Hepatocellular liver injury in hospitalized patients affected by COVID-19: Presence of different risk factors at different time points
et al., Digestive and Liver Disease, doi:10.1016/j.dld.2021.12.014, May 2022
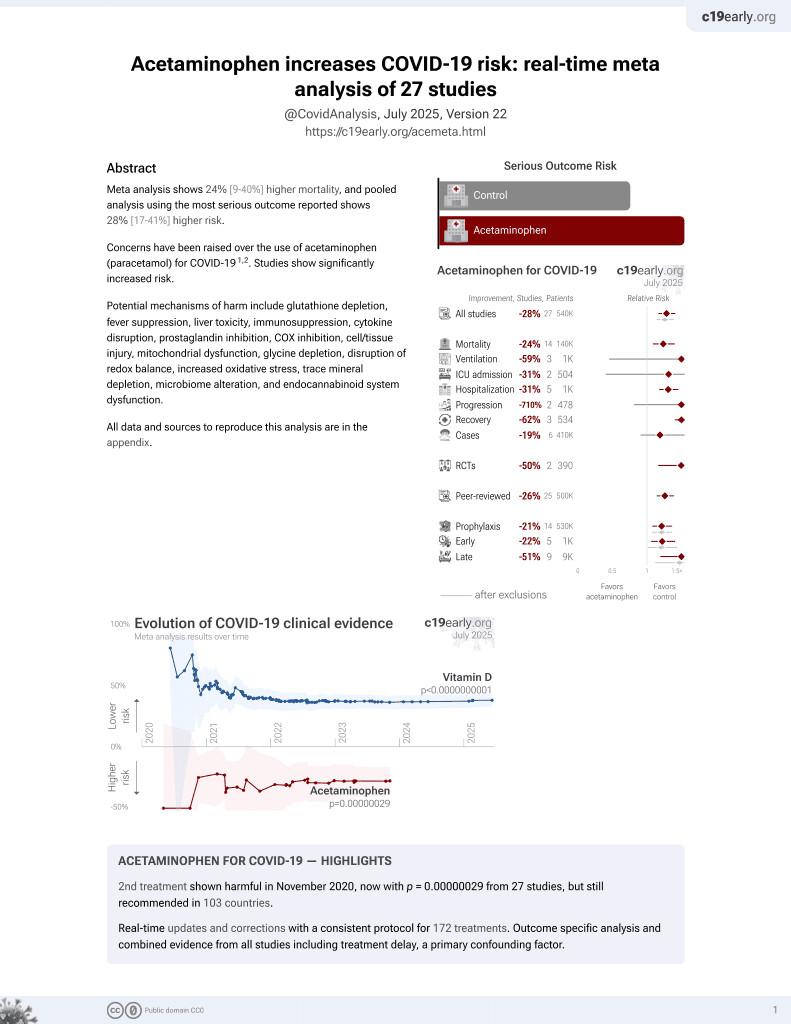
2nd treatment shown to increase risk in
November 2020, now with p = 0.00000029 from 27 studies, but still recommended in 103 countries.
6,400+ studies for
210+ treatments. c19early.org
|
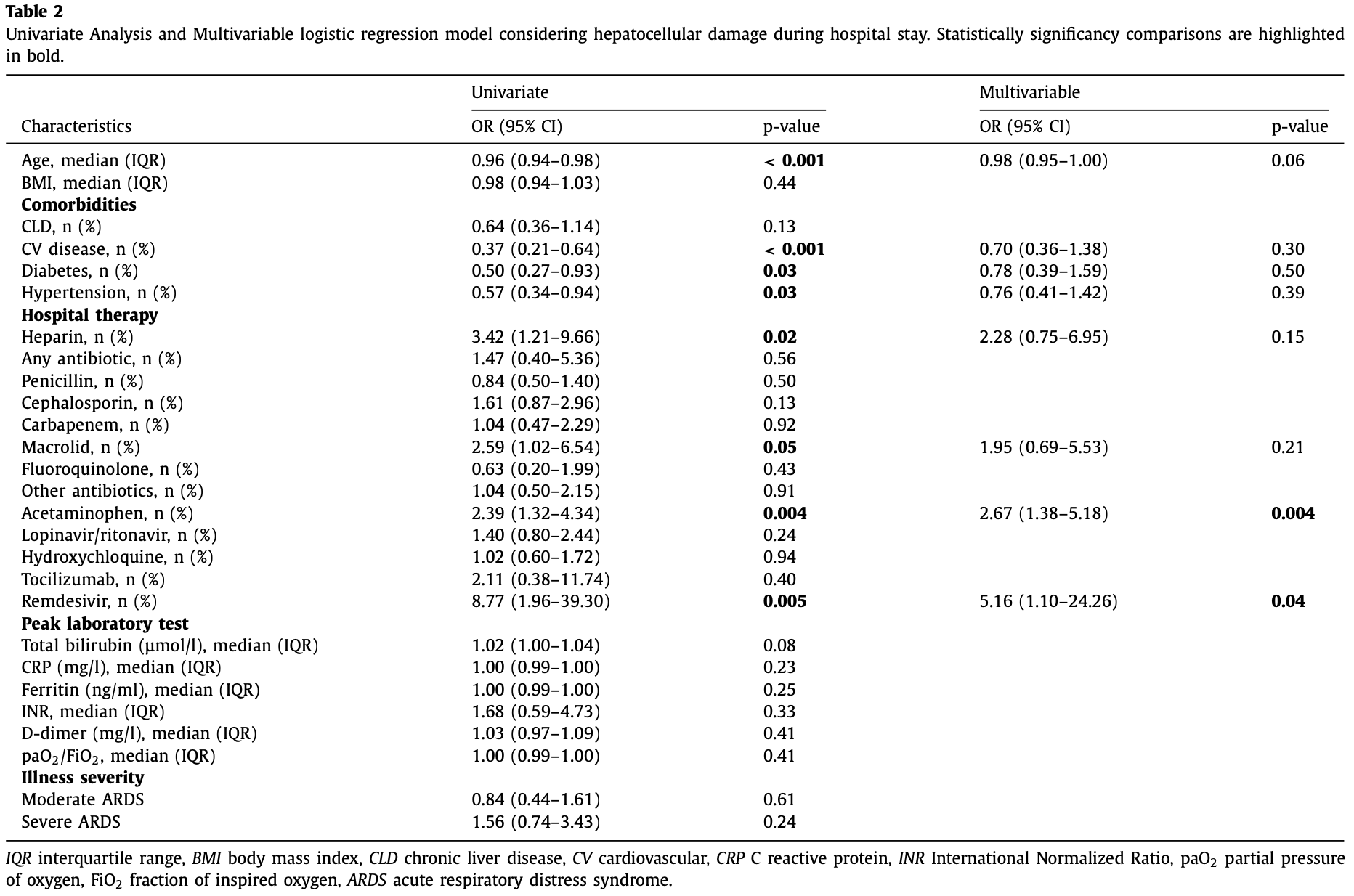
Retrospective 292 patients in Switzerland showing liver damage associated with acetaminophen treatment and remdesivir treatment.
Acetaminophen is also known as paracetamol, Tylenol, Panadol, Calpol, Tempra, Calprofen, Doliprane, Efferalgan, Grippostad C, Dolo, Acamol, Fevadol, Crocin, and Perfalgan.
Study covers acetaminophen and remdesivir.
|
risk of liver damage, 167.0% higher, OR 2.67, p = 0.004, treatment 190, control 102, adjusted per study, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Leo et al., 31 May 2022, retrospective, Switzerland, peer-reviewed, 7 authors.
Contact: massimo.leo@aphp.fr.
Hepatocellular liver injury in hospitalized patients affected by COVID-19: Presence of different risk factors at different time points
Digestive and Liver Disease, doi:10.1016/j.dld.2021.12.014
Background: Prevalence and clinical impact of increased liver function tests in patients affected by Coronavirus disease 2019 (COVID-19) is controversial. Aims: This observational study evaluates the prevalence of transaminases elevation in hospitalized patients affected by COVID-19 and investigates the presence of factors associated with hepatocellular injury and with mortality. Methods: Data of 292 adult patients with confirmed COVID-19 admitted to the Ente Ospedaliero Cantonale (Switzerland) were retrospectively analyzed. Results: Transaminases were increased in about one-third of patients on hospital admission and twothirds of patients during the hospital stay. On hospital admission, transaminases were more commonly elevated in younger patients, who also reported elevated C reactive protein and a higher degree of respiratory failure. Independent factors associated with abnormal transaminases during hospitalization were drugs, in particular paracetamol (OR = 2.67; 95% CI = 1.38-5.18; p = 0.004) and remdesivir (OR = 5.16; 95% CI = 1.10-24.26; p = 0.04). Mortality was independently associated to age (OR = 1.09; 95% CI = 1.05-1.13; p < 0.001), admission to intensive care unit (OR = 5.22; 95% CI = 2.28-11.90; p < 0.001) and alkaline phosphatase peak (OR = 1.01; 95% CI = 1.00-1.01; p = 0.01). Conclusions: On hospital admission, factors associated with liver damage were linked to demographic and clinical characteristics (age, inflammation and hypoxia) while, during hospitalization, drug treatment was related to development and progression of hepatocellular damage. Mortality was associated with alkaline phosphate peak value.
Conflict of Interest Massimo Leo, Antonio Galante, Alberto Pagnamenta, Lorenzo Ruinelli, Francesca Romana Ponziani, Antonio Gasbarrini and Andrea De Gottardi declare that there are no conflicts of interest.
References
Bedogni, Miglioli, Masutti, Prevalence of and risk factors for nonalcoholic fatty liver disease: the Dionysos nutrition and liver study, Hepatology
Bertolini, Van De Peppel, Bodewes, Abnormal liver function tests in patients with COVID-19: relevance and potential pathogenesis, Hepatology
Bloom, Meyerowitz, Reinus, Liver biochemistries in hospitalized patients with COVID-19, Hepatology
Brienza, Revelly, Ayuse, Effects of PEEP on liver arterial and venous blood flows, Am J Respir Crit Care Med
Cai, Huang, Yu, COVID-19: abnormal liver function tests, J Hepatol
Chai, Hu, Zhang, Specific ACE2 expression in cholangiocytes may cause liver damage after 2019-nCoV infection, bioRxiv
Chen, Zhou, Dong, Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study, Lancet
Ding, Li, Chen, Association of liver abnormalities with in-hospital mortality in patients with COVID-19, J Hepatol
Fan, Chen, Li, Clinical features of COVID-19-related liver functional abnormality, Clin Gastroenterol Hepatol
Gordon, Jang, Bouhaddou, A SARS-CoV-2 protein interaction map reveals targets for drug repurposing, Nature
Guan, Ni, Hu, Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med
Hoffmann, Kleine-Weber, Schroeder, SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor, Cell
Huang, Wang, Li, Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China, Lancet
Jenniskens, Langouche, Van Den Berghe, Cholestatic Alterations in the Critically Ill: some New Light on an Old Problem, Chest
Ji, Qin, Xu, Non-alcoholic fatty liver diseases in patients with COVID-19: a retrospective study, J Hepatol
Lei, Liu, Zhou, Longitudinal association between markers of liver injury and mortality in COVID-19 in China, Hepatology
Liu, Wang, Qu, General anatomy report of novel coronavirus pneumonia patients, Journal of Forensic Medicine
Mao, Qiu, He, Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and metaanalysis, Lancet Gastroenterol Hepatol
Massart, Begriche, Moreau, Role of nonalcoholic fatty liver disease as risk factor for drug-induced hepatotoxicity, J Clin Transl Res
Mcdonald, Kubes, Innate immune cell trafficking and function during sterile inflammation of the liver, Gastroenterology
Palomar-Lever, Barraza, Galicia-Alba, Hepatic steatosis as an independent risk factor for severe disease in patients with COVID-19: a computed tomography study, JGH Open
Philips, Ahamed, Augustine, SARS-CoV-2 related liver impairment -perception may not be the reality, J Hepatol
Phipps, Barraza, Lasota, Acute liver injury in COVID-19: prevalence and association with clinical outcomes in a large U.S. cohort, Hepatology
Ponziani, Zompo, Nesci, Liver involvement is not associated with mortality: results from a large cohort of SARS-CoV-2-positive patients, Aliment Pharmacol Ther
Schaefer, Bloom, Interrelationship between coronavirus infection and liver disease, Clin Liver Dis (Hoboken)
Wang, Liu, Liu, SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19, J Hepatol
Weber, Mayerle, Irlbeck, Severe liver failure during SARS-CoV-2 infection, Gut
Wu, Mcgoogan, Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention, JAMA
Xu, Liu, Lu, Liver injury during highly pathogenic human coronavirus infections, Liver Int
Zhang, Shi, Wang, Liver injury in COVID-19: management and challenges, Lancet Gastroenterol Hepatol
Zompo, Siena, Ianiro, Prevalence of liver injury and correlation with clinical outcomes in patients with COVID-19: systematic review with meta-analysis, Eur Rev Med Pharmacol Sci
DOI record:
{
"DOI": "10.1016/j.dld.2021.12.014",
"ISSN": [
"1590-8658"
],
"URL": "http://dx.doi.org/10.1016/j.dld.2021.12.014",
"alternative-id": [
"S1590865821009233"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Hepatocellular liver injury in hospitalized patients affected by COVID-19: Presence of different risk factors at different time points"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Digestive and Liver Disease"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.dld.2021.12.014"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 Published by Elsevier Ltd on behalf of Editrice Gastroenterologica Italiana S.r.l."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-0581-4850",
"affiliation": [],
"authenticated-orcid": false,
"family": "Leo",
"given": "M.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Galante",
"given": "A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pagnamenta",
"given": "A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ruinelli",
"given": "L.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ponziani",
"given": "F.R.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gasbarrini",
"given": "A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "De Gottardi",
"given": "A.",
"sequence": "additional"
}
],
"container-title": "Digestive and Liver Disease",
"container-title-short": "Digestive and Liver Disease",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"dldjournalonline.com",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
12,
27
]
],
"date-time": "2021-12-27T03:32:49Z",
"timestamp": 1640575969000
},
"deposited": {
"date-parts": [
[
2022,
4,
25
]
],
"date-time": "2022-04-25T11:25:29Z",
"timestamp": 1650885929000
},
"indexed": {
"date-parts": [
[
2023,
1,
12
]
],
"date-time": "2023-01-12T07:52:31Z",
"timestamp": 1673509951295
},
"is-referenced-by-count": 3,
"issue": "5",
"issued": {
"date-parts": [
[
2022,
5
]
]
},
"journal-issue": {
"issue": "5",
"published-print": {
"date-parts": [
[
2022,
5
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
5,
1
]
],
"date-time": "2022-05-01T00:00:00Z",
"timestamp": 1651363200000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S1590865821009233?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S1590865821009233?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "565-571",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2022,
5
]
]
},
"published-print": {
"date-parts": [
[
2022,
5
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1056/NEJMoa2002032",
"article-title": "Clinical characteristics of coronavirus disease 2019 in China",
"author": "Guan",
"doi-asserted-by": "crossref",
"first-page": "1708",
"journal-title": "N Engl J Med",
"key": "10.1016/j.dld.2021.12.014_bib0001",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.2648",
"article-title": "Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "1239",
"journal-title": "JAMA",
"key": "10.1016/j.dld.2021.12.014_bib0002",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1016/S2468-1253(20)30126-6",
"article-title": "Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis",
"author": "Mao",
"doi-asserted-by": "crossref",
"first-page": "667",
"journal-title": "Lancet Gastroenterol Hepatol",
"key": "10.1016/j.dld.2021.12.014_bib0003",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/j.jhep.2020.04.006",
"article-title": "COVID-19: abnormal liver function tests",
"author": "Cai",
"doi-asserted-by": "crossref",
"first-page": "566",
"journal-title": "J Hepatol",
"key": "10.1016/j.dld.2021.12.014_bib0004",
"volume": "73",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "China. Lancet.",
"key": "10.1016/j.dld.2021.12.014_bib0005",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1002/hep.31326",
"article-title": "Liver biochemistries in hospitalized patients with COVID-19",
"author": "Bloom",
"doi-asserted-by": "crossref",
"first-page": "890",
"journal-title": "Hepatology",
"key": "10.1016/j.dld.2021.12.014_bib0006",
"volume": "73",
"year": "2020"
},
{
"DOI": "10.1002/hep.31404",
"article-title": "Acute liver injury in COVID-19: prevalence and association with clinical outcomes in a large U.S. cohort",
"author": "Phipps",
"doi-asserted-by": "crossref",
"first-page": "807",
"journal-title": "Hepatology",
"key": "10.1016/j.dld.2021.12.014_bib0007",
"volume": "72",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30211-7",
"article-title": "Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "507",
"journal-title": "Lancet",
"key": "10.1016/j.dld.2021.12.014_bib0008",
"volume": "395",
"year": "2020"
},
{
"article-title": "Prevalence of liver injury and correlation with clinical outcomes in patients with COVID-19: systematic review with meta-analysis",
"author": "Del Zompo",
"first-page": "13072",
"journal-title": "Eur Rev Med Pharmacol Sci",
"key": "10.1016/j.dld.2021.12.014_bib0009",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1136/gutjnl-2020-321350",
"article-title": "Severe liver failure during SARS-CoV-2 infection",
"author": "Weber",
"doi-asserted-by": "crossref",
"first-page": "1365",
"journal-title": "Gut",
"key": "10.1016/j.dld.2021.12.014_bib0010",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1016/S2468-1253(20)30057-1",
"article-title": "Liver injury in COVID-19: management and challenges",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "428",
"journal-title": "Lancet Gastroenterol Hepatol",
"key": "10.1016/j.dld.2021.12.014_bib0011",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1002/cld.967",
"article-title": "Interrelationship between coronavirus infection and liver disease",
"author": "Schaefer",
"doi-asserted-by": "crossref",
"first-page": "175",
"journal-title": "Clin Liver Dis (Hoboken)",
"key": "10.1016/j.dld.2021.12.014_bib0012",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1053/j.gastro.2016.09.048",
"article-title": "Innate immune cell trafficking and function during sterile inflammation of the liver",
"author": "McDonald",
"doi-asserted-by": "crossref",
"first-page": "1087",
"journal-title": "Gastroenterology",
"key": "10.1016/j.dld.2021.12.014_bib0013",
"volume": "151",
"year": "2016"
},
{
"DOI": "10.1111/liv.14435",
"article-title": "Liver injury during highly pathogenic human coronavirus infections",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "998",
"journal-title": "Liver Int",
"key": "10.1016/j.dld.2021.12.014_bib0014",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.1164/ajrccm.152.2.7633699",
"article-title": "Effects of PEEP on liver arterial and venous blood flows",
"author": "Brienza",
"doi-asserted-by": "crossref",
"first-page": "504",
"journal-title": "Am J Respir Crit Care Med",
"key": "10.1016/j.dld.2021.12.014_bib0015",
"volume": "152",
"year": "1995"
},
{
"article-title": "Specific ACE2 expression in cholangiocytes may cause liver damage after 2019-nCoV infection",
"author": "Chai",
"journal-title": "bioRxiv",
"key": "10.1016/j.dld.2021.12.014_bib0016",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"article-title": "SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor",
"author": "Hoffmann",
"doi-asserted-by": "crossref",
"first-page": "271",
"journal-title": "Cell.",
"key": "10.1016/j.dld.2021.12.014_bib0017",
"volume": "181",
"year": "2020"
},
{
"article-title": "General anatomy report of novel coronavirus pneumonia patients",
"author": "Liu",
"first-page": "21",
"journal-title": "Journal of Forensic Medicine",
"key": "10.1016/j.dld.2021.12.014_bib0018",
"volume": "36",
"year": "2020"
},
{
"DOI": "10.1016/j.jhep.2020.05.002",
"article-title": "SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "807",
"journal-title": "J Hepatol",
"key": "10.1016/j.dld.2021.12.014_bib0019",
"volume": "73",
"year": "2020"
},
{
"DOI": "10.1016/j.jhep.2020.05.025",
"article-title": "SARS-CoV-2 related liver impairment - perception may not be the reality",
"author": "Philips",
"doi-asserted-by": "crossref",
"first-page": "991",
"journal-title": "J Hepatol",
"key": "10.1016/j.dld.2021.12.014_bib0020",
"volume": "73",
"year": "2020"
},
{
"DOI": "10.1016/j.cgh.2020.04.002",
"article-title": "Clinical features of COVID-19-related liver functional abnormality",
"author": "Fan",
"doi-asserted-by": "crossref",
"first-page": "1561",
"journal-title": "Clin Gastroenterol Hepatol",
"key": "10.1016/j.dld.2021.12.014_bib0021",
"volume": "18",
"year": "2020"
},
{
"article-title": "Liver involvement is not associated with mortality: results from a large cohort of SARS-CoV-2-positive patients",
"author": "Ponziani",
"first-page": "1060",
"journal-title": "Aliment Pharmacol Ther",
"key": "10.1016/j.dld.2021.12.014_bib0022",
"volume": "52",
"year": "2020"
},
{
"DOI": "10.1016/j.jhep.2020.12.012",
"article-title": "Association of liver abnormalities with in-hospital mortality in patients with COVID-19",
"author": "Ding",
"doi-asserted-by": "crossref",
"first-page": "1295",
"journal-title": "J Hepatol",
"key": "10.1016/j.dld.2021.12.014_bib0023",
"volume": "74",
"year": "2021"
},
{
"key": "10.1016/j.dld.2021.12.014_bib0024",
"unstructured": "National Institutes of Health, National Cancer Institute, U.S. Department of Health and Human Services. Common Terminology Criteria for Adverse Events (CTCAE) version 5.0. https://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_8.5x11.pdf. Published November 27, 2017."
},
{
"DOI": "10.1038/s41586-020-2286-9",
"article-title": "A SARS-CoV-2 protein interaction map reveals targets for drug repurposing",
"author": "Gordon",
"doi-asserted-by": "crossref",
"first-page": "459",
"journal-title": "Nature",
"key": "10.1016/j.dld.2021.12.014_bib0025",
"volume": "583",
"year": "2020"
},
{
"DOI": "10.1002/hep.31301",
"article-title": "Longitudinal association between markers of liver injury and mortality in COVID-19 in China",
"author": "Lei",
"doi-asserted-by": "crossref",
"first-page": "389",
"journal-title": "Hepatology",
"key": "10.1016/j.dld.2021.12.014_bib0026",
"volume": "72",
"year": "2020"
},
{
"DOI": "10.1016/j.jhep.2020.03.044",
"article-title": "Non-alcoholic fatty liver diseases in patients with COVID-19: a retrospective study",
"author": "Ji",
"doi-asserted-by": "crossref",
"first-page": "451",
"journal-title": "J Hepatol",
"key": "10.1016/j.dld.2021.12.014_bib0027",
"volume": "73",
"year": "2020"
},
{
"DOI": "10.1002/jgh3.12395",
"article-title": "Hepatic steatosis as an independent risk factor for severe disease in patients with COVID-19: a computed tomography study",
"author": "Palomar-Lever",
"doi-asserted-by": "crossref",
"first-page": "1102",
"journal-title": "JGH Open",
"key": "10.1016/j.dld.2021.12.014_bib0028",
"volume": "4",
"year": "2020"
},
{
"DOI": "10.1002/hep.20734",
"article-title": "Prevalence of and risk factors for nonalcoholic fatty liver disease: the Dionysos nutrition and liver study",
"author": "Bedogni",
"doi-asserted-by": "crossref",
"first-page": "44",
"journal-title": "Hepatology",
"key": "10.1016/j.dld.2021.12.014_bib0029",
"volume": "42",
"year": "2005"
},
{
"article-title": "Role of nonalcoholic fatty liver disease as risk factor for drug-induced hepatotoxicity",
"author": "Massart",
"first-page": "212",
"journal-title": "J Clin Transl Res",
"key": "10.1016/j.dld.2021.12.014_bib0030",
"volume": "3",
"year": "2017"
},
{
"DOI": "10.1016/j.chest.2017.08.018",
"article-title": "Cholestatic Alterations in the Critically Ill: some New Light on an Old Problem",
"author": "Jenniskens",
"doi-asserted-by": "crossref",
"first-page": "733",
"journal-title": "Chest",
"key": "10.1016/j.dld.2021.12.014_bib0031",
"volume": "153",
"year": "2018"
},
{
"DOI": "10.1002/hep.31480",
"article-title": "Abnormal liver function tests in patients with COVID-19: relevance and potential pathogenesis",
"author": "Bertolini",
"doi-asserted-by": "crossref",
"first-page": "1864",
"journal-title": "Hepatology",
"key": "10.1016/j.dld.2021.12.014_bib0032",
"volume": "72",
"year": "2020"
}
],
"reference-count": 32,
"references-count": 32,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S1590865821009233"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Gastroenterology",
"Hepatology"
],
"subtitle": [],
"title": "Hepatocellular liver injury in hospitalized patients affected by COVID-19: Presence of different risk factors at different time points",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "54"
}