Cannabis, Tobacco Use, and COVID-19 Outcomes
et al., JAMA Network Open, doi:10.1001/jamanetworkopen.2024.17977, Jun 2024
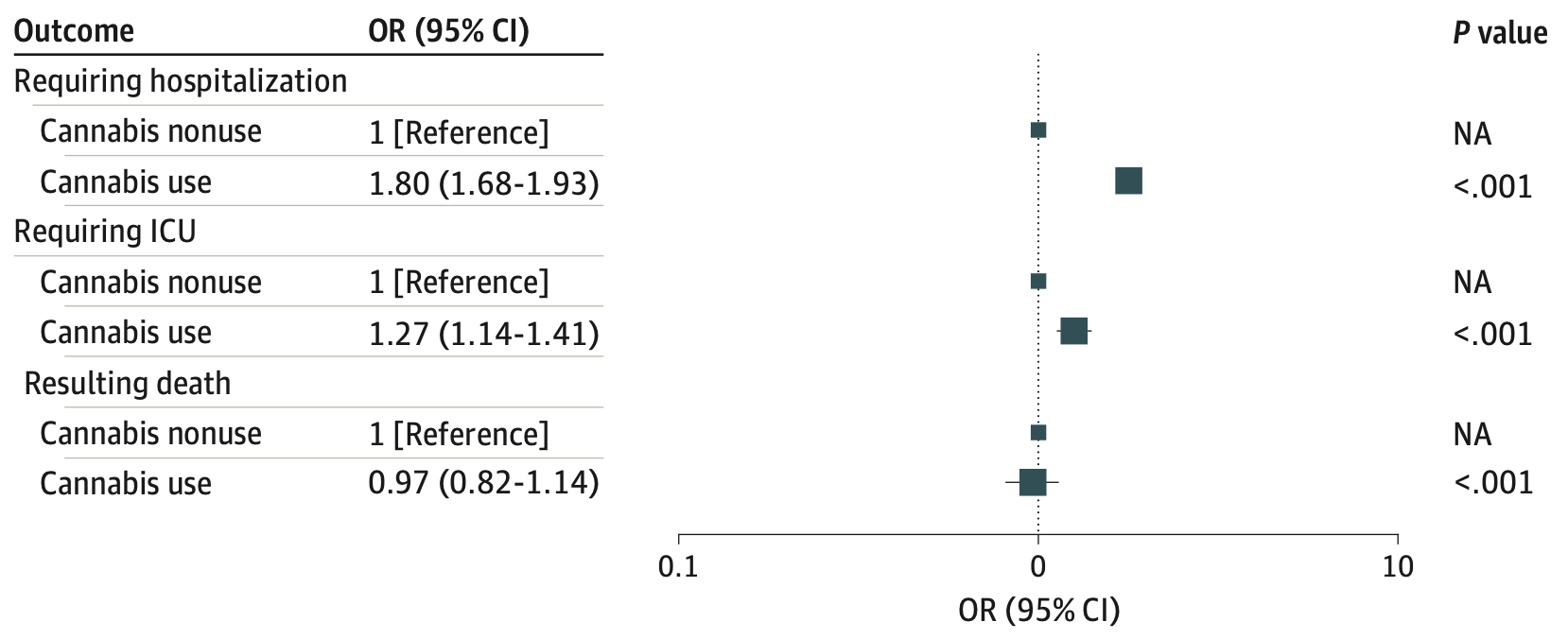
Retrospective 72,501 COVID-19 patients in the USA showing cannabis use associated with higher risk of hospitalization and ICU admission.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 3.0% lower, OR 0.97, p = 0.73, treatment 7,060, control 65,441, adjusted per study, multivariable, RR approximated with OR.
|
|
risk of ICU admission, 27.0% higher, OR 1.27, p < 0.001, treatment 7,060, control 65,441, adjusted per study, multivariable, RR approximated with OR.
|
|
risk of hospitalization, 80.0% higher, OR 1.80, p < 0.001, treatment 7,060, control 65,441, adjusted per study, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Griffith et al., 21 Jun 2024, retrospective, USA, peer-reviewed, mean age 48.9, 12 authors, study period 1 February, 2020 - 31 January, 2022.
Cannabis, Tobacco Use, and COVID-19 Outcomes
JAMA Network Open, doi:10.1001/jamanetworkopen.2024.17977
IMPORTANCE It is unclear whether cannabis use is associated with adverse health outcomes in patients with COVID-19 when accounting for known risk factors, including tobacco use. OBJECTIVE To examine whether cannabis and tobacco use are associated with adverse health outcomes from COVID-19 in the context of other known risk factors. DESIGN, SETTING, AND PARTICIPANTS This retrospective cohort study used electronic health record data from February 1, 2020, to January 31, 2022. This study included patients who were identified as having COVID-19 during at least 1 medical visit at a large academic medical center in the Midwest US. EXPOSURES Current cannabis use and tobacco smoking, as documented in the medical encounter. MAIN OUTCOMES AND MEASURES Health outcomes of hospitalization, intensive care unit (ICU) admission, and all-cause mortality following COVID-19 infection. The association between substance use (cannabis and tobacco) and these COVID-19 outcomes was assessed using multivariable modeling. RESULTS A total of 72 501 patients with COVID-19 were included (mean [SD] age, 48.9 [19.3] years; 43 315 [59.7%] female; 9710 [13.4%] had current smoking; 17 654 [24.4%] had former smoking; and 7060 [9.7%] had current use of cannabis). Current tobacco smoking was significantly associated with increased risk of hospitalization (odds ratio [OR], 1.72; 95% CI, 1.62-1.82; P < .001), ICU admission (OR, 1.22; 95% CI, 1.10-1.34; P < .001), and all-cause mortality (OR, 1.37, 95% CI, 1.20-1.57; P < .001) after adjusting for other factors. Cannabis use was significantly associated with increased risk of hospitalization (OR, 1.80; 95% CI, 1.68-1.93; P < .001) and ICU admission (OR, 1.27; 95% CI, 1.14-1.41; P < .001) but not with all-cause mortality (OR, 0.97; 95% CI, 0.82-1.14, P = .69) after adjusting for tobacco smoking, vaccination, comorbidity, diagnosis date, and demographic factors.
CONCLUSIONS AND RELEVANCE The findings of this cohort study suggest that cannabis use may be an independent risk factor for COVID-19-related complications, even after considering cigarette smoking, vaccination status, comorbidities, and other risk factors.
infection in a small cohort of college students. 10 We present a potential association between alcohol abuse and increased risk of hospitalization following COVID-19 infection. Notably, further studies are needed, as our findings were limited by small sample sizes and limited documentation within our EHR database.
Limitations This study has limitations. First, the study spanned 24 months (February 2020 to January 2022), which may have included significantly different SARS-CoV-2 disease manifestations due to the emergence of new variants, time-varying policies related to universal masking and lockdowns, and the introduction of the COVID-19 vaccine in December 2020. To reduce this concern, we included date of diagnosis and vaccination before diagnosis in our multivariable models to reduce the confounding effect of different outcomes related to time. However, caution should still be exercised when interpreting our results due to the potential for persistent confounding. Second, EHR data are limited by relying on patient self-report of substance use and subsequent documentation by medical staff. Therefore, substance use data quality within EHR often suffers from variable reporting and missing documentation. The best existing measure in the EHR data, current cannabis use, is a very crude measure without specific details on cannabis type, frequency, or recency. We have tried to reduce this bias by using data from all available hospital encounters. These findings should be..
References
Angelo, Land, Mayne, Assessing electronic nicotine delivery systems use at NCI-designated cancer centers in the Cancer Moonshot-Funded Cancer Center Cessation Initiative, Cancer Prev Res, doi:10.1158/1940-6207.CAPR-21-0105
Borgonhi, Volpatto, Ornell, Rabelo-Da-Ponte, Kessler, Multiple clinical risks for cannabis users during the COVID-19 pandemic, Addict Sci Clin Pract, doi:10.1186/s13722-021-00214-0
Croyle, Morgan, Fiore, Addressing a core gap in cancer care-the NCI Moonshot Program to help oncology patients stop smoking, N Engl J Med, doi:10.1056/NEJMp1813913
Gaiha, Cheng, Halpern-Felsher, Association between youth smoking, electronic cigarette use, and COVID-19, J Adolesc Health, doi:10.1016/j.jadohealth.2020.07.002
Griffith, Morris, Tudball, Collider bias undermines our understanding of COVID-19 disease risk and severity, Nat Commun, doi:10.1038/s41467-020-19478-2
Grossman, Benjamin-Neelon, Sonnenschein, Alcohol consumption during the COVID-19 Pandemic: a cross-sectional survey of US adults, Int J Environ Res Public Health, doi:10.3390/ijerph17249189
Hopkinson, Rossi, Moustafa, Current smoking and COVID-19 risk: results from a population symptom app in over 2.4 million people, Thorax, doi:10.1136/thoraxjnl-2020-216422
Huang, Xu, Cannabis use is associated with lower COVID-19 susceptibility but poorer survival, Front Public Health, doi:10.3389/fpubh.2022.829715
Kianersi, Ludema, Macy, Chen, Rosenberg, Relationship between high-risk alcohol consumption and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) seroconversion: a prospective seroepidemiological cohort study among American college students, Addiction, doi:10.1111/add.15835
Leung, Yang, Tam, ACE-2 expression in the small airway epithelia of smokers and COPD patients: implications for COVID-19, Eur Respir J, doi:10.1183/13993003.00688-2020
Li, Ashcroft, Chung, Risk factors for poor outcomes in hospitalised COVID-19 patients: a systematic review and meta-analysis, J Glob Health, doi:10.7189/jogh.11.10001
Lowe, Zein, Hatipoglu, Attaway, Association of smoking and cumulative pack-year exposure with COVID-19 outcomes in the Cleveland Clinic COVID-19 registry, JAMA Intern Med, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jamainternmed.2020.8360&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2024.17977
Miyara, Tubach, Pourcher, Lower rate of daily smokers with symptomatic COVID-19: a monocentric self-report of smoking habit study, Front Med, doi:10.3389/fmed.2021.668995
Nguyen, Yang, Nicolaescu, Cannabidiol inhibits SARS-CoV-2 replication through induction of the host ER stress and innate immune responses, Sci Adv, doi:10.1126/sciadv.abi6110
Patanavanich, Glantz, Smoking is associated with COVID-19 progression: a meta-analysis, Nicotine Tob Res, doi:10.1093/ntr/ntaa082
Shover, Yan, Jackson, Cannabis consumption is associated with lower COVID-19 severity among hospitalized patients: a retrospective cohort analysis, J Cannabis Res, doi:10.1186/s42238-022-00152-x
Simons, Shahab, Brown, Perski, The association of smoking status with SARS-CoV-2 infection, hospitalization and mortality from COVID-19: a living rapid evidence review with bayesian meta-analyses (version 7), Addiction, doi:10.1111/add.15276
Tegria, None
Vogel, Data and methods around reference values in pediatrics
Von Elm, Altman, Egger, Pocock, Gøtzsche et al., Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies, BMJ, doi:10.1136/bmj.39335.541782.AD
Wang, Kaelber, Xu, Volkow, COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States, Mol Psychiatry, doi:10.1038/s41380-020-00880-7
Wang, Wang, Davis, Volkow, Xu, Increased risk for COVID-19 breakthrough infection in fully vaccinated patients with substance use disorders in the United States between December 2020 and August 2021, World Psychiatry, doi:10.1002/wps.20921
Zhou, Yang, Chi, Comorbidities and the risk of severe or fatal outcomes associated with coronavirus disease 2019: a systematic review and meta-analysis, Int J Infect Dis, doi:10.1016/j.ijid.2020.07.029
DOI record:
{
"DOI": "10.1001/jamanetworkopen.2024.17977",
"ISSN": [
"2574-3805"
],
"URL": "http://dx.doi.org/10.1001/jamanetworkopen.2024.17977",
"abstract": "<jats:sec id=\"ab-zoi240587-4\"><jats:title>Importance</jats:title><jats:p>It is unclear whether cannabis use is associated with adverse health outcomes in patients with COVID-19 when accounting for known risk factors, including tobacco use.</jats:p></jats:sec><jats:sec id=\"ab-zoi240587-5\"><jats:title>Objective</jats:title><jats:p>To examine whether cannabis and tobacco use are associated with adverse health outcomes from COVID-19 in the context of other known risk factors.</jats:p></jats:sec><jats:sec id=\"ab-zoi240587-6\"><jats:title>Design, Setting, and Participants</jats:title><jats:p>This retrospective cohort study used electronic health record data from February 1, 2020, to January 31, 2022. This study included patients who were identified as having COVID-19 during at least 1 medical visit at a large academic medical center in the Midwest US.</jats:p></jats:sec><jats:sec id=\"ab-zoi240587-7\"><jats:title>Exposures</jats:title><jats:p>Current cannabis use and tobacco smoking, as documented in the medical encounter.</jats:p></jats:sec><jats:sec id=\"ab-zoi240587-8\"><jats:title>Main Outcomes and Measures</jats:title><jats:p>Health outcomes of hospitalization, intensive care unit (ICU) admission, and all-cause mortality following COVID-19 infection. The association between substance use (cannabis and tobacco) and these COVID-19 outcomes was assessed using multivariable modeling.</jats:p></jats:sec><jats:sec id=\"ab-zoi240587-9\"><jats:title>Results</jats:title><jats:p>A total of 72 501 patients with COVID-19 were included (mean [SD] age, 48.9 [19.3] years; 43 315 [59.7%] female; 9710 [13.4%] had current smoking; 17 654 [24.4%] had former smoking; and 7060 [9.7%] had current use of cannabis). Current tobacco smoking was significantly associated with increased risk of hospitalization (odds ratio [OR], 1.72; 95% CI, 1.62-1.82; <jats:italic>P</jats:italic> &amp;lt; .001), ICU admission (OR, 1.22; 95% CI, 1.10-1.34; <jats:italic>P</jats:italic> &amp;lt; .001), and all-cause mortality (OR, 1.37, 95% CI, 1.20-1.57; <jats:italic>P</jats:italic> &amp;lt; .001) after adjusting for other factors. Cannabis use was significantly associated with increased risk of hospitalization (OR, 1.80; 95% CI, 1.68-1.93; <jats:italic>P</jats:italic> &amp;lt; .001) and ICU admission (OR, 1.27; 95% CI, 1.14-1.41; <jats:italic>P</jats:italic> &amp;lt; .001) but not with all-cause mortality (OR, 0.97; 95% CI, 0.82-1.14, <jats:italic>P</jats:italic> = .69) after adjusting for tobacco smoking, vaccination, comorbidity, diagnosis date, and demographic factors.</jats:p></jats:sec><jats:sec id=\"ab-zoi240587-10\"><jats:title>Conclusions and Relevance</jats:title><jats:p>The findings of this cohort study suggest that cannabis use may be an independent risk factor for COVID-19–related complications, even after considering cigarette smoking, vaccination status, comorbidities, and other risk factors.</jats:p></jats:sec>",
"author": [
{
"affiliation": [
{
"name": "Washington University School of Medicine, St Louis, Missouri"
}
],
"family": "Griffith",
"given": "Nicholas B.",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Center for Tobacco Research and Intervention, School of Medicine and Public Health, University of Wisconsin, Madison"
}
],
"family": "Baker",
"given": "Timothy B.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Cardiothoracic Surgery, Department of Surgery, Washington University School of Medicine, St Louis, Missouri"
},
{
"name": "Division of Public Health Sciences, Department of Surgery, Washington University School of Medicine, St Louis, Missouri"
}
],
"family": "Heiden",
"given": "Brendan T.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Psychiatry, Washington University School of Medicine, St Louis, Missouri"
}
],
"family": "Smock",
"given": "Nina",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Psychiatry, Washington University School of Medicine, St Louis, Missouri"
}
],
"family": "Pham",
"given": "Giang",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Psychiatry, Washington University School of Medicine, St Louis, Missouri"
}
],
"family": "Chen",
"given": "Jingling",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Washington University School of Medicine, St Louis, Missouri"
}
],
"family": "Yu",
"given": "Justin",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Psychiatry, Washington University School of Medicine, St Louis, Missouri"
}
],
"family": "Reddy",
"given": "James",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Washington University School of Medicine, St Louis, Missouri"
}
],
"family": "Lai",
"given": "Albert M.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Washington University School of Medicine, St Louis, Missouri"
}
],
"family": "Hogue",
"given": "Eric",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Psychiatry, Washington University School of Medicine, St Louis, Missouri"
}
],
"family": "Bierut",
"given": "Laura J.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Psychiatry, Washington University School of Medicine, St Louis, Missouri"
},
{
"name": "Alvin J. Siteman Cancer Center at Barnes-Jewish Hospital, Washington University School of Medicine, St Louis, Missouri"
}
],
"family": "Chen",
"given": "Li-Shiun",
"sequence": "additional"
}
],
"container-title": "JAMA Network Open",
"container-title-short": "JAMA Netw Open",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
6,
21
]
],
"date-time": "2024-06-21T15:34:21Z",
"timestamp": 1718984061000
},
"deposited": {
"date-parts": [
[
2024,
6,
21
]
],
"date-time": "2024-06-21T15:34:26Z",
"timestamp": 1718984066000
},
"indexed": {
"date-parts": [
[
2024,
6,
22
]
],
"date-time": "2024-06-22T00:25:33Z",
"timestamp": 1719015933097
},
"is-referenced-by-count": 0,
"issue": "6",
"issued": {
"date-parts": [
[
2024,
6,
21
]
]
},
"journal-issue": {
"issue": "6",
"published-print": {
"date-parts": [
[
2024,
6,
3
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://jamanetwork.com/journals/jamanetworkopen/articlepdf/2820235/griffith_2024_oi_240587_1718143972.13933.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "10",
"original-title": [],
"page": "e2417977",
"prefix": "10.1001",
"published": {
"date-parts": [
[
2024,
6,
21
]
]
},
"published-online": {
"date-parts": [
[
2024,
6,
21
]
]
},
"publisher": "American Medical Association (AMA)",
"reference": [
{
"DOI": "10.1016/j.ijid.2020.07.029",
"article-title": "Comorbidities and the risk of severe or fatal outcomes associated with coronavirus disease 2019: a systematic review and meta-analysis.",
"author": "Zhou",
"doi-asserted-by": "publisher",
"first-page": "47",
"journal-title": "Int J Infect Dis",
"key": "zoi240587r2",
"volume": "99",
"year": "2020"
},
{
"DOI": "10.7189/jogh.11.10001",
"article-title": "Risk factors for poor outcomes in hospitalised COVID-19 patients: a systematic review and meta-analysis.",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "10001",
"journal-title": "J Glob Health",
"key": "zoi240587r3",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1111/add.v116.6",
"article-title": "The association of smoking status with SARS-CoV-2 infection, hospitalization and mortality from COVID-19: a living rapid evidence review with bayesian meta-analyses (version 7).",
"author": "Simons",
"doi-asserted-by": "publisher",
"first-page": "1319",
"issue": "6",
"journal-title": "Addiction",
"key": "zoi240587r4",
"volume": "116",
"year": "2021"
},
{
"DOI": "10.1136/thoraxjnl-2020-216422",
"article-title": "Current smoking and COVID-19 risk: results from a population symptom app in over 2.4 million people.",
"author": "Hopkinson",
"doi-asserted-by": "publisher",
"first-page": "714",
"issue": "7",
"journal-title": "Thorax",
"key": "zoi240587r5",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.3389/fmed.2021.668995",
"article-title": "Lower rate of daily smokers with symptomatic COVID-19: a monocentric self-report of smoking habit study.",
"author": "Miyara",
"doi-asserted-by": "publisher",
"journal-title": "Front Med (Lausanne)",
"key": "zoi240587r6",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.1186/s13722-021-00214-0",
"article-title": "Multiple clinical risks for cannabis users during the COVID-19 pandemic.",
"author": "Borgonhi",
"doi-asserted-by": "publisher",
"first-page": "5",
"issue": "1",
"journal-title": "Addict Sci Clin Pract",
"key": "zoi240587r7",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1001/jamainternmed.2020.8360",
"article-title": "Association of smoking and cumulative pack-year exposure with COVID-19 outcomes in the Cleveland Clinic COVID-19 registry.",
"author": "Lowe",
"doi-asserted-by": "publisher",
"first-page": "709",
"issue": "5",
"journal-title": "JAMA Intern Med",
"key": "zoi240587r8",
"volume": "181",
"year": "2021"
},
{
"DOI": "10.1093/ntr/ntaa082",
"article-title": "Smoking is associated with COVID-19 progression: a meta-analysis.",
"author": "Patanavanich",
"doi-asserted-by": "publisher",
"first-page": "1653",
"issue": "9",
"journal-title": "Nicotine Tob Res",
"key": "zoi240587r9",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1111/add.v117.7",
"article-title": "Relationship between high-risk alcohol consumption and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) seroconversion: a prospective sero-epidemiological cohort study among American college students.",
"author": "Kianersi",
"doi-asserted-by": "publisher",
"first-page": "1908",
"issue": "7",
"journal-title": "Addiction",
"key": "zoi240587r10",
"volume": "117",
"year": "2022"
},
{
"DOI": "10.1002/wps.v21.1",
"article-title": "Increased risk for COVID-19 breakthrough infection in fully vaccinated patients with substance use disorders in the United States between December 2020 and August 2021.",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "124",
"issue": "1",
"journal-title": "World Psychiatry",
"key": "zoi240587r11",
"volume": "21",
"year": "2022"
},
{
"DOI": "10.1038/s41380-020-00880-7",
"article-title": "COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States.",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "30",
"issue": "1",
"journal-title": "Mol Psychiatry",
"key": "zoi240587r12",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.3389/fpubh.2022.829715",
"article-title": "Cannabis use is associated with lower COVID-19 susceptibility but poorer survival.",
"author": "Huang",
"doi-asserted-by": "publisher",
"journal-title": "Front Public Health",
"key": "zoi240587r13",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1186/s42238-022-00152-x",
"article-title": "Cannabis consumption is associated with lower COVID-19 severity among hospitalized patients: a retrospective cohort analysis.",
"author": "Shover",
"doi-asserted-by": "publisher",
"first-page": "46",
"issue": "1",
"journal-title": "J Cannabis Res",
"key": "zoi240587r14",
"volume": "4",
"year": "2022"
},
{
"DOI": "10.1056/NEJMp1813913",
"article-title": "Addressing a core gap in cancer care—the NCI Moonshot Program to help oncology patients stop smoking.",
"author": "Croyle",
"doi-asserted-by": "publisher",
"first-page": "512",
"issue": "6",
"journal-title": "N Engl J Med",
"key": "zoi240587r15",
"volume": "380",
"year": "2019"
},
{
"DOI": "10.1136/bmj.39335.541782.AD",
"article-title": "Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies.",
"author": "von Elm",
"doi-asserted-by": "publisher",
"first-page": "806",
"issue": "7624",
"journal-title": "BMJ",
"key": "zoi240587r16",
"volume": "335",
"year": "2007"
},
{
"DOI": "10.1158/1940-6207.CAPR-21-0105",
"article-title": "Assessing electronic nicotine delivery systems use at NCI-designated cancer centers in the Cancer Moonshot-Funded Cancer Center Cessation Initiative.",
"author": "D’Angelo",
"doi-asserted-by": "publisher",
"first-page": "763",
"issue": "8",
"journal-title": "Cancer Prev Res (Phila)",
"key": "zoi240587r17",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1183/13993003.00688-2020",
"article-title": "ACE-2 expression in the small airway epithelia of smokers and COPD patients: implications for COVID-19.",
"author": "Leung",
"doi-asserted-by": "publisher",
"issue": "5",
"journal-title": "Eur Respir J",
"key": "zoi240587r21",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.1126/sciadv.abi6110",
"article-title": "Cannabidiol inhibits SARS-CoV-2 replication through induction of the host ER stress and innate immune responses.",
"author": "Nguyen",
"doi-asserted-by": "publisher",
"issue": "8",
"journal-title": "Sci Adv",
"key": "zoi240587r22",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.1038/s41467-020-19478-2",
"article-title": "Collider bias undermines our understanding of COVID-19 disease risk and severity.",
"author": "Griffith",
"doi-asserted-by": "publisher",
"first-page": "5749",
"issue": "1",
"journal-title": "Nat Commun",
"key": "zoi240587r23",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.jadohealth.2020.07.002",
"article-title": "Association between youth smoking, electronic cigarette use, and COVID-19.",
"author": "Gaiha",
"doi-asserted-by": "publisher",
"first-page": "519",
"issue": "4",
"journal-title": "J Adolesc Health",
"key": "zoi240587r24",
"volume": "67",
"year": "2020"
},
{
"DOI": "10.3390/ijerph17249189",
"article-title": "Alcohol consumption during the COVID-19 Pandemic: a cross-sectional survey of US adults.",
"author": "Grossman",
"doi-asserted-by": "publisher",
"first-page": "9189",
"issue": "24",
"journal-title": "Int J Environ Res Public Health",
"key": "zoi240587r25",
"volume": "17",
"year": "2020"
},
{
"key": "zoi240587r1",
"unstructured": "US Centers for Disease Control and Prevention. COVID data tracker. Accessed February 22, 2022. https://covid.cdc.gov/covid-data-tracker"
},
{
"key": "zoi240587r18",
"unstructured": "Tegria. Accessed May 14, 2024. https://tegria.com/bluetree-is-now-tegria"
},
{
"key": "zoi240587r19",
"unstructured": "US Centers for Disease Control and Prevention. Underlying medical conditions associated with higher risk for severe COVID-19: information for healthcare professionals. Accessed February 22, 2022. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html"
},
{
"key": "zoi240587r20",
"unstructured": "Vogel? M. Data and methods around reference values in pediatrics. Accessed October 12, 2022. https://cran.r-project.org/web/packages/childsds/childsds.pdf"
}
],
"reference-count": 25,
"references-count": 25,
"relation": {},
"resource": {
"primary": {
"URL": "https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2820235"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Cannabis, Tobacco Use, and COVID-19 Outcomes",
"type": "journal-article",
"volume": "7"
}