Zinc Levels of Patients With A Moderate to Severe COVID-19 Infection at Hospital Admission and After 4th Days of Ward Hospitalization and Their Clinical Outcome
et al., Journal of Trace Elements in Medicine and Biology, doi:10.1016/j.jtemb.2023.127200, May 2023
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000028 from 47 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
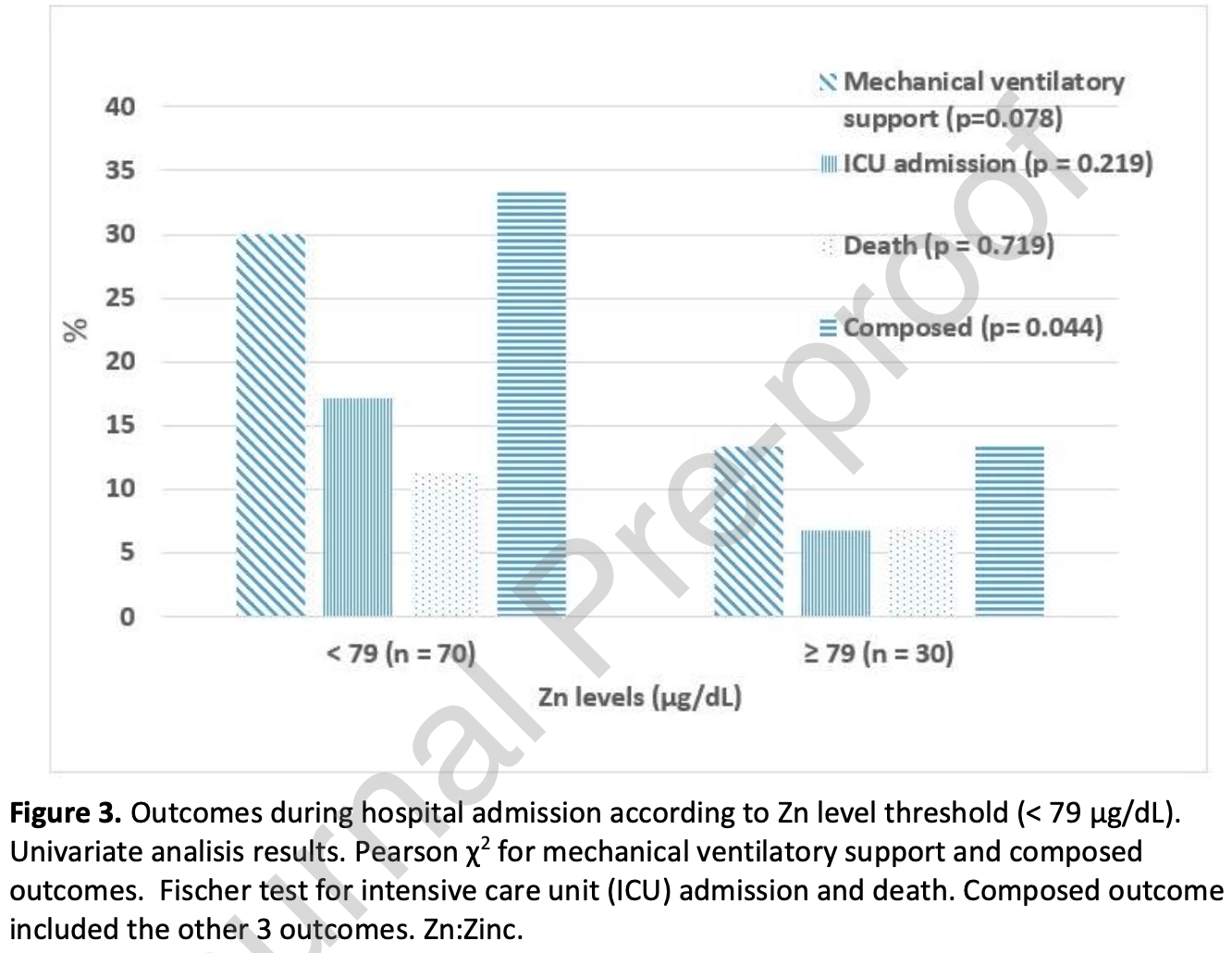
Prospective analysis of 100 hospitalized COVID-19 patients in Spain, showing higher risk of death/mechanical ventilation/ICU admission with zinc levels <79µg/dL, without statistical significance.
|
risk of death/mechanical ventilation/ICU admission, 54.6% lower, OR 0.45, p = 0.21, high zinc levels (≥79µg/dL) 30, low zinc levels (<79µg/dL) 70, adjusted per study, inverted to make OR<1 favor high zinc levels (≥79µg/dL), RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Jiménez et al., 13 May 2023, prospective, Spain, peer-reviewed, 8 authors, study period 4 September, 2020 - 24 April, 2021.
Contact: arturocorbaton@yahoo.es.
Zinc levels of patients with a moderate to severe COVID-19 infection at hospital admission and after 4th days of ward hospitalization and their clinical outcome
Journal of Trace Elements in Medicine and Biology, doi:10.1016/j.jtemb.2023.127200
This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Authors' Contributions LRJ and ACA are responsible for conceiving and designing the study as well as data interpretation and preparation of the draft of the manuscript. ACA, LRJ, PMS, RPM and MGM participated actively in the development of the field study. MFF extracted the data and take responsibility together with LRJ and ACA for the integrity of the analyses. MMG and ISF participated in the design and development of the field studies. MMG participated in the critical revision and gave final approval of the manuscript to be published.
Declaration of Competing Interest The authors declare no conflict of interest.
Authorship contributions
References
Adhikari, Meng, Wu, Mao, Ye et al., Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review, Infect Dis Poverty, doi:10.1186/s40249-020-00646-x
Arnaud, Touvier, Galan, Andriollo-Sanchez, Ruffieux, Determinants of serum zinc concentrations in a population of French middle-age subjects (SU.VI.MAX cohort), European Journal of Clinical Nutrition, doi:10.1038/ejcn.2010.118.hal-00560303
Bego, Meseldžić, Prnjavora, Prnjavorac, Marjanović et al., Association of Trace Element Status in COVID-19 Patients with Disease Severity, J Trace Elem Med Biol
Besecker, Exline, Hollyfield, A comparison of zinc metabolism, inflammation, and disease severity in critically ill infected and noninfected adults early after intensive care unit admission, Am J Clin Nutr
Besecker, Exline, Hollyfield, Phillips, Disilvestro et al., A comparison of zinc metabolism, inflammation, and disease severity in critically ill infected and noninfected adults early after intensive care unit admission, Am J Clin Nutr, doi:10.3945/ajcn.110.008417
Boretti, Banik, Zinc role in Covid-19 disease and prevention, Vacunas
Cvijanovich, King, Hr, Gildengorin, Wong, Zinc homeostasis in pediatric critical illness, Pediatr Crit Care Med, doi:10.1097/PCC.0b013e31819371ce
De, Silleras, García, Miján De La, The zinc status in a selected Spanish population. A multivariate analysis, Nutr Hosp
Dubourg, Lagier, Brouqui, Casalta, Jacomo et al., Low blood zinc concentrations in patients with poor clinical outcome during SARS-CoV-2 infection: is there a need to supplement with zinc COVID-19 patients?, J Microbiol Immunol Infect, doi:10.1016/j.jmii.2021.01.012
Duncan, Talwar, Mcmillan, Quantitative data on the magnitude of the systemic inflammatory response and its effect on micronutrient status based on plasma measurements, Am J Clin Nutr
Florea, Molina-López, Hogstrand, Lengyel, De La Cruz et al., Changes in zinc status and zinc transporters expression in whole blood of patients with Systemic Inflammatory Response Syndrome (SIRS), J Trace Elements in Medicine and Biology
Fromonot, Gette, Lassoued, Guéant, Rosa-Maria Guéant-Rodriguez 3, Régis Guieu. Hypozincemia in the early stage of COVID-19 is associated with an increased risk of severe COVID-19, Clin Nutr
Gammoh, Rink, Zinc in Infection and Inflammation, Nutrients, doi:10.3390/nu9060624
Golin, Tinkov, Aschner, Farina, Da Rocha, Relationship between selenium status, selenoproteins and COVID-19 and other inflammatory diseases: A critical review, J Trace Elem Med Biol, doi:10.1016/j.jtemb.2022.127099
Heyland, Jones, Cvijanovich, Wong, Zinc supplementation in critically ill patients: a key pharmaconutrient?, JPEN J Parenter Enteral Nutr, doi:10.1177/0148607108322402
Hotz, Peerson, Brown, Suggested lower cutoffs of serum zinc concentrations for assessing zinc status: Reanalysis of the second National Health and Nutrition Examination Survey data (1976-1980, Am J Clin Nutr
Ivanova, Pal, Simonelli, Atanasova, Ventriglia et al., Evaluation of zinc, copper, and Cu:Zn ratio in serum, and their implications in the course of COVID-19, J Trace Elem Med Biol, doi:10.1016/j.jtemb.2022.126944
Jahromi, Tabriz, Togha, Ariyanfar, Ghorbani et al., The correlation between serum selenium, zinc, and COVID-19 severity: an observational study, BMC Infect Dis, doi:10.1186/s12879-021-06617-3
Kdigo Ckd, Group, Dueñas Ricaurte, Araque, Varela, KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease, Nutrición Clínica
Keen, Gershwin, Zinc deficiency and immune function, Annu Rev Nutr
Kong, Jung, Yu, Park, Kang, Association Between Cardiovascular Risk Factors and the Severity of Coronavirus Disease 2019: Nationwide Epidemiological Study in Korea
Linko, Karlsson, Pettila, Serum zinc in critically ill adult patients with acute respiratory failure, Acta Anaesthesiol Scand
Linko, Karlsson, Pettilä, Varpula, Okkonen et al., Serum zinc in critically ill adult patients with acute respiratory failure, Acta Anaesthesiol Scand, doi:10.1111/j.1399-6576.2011.02425.x
Lowe, Fekete, Decsi, Methods of assessment of zinc status in humans: a systematic review, Am J Clin Nutr
Maares, Haase, Zinc and immunity: An essential interrelation, Archives of Biochemistry and Biophysics
Manzanares, Langlois, Hardy, Update on antioxidant micronutrients in the critically ill, Curr Opin Clin Nutr Metab Care, doi:10.1097/MCO.0
Matsushita, Ding, Kou, Hu, Gao, The Relationship of COVID-19 Severity with Cardiovascular Disease and Its Traditional Risk Factors: A Systematic Review and Meta-Analysis, Global Heart
Mayor-Ibarguren, Busca-Arenzana, Robles-Marhuenda, A Hypothesis for the Possible Role of Zinc in the Immunological Pathways Related to COVID-19 Infection, Front. Immunol
Olechnowicz, Tinkov, Skalny, Suliburska, Zinc status is associated with inflammation, oxidative stress, lipid, and glucose metabolism, J Physiol Sci
Prasad, Impact of the discovery of human zinc deficiency on health, J Am Coll Nutr, doi:10.1080/07315724.2009.10719780
Read, Obeid, Ahlenstiel, Ahlenstiel, The Role of Zinc in Antiviral Immunity, Adv Nutr, doi:10.1093/advances/nmz013
Roohani, Hurrell, Kelishadi, Schulin, Zinc and its importance for human health: An integrative review, J Res Med Sci
Velthuis, Van Den Worm, Sims, Baric, Snijder et al., +) inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture, PLoS Pathog, doi:10.1371/journal.ppat.1001176
Vogel-González, Talló-Parra, Herrera-Fernández, Pérez-Vilaró, Chillón et al., Low Zinc Levels at Admission Associates with Poor Clinical Outcomes in SARS-CoV-2 Infection, Nutrients
Wessells, Brown, Estimating the global prevalence of zinc deficiency: results based zinc availability in national food supplies and the prevalence of stunting, PLoS One, doi:10.1371/journal.pone.0050568
Wessels, Maywald, Rink, Zinc as a Gatekeeper of Immune Function, Nutrients, doi:10.3390/nu9121286
Wessels, Rolles, Rink, The Potential Impact of Zinc Supplementation on COVID-19, Pathogenesis. Front. Immunol, doi:10.3389/fimmu.2020.01712
Xu, Liang, Shi, Zhang, Wang, A meta-analysis on the risk factors adjusted association between cardiovascular disease and COVID-19 severity, BMC Public Health
Yasuda, Tsutsui, Infants and elderlies are susceptible to zinc deficiency, Sci Rep
DOI record:
{
"DOI": "10.1016/j.jtemb.2023.127200",
"ISSN": [
"0946-672X"
],
"URL": "http://dx.doi.org/10.1016/j.jtemb.2023.127200",
"alternative-id": [
"S0946672X23000767"
],
"article-number": "127200",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Zinc Levels of Patients With A Moderate to Severe COVID-19 Infection at Hospital Admission and After 4th Days of Ward Hospitalization and Their Clinical Outcome"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Journal of Trace Elements in Medicine and Biology"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.jtemb.2023.127200"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2023 Published by Elsevier GmbH."
}
],
"author": [
{
"affiliation": [],
"family": "Jiménez",
"given": "Laura Rodelgo",
"sequence": "first"
},
{
"affiliation": [],
"family": "Anchuelo",
"given": "Arturo Corbatón",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Soler",
"given": "Pablo Matías",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Muñoz",
"given": "Raúl Perales",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ferrer",
"given": "Manuel Fuentes",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fornie",
"given": "Iñigo Sagastagoitia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mosquera",
"given": "Marina Gil",
"sequence": "additional"
},
{
"affiliation": [],
"family": "González",
"given": "Mercedes Martínez-Novillo",
"sequence": "additional"
}
],
"container-title": "Journal of Trace Elements in Medicine and Biology",
"container-title-short": "Journal of Trace Elements in Medicine and Biology",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2023,
5,
13
]
],
"date-time": "2023-05-13T06:11:08Z",
"timestamp": 1683958268000
},
"deposited": {
"date-parts": [
[
2023,
5,
13
]
],
"date-time": "2023-05-13T06:11:46Z",
"timestamp": 1683958306000
},
"indexed": {
"date-parts": [
[
2023,
5,
14
]
],
"date-time": "2023-05-14T04:15:44Z",
"timestamp": 1684037744643
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
5
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
5,
1
]
],
"date-time": "2023-05-01T00:00:00Z",
"timestamp": 1682899200000
}
},
{
"URL": "https://doi.org/10.15223/policy-017",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
5,
1
]
],
"date-time": "2023-05-01T00:00:00Z",
"timestamp": 1682899200000
}
},
{
"URL": "https://doi.org/10.15223/policy-037",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
5,
1
]
],
"date-time": "2023-05-01T00:00:00Z",
"timestamp": 1682899200000
}
},
{
"URL": "https://doi.org/10.15223/policy-012",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
5,
1
]
],
"date-time": "2023-05-01T00:00:00Z",
"timestamp": 1682899200000
}
},
{
"URL": "https://doi.org/10.15223/policy-029",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
5,
1
]
],
"date-time": "2023-05-01T00:00:00Z",
"timestamp": 1682899200000
}
},
{
"URL": "https://doi.org/10.15223/policy-004",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
5,
1
]
],
"date-time": "2023-05-01T00:00:00Z",
"timestamp": 1682899200000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0946672X23000767?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0946672X23000767?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "127200",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2023,
5
]
]
},
"published-print": {
"date-parts": [
[
2023,
5
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.5334/gh.814",
"article-title": "The Relationship of COVID-19 Severity with Cardiovascular Disease and Its Traditional Risk Factors: A Systematic Review and Meta-Analysis",
"author": "Matsushita",
"doi-asserted-by": "crossref",
"first-page": "64",
"issue": "1",
"journal-title": "Global Heart.",
"key": "10.1016/j.jtemb.2023.127200_bib1",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1186/s12889-021-11051-w",
"article-title": "A meta-analysis on the risk factors adjusted association between cardiovascular disease and COVID-19 severity",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "1533",
"journal-title": "BMC Public Health",
"key": "10.1016/j.jtemb.2023.127200_bib2",
"volume": "21",
"year": "2021"
},
{
"author": "Kong",
"journal-title": "Association Between Cardiovascular Risk Factors and the Severity of Coronavirus Disease 2019: Nationwide Epidemiological Study in Korea",
"key": "10.1016/j.jtemb.2023.127200_bib3",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1016/j.abb.2016.03.022",
"article-title": "Zinc and immunity: An essential interrelation",
"author": "Maares",
"doi-asserted-by": "crossref",
"first-page": "58",
"journal-title": "Archives of Biochemistry and Biophysics",
"key": "10.1016/j.jtemb.2023.127200_bib4",
"volume": "611",
"year": "2016"
},
{
"DOI": "10.3390/nu9121286",
"article-title": "Zinc as a Gatekeeper of Immune Function",
"author": "Wessels",
"doi-asserted-by": "crossref",
"first-page": "1286",
"issue": "12",
"journal-title": "Nutrients.",
"key": "10.1016/j.jtemb.2023.127200_bib5",
"volume": "9",
"year": "2017"
},
{
"DOI": "10.3390/nu9060624",
"article-title": "Zinc in Infection and Inflammation",
"author": "Gammoh",
"doi-asserted-by": "crossref",
"first-page": "624",
"issue": "6",
"journal-title": "Nutrients.",
"key": "10.1016/j.jtemb.2023.127200_bib6",
"volume": "9",
"year": "2017"
},
{
"article-title": "Zinc and its importance for human health: An integrative review",
"author": "Roohani",
"first-page": "144",
"issue": "2",
"journal-title": "J Res Med Sci.",
"key": "10.1016/j.jtemb.2023.127200_bib7",
"volume": "18",
"year": "2013"
},
{
"DOI": "10.1080/07315724.2009.10719780",
"article-title": "Impact of the discovery of human zinc deficiency on health",
"author": "Prasad",
"doi-asserted-by": "crossref",
"first-page": "257",
"issue": "3",
"journal-title": "J Am Coll Nutr",
"key": "10.1016/j.jtemb.2023.127200_bib8",
"volume": "28",
"year": "2009"
},
{
"DOI": "10.1371/journal.pone.0050568",
"article-title": "Estimating the global prevalence of zinc deficiency: results based on zinc availability in national food supplies and the prevalence of stunting",
"author": "Wessells",
"doi-asserted-by": "crossref",
"issue": "11",
"journal-title": "PLoS One.",
"key": "10.1016/j.jtemb.2023.127200_bib9",
"volume": "7",
"year": "2012"
},
{
"article-title": "The zinc status in a selected Spanish population. A multivariate analysis",
"author": "de Mateo Silleras 1",
"first-page": "32",
"issue": "1",
"journal-title": "Nutr Hosp",
"key": "10.1016/j.jtemb.2023.127200_bib10",
"volume": "15",
"year": "2000"
},
{
"DOI": "10.1093/ajcn/78.4.756",
"article-title": "Suggested lower cutoffs of serum zinc concentrations for assessing zinc status: Reanalysis of the second National Health and Nutrition Examination Survey data (1976-1980)",
"author": "Hotz",
"doi-asserted-by": "crossref",
"first-page": "756",
"journal-title": "Am J Clin Nutr",
"key": "10.1016/j.jtemb.2023.127200_bib11",
"volume": "78",
"year": "2003"
},
{
"DOI": "10.1097/MCO.0b013e32836599e5",
"article-title": "Update on antioxidant micronutrients in the critically ill",
"author": "Manzanares",
"doi-asserted-by": "crossref",
"first-page": "719",
"issue": "6",
"journal-title": "Curr Opin Clin Nutr Metab Care",
"key": "10.1016/j.jtemb.2023.127200_bib12",
"volume": "16",
"year": "2013"
},
{
"DOI": "10.3389/fimmu.2020.01712",
"article-title": "The Potential Impact of Zinc Supplementation on COVID-19 Pathogenesis",
"author": "Wessels",
"doi-asserted-by": "crossref",
"first-page": "1712",
"journal-title": "Front. Immunol.",
"key": "10.1016/j.jtemb.2023.127200_bib13",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1097/PCC.0b013e31819371ce",
"article-title": "Zinc homeostasis in pediatric critical illness",
"author": "Cvijanovich",
"doi-asserted-by": "crossref",
"first-page": "29",
"issue": "1",
"journal-title": "Pediatr Crit Care Med",
"key": "10.1016/j.jtemb.2023.127200_bib14",
"volume": "10",
"year": "2009"
},
{
"DOI": "10.1016/j.jtemb.2017.11.013",
"article-title": "Changes in zinc status and zinc transporters expression in whole blood of patients with Systemic Inflammatory Response Syndrome (SIRS)",
"author": "Florea",
"doi-asserted-by": "crossref",
"first-page": "202",
"journal-title": "J Trace Elements in Medicine and Biology",
"key": "10.1016/j.jtemb.2023.127200_bib15",
"volume": "49",
"year": "2018"
},
{
"DOI": "10.1016/j.jtemb.2022.126944",
"article-title": "Evaluation of zinc, copper, and Cu:Zn ratio in serum, and their implications in the course of COVID-19",
"author": "Ivanova",
"doi-asserted-by": "crossref",
"journal-title": "J Trace Elem Med Biol.",
"key": "10.1016/j.jtemb.2023.127200_bib16",
"volume": "71",
"year": "2022"
},
{
"DOI": "10.1016/j.jmii.2021.01.012",
"article-title": "Low blood zinc concentrations in patients with poor clinical outcome during SARS-CoV-2 infection: is there a need to supplement with zinc COVID-19 patients?",
"author": "Dubourg",
"doi-asserted-by": "crossref",
"first-page": "997",
"issue": "5",
"journal-title": "J Microbiol Immunol Infect.",
"key": "10.1016/j.jtemb.2023.127200_bib17",
"volume": "54",
"year": "2021"
},
{
"DOI": "10.1186/s40249-020-00646-x",
"article-title": "Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review",
"author": "Adhikari",
"doi-asserted-by": "crossref",
"first-page": "29",
"issue": "1",
"journal-title": "Infect Dis Poverty.",
"key": "10.1016/j.jtemb.2023.127200_bib18",
"volume": "9",
"year": "2020"
},
{
"article-title": "KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease",
"author": "KDIGO CKD Work Group",
"first-page": "1",
"journal-title": "Kidney Int Suppl",
"key": "10.1016/j.jtemb.2023.127200_bib19",
"volume": "3",
"year": "2013"
},
{
"article-title": "Evaluation of zinc levels in biological samples of hypertensive patients in Valladolid",
"author": "Dueñas Ricaurte",
"first-page": "133",
"issue": "1",
"journal-title": "Nutrición Clínica",
"key": "10.1016/j.jtemb.2023.127200_bib20",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.1177/0148607108322402",
"article-title": "Zinc supplementation in critically ill patients: a key pharmaconutrient?",
"author": "Heyland",
"doi-asserted-by": "crossref",
"first-page": "509",
"issue": "5",
"journal-title": "JPEN J Parenter Enteral Nutr.",
"key": "10.1016/j.jtemb.2023.127200_bib21",
"volume": "32",
"year": "2008"
},
{
"DOI": "10.1111/j.1399-6576.2011.02425.x",
"article-title": "Serum zinc in critically ill adult patients with acute respiratory failure",
"author": "Linko",
"doi-asserted-by": "crossref",
"first-page": "615",
"issue": "5",
"journal-title": "Acta Anaesthesiol Scand",
"key": "10.1016/j.jtemb.2023.127200_bib22",
"volume": "55",
"year": "2011"
},
{
"DOI": "10.3945/ajcn.110.008417",
"article-title": "A comparison of zinc metabolism, inflammation, and disease severity in critically ill infected and noninfected adults early after intensive care unit admission",
"author": "Besecker",
"doi-asserted-by": "crossref",
"first-page": "1356",
"issue": "6",
"journal-title": "Am J Clin Nutr.",
"key": "10.1016/j.jtemb.2023.127200_bib23",
"volume": "93",
"year": "2011"
},
{
"DOI": "10.3945/ajcn.2009.27230G",
"article-title": "Methods of assessment of zinc status in humans: a systematic review",
"author": "Lowe",
"doi-asserted-by": "crossref",
"first-page": "2040S",
"journal-title": "Am J Clin Nutr",
"key": "10.1016/j.jtemb.2023.127200_bib24",
"volume": "89",
"year": "2009"
},
{
"DOI": "10.1371/journal.ppat.1001176",
"article-title": "Zn(2+) inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture",
"author": "te Velthuis",
"doi-asserted-by": "crossref",
"issue": "11",
"journal-title": "PLoS Pathog",
"key": "10.1016/j.jtemb.2023.127200_bib25",
"volume": "6",
"year": "2010"
},
{
"DOI": "10.1093/advances/nmz013",
"article-title": "The Role of Zinc in Antiviral Immunity",
"author": "Read",
"doi-asserted-by": "crossref",
"first-page": "696",
"issue": "4",
"journal-title": "Adv Nutr.",
"key": "10.1016/j.jtemb.2023.127200_bib26",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1016/j.vacun.2021.08.003",
"article-title": "Zinc role in Covid-19 disease and prevention",
"author": "Boretti",
"doi-asserted-by": "crossref",
"first-page": "147",
"issue": "2",
"journal-title": "Vacunas",
"key": "10.1016/j.jtemb.2023.127200_bib27",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1038/srep21850",
"article-title": "Infants and elderlies are susceptible to zinc deficiency",
"author": "Yasuda",
"doi-asserted-by": "crossref",
"first-page": "21850",
"journal-title": "Sci Rep",
"key": "10.1016/j.jtemb.2023.127200_bib28",
"volume": "6",
"year": "2016"
},
{
"DOI": "10.3389/fimmu.2020.01736",
"article-title": "A Hypothesis for the Possible Role of Zinc in the Immunological Pathways Related to COVID-19 Infection",
"author": "Mayor-Ibarguren",
"doi-asserted-by": "crossref",
"first-page": "1736",
"journal-title": "Front. Immunol. 2020",
"key": "10.1016/j.jtemb.2023.127200_bib29",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.3390/nu13020562",
"article-title": "Low Zinc Levels at Admission Associates with Poor Clinical Outcomes in SARS-CoV-2 Infection",
"author": "Vogel-González",
"doi-asserted-by": "crossref",
"first-page": "562",
"journal-title": "Nutrients.",
"key": "10.1016/j.jtemb.2023.127200_bib30",
"volume": "13",
"year": "2021"
},
{
"article-title": "Hypozincemia in the early stage of COVID-19 is associated with an increased risk of severe COVID-19",
"author": "Fromonot",
"journal-title": "Clin Nutr",
"key": "10.1016/j.jtemb.2023.127200_bib31",
"year": "2021"
},
{
"DOI": "10.1016/j.jtemb.2022.127055",
"article-title": "Association of Trace Element Status in COVID-19 Patients with Disease Severity",
"author": "Bego",
"doi-asserted-by": "crossref",
"journal-title": "J Trace Elem Med Biol",
"key": "10.1016/j.jtemb.2023.127200_bib32",
"volume": "74",
"year": "2022"
},
{
"DOI": "10.1111/j.1399-6576.2011.02425.x",
"article-title": "Serum zinc in critically ill adult patients with acute respiratory failure",
"author": "Linko",
"doi-asserted-by": "crossref",
"first-page": "615",
"journal-title": "Acta Anaesthesiol Scand",
"key": "10.1016/j.jtemb.2023.127200_bib33",
"volume": "55",
"year": "2011"
},
{
"DOI": "10.3945/ajcn.110.008417",
"article-title": "A comparison of zinc metabolism, inflammation, and disease severity in critically ill infected and noninfected adults early after intensive care unit admission",
"author": "Besecker",
"doi-asserted-by": "crossref",
"first-page": "1356",
"journal-title": "Am J Clin Nutr",
"key": "10.1016/j.jtemb.2023.127200_bib34",
"volume": "93",
"year": "2011"
},
{
"DOI": "10.3945/ajcn.111.023812",
"article-title": "Quantitative data on the magnitude of the systemic inflammatory response and its effect on micronutrient status based on plasma measurements",
"author": "Duncan",
"doi-asserted-by": "crossref",
"first-page": "64",
"journal-title": "Am J Clin Nutr",
"key": "10.1016/j.jtemb.2023.127200_bib35",
"volume": "95",
"year": "2012"
},
{
"DOI": "10.1007/s12576-017-0571-7",
"article-title": "Zinc status is associated with inflammation, oxidative stress, lipid, and glucose metabolism",
"author": "Olechnowicz",
"doi-asserted-by": "crossref",
"first-page": "19",
"journal-title": "J Physiol Sci",
"key": "10.1016/j.jtemb.2023.127200_bib36",
"volume": "68",
"year": "2018"
},
{
"DOI": "10.1146/annurev.nu.10.070190.002215",
"article-title": "Zinc deficiency and immune function",
"author": "Keen",
"doi-asserted-by": "crossref",
"first-page": "415",
"journal-title": "Annu Rev Nutr",
"key": "10.1016/j.jtemb.2023.127200_bib37",
"volume": "10",
"year": "1990"
},
{
"DOI": "10.1038/ejcn.2010.118",
"article-title": "Determinants of serum zinc concentrations in a population of French middle-age subjects (SU.VI.MAX cohort)",
"author": "Arnaud",
"doi-asserted-by": "crossref",
"journal-title": "European Journal of Clinical Nutrition",
"key": "10.1016/j.jtemb.2023.127200_bib38",
"year": "2010"
},
{
"DOI": "10.1016/j.jtemb.2022.127099",
"article-title": "Relationship between selenium status, selenoproteins and COVID-19 and other inflammatory diseases: A critical review",
"author": "Golin",
"doi-asserted-by": "crossref",
"journal-title": "J Trace Elem Med Biol",
"key": "10.1016/j.jtemb.2023.127200_bib39",
"volume": "75",
"year": "2023"
},
{
"DOI": "10.1186/s12879-021-06617-3",
"article-title": "The correlation between serum selenium, zinc, and COVID-19 severity: an observational study",
"author": "Razeghi Jahromi",
"doi-asserted-by": "crossref",
"first-page": "899",
"issue": "1",
"journal-title": "BMC Infect Dis.",
"key": "10.1016/j.jtemb.2023.127200_bib40",
"volume": "21",
"year": "2021"
}
],
"reference-count": 40,
"references-count": 40,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0946672X23000767"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Inorganic Chemistry",
"Molecular Medicine",
"Biochemistry"
],
"subtitle": [],
"title": "Zinc Levels of Patients With A Moderate to Severe COVID-19 Infection at Hospital Admission and After 4th Days of Ward Hospitalization and Their Clinical Outcome",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy"
}
