Prognostic factors in hospitalized patients with COVID-19 pneumonia and effectiveness of prophylactic anticoagulant therapy: a single-center retrospective study
et al., BMC Infectious Diseases, doi:10.1186/s12879-025-10666-3, Mar 2025
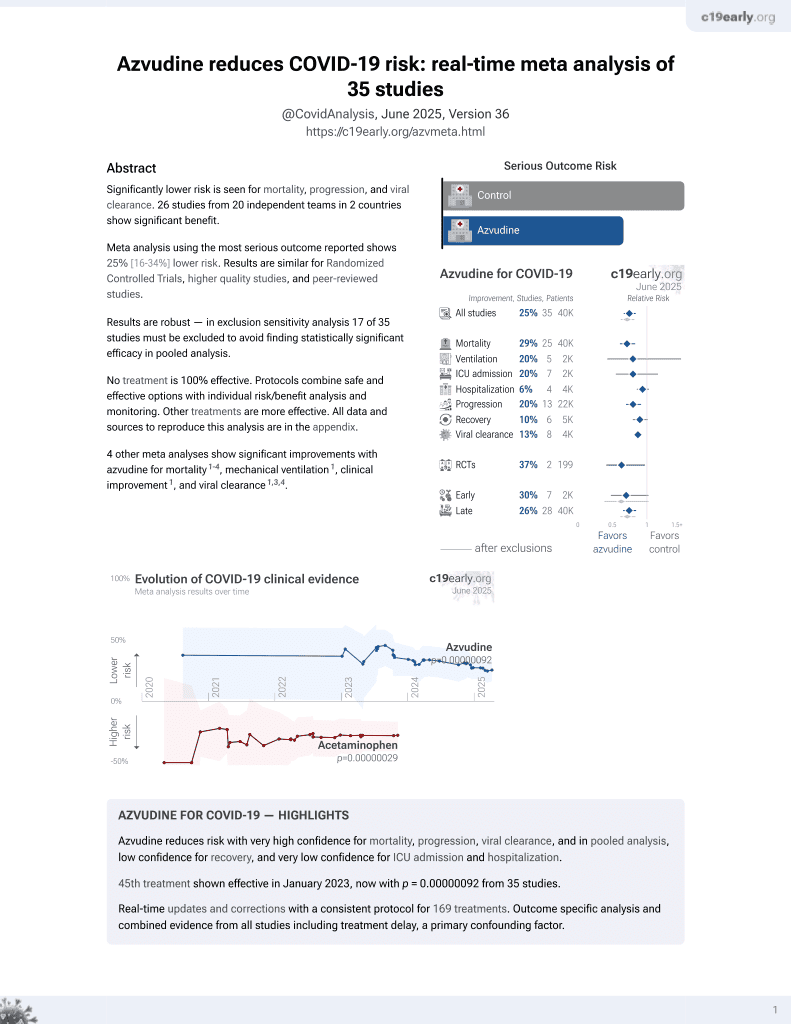
Azvudine for COVID-19
48th treatment shown to reduce risk in
January 2023, now with p = 0.000000017 from 39 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 2,520 hospitalized COVID-19 pneumonia patients focusing on prophylactic anticoagulation but also reporting results for azvudine and paxlovid.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments3.
Study covers azvudine and paxlovid.
|
risk of death, 47.5% higher, RR 1.48, p < 0.001, treatment 165 of 865 (19.1%), control 214 of 1,655 (12.9%), all.
|
|
risk of death, 54.6% higher, RR 1.55, p < 0.001, treatment 158 of 832 (19.0%), control 198 of 1,612 (12.3%), w/o VTE.
|
|
risk of death, 43.0% lower, RR 0.57, p = 0.21, treatment 7 of 33 (21.2%), control 16 of 43 (37.2%), NNT 6.3, VTE.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Xiong et al., Real-world data of Azvudine-induced hepatotoxicity among hospitalized COVID-19 patients in China: a retrospective case-control study, Frontiers in Pharmacology, doi:10.3389/fphar.2025.1558054.
He et al., 3 Mar 2025, retrospective, China, peer-reviewed, median age 71.0, 8 authors, study period December 2022 - January 2023.
Contact: guoluhx@126.com.
Prognostic factors in hospitalized patients with COVID-19 pneumonia and effectiveness of prophylactic anticoagulant therapy: a single-center retrospective study
BMC Infectious Diseases, doi:10.1186/s12879-025-10666-3
Background COVID-19 pneumonia patients encounter the potential risk of venous thromboembolism (VTE) and mortality during hospitalization. This study aimed to analyzed risk factors of all-cause mortality in hospitalized patients with COVID-19 pneumonia, and investigated the effectiveness of prophylactic anticoagulation and hospital stays on the mortality in hospitalized patients with nonVTE.
Methods We retrospectively analyzed all COVID-19 pneumonia patients who were admitted to our medical center from December 2022 to January 2023. Clinical data and outcome events were collected from patients' electronic medical records. Cox regression was used to identify poor prognostic factors of COVID-19 pneumonia patients with VTE and nonVTE. Landmark analysis was conducted to identify time points of hospital stays between anticoagulation treatment and in-hospital survival outcomes in COVID-19 pneumonia patients with nonVTE. Binary logistic regression analysis was performed to investigate factors related to prolonged hospital stays.
Results Among 2,520 COVID-19 pneumonia patients, 1047 received prophylactic anticoagulation and 76 complicated with VTE during hospitalization. Survival curve analysis showed no statistically significant difference in mortality between COVID-19 pneumonia patients with VTE and nonVTE in prophylactic anticoagulant group (P = 0.63). Multivariate cox regression analysis revealed that male(HR = 1.398, 95%CI= [1.021,1.915]), BMI (HR = 0.935, 95%CI= [0.900,0.972]), lymphocytes (HR = 0.576, 95%CI= [0.409,0.809]), platelets (HR = 0.997, 95%CI= [0.995,0.999]), albumin (HR = 0.950, 95%CI= [0.926,0.975]), lactate dehydrogenase (HR = 1.001, 95%CI= [1.001,1.002]) were risk factors for mortality in COVID-19 pneumonia patients with nonVTE, while sCRP (HR = 1.010, 95%CI= [1.004,1.015]), anticoagulant therapy (HR = 0.247, 95%CI= [0.096,0.632]) were risk factors for mortality in COVID-19 pneumonia patients with VTE. Landmark analysis showed that for the hospital stays of 11 days, the difference in the impact of prophylactic anticoagulation on mortality was statistically significant in COVID-19 pneumonia patients with nonVTE (≤ 11days, P = 0.014; > 11days, P = 0.01). CVD (OR = 1.717, 95%CI= [1.248,2.363]), CRD (OR = 1.605, 95%CI= [1.133,2.274]), sCRP (OR = 1.003, 95%CI= [1.000,1.006]), Alb (OR = 0.959, 95%CI = [0.932,0.987]) and use of glucocorticoid (OR = 1.428, 95%CI= [1.057,1.930]) were independent factors associated with hospital stays > 11 days in anticoagulant group.
Supplementary Information The online version contains supplementary material available at h t t p s : / / d o i . o r g / 1 0 . 1 1 8 6 / s 1 2 8 7 9 -0 2 5 -1 0 6 6 6 -3.
Supplementary Material 1
Author contributions Conception and design: X He, L Guo; administrative support: L Luo, L Guo; provision of study materials or patients: L Guo, J Ji; collection and assembly of data: X He, C Zhang, Y Liu, W Feng; data analysis and interpretation: X He, J Ji, H Fan, L Guo; manuscript writing: all authors; and final approval of the manuscript: all authors.
Data availability The original data presented in the study are included in the manuscript/ Supplementary Material, further inquiries can be directed to the corresponding author.
Declarations Ethics approval and consent to participate The study was carried out according to the principles of the Declaration of Helsinki, and was approved by Institutional Review Board of Sichuan Provincial People's Hospital, University of Electronic Science and Technology of China (Process No. 2024 -570). Written informed consent was obtained from all patients or their guardians before enrolment in the study. the study was conducted in accordance with the principles established in the Declaration of helsinki and the international council for harmonisation Guidelines for Good clinical Practice.
Consent for publication Authors are all agreed to publication.
Conflict of interest Authors have no conflict of interest.
Competing interests The..
References
Attaway, Scheraga, Bhimraj, Severe covid-19 pneumonia: pathogenesis and clinical management, BMJ
Az, Sogut, Akdemir, Impacts of demographic and clinical characteristics on disease severity and mortality in patients with confirmed COVID-19, Int J Gen Med
Barbar, Noventa, Rossetto, A risk assessment model for the identification of hospitalized medical patients at risk for venous thromboembolism: the Padua prediction Score[J], J Thromb Haemost
Berenguer, Ryan, Rodriguez-Bano, Characteristics and predictors of death among 4035 consecutively hospitalized patients with COVID-19 in Spain[J], Clin Microbiol Infect
Bijlsma, Bobeldijk, Verheij, Large-scale human metabolomics studies: a strategy for data (pre-) processing and validation, J]. Anal Chem
Bonfim, Guerini, Zambon, Optimal dosing of heparin for prophylactic anticoagulation in critically ill COVID-19 patients a systematic review and meta-analysis of randomized controlled trials[J], J Crit Care
Cangemi, Calvieri, Falcone, Comparison of thrombotic events and mortality in patients with Community-Acquired pneumonia and COVID-19: A multicenter observational Study, J]. Thromb Haemost
Chan, Baker, Conroy, Burden of cardiovascular disease on coronavirus disease 2019 hospitalizations in the USA, Coron Artery Dis
Chen, Zhang, Liu, Effect of anticoagulation on the incidence of venous thromboembolism, major bleeding, and mortality among hospitalized COVID-19 patients: an updated meta-analysis, J]. Front Cardiovasc Med
Chen, Zhang, Zheng, DVT incidence and risk factors in critically ill patients with COVID-19, J Thromb Thrombolysis
Cohen, Gianos, Barish, Prevalence and predictors of venous thromboembolism or mortality in hospitalized COVID-19 Patients[J], Thromb Haemost
Connors, Levy, COVID-19 and its implications for thrombosis and anticoagulation, J]. Blood
Fernandez-Capitan, Barba, Diaz-Pedroche, Presenting characteristics, treatment patterns, and outcomes among patients with venous thromboembolism during hospitalization for COVID-19, Semin Thromb Hemost
Filippi, Turcato, Milan, Long term follow-up of a multicentre cohort of COVID-19 patients with pulmonary embolism: anticoagulation management and outcomes, J]. Thromb Res
Gabet, Grave, Tuppin, One year prevalence of venous thromboembolism in hospitalized COVID-19 patients in France: patients' characteristics, time trends, and Outcomes, J]. Thromb Haemost
Gromadzinski, Zechowicz, Moczulska, Clinical characteristics and predictors of In-Hospital mortality of patients hospitalized with COVID-19 Infection[J], J Clin Med
He, Wang, Wang, Efficacy and safety of glucocorticoids use in patients with COVID-19: a systematic review and network meta-analysis, J]. BMC Infect Dis
Hsu, Liu, Zayac, Intensity of anticoagulation and survival in patients hospitalized with COVID-19 pneumonia[J], Thromb Res
Hyams, Qian, Nava, Impact of SARS-CoV-2 infective exacerbation of chronic obstructive pulmonary disease on clinical outcomes in a prospective cohort study of hospitalised adults[J], J R Soc Med
Iam-Arunthai, Chamnanchanunt, Thungthong, COVID-19 with high-sensitivity CRP associated with worse dynamic clinical parameters and outcomes, J]. Front Med
Iam-Arunthai, Chamnanchanunt, Thungthong, Thrombosis and bleeding risk scores are strongly associated with mortality in hospitalized patients with COVID-19: A multicenter cohort Study[J], J Clin Med
Labbe, Contou, Heming, Effects of Standard-Dose prophylactic, High-Dose prophylactic, and therapeutic anticoagulation in patients with hypoxemic COVID-19 pneumonia: the ANTICOVID randomized clinical Trial[J], JAMA Intern Med
Lee, Jehangir, Lin, 3D-PAST: risk assessment model for predicting venous thromboembolism in COVID-19[J], J Clin Med
Li, Chen, Hu, Impact of corticosteroid therapy on outcomes of persons with SARS-CoV-2, SARS-CoV, or MERS-CoV infection: a systematic review and meta-analysis, Leukemia
Li, Xu, Xiang, Risk factors for systemic and venous thromboembolism, mortality and bleeding risks in 1125 patients with COVID-19: relationship with anticoagulation status, J]. Aging
Murthy, Gordon, Lowry, Evolution of serious and life-threatening COVID-19 pneumonia as the SARS-CoV-2 pandemic progressed: an observational study of mortality to 60 days after admission to a 15-hospital US health system, BMJ Open
Niculae, Gorea, Tirlescu, Pulmonary thrombosis despite therapeutic anticoagulation in COVID-19 pneumonia: A case report and literature Review, J]. Viruses
Norman, Monteiro, Salama, Sample size calculations: should the emperor's clothes be off the Peg or made to measure?, BMJ
Parisi, Costanzo, Castelnuovo, Different anticoagulant regimens, mortality, and bleeding in hospitalized patients with COVID-19: A systematic review and an updated Meta-Analysis[J], Semin Thromb Hemost
Piazza, Campia, Hurwitz, Registry of arterial and venous thromboembolic complications in patients with COVID-19[J], J Am Coll Cardiol
Poor, Pulmonary thrombosis and thromboembolism in COVID-19, J]. Chest
Prince, Dev, Lane, Major hemorrhage and mortality in COVID-19 patients on therapeutic anticoagulation for venous thromboembolism[J], J Thromb Thrombolysis
Ramirez, Mora, Campillo, A clinical prediction rule for thrombosis in critically ill COVID-19 patients: step 1 results of the thromcco Study[J], J Clin Med
Ramon, Bas, Herrero, Personalized assessment of mortality risk and hospital stay duration in hospitalized patients with COVID-19 treated with Remdesivir: A machine learning Approach, J]. J Clin Med
Rentsch, Beckman, Tomlinson, Early initiation of prophylactic anticoagulation for prevention of coronavirus disease 2019 mortality in patients admitted to hospital in the united States: cohort study, BMJ
Simon, Borgne, Lefevbre, Platelet-to-Lymphocyte ratio (PLR) is not a predicting marker of severity but of mortality in COVID-19 patients admitted to the emergency department: A retrospective multicenter Study[J], J Clin Med
Spyropoulos, To prophylax or not, and how much and how long? Controversies in VTE prevention for medical inpatients, including COVID-19 inpatients[J], Hematol Am Soc Hematol Educ Program
Tian, Jiang, Yao, Predictors of mortality in hospitalized COVID-19 patients: A systematic review and meta-analysis, J Med Virol
Vergori, Lorenzini, Cozzi-Lepri, Prophylactic heparin and risk of orotracheal intubation or death in patients with mild or moderate COVID-19 pneumonia, J]. Sci Rep
Zhai, Li, Chen, Prevention and treatment of venous thromboembolism associated with coronavirus disease 2019 infection: A consensus statement before Guidelines, J]. Thromb Haemost
Zhang, Bastard, Cobat, Human genetic and immunological determinants of critical COVID-19 pneumonia, Nature
DOI record:
{
"DOI": "10.1186/s12879-025-10666-3",
"ISSN": [
"1471-2334"
],
"URL": "http://dx.doi.org/10.1186/s12879-025-10666-3",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>COVID-19 pneumonia patients encounter the potential risk of venous thromboembolism (VTE) and mortality during hospitalization. This study aimed to analyzed risk factors of all-cause mortality in hospitalized patients with COVID-19 pneumonia, and investigated the effectiveness of prophylactic anticoagulation and hospital stays on the mortality in hospitalized patients with nonVTE.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>We retrospectively analyzed all COVID-19 pneumonia patients who were admitted to our medical center from December 2022 to January 2023. Clinical data and outcome events were collected from patients’ electronic medical records. Cox regression was used to identify poor prognostic factors of COVID-19 pneumonia patients with VTE and nonVTE. Landmark analysis was conducted to identify time points of hospital stays between anticoagulation treatment and in-hospital survival outcomes in COVID-19 pneumonia patients with nonVTE. Binary logistic regression analysis was performed to investigate factors related to prolonged hospital stays.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>Among 2,520 COVID-19 pneumonia patients, 1047 received prophylactic anticoagulation and 76 complicated with VTE during hospitalization. Survival curve analysis showed no statistically significant difference in mortality between COVID-19 pneumonia patients with VTE and nonVTE in prophylactic anticoagulant group (<jats:italic>P</jats:italic> = 0.63). Multivariate cox regression analysis revealed that male(HR = 1.398, 95%CI= [1.021,1.915]), BMI (HR = 0.935, 95%CI= [0.900,0.972]), lymphocytes (HR = 0.576, 95%CI= [0.409,0.809]), platelets (HR = 0.997, 95%CI= [0.995,0.999]), albumin (HR = 0.950, 95%CI= [0.926,0.975]), lactate dehydrogenase (HR = 1.001, 95%CI= [1.001,1.002]) were risk factors for mortality in COVID-19 pneumonia patients with nonVTE, while sCRP (HR = 1.010, 95%CI= [1.004,1.015]), anticoagulant therapy (HR = 0.247, 95%CI= [0.096,0.632]) were risk factors for mortality in COVID-19 pneumonia patients with VTE. Landmark analysis showed that for the hospital stays of 11 days, the difference in the impact of prophylactic anticoagulation on mortality was statistically significant in COVID-19 pneumonia patients with nonVTE (≤ 11days, <jats:italic>P</jats:italic> = 0.014; > 11days, <jats:italic>P</jats:italic> = 0.01). CVD (OR = 1.717, 95%CI= [1.248,2.363]), CRD (OR = 1.605, 95%CI= [1.133,2.274]), sCRP (OR = 1.003, 95%CI= [1.000,1.006]), Alb (OR = 0.959, 95%CI = [0.932,0.987]) and use of glucocorticoid (OR = 1.428, 95%CI= [1.057,1.930]) were independent factors associated with hospital stays > 11 days in anticoagulant group.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Conclusions</jats:title>\n <jats:p>This study indicated that Male, lower BMI, peripheral blood lymphocytes, platelets, albumin and elevated lactate dehydrogenase were associated with poor hospitalisation outcomes in COVID-19 pneumonia patients with nonVTE. As for COVID-19 pneumonia patients with VTE, poor hospitalisation outcomes were associated with elevated sCRP levels and no given anticoagulant therapy. No significant difference in mortality between hospitalized COVID-19 pneumonia patients with VTE and nonVTE when receiving prophylactic anticoagulation. Prolonged hospital stays (> 11 days) may limit the effectiveness of prophylactic anticoagulation on lower in-hospital mortality for COVID-19 pneumonia patients with nonVTE.</jats:p>\n </jats:sec>",
"alternative-id": [
"10666"
],
"article-number": "303",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "5 November 2024"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "18 February 2025"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "3 March 2025"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Ethics approval and consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "The study was carried out according to the principles of the Declaration of Helsinki, and was approved by Institutional Review Board of Sichuan Provincial People’s Hospital, University of Electronic Science and Technology of China (Process No. 2024 − 570). Written informed consent was obtained from all patients or their guardians before enrolment in the study. the study was conducted in accordance with the principles established in the Declaration of helsinki and the international council for harmonisation Guidelines for Good clinical Practice."
},
{
"group": {
"label": "Consent for publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "Authors are all agreed to publication."
},
{
"group": {
"label": "Conflict of interest",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "Authors have no conflict of interest."
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 5,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "He",
"given": "Xing",
"sequence": "first"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Chun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ji",
"given": "Jiaqi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Liu",
"given": "Yang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Feng",
"given": "Wanjie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Luo",
"given": "Linjie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fan",
"given": "Hong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Guo",
"given": "Lu",
"sequence": "additional"
}
],
"container-title": "BMC Infectious Diseases",
"container-title-short": "BMC Infect Dis",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2025,
3,
3
]
],
"date-time": "2025-03-03T14:35:44Z",
"timestamp": 1741012544000
},
"deposited": {
"date-parts": [
[
2025,
3,
3
]
],
"date-time": "2025-03-03T14:35:55Z",
"timestamp": 1741012555000
},
"funder": [
{
"award": [
"Q21048"
],
"name": "Sichuan Medical Association Youth Innovation Project"
},
{
"award": [
"KY2022SJ0116"
],
"name": "Scientific Research Project of Sichuan Medical and Healthcare Promotion Institute"
},
{
"award": [
"2022-YF09-00003-SN"
],
"name": "Major Science and Technology Application Demonstration Project of Chengdu Science and Technology Bureau"
}
],
"indexed": {
"date-parts": [
[
2025,
3,
4
]
],
"date-time": "2025-03-04T05:42:50Z",
"timestamp": 1741066970252,
"version": "3.38.0"
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2025,
3,
3
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2025,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
3,
3
]
],
"date-time": "2025-03-03T00:00:00Z",
"timestamp": 1740960000000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
3,
3
]
],
"date-time": "2025-03-03T00:00:00Z",
"timestamp": 1740960000000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1186/s12879-025-10666-3.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1186/s12879-025-10666-3/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1186/s12879-025-10666-3.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1186",
"published": {
"date-parts": [
[
2025,
3,
3
]
]
},
"published-online": {
"date-parts": [
[
2025,
3,
3
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1038/s41586-022-04447-0",
"author": "Q Zhang",
"doi-asserted-by": "publisher",
"first-page": "587",
"issue": "7902",
"journal-title": "Nature",
"key": "10666_CR1",
"unstructured": "Zhang Q, Bastard P, Cobat A, et al. Human genetic and immunological determinants of critical COVID-19 pneumonia[J]. Nature. 2022;603(7902):587–98.",
"volume": "603",
"year": "2022"
},
{
"DOI": "10.3390/jcm12010143",
"doi-asserted-by": "crossref",
"key": "10666_CR2",
"unstructured": "Gromadzinski L, Zechowicz M, Moczulska B et al. Clinical characteristics and predictors of In-Hospital mortality of patients hospitalized with COVID-19 Infection[J]. J Clin Med, 2022,12(1)."
},
{
"DOI": "10.1136/bmj.n436",
"author": "AH Attaway",
"doi-asserted-by": "publisher",
"first-page": "n436",
"journal-title": "BMJ",
"key": "10666_CR3",
"unstructured": "Attaway AH, Scheraga RG, Bhimraj A, et al. Severe covid-19 pneumonia: pathogenesis and clinical management[J]. BMJ. 2021;372:n436.",
"volume": "372",
"year": "2021"
},
{
"DOI": "10.1182/blood.2020006000",
"author": "JM Connors",
"doi-asserted-by": "publisher",
"first-page": "2033",
"issue": "23",
"journal-title": "Blood",
"key": "10666_CR4",
"unstructured": "Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation[J]. Blood. 2020;135(23):2033–40.",
"volume": "135",
"year": "2020"
},
{
"DOI": "10.1055/s-0042-1743475",
"author": "A Gabet",
"doi-asserted-by": "publisher",
"first-page": "1532",
"issue": "9",
"journal-title": "Thromb Haemost",
"key": "10666_CR5",
"unstructured": "Gabet A, Grave C, Tuppin P, et al. One year prevalence of venous thromboembolism in hospitalized COVID-19 patients in France: patients’ characteristics, time trends, and Outcomes[J]. Thromb Haemost. 2022;122(9):1532–41.",
"volume": "122",
"year": "2022"
},
{
"DOI": "10.1016/j.jacc.2020.08.070",
"author": "G Piazza",
"doi-asserted-by": "publisher",
"first-page": "2060",
"issue": "18",
"journal-title": "J Am Coll Cardiol",
"key": "10666_CR6",
"unstructured": "Piazza G, Campia U, Hurwitz S, et al. Registry of arterial and venous thromboembolic complications in patients with COVID-19[J]. J Am Coll Cardiol. 2020;76(18):2060–72.",
"volume": "76",
"year": "2020"
},
{
"DOI": "10.1055/s-0040-1718402",
"author": "C Fernandez-Capitan",
"doi-asserted-by": "publisher",
"first-page": "351",
"issue": "4",
"journal-title": "Semin Thromb Hemost",
"key": "10666_CR7",
"unstructured": "Fernandez-Capitan C, Barba R, Diaz-Pedroche M, et al. Presenting characteristics, treatment patterns, and outcomes among patients with venous thromboembolism during hospitalization for COVID-19[J]. Semin Thromb Hemost. 2021;47(4):351–61.",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.3389/fcvm.2024.1381408",
"author": "X Chen",
"doi-asserted-by": "publisher",
"first-page": "1381408",
"journal-title": "Front Cardiovasc Med",
"key": "10666_CR8",
"unstructured": "Chen X, Zhang S, Liu H, et al. Effect of anticoagulation on the incidence of venous thromboembolism, major bleeding, and mortality among hospitalized COVID-19 patients: an updated meta-analysis[J]. Front Cardiovasc Med. 2024;11:1381408.",
"volume": "11",
"year": "2024"
},
{
"DOI": "10.1016/j.chest.2021.06.016",
"author": "HD Poor",
"doi-asserted-by": "publisher",
"first-page": "1471",
"issue": "4",
"journal-title": "Chest",
"key": "10666_CR9",
"unstructured": "Poor HD. Pulmonary thrombosis and thromboembolism in COVID-19[J]. Chest. 2021;160(4):1471–80.",
"volume": "160",
"year": "2021"
},
{
"DOI": "10.1136/bmj.n311",
"author": "CT Rentsch",
"doi-asserted-by": "publisher",
"first-page": "n311",
"journal-title": "BMJ",
"key": "10666_CR10",
"unstructured": "Rentsch CT, Beckman JA, Tomlinson L, et al. Early initiation of prophylactic anticoagulation for prevention of coronavirus disease 2019 mortality in patients admitted to hospital in the united States: cohort study[J]. BMJ. 2021;372:n311.",
"volume": "372",
"year": "2021"
},
{
"DOI": "10.1002/jmv.26050",
"author": "W Tian",
"doi-asserted-by": "publisher",
"first-page": "1875",
"issue": "10",
"journal-title": "J Med Virol",
"key": "10666_CR11",
"unstructured": "Tian W, Jiang W, Yao J, et al. Predictors of mortality in hospitalized COVID-19 patients: A systematic review and meta-analysis[J]. J Med Virol. 2020;92(10):1875–83.",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.18632/aging.202769",
"author": "W Li",
"doi-asserted-by": "publisher",
"first-page": "9225",
"issue": "7",
"journal-title": "Aging",
"key": "10666_CR12",
"unstructured": "Li W, Xu Z, Xiang H, et al. Risk factors for systemic and venous thromboembolism, mortality and bleeding risks in 1125 patients with COVID-19: relationship with anticoagulation status[J]. Aging. 2021;13(7):9225–42.",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1055/a-1692-9939",
"author": "R Cangemi",
"doi-asserted-by": "publisher",
"first-page": "257",
"issue": "2",
"journal-title": "Thromb Haemost",
"key": "10666_CR13",
"unstructured": "Cangemi R, Calvieri C, Falcone M, et al. Comparison of thrombotic events and mortality in patients with Community-Acquired pneumonia and COVID-19: A multicenter observational Study[J]. Thromb Haemost. 2022;122(2):257–66.",
"volume": "122",
"year": "2022"
},
{
"DOI": "10.1016/j.thromres.2020.09.030",
"author": "A Hsu",
"doi-asserted-by": "publisher",
"first-page": "375",
"journal-title": "Thromb Res",
"key": "10666_CR14",
"unstructured": "Hsu A, Liu Y, Zayac AS, et al. Intensity of anticoagulation and survival in patients hospitalized with COVID-19 pneumonia[J]. Thromb Res. 2020;196:375–8.",
"volume": "196",
"year": "2020"
},
{
"DOI": "10.1016/j.jcrc.2023.154344",
"author": "L Bonfim",
"doi-asserted-by": "publisher",
"first-page": "154344",
"journal-title": "J Crit Care",
"key": "10666_CR15",
"unstructured": "Bonfim L, Guerini IS, Zambon MG, et al. Optimal dosing of heparin for prophylactic anticoagulation in critically ill COVID-19 patients a systematic review and meta-analysis of randomized controlled trials[J]. J Crit Care. 2023;77:154344.",
"volume": "77",
"year": "2023"
},
{
"DOI": "10.3390/v15071535",
"doi-asserted-by": "crossref",
"key": "10666_CR16",
"unstructured": "Niculae CM, Gorea ME, Tirlescu LG et al. Pulmonary thrombosis despite therapeutic anticoagulation in COVID-19 pneumonia: A case report and literature Review[J]. Viruses, 2023,15(7)."
},
{
"DOI": "10.1182/hematology.2022000403",
"author": "AC Spyropoulos",
"doi-asserted-by": "publisher",
"first-page": "506",
"issue": "1",
"journal-title": "Hematol Am Soc Hematol Educ Program",
"key": "10666_CR17",
"unstructured": "Spyropoulos AC. To prophylax or not, and how much and how long? Controversies in VTE prevention for medical inpatients, including COVID-19 inpatients[J]. Hematol Am Soc Hematol Educ Program. 2022;2022(1):506–14.",
"volume": "2022",
"year": "2022"
},
{
"key": "10666_CR18",
"unstructured": "World Health Organization. (2020). Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: interim guidance, 13 March 2020. World Health Organization. https://iris.who.int/handle/10665/331446. (accessed on 19 August 2024).[Z]."
},
{
"DOI": "10.1111/j.1538-7836.2010.04044.x",
"author": "S Barbar",
"doi-asserted-by": "publisher",
"first-page": "2450",
"issue": "11",
"journal-title": "J Thromb Haemost",
"key": "10666_CR19",
"unstructured": "Barbar S, Noventa F, Rossetto V, et al. A risk assessment model for the identification of hospitalized medical patients at risk for venous thromboembolism: the Padua prediction Score[J]. J Thromb Haemost. 2010;8(11):2450–7.",
"volume": "8",
"year": "2010"
},
{
"DOI": "10.1055/s-0040-1710019",
"author": "Z Zhai",
"doi-asserted-by": "publisher",
"first-page": "937",
"issue": "6",
"journal-title": "Thromb Haemost",
"key": "10666_CR20",
"unstructured": "Zhai Z, Li C, Chen Y, et al. Prevention and treatment of venous thromboembolism associated with coronavirus disease 2019 infection: A consensus statement before Guidelines[J]. Thromb Haemost. 2020;120(6):937–48.",
"volume": "120",
"year": "2020"
},
{
"DOI": "10.1136/bmj.e5278",
"author": "G Norman",
"doi-asserted-by": "publisher",
"first-page": "e5278",
"journal-title": "BMJ",
"key": "10666_CR21",
"unstructured": "Norman G, Monteiro S, Salama S. Sample size calculations: should the emperor’s clothes be off the Peg or made to measure?[J]. BMJ. 2012;345:e5278.",
"volume": "345",
"year": "2012"
},
{
"DOI": "10.1021/ac051495j",
"author": "S Bijlsma",
"doi-asserted-by": "publisher",
"first-page": "567",
"issue": "2",
"journal-title": "Anal Chem",
"key": "10666_CR22",
"unstructured": "Bijlsma S, Bobeldijk I, Verheij ER, et al. Large-scale human metabolomics studies: a strategy for data (pre-) processing and validation[J]. Anal Chem. 2006;78(2):567–74.",
"volume": "78",
"year": "2006"
},
{
"DOI": "10.1136/bmjopen-2023-075028",
"author": "SC Murthy",
"doi-asserted-by": "publisher",
"first-page": "e075028",
"issue": "7",
"journal-title": "BMJ Open",
"key": "10666_CR23",
"unstructured": "Murthy SC, Gordon SM, Lowry AM, et al. Evolution of serious and life-threatening COVID-19 pneumonia as the SARS-CoV-2 pandemic progressed: an observational study of mortality to 60 days after admission to a 15-hospital US health system[J]. BMJ Open. 2024;14(7):e075028.",
"volume": "14",
"year": "2024"
},
{
"DOI": "10.3390/jcm11143949",
"doi-asserted-by": "crossref",
"key": "10666_CR24",
"unstructured": "Lee Y, Jehangir Q, Lin CH et al. 3D-PAST: risk assessment model for predicting venous thromboembolism in COVID-19[J]. J Clin Med, 2022,11(14)."
},
{
"DOI": "10.3390/jcm12041253",
"doi-asserted-by": "crossref",
"key": "10666_CR25",
"unstructured": "Ramirez CK, Mora E, Campillo MS et al. A clinical prediction rule for thrombosis in critically ill COVID-19 patients: step 1 results of the thromcco Study[J]. J Clin Med, 2023,12(4)."
},
{
"DOI": "10.1007/s11239-020-02181-w",
"author": "S Chen",
"doi-asserted-by": "publisher",
"first-page": "33",
"issue": "1",
"journal-title": "J Thromb Thrombolysis",
"key": "10666_CR26",
"unstructured": "Chen S, Zhang D, Zheng T, et al. DVT incidence and risk factors in critically ill patients with COVID-19[J]. J Thromb Thrombolysis. 2021;51(1):33–9.",
"volume": "51",
"year": "2021"
},
{
"DOI": "10.1055/s-0041-1726034",
"author": "R Parisi",
"doi-asserted-by": "publisher",
"first-page": "372",
"issue": "4",
"journal-title": "Semin Thromb Hemost",
"key": "10666_CR27",
"unstructured": "Parisi R, Costanzo S, Di Castelnuovo A, et al. Different anticoagulant regimens, mortality, and bleeding in hospitalized patients with COVID-19: A systematic review and an updated Meta-Analysis[J]. Semin Thromb Hemost. 2021;47(4):372–91.",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.2147/IJGM.S317350",
"author": "A Az",
"doi-asserted-by": "publisher",
"first-page": "2989",
"journal-title": "Int J Gen Med",
"key": "10666_CR28",
"unstructured": "Az A, Sogut O, Akdemir T, et al. Impacts of demographic and clinical characteristics on disease severity and mortality in patients with confirmed COVID-19[J]. Int J Gen Med. 2021;14:2989–3000.",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1016/j.cmi.2020.07.024",
"author": "J Berenguer",
"doi-asserted-by": "publisher",
"first-page": "1525",
"issue": "11",
"journal-title": "Clin Microbiol Infect",
"key": "10666_CR29",
"unstructured": "Berenguer J, Ryan P, Rodriguez-Bano J, et al. Characteristics and predictors of death among 4035 consecutively hospitalized patients with COVID-19 in Spain[J]. Clin Microbiol Infect. 2020;26(11):1525–36.",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.3390/jcm13071837",
"doi-asserted-by": "crossref",
"key": "10666_CR30",
"unstructured": "Ramon A, Bas A, Herrero S et al. Personalized assessment of mortality risk and hospital stay duration in hospitalized patients with COVID-19 treated with Remdesivir: A machine learning Approach[J]. J Clin Med, 2024,13(7)."
},
{
"DOI": "10.3390/jcm11164903",
"doi-asserted-by": "crossref",
"key": "10666_CR31",
"unstructured": "Simon P, Le Borgne P, Lefevbre F et al. Platelet-to-Lymphocyte ratio (PLR) is not a predicting marker of severity but of mortality in COVID-19 patients admitted to the emergency department: A retrospective multicenter Study[J]. J Clin Med, 2022,11(16)."
},
{
"DOI": "10.3389/fmed.2024.1346646",
"author": "K Iam-Arunthai",
"doi-asserted-by": "publisher",
"first-page": "1346646",
"journal-title": "Front Med (Lausanne)",
"key": "10666_CR32",
"unstructured": "Iam-Arunthai K, Chamnanchanunt S, Thungthong P, et al. COVID-19 with high-sensitivity CRP associated with worse dynamic clinical parameters and outcomes[J]. Front Med (Lausanne). 2024;11:1346646.",
"volume": "11",
"year": "2024"
},
{
"DOI": "10.1007/s11239-022-02666-w",
"author": "MR Prince",
"doi-asserted-by": "publisher",
"first-page": "431",
"issue": "3",
"journal-title": "J Thromb Thrombolysis",
"key": "10666_CR33",
"unstructured": "Prince MR, Dev H, Lane EG, et al. Major hemorrhage and mortality in COVID-19 patients on therapeutic anticoagulation for venous thromboembolism[J]. J Thromb Thrombolysis. 2022;54(3):431–7.",
"volume": "54",
"year": "2022"
},
{
"DOI": "10.1055/a-1366-9656",
"author": "SL Cohen",
"doi-asserted-by": "publisher",
"first-page": "1043",
"issue": "8",
"journal-title": "Thromb Haemost",
"key": "10666_CR34",
"unstructured": "Cohen SL, Gianos E, Barish MA, et al. Prevalence and predictors of venous thromboembolism or mortality in hospitalized COVID-19 Patients[J]. Thromb Haemost. 2021;121(8):1043–53.",
"volume": "121",
"year": "2021"
},
{
"DOI": "10.3390/jcm13051437",
"doi-asserted-by": "crossref",
"key": "10666_CR35",
"unstructured": "Iam-Arunthai K, Chamnanchanunt S, Thungthong P et al. Thrombosis and bleeding risk scores are strongly associated with mortality in hospitalized patients with COVID-19: A multicenter cohort Study[J]. J Clin Med, 2024,13(5)."
},
{
"DOI": "10.1097/MCA.0000000000001390",
"doi-asserted-by": "crossref",
"key": "10666_CR36",
"unstructured": "Chan K, Baker J, Conroy A, et al. Burden of cardiovascular disease on coronavirus disease 2019 hospitalizations in the USA[J]. Coron Artery Dis; 2024."
},
{
"DOI": "10.1177/01410768231184162",
"author": "C Hyams",
"doi-asserted-by": "publisher",
"first-page": "371",
"issue": "11",
"journal-title": "J R Soc Med",
"key": "10666_CR37",
"unstructured": "Hyams C, Qian G, Nava G, et al. Impact of SARS-CoV-2 infective exacerbation of chronic obstructive pulmonary disease on clinical outcomes in a prospective cohort study of hospitalised adults[J]. J R Soc Med. 2023;116(11):371–85.",
"volume": "116",
"year": "2023"
},
{
"DOI": "10.1186/s12879-023-08874-w",
"author": "Q He",
"doi-asserted-by": "publisher",
"first-page": "896",
"issue": "1",
"journal-title": "BMC Infect Dis",
"key": "10666_CR38",
"unstructured": "He Q, Wang C, Wang Y, et al. Efficacy and safety of glucocorticoids use in patients with COVID-19: a systematic review and network meta–analysis[J]. BMC Infect Dis. 2023;23(1):896.",
"volume": "23",
"year": "2023"
},
{
"DOI": "10.1038/s41375-020-0848-3",
"author": "H Li",
"doi-asserted-by": "publisher",
"first-page": "1503",
"issue": "6",
"journal-title": "Leukemia",
"key": "10666_CR39",
"unstructured": "Li H, Chen C, Hu F, et al. Impact of corticosteroid therapy on outcomes of persons with SARS-CoV-2, SARS-CoV, or MERS-CoV infection: a systematic review and meta-analysis[J]. Leukemia. 2020;34(6):1503–11.",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.1038/s41598-021-90713-6",
"author": "A Vergori",
"doi-asserted-by": "publisher",
"first-page": "11334",
"issue": "1",
"journal-title": "Sci Rep",
"key": "10666_CR40",
"unstructured": "Vergori A, Lorenzini P, Cozzi-Lepri A, et al. Prophylactic heparin and risk of orotracheal intubation or death in patients with mild or moderate COVID-19 pneumonia[J]. Sci Rep. 2021;11(1):11334.",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1001/jamainternmed.2023.0456",
"author": "V Labbe",
"doi-asserted-by": "publisher",
"first-page": "520",
"issue": "6",
"journal-title": "JAMA Intern Med",
"key": "10666_CR41",
"unstructured": "Labbe V, Contou D, Heming N, et al. Effects of Standard-Dose prophylactic, High-Dose prophylactic, and therapeutic anticoagulation in patients with hypoxemic COVID-19 pneumonia: the ANTICOVID randomized clinical Trial[J]. JAMA Intern Med. 2023;183(6):520–31.",
"volume": "183",
"year": "2023"
},
{
"DOI": "10.1016/j.thromres.2023.06.019",
"author": "L Filippi",
"doi-asserted-by": "publisher",
"first-page": "73",
"journal-title": "Thromb Res",
"key": "10666_CR42",
"unstructured": "Filippi L, Turcato G, Milan M, et al. Long term follow-up of a multicentre cohort of COVID-19 patients with pulmonary embolism: anticoagulation management and outcomes[J]. Thromb Res. 2023;229:73–6.",
"volume": "229",
"year": "2023"
}
],
"reference-count": 42,
"references-count": 42,
"relation": {},
"resource": {
"primary": {
"URL": "https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-025-10666-3"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Prognostic factors in hospitalized patients with COVID-19 pneumonia and effectiveness of prophylactic anticoagulant therapy: a single-center retrospective study",
"type": "journal-article",
"update-policy": "https://doi.org/10.1007/springer_crossmark_policy",
"volume": "25"
}