Evaluating the Effects of Clinical Characteristics and Therapeutic Regimens on Mortality in Hospitalized Patients with Severe COVID-19
et al., Journal of Pharmaceutical Care, doi:10.18502/jpc.v10i3.10790, Oct 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 478 moderate to severe hospitalized patients in Iran, showing lower mortality with vitamin D treatment.
This is the 103rd of 136 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
40 studies are RCTs, which show efficacy with p=0.0000001.
Study covers aspirin and vitamin D.
|
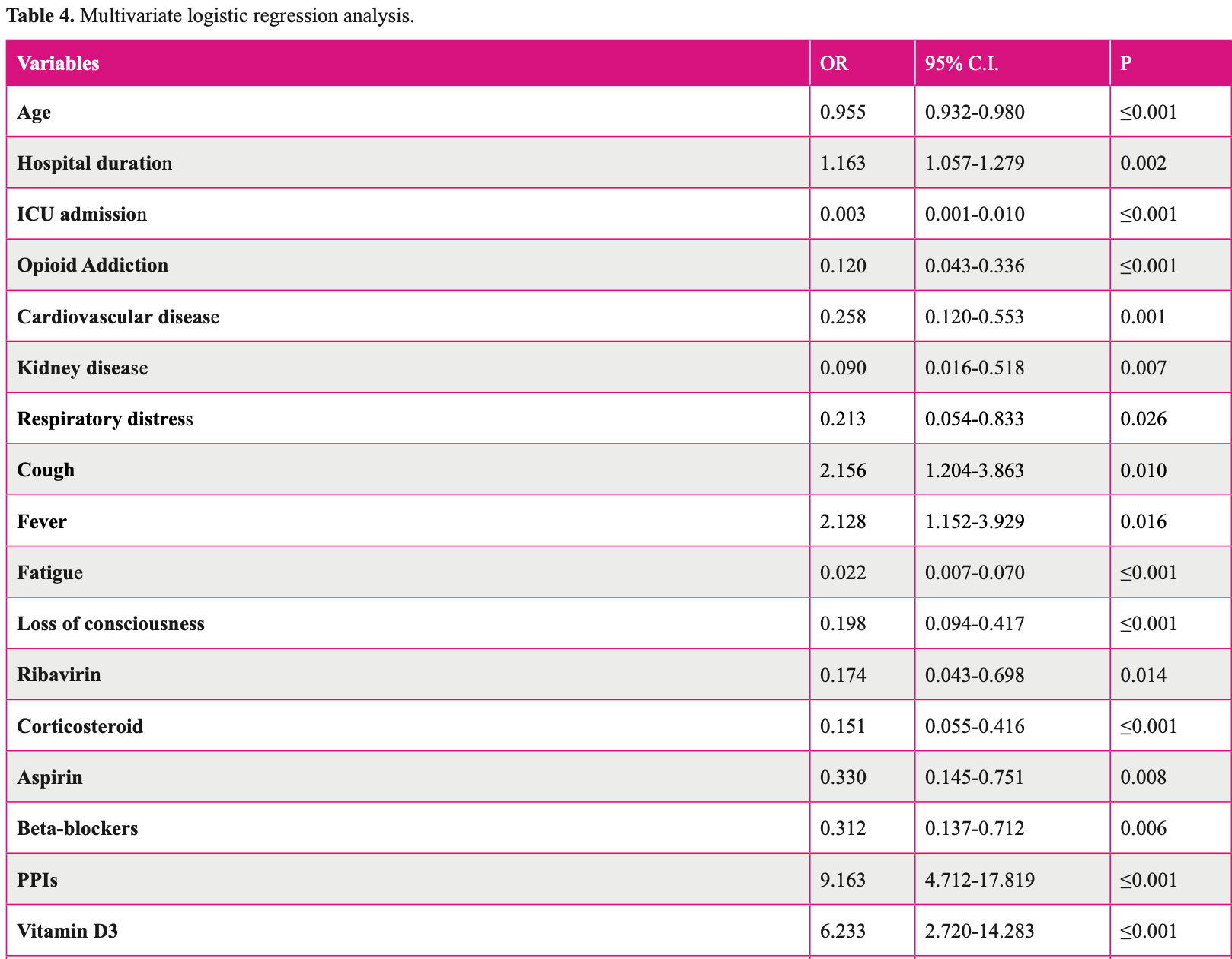
risk of death, 79.0% lower, RR 0.21, p < 0.001, treatment 10 of 124 (8.1%), control 93 of 329 (28.3%), NNT 4.9, adjusted per study, inverted to make RR<1 favor treatment, odds ratio converted to relative risk, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Karimpour-Razkenari et al., 3 Oct 2022, retrospective, Iran, peer-reviewed, median age 58.5, 9 authors, study period 23 February, 2020 - 23 May, 2020, dosage not specified.
Contact: ghazaeianm@gmail.com.
Evaluating the Effects of Clinical Characteristics and Therapeutic Regimens on Mortality in Hospitalized Patients with Severe COVID-19
The coronavirus disease 2019 (COVID-19) is highly contagious and has turned into a global health problem. In this study, we investigated the role of clinical and laboratory characteristics along with administered therapeutic agents in patients with COVID-19, and identified some effective factors on the mortality of these individuals.
Methods: In this retrospective study, we evaluated the data from all the hospitalized patients who had been diagnosed with COVID-19 between February 23 and May 23, 2020. The data were obtained from medical records. Additionally, a checklist was used to record demographic, clinical, laboratory, imaging, and treatment data for each patient. Results: Totally, 478 patients were involved in this study, and their median age was 58.5 years. Of these, 53.3% patients were male. The most common pre-existing underlying disease was hypertension (37.9%), and the mortality group had significantly more comorbidities (85.4%). Higher neutrophil lymphocyte ratio (NLR), lymphopenia, and reduced hemoglobin were more frequent in the mortality group (p < 0.001). Similarly, the need to be admitted to the intensive care unit was significantly greater in the mortality group (p<0.001). The most frequently administered therapeutic regimens included hydroxychloroquine and lopinavir/ritonavir, which did not have any correlation with survival outcome.
Conclusion: Older age, opioid addiction, cardiovascular disease, kidney disease, baseline NLR and hemoglobin, and ICU admission were independently associated with COVID-19 mortality. On the other hand, hydroxychloroquine and lopinavir/ritonavir indicated no beneficial effects on patients' outcome.
September 2022;10(3)
Evaluating the Effects of Clinical Characteristics and Therapeutic Regimens
References
Adham, Habibzadeh, Ghobadi, Abbasi-Ghahramanloo, Moradi-Asl, Epidemiological Characteristics and Mortality Risk Factors among COVID-19 Patients in Ardabil, Northwest of Iran, BMC Emerg Med
Amrein, Schnedl, Holl, Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial, JAMA
Anai, Akaike, Iwagoe, Decrease in hemoglobin level predicts increased risk for severe respiratory failure in COVID-19 patients with pneumonia, Respir Investig
Burton, Fort, Seoane, Hospitalization and mortality among black patients and white patients with Covid-19, New Engl J Med
Carpagnano, Lecce, Quaranta, Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19, J Endocrinol Invest
Cfd, Prevention, Coronavirus disease
Cfd, Prevention, Coronavirus disease 2019 (COVID-19): people who are at increased risk for severe illness
Cfd, Prevention, Health equity considerations and racial and ethnic minority groups
Chen, Zhou, Dong, Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study, Lancet
Dubey, Ghosh, Chatterjee, Biswas, Chatterjee et al., COVID-19 and addiction, Diabetes Metab Syndr
Estebanez, Ramirez-Olivencia, Mata, Clinical evaluation of IFN beta1b in COVID-19 pneumonia: a retrospective study
Huang, Pranata, Lim, Oehadian, Alisjahbana, C-reactive protein, procalcitonin, D-dimer, and ferritin in severe coronavirus disease-2019: a meta-analysis, Ther Adv Respir Dis
Khwaja, KDIGO clinical practice guidelines for acute kidney injury, Nephron Clin Pract
Lescot, Karvellas, Beaussier, Magder, Riou, Acquired liver injury in the intensive care unit, Anesthesiology
Mao, Wang, Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China, JAMA Neurol
Mardani, Vasmehjani, Zali, Laboratory parameters in detection of COVID-19 patients with positive RT-PCR; a diagnostic accuracy study, Arch Acad Emerg Med
Mcmichael, Clark, Pogosjans, COVID-19 in a long-term care facility-King County, Washington, MMWR Morb Mortal Wkly Rep
Mirjalili, Dastgheib, Shaker, Proportion and mortality of Iranian diabetes mellitus, chronic kidney disease, hypertension and cardiovascular disease patients with COVID-19: a meta-analysis, J Diabetes Metab Disord
Onder, Rezza, Brusaferro, Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy, JAMA
Organization, Anaemia -WHO | World Health Organization
Palaiodimos, Kokkinidis, Li, Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, Metabolism
Rahmani, Davoudi-Monfared, Nourian, Comparing outcomes of hospitalized patients with moderate and severe COVID-19 following treatment with hydroxychloroquine plus atazanavir/ritonavir, DARU
Ren, Wang, Wu, Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study, Chin Med J (Engl)
Rouhani, Karimpour-Razkenari, Forutan, Ghazaeian, Salehifar et al., Efficacy and Safety of Interferon Beta-1b in the Management of Patients with COVID-19: A Prospective, Open-Label, Non-Randomized Trial, J Pharm Care
Sobhani, Aryan, Kalantari, Soltani, Malek et al., Association between Clinical Characteristics and Laboratory Findings with Outcome of Hospitalized COVID-19 Patients: A Report from Northeast Iran, I Interdiscip Perspect Infect Dis
Stokes, Zambrano, Anderson, Coronavirus disease 2019 case surveillance-United States, MMWR Morb Mortal Wkly Rep
Taneri, Gómez-Ochoa, Llanaj, Anemia and iron metabolism in COVID-19: a systematic review and meta-analysis, Europ J Epidemiol
Terpos, Ntanasis-Stathopoulos, Elalamy, Hematological findings and complications of COVID-19, Am J Hematol
Wj, Zy, Hu, Clinical characteristics of coronavirus disease 2019 in China, New Engl J Med
Wu, Mcgoogan, Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention, JAMA
DOI record:
{
"DOI": "10.18502/jpc.v10i3.10790",
"ISSN": [
"2322-4509",
"2322-4630"
],
"URL": "http://dx.doi.org/10.18502/jpc.v10i3.10790",
"abstract": "<jats:p>Background: The coronavirus disease 2019 (COVID-19) is highly contagious and has turned into a global health problem. In this study, we investigated the role of clinical and laboratory characteristics along with administered therapeutic agents in patients with COVID-19, and identified some effective factors on the mortality of these individuals.
\nMethods: In this retrospective study, we evaluated the data from all the hospitalized patients who had been diagnosed with COVID-19 between February 23 and May 23, 2020. The data were obtained from medical records. Additionally, a checklist was used to record demographic, clinical, laboratory, imaging, and treatment data for each patient.
\nResults: Totally, 478 patients were involved in this study, and their median age was 58.5 years. Of these, 53.3% patients were male. The most common pre-existing underlying disease was hypertension (37.9%), and the mortality group had significantly more comorbidities (85.4%). Higher neutrophil lymphocyte ratio (NLR), lymphopenia, and reduced hemoglobin were more frequent in the mortality group (p < 0.001). Similarly, the need to be admitted to the intensive care unit was significantly greater in the mortality group (p<0.001). The most frequently administered therapeutic regimens included hydroxychloroquine and lopinavir/ritonavir, which did not have any correlation with survival outcome.
\nConclusion: Older age, opioid addiction, cardiovascular disease, kidney disease, baseline NLR and hemoglobin, and ICU admission were independently associated with COVID-19 mortality. On the other hand, hydroxychloroquine and lopinavir/ritonavir indicated no beneficial effects on patients’ outcome.</jats:p>",
"author": [
{
"affiliation": [],
"family": "Karimpour-razkenari",
"given": "Elahe",
"sequence": "first"
},
{
"affiliation": [],
"family": "Boskabadi",
"given": "Javad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ghazaeian",
"given": "Monireh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Samaee",
"given": "Hamidreza",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Azizi",
"given": "Hanieh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Esfandiari",
"given": "Fatemeh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mousavi",
"given": "Seyed Abdollah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fallah",
"given": "Sahar",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Talebi",
"given": "Sekineh",
"sequence": "additional"
}
],
"container-title": "Journal of Pharmaceutical Care",
"container-title-short": "jpc",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
10,
8
]
],
"date-time": "2022-10-08T08:19:24Z",
"timestamp": 1665217164000
},
"deposited": {
"date-parts": [
[
2022,
10,
8
]
],
"date-time": "2022-10-08T08:19:38Z",
"timestamp": 1665217178000
},
"indexed": {
"date-parts": [
[
2022,
10,
8
]
],
"date-time": "2022-10-08T08:45:10Z",
"timestamp": 1665218710832
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
10,
3
]
]
},
"member": "7770",
"original-title": [],
"prefix": "10.18502",
"published": {
"date-parts": [
[
2022,
10,
3
]
]
},
"published-online": {
"date-parts": [
[
2022,
10,
3
]
]
},
"publisher": "Knowledge E DMCC",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://publish.kne-publishing.com/index.php/JPC/article/view/10790"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Earth and Planetary Sciences",
"Water Science and Technology",
"Geography, Planning and Development"
],
"subtitle": [],
"title": "Evaluating the Effects of Clinical Characteristics and Therapeutic Regimens on Mortality in Hospitalized Patients with Severe COVID-19",
"type": "journal-article"
}
