophysiology and Treatments of Hyperuricemia and Its Association with Metabolic Syndrome, Cardiovascular Diseases and Chronic Kidney Disease
Yu, Chang, Azvudine(FNC):a promising clinical candidate for COVID-19 treatment
Zhang, Qin, Cheng, Shen, Li, In-Hospital Use of Statins Is Associated with a Reduced Risk of Mortality among Individuals with COVID-19, Cell Metabolism
DOI record:
{
"DOI": "10.21203/rs.3.rs-3707560/v1",
"URL": "http://dx.doi.org/10.21203/rs.3.rs-3707560/v1",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:p><jats:bold>Background</jats:bold> COVID-19 leaded to significant morbidity and mortality. To investigate contributing factors to severity and examine whether Azvudine can reduce mortality, we conducted a single-center, retrospective cohort study.<jats:bold>Method</jats:bold> 4201 COVID-19 patients discharged from our hospital were enrolled. Logistic regression analysis and ROC curve were used to investigate the role of comorbidities, laboratory parameters and clinical manifestation on progression of COVID-19. Propensity-score models conditional on baseline characteristics and Univariate Cox regression model were used to examine whether Azvudine can reduce the mortality of COVID-19.<jats:bold>Result</jats:bold> Age, male sex, cerebrovascular disease, chronic kidney disease, liver disease, tumor and chronic lung disease were associated with elevated risk of mortality and chronic kidney disease contributed the most risk. Uric acid showed a U-shape risk of severity. Both hyperuricemia and hypouricemia increased the risk of severity. D-dimer, NT-BNP, LDH and FT3 were the most sensitive and specific markers for the prediction of mortality. Poor appetite, consciousness deterioration, polypnea and persistent high fever were associated with elevated risk of severity. Compared with no antiviral group, Azvudine can reduce the COVID-19 mortality (hazard ratio 0.708(95% confidence interval 0.516 to 0.971), P = 0.032. There was no significant difference in mortality reduction between Molnupiravir and Azvudine(P = 0.486).<jats:bold>Conclusions</jats:bold> Among COVID-19 patients, age, male sex and comorbidities can affect progression of COVID-19. D-dimer, NT-BNP, LDH, FT3, UA, poor appetite, consciousness deterioration, polypnea and persistent high fever can help doctors predict severe illness. Azvudine is neck and neck with Molnupiravir in the mortality reduction among COIVD-19.</jats:p>",
"accepted": {
"date-parts": [
[
2023,
12,
5
]
]
},
"author": [
{
"affiliation": [
{
"name": "The Fifth Affiliated Hospital of Sun Yat-sen University"
}
],
"family": "Li",
"given": "Lishan",
"sequence": "first"
},
{
"affiliation": [
{
"name": "The Fifth Affiliated Hospital of Sun Yat-sen University"
}
],
"family": "Li",
"given": "Li",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "The Fifth Affiliated Hospital of Sun Yat-sen University"
}
],
"family": "Ye",
"given": "Lihua",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "The Fifth Affiliated Hospital of Sun Yat-sen University"
}
],
"family": "Lu",
"given": "Baijie",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "The Fifth Affiliated Hospital of Sun Yat-sen University"
}
],
"family": "Wang",
"given": "Jieling",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "The Fifth Affiliated Hospital of Sun Yat-sen University"
}
],
"family": "Wei",
"given": "Guanhua",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "The Fifth Affiliated Hospital of Sun Yat-sen University"
}
],
"family": "Bian",
"given": "Zhuang",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
1,
5
]
],
"date-time": "2024-01-05T17:52:08Z",
"timestamp": 1704477128000
},
"deposited": {
"date-parts": [
[
2024,
1,
5
]
],
"date-time": "2024-01-05T17:52:15Z",
"timestamp": 1704477135000
},
"group-title": "In Review",
"indexed": {
"date-parts": [
[
2024,
1,
6
]
],
"date-time": "2024-01-06T00:18:42Z",
"timestamp": 1704500322336
},
"institution": [
{
"name": "Research Square"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
1,
5
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
1,
5
]
],
"date-time": "2024-01-05T00:00:00Z",
"timestamp": 1704412800000
}
}
],
"link": [
{
"URL": "https://www.researchsquare.com/article/rs-3707560/v1",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.researchsquare.com/article/rs-3707560/v1.html",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "8761",
"original-title": [],
"posted": {
"date-parts": [
[
2024,
1,
5
]
]
},
"prefix": "10.21203",
"published": {
"date-parts": [
[
2024,
1,
5
]
]
},
"publisher": "Research Square Platform LLC",
"reference": [
{
"author": "Singh AK",
"key": "ref1",
"unstructured": "Singh AK, Singh A, Singh R, Misra A. \"Molnupiravir in COVID-19: A systematic review of literature,\" Diabetes & Metabolic Syndrome: Clinical Research & Reviews, vol. 15, p. 102329, 2021.",
"year": "2021"
},
{
"author": "Yu B",
"key": "ref2",
"unstructured": "Yu B, Chang J. \"Azvudine(FNC):a promising clinical candidate for COVID-19 treatment,\", p. 005, 2020.",
"year": "2020"
},
{
"author": "Boonpiyathad T",
"journal-title": "\"Immunologic Mech asthma \" Seminars Immunol",
"key": "ref3",
"unstructured": "Boonpiyathad T, Szener ZC, Satitsuksanoa P, Akdis CA. \"Immunologic Mech asthma \" Seminars Immunol, 2019.",
"year": "2019"
},
{
"DOI": "10.1097/ACI.0000000000000699",
"article-title": "Coronavirus disease 2019 and asthma, allergic rhinitis: molecular mechanisms and host–environmental interactions,",
"author": "Wakabayashi M",
"doi-asserted-by": "crossref",
"journal-title": "Curr Opin Allergy Clin Immunol",
"key": "ref4",
"unstructured": "Wakabayashi M, Pawankar R, Narazaki H, Ueda T, Itabashi T. Coronavirus disease 2019 and asthma, allergic rhinitis: molecular mechanisms and host–environmental interactions, Curr Opin Allergy Clin Immunol, vol. 21, 2021.",
"volume": "21",
"year": "2021"
},
{
"article-title": "Angiotensin-converting enzyme 2, coronavirus disease 2019 and abdominal aortic aneurysms,",
"author": "Xu B",
"journal-title": "J Vasc Surg",
"key": "ref5",
"unstructured": "Xu B, Li G, Guo J, Ikezoe T, Dalman RL. Angiotensin-converting enzyme 2, coronavirus disease 2019 and abdominal aortic aneurysms, J Vasc Surg, 2021.",
"year": "2021"
},
{
"author": "Schlter F",
"key": "ref6",
"unstructured": "Schlter F, Dürholz K, Bucci L, Burmester G, Schett G. Does methotrexate influence COVID-19 infection? Case series and mechanistic data. Volume 23. Arthritis Research & Therapy; 2021.",
"volume-title": "Does methotrexate influence COVID-19 infection? Case series and mechanistic data",
"year": "2021"
},
{
"article-title": "Characteristics associated with hospitalisation for COVID-19 in people with rheumatic disease: data from the COVID-19 Global Rheumatology Alliance physician-reported registry,",
"author": "Gianfrancesco M",
"journal-title": "Ann Rheum Dis",
"key": "ref7",
"unstructured": "Gianfrancesco M, Hyrich KL, Aladely S, Carmona L, Danila MI, Gossec L, Izadi Z, Jacobsohn L, Katz P, Lawsontovey S. Characteristics associated with hospitalisation for COVID-19 in people with rheumatic disease: data from the COVID-19 Global Rheumatology Alliance physician-reported registry, Ann Rheum Dis, vol. 79, pp. annrheumdis-2020-217871, 2020.",
"volume": "79"
},
{
"key": "ref8"
},
{
"DOI": "10.1186/s12916-020-01673-z",
"article-title": "New insights into genetic susceptibility of COVID-19: an ACE2 and TMPRSS2 polymorphism analysis",
"author": "Hou Y",
"doi-asserted-by": "crossref",
"first-page": "216",
"journal-title": "BMC Med",
"key": "ref9",
"unstructured": "Hou Y, Zhao J, Martin W, Kallianpur A, Cheng F. New insights into genetic susceptibility of COVID-19: an ACE2 and TMPRSS2 polymorphism analysis. BMC Med. 2020;18:216.",
"volume": "18",
"year": "2020"
},
{
"author": "A PM",
"key": "ref10",
"unstructured": "A PM, F MAE, C MB, D ES, H RSTG, M. JJ, B. and H. A. S. C. Uk, \"COVID-19: consider cytokine storm syndromes and immunosuppression,\" The Lancet, vol. 395, 2020.",
"year": "2020"
},
{
"DOI": "10.1177/1470320320981321",
"article-title": "Effects of ACEI and ARB on COVID-19 patients: A meta-analysis",
"author": "Xue Y",
"doi-asserted-by": "crossref",
"first-page": "147032032098132",
"journal-title": "J Renin-Angiotensin-Aldosterone Syst",
"key": "ref11",
"unstructured": "Xue Y, Sun S, Cai J, Zeng L, Huo J. Effects of ACEI and ARB on COVID-19 patients: A meta-analysis. J Renin-Angiotensin-Aldosterone Syst. 2020;21:147032032098132.",
"volume": "21",
"year": "2020"
},
{
"article-title": "Renin-angiotensin system blocker and outcomes of COVID-19: a systematic review and meta-analysis,",
"author": "Lee HW",
"journal-title": "Thorax: The Journal of the British Thoracic Society",
"key": "ref12",
"unstructured": "Lee HW, Chang-HwanJang E, JinLee C-H. Renin-angiotensin system blocker and outcomes of COVID-19: a systematic review and meta-analysis, Thorax: The Journal of the British Thoracic Society, vol. 76, 2021.",
"volume": "76",
"year": "2021"
},
{
"article-title": "In-Hospital Use of Statins Is Associated with a Reduced Risk of Mortality among Individuals with COVID-19,",
"author": "Zhang XJ",
"journal-title": "Cell Metabol",
"key": "ref13",
"unstructured": "Zhang XJ, Qin JJ, Cheng X, Shen L, Li H. In-Hospital Use of Statins Is Associated with a Reduced Risk of Mortality among Individuals with COVID-19, Cell Metabol, 2020.",
"year": "2020"
},
{
"DOI": "10.3390/ijms22084177",
"article-title": "COVID-19: direct and indirect mechanisms of statins",
"author": "Pawlos A",
"doi-asserted-by": "crossref",
"first-page": "4177",
"journal-title": "Int J Mol Sci",
"key": "ref14",
"unstructured": "Pawlos A, Niedzielski M, Gorzelak-Pabiś P, Broncel M, Woźniak E. COVID-19: direct and indirect mechanisms of statins. Int J Mol Sci. 2021;22:4177.",
"volume": "22",
"year": "2021"
},
{
"author": "Group TRC",
"key": "ref15",
"unstructured": "Group TRC. \"Aspirin in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial,\" 2022.",
"year": "2022"
},
{
"DOI": "10.1007/s40618-021-01599-0",
"article-title": "Thyroid dysfunction in COVID-19 patients",
"author": "Baldelli R",
"doi-asserted-by": "crossref",
"first-page": "2735",
"journal-title": "J Endocrinol Investig",
"key": "ref16",
"unstructured": "Baldelli R, Nicastri E, Petrosillo N, Marchioni L, Gubbiotti A, Sperduti I, Di Giacinto P, Rizza L, Rota F, Franco M. Thyroid dysfunction in COVID-19 patients. J Endocrinol Investig. 2021;44:2735–9.",
"volume": "44",
"year": "2021"
},
{
"author": "Felsenstein S",
"key": "ref17",
"unstructured": "Felsenstein S, Herbert JA, Mcnamara PS, Hedrich CM. \"COVID-19: Immunology and treatment options,\" Clinical Immunology, vol. 215, p. 108448, 2020.",
"year": "2020"
},
{
"author": "Macchia I",
"first-page": "1170035",
"journal-title": "\"Eosinophils as potential biomarkers in respiratory viral infections \" Front Immunol",
"key": "ref18",
"unstructured": "Macchia I, La Sorsa V, Urbani F, Moretti S, Antonucci C, Afferni C, Schiavoni G. \"Eosinophils as potential biomarkers in respiratory viral infections \" Front Immunol. 2023;14:1170035.",
"volume": "14",
"year": "2023"
},
{
"author": "Dugerdil A",
"key": "ref19",
"unstructured": "Dugerdil A, Semenzato L, Weill A, Zureik M, Flahault A. \"Severe SARS-CoV-2 infection as a marker of undiagnosed cancer: a population-based study,\" Sci Rep, vol. 13, p. 8729, May 30 2023.",
"year": "2023"
},
{
"author": "Dufour I",
"key": "ref20",
"unstructured": "Dufour I, Werion A, Belkhir L, Wisniewska A, Yildiz H. \"Serum uric acid, disease severity and outcomes in COVID-19,\" Critical Care, vol. 25, 2021.",
"year": "2021"
},
{
"author": "Yanai H",
"key": "ref21",
"unstructured": "Yanai H, Adachi H, Hakoshima M, Katsuyama H. Molecular Biological and Clinical Understanding of the Pathophysiology and Treatments of Hyperuricemia and Its Association with Metabolic Syndrome. Cardiovascular Diseases and Chronic Kidney Disease,\"; 2021.",
"volume-title": "Molecular Biological and Clinical Understanding of the Pathophysiology and Treatments of Hyperuricemia and Its Association with Metabolic Syndrome",
"year": "2021"
}
],
"reference-count": 21,
"references-count": 21,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.researchsquare.com/article/rs-3707560/v1"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "Risk of severe case in COVID-19 patients and Azvudine: A Retrospective cohort study after exit from ‘zero-COVID’ policy",
"type": "posted-content"
}