Clinical characteristics of hospitalised patients with COVID-19 and the impact on mortality: a single-network, retrospective cohort study from Pennsylvania state
et al., BMJ Open, doi:10.1136/bmjopen-2020-042549, Apr 2021
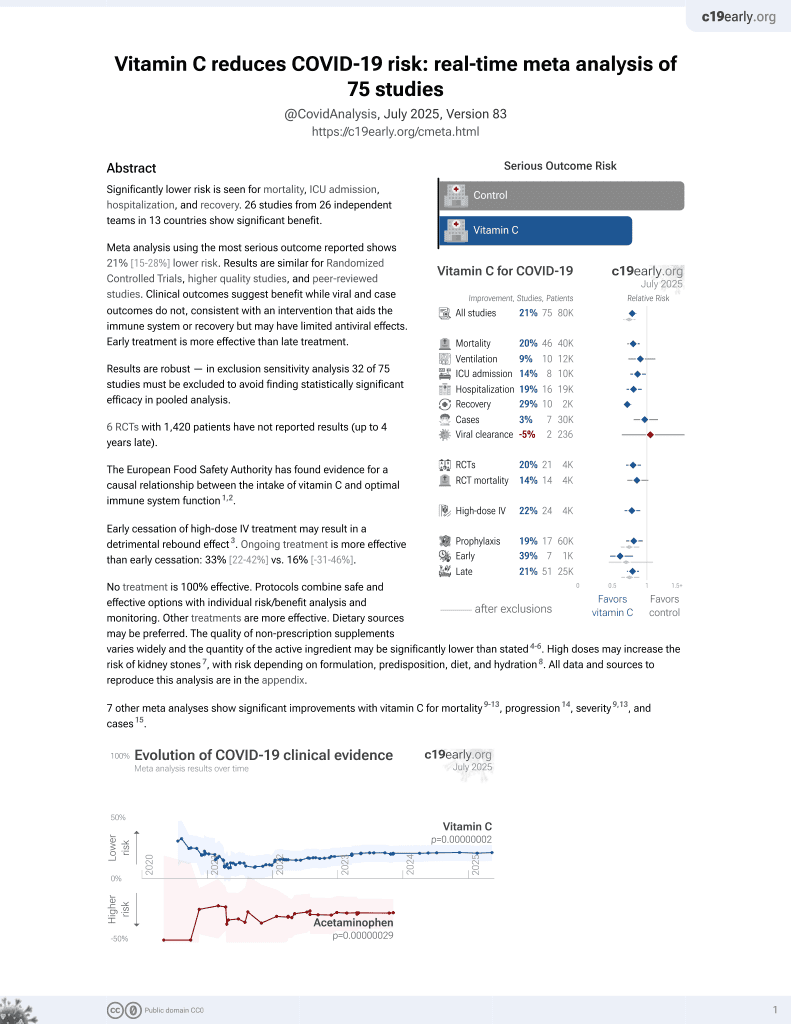
Vitamin C for COVID-19
6th treatment shown to reduce risk in
September 2020, now with p = 0.000000076 from 73 studies, recognized in 22 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
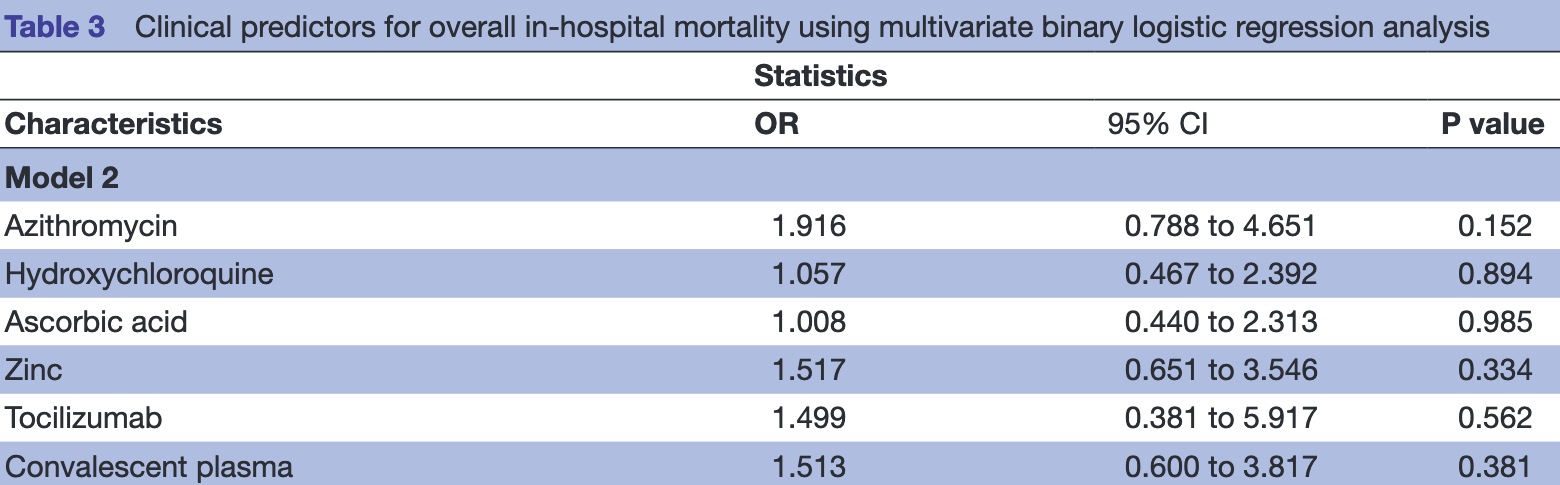
Retrospective 283 patients in the USA showing higher mortality with all treatments (not statistically significant). Confounding by indication is likely. In the supplementary appendix, authors note that the treatments were usually given for patients that required oxygen therapy. Oxygen therapy and ICU admission (possibly, the paper includes ICU admission for model 2 in some places but not others) were the only variables indicating severity used in adjustments.
This is the 19th of 73 COVID-19 controlled studies for vitamin C, which collectively show efficacy with p=0.000000076.
20 studies are RCTs, which show efficacy with p=0.0016.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
This study is excluded in the after exclusion results of meta-analysis:
substantial unadjusted confounding by indication likely.
|
risk of death, 0.7% higher, RR 1.01, p = 0.98, treatment 19 of 55 (34.5%), control 36 of 226 (15.9%), adjusted per study, odds ratio converted to relative risk, multivariate logistic regression.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Gadhiya et al., 8 Apr 2021, retrospective, USA, peer-reviewed, 4 authors, dosage not specified.
Clinical characteristics of hospitalised patients with COVID-19 and the impact on mortality: a single-network, retrospective cohort study from Pennsylvania state
BMJ Open, doi:10.1136/bmjopen-2020-042549
Objective COVID-19 is a respiratory disease caused by SARS-CoV-2 with the highest burden in the USA. Data on clinical characteristics of patients with COVID-19 in US population are limited. Thus, we aim to determine the clinical characteristics and risk factors for in-hospital mortality from COVID-19. Design Retrospective observational study. Setting Single-network hospitals in Pennsylvania state. Participants Patients with confirmed SARS-CoV-2 infection who were hospitalised from 1 March to 31 May 2020. Primary and secondary outcome measures Primary outcome was in-hospital mortality. Secondary outcomes were complications, such as acute kidney injury (AKI) and acute respiratory distress syndrome (ARDS). Results Of 283 patients, 19.4% were non-survivors. The mean age of all patients was 64.1±15.9 years. 56.2% were male and 50.2% were white. Several factors were identified from our adjusted multivariate analyses to be associated with in-hospital mortality: increasing age (per 1-year increment; OR 1.07 (1.045 to 1.105)), hypoxia (oxygen saturation <95%; OR 4.630 (1.934 to 1.111)), opacity/infiltrate on imaging (OR 3.077 (1.276 to 7.407)), leucocytosis (white blood cell >10 109/µL ; OR 2.732 (1.412 to 5.263)), ferritin >336 ng/mL (OR 4.016 (1.195 to 13.514)), lactate dehydrogenase >200 U/L (OR 7.752 (1.639 to 37.037)), procalcitonin >0.25 ng/ mL (OR 2.404 (1.011 to 5.714)), troponin I >0.03 ng/ mL (OR 2.242 (1.080 to 4.673)), need for advanced oxygen support other than simple nasal cannula (OR 4.608-13.889 (2.053 to 31.250)), intensive care unit admission/transfer (OR 13.699 (6.135 to 30.303)), renal replacement therapy (OR 21.277 (5.025 to 90.909)), need for vasopressor (OR 22.222 (9.434 to 52.632)), ARDS (OR 23.810 (10.204 to 55.556)), respiratory acidosis (OR 7.042 (2.915 to 16.949)), and AKI (OR 3.571 (1.715 to 7.407)). When critically ill patients were analysed independently, increasing Sequential Organ Failure Assessment score (OR 1.544 (1.168 to 2.039)), AKI (OR 2.128 (1.111 to 6.667)) and ARDS (OR 6.410 (2.237 to 18.182)) were predictive of in-hospital mortality. Conclusion We reported the characteristics of ethnically diverse, hospitalised patients with COVID-19 from Pennsylvania state.
Competing interests None declared. Patient consent for publication Not required.
Ethics approval The protocol of this study has been approved by the UPMC Pinnacle Institutional Review Board and UPMC Pinnacle Ethics Committee (#20E024). Provenance and peer review Not commissioned; externally peer reviewed. Data availability statement Data are available upon reasonable request. Raw data are available upon reasonable request. Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise. Open access This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is..
References
-Y, Hu, Clinical characteristics of coronavirus disease 2019 in China, New England Journal of Medicine
Alattar, Ibrahim, Shaar, Tocilizumab for the treatment of severe coronavirus disease 2019, J Med Virol
Annane, Pastores, Rochwerg, Guidelines for the diagnosis and management of critical illness-related corticosteroid insufficiency (CIRCI) in critically ill patients (Part I): Society of critical care medicine (SCCM) and European Society of intensive care medicine (ESICM) 2017, Crit Care Med, doi:10.1097/CCM.0000000000002737
Annetta, Maviglia, Proietti, Use of corticosteroids in critically ill septic patients : a review of mechanisms of adrenal insufficiency in sepsis and treatment, Curr Drug Targets, doi:10.2174/138945009789108792
Arentz, Yim, Klaff, Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state, JAMA, doi:10.1001/jama.2020.4326
Beigel, Tomashek, Dodd, Remdesivir for the treatment of Covid-19 -final report, N Engl J Med, doi:10.1056/NEJMoa2007764
Bhimraj, Morgan, Shumaker, Infectious diseases Society of America guidelines on the treatment and management of patients with COVID-19, Clin Infect Dis
Biot, Daher, Chavain, Design and synthesis of hydroxyferroquine derivatives with antimalarial and antiviral activities, J Med Chem, doi:10.1021/jm0601856
Caly, Druce, Catton, The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro, Antiviral Res, doi:10.1016/j.antiviral.2020.104787
Campochiaro, Della-Torre, Cavalli, Efficacy and safety of tocilizumab in severe COVID-19 patients: a single-centre retrospective cohort study, Eur J Intern Med, doi:10.1016/j.ejim.2020.05.021
Cavalcanti, Zampieri, Rosa, Hydroxychloroquine with or without azithromycin in mild-to-moderate Covid-19, N Engl J Med Overseas Ed, doi:10.1056/NEJMoa2019014
Cheng, Luo, Wang, Kidney disease is associated with in-hospital death of patients with COVID-19, Kidney Int, doi:10.1016/j.kint.2020.03.005
Colafrancesco, Alessandri, Conti, COVID-19 gone bad: a new character in the spectrum of the hyperferritinemic syndrome?, Autoimmun Rev, doi:10.1016/j.autrev.2020.102573
Combes, Costa, Trouillet, Morbidity, mortality, and quality-of-life outcomes of patients requiring >or=14 days of mechanical ventilation, Crit Care Med, doi:10.1097/01.CCM.0000065188.87029.C3
Elseviers, Lins, Van Der Niepen, Renal replacement therapy is an independent risk factor for mortality in critically ill patients with acute kidney injury, Crit Care, doi:10.1186/cc9355
Ferguson, Camporota, The Berlin definition of ARDS: an expanded rationale, Justification, and supplementary material, Intensive Care Med, doi:10.1007/s00134-012-2682-1
Ferreira, Bota, Bross, Serial evaluation of the SOFA score to predict outcome in critically ill patients, JAMA, doi:10.1001/jama.286.14.1754
Fowler, Truwit, Hite, Effect of vitamin C infusion on organ failure and biomarkers of inflammation and vascular injury in patients with sepsis and severe acute respiratory failure: the CITRIS-ALI randomized clinical trial, JAMA, doi:10.1001/jama.2019.11825
Gao, Tian, Yang, Breakthrough: chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies, Biosci Trends, doi:10.5582/bst.2020.01047
Gautret, Lagier, Parola, Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an openlabel non-randomized clinical trial, Int J Antimicrob Agents, doi:10.1016/j.ijantimicag.2020.105949
Gautret, Lagier, Parola, Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an openlabel non-randomized clinical trial, Int J Antimicrob Agents, doi:10.1016/j.ijantimicag.2020.105949
Geleris, Sun, Platt, Observational study of hydroxychloroquine in hospitalized patients with Covid-19, N Engl J Med, doi:10.1056/NEJMoa2012410
Gustot, Multiple organ failure in sepsis: prognosis and role of systemic inflammatory, Curr Opin Crit Care, doi:10.1097/MCC.0b013e328344b446
Hazra, Using the confidence interval confidently, J Thorac Dis, doi:10.21037/jtd.2017.09.14
Jose, Manuel, COVID-19 cytokine storm: the interplay between inflammation and coagulation, Lancet Respir Med, doi:10.1016/S2213-2600(20)30216-2
José, Williams, Chambers, Proteinase-Activated receptors in fibroproliferative lung disease, Thorax, doi:10.1136/thoraxjnl-2013-204367
Joyner, Wright, Fairweather, Early safety indicators of COVID-19 convalescent plasma in 5,000 patients, medRxiv, doi:10.1101/2020.05.12.20099879
Khwaja, KDIGO clinical practice guidelines for acute kidney injury, Nephron Clin Pract, doi:10.1159/000339789
Kiabi, Alipour, Darvishi-Khezri, Zinc supplementation in adult mechanically ventilated trauma patients is associated with decreased occurrence of ventilator-associated pneumonia: a secondary analysis of a prospective, observational study, Indian J Crit Care Med, doi:10.4103/0972-5229.198324
Levey, Stevens, Schmid, A new equation to estimate glomerular filtration rate, Ann Intern Med, doi:10.7326/0003-4819-150-9-200905050-00006
Li, Han, Woodward, The impact of 2019 novel coronavirus on heart injury: a systematic review and meta-analysis
Li, Xu, Yu, Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan, J Allergy Clin Immunol
Luo, Liu, Qiu, Tocilizumab treatment in COVID-19: a single center experience, J Med Virol, doi:10.1002/jmv.25801
Martin, Viviand, Leone, Effect of norepinephrine on the outcome of septic shock, Crit Care Med, doi:10.1097/00003246-200008000-00012
Meduri, Kohler, Headley, Inflammatory cytokines in the BAL of patients with ARDS. persistent elevation over time predicts poor outcome, Chest, doi:10.1378/chest.108.5.1303
Morris, Cleary, Clarke, Secondary bacterial infections associated with influenza pandemics, Front Microbiol, doi:10.3389/fmicb.2017.01041
Myers, Parodi, Escobar, Characteristics of hospitalized adults with COVID-19 in an integrated health care system in California, JAMA, doi:10.1001/jama.2020.7202
Rh, Liang, Yang, Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study, Eur Respir J
Richardson, Hirsch, Narasimhan, Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the new York City area, JAMA, doi:10.1001/jama.2020.6775
Ruocco, Cechinatti, Barbosa, Zinc and selenium status in critically ill patients according to severity stratification, Nutrition, doi:10.1016/j.nut.2017.07.009
Salazar, Perez, Ashraf, Treatment of coronavirus disease 2019 (COVID-19) patients with convalescent plasma, Am J Pathol
Scaroni, Armigliato, Cannavò, COVID-19 outbreak and steroids administration: are patients treated for Sars-Cov-2 at risk of adrenal insufficiency?, J Endocrinol Invest, doi:10.1007/s40618-020-01253-1
Tisoncik, Korth, Simmons, Into the eye of the cytokine storm, Microbiol Mol Biol Rev, doi:10.1128/MMBR.05015-11
Van Smeden, De Groot, Moons, No rationale for 1 variable per 10 events criterion for binary logistic regression analysis, BMC Med Res Methodol, doi:10.1186/s12874-016-0267-3
Velthuis, Van Den Worm, She, Sims, Zn(2+) inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture, PLoS Pathog, doi:10.1371/journal.ppat.1001176
Vittinghoff, Mcculloch, Relaxing the rule of ten events per variable in logistic and COX regression, Am J Epidemiol, doi:10.1093/aje/kwk052
Vrsalovic, Presecki, Cardiac troponins predict mortality in patients with COVID-19: a meta-analysis of adjusted risk estimates, J Infect, doi:10.1016/j.jinf.2020.05.022
Wang, Calfee, Paul, One-Year mortality and predictors of death among hospital survivors of acute respiratory distress syndrome, Intensive Care Med, doi:10.1007/s00134-013-3186-3
Zhang, Jativa, Vitamin C supplementation in the critically ill: a systematic review and meta-analysis, SAGE Open Med, doi:10.1177/2050312118807615
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
DOI record:
{
"DOI": "10.1136/bmjopen-2020-042549",
"ISSN": [
"2044-6055",
"2044-6055"
],
"URL": "http://dx.doi.org/10.1136/bmjopen-2020-042549",
"abstract": "<jats:sec><jats:title>Objective</jats:title><jats:p>COVID-19 is a respiratory disease caused by SARS-CoV-2 with the highest burden in the USA. Data on clinical characteristics of patients with COVID-19 in US population are limited. Thus, we aim to determine the clinical characteristics and risk factors for in-hospital mortality from COVID-19.</jats:p></jats:sec><jats:sec><jats:title>Design</jats:title><jats:p>Retrospective observational study.</jats:p></jats:sec><jats:sec><jats:title>Setting</jats:title><jats:p>Single-network hospitals in Pennsylvania state.</jats:p></jats:sec><jats:sec><jats:title>Participants</jats:title><jats:p>Patients with confirmed SARS-CoV-2 infection who were hospitalised from 1 March to 31 May 2020.</jats:p></jats:sec><jats:sec><jats:title>Primary and secondary outcome measures</jats:title><jats:p>Primary outcome was in-hospital mortality. Secondary outcomes were complications, such as acute kidney injury (AKI) and acute respiratory distress syndrome (ARDS).</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Of 283 patients, 19.4% were non-survivors. The mean age of all patients was 64.1±15.9 years. 56.2% were male and 50.2% were white. Several factors were identified from our adjusted multivariate analyses to be associated with in-hospital mortality: increasing age (per 1-year increment; OR 1.07 (1.045 to 1.105)), hypoxia (oxygen saturation <95%; OR 4.630 (1.934 to 1.111)), opacity/infiltrate on imaging (OR 3.077 (1.276 to 7.407)), leucocytosis (white blood cell >10<jats:sup>109/µL</jats:sup>; OR 2.732 (1.412 to 5.263)), ferritin >336 ng/mL (OR 4.016 (1.195 to 13.514)), lactate dehydrogenase >200 U/L (OR 7.752 (1.639 to 37.037)), procalcitonin >0.25 ng/mL (OR 2.404 (1.011 to 5.714)), troponin I >0.03 ng/mL (OR 2.242 (1.080 to 4.673)), need for advanced oxygen support other than simple nasal cannula (OR 4.608–13.889 (2.053 to 31.250)), intensive care unit admission/transfer (OR 13.699 (6.135 to 30.303)), renal replacement therapy (OR 21.277 (5.025 to 90.909)), need for vasopressor (OR 22.222 (9.434 to 52.632)), ARDS (OR 23.810 (10.204 to 55.556)), respiratory acidosis (OR 7.042 (2.915 to 16.949)), and AKI (OR 3.571 (1.715 to 7.407)). When critically ill patients were analysed independently, increasing Sequential Organ Failure Assessment score (OR 1.544 (1.168 to 2.039)), AKI (OR 2.128 (1.111 to 6.667)) and ARDS (OR 6.410 (2.237 to 18.182)) were predictive of in-hospital mortality.</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>We reported the characteristics of ethnically diverse, hospitalised patients with COVID-19 from Pennsylvania state.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/bmjopen-2020-042549"
],
"author": [
{
"affiliation": [],
"family": "Gadhiya",
"given": "Kinjal P",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-5041-4290",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hansrivijit",
"given": "Panupong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gangireddy",
"given": "Mounika",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Goldman",
"given": "John D",
"sequence": "additional"
}
],
"clinical-trial-number": [
{
"clinical-trial-number": "nct04264533",
"registry": "10.18810/clinical-trials-gov"
},
{
"clinical-trial-number": "nct04317092",
"registry": "10.18810/clinical-trials-gov"
},
{
"clinical-trial-number": "nct04320615",
"registry": "10.18810/clinical-trials-gov"
},
{
"clinical-trial-number": "nct04342182",
"registry": "10.18810/clinical-trials-gov"
}
],
"container-title": "BMJ Open",
"container-title-short": "BMJ Open",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2021,
4,
9
]
],
"date-time": "2021-04-09T02:05:52Z",
"timestamp": 1617933952000
},
"deposited": {
"date-parts": [
[
2022,
12,
23
]
],
"date-time": "2022-12-23T21:14:52Z",
"timestamp": 1671830092000
},
"indexed": {
"date-parts": [
[
2024,
3,
19
]
],
"date-time": "2024-03-19T11:09:16Z",
"timestamp": 1710846556414
},
"is-referenced-by-count": 6,
"issue": "4",
"issued": {
"date-parts": [
[
2021,
4
]
]
},
"journal-issue": {
"issue": "4",
"published-online": {
"date-parts": [
[
2021,
4,
8
]
]
},
"published-print": {
"date-parts": [
[
2021,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 6,
"start": {
"date-parts": [
[
2021,
4,
7
]
],
"date-time": "2021-04-07T00:00:00Z",
"timestamp": 1617753600000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjopen-2020-042549",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "e042549",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2021,
4
]
]
},
"published-online": {
"date-parts": [
[
2021,
4,
8
]
]
},
"published-print": {
"date-parts": [
[
2021,
4
]
]
},
"publisher": "BMJ",
"reference": [
{
"key": "2021040819050964000_11.4.e042549.1",
"unstructured": "WHO . Coronavirus disease (COVID-19) pandemic. Available: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [Accessed 29 Aug 2020]."
},
{
"key": "2021040819050964000_11.4.e042549.2",
"unstructured": "Department of Health . COVID-19 data for Pennsylvania. Available: https://www.health.pa.gov/topics/disease/coronavirus/Pages/Cases.aspx [Accessed 29 Aug 2020]."
},
{
"DOI": "10.1001/jama.2020.4326",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.3"
},
{
"DOI": "10.1001/jama.2020.7202",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.4"
},
{
"DOI": "10.1001/jama.2020.6775",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.5"
},
{
"DOI": "10.1056/NEJMoa2002032",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.6"
},
{
"DOI": "10.1183/13993003.00524-2020",
"doi-asserted-by": "crossref",
"key": "2021040819050964000_11.4.e042549.7",
"unstructured": "RH D , Liang LR , Yang CQ . Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J 2020;55."
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.8"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105949",
"doi-asserted-by": "crossref",
"key": "2021040819050964000_11.4.e042549.9",
"unstructured": "Gautret P , Lagier J-C , Parola P , et al . Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents 2020;56:105949. doi:10.1016/j.ijantimicag.2020.105949"
},
{
"DOI": "10.1001/jama.2019.11825",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.10"
},
{
"DOI": "10.1016/j.antiviral.2020.104787",
"article-title": "The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro",
"author": "Caly",
"doi-asserted-by": "crossref",
"journal-title": "Antiviral Res",
"key": "2021040819050964000_11.4.e042549.11",
"volume": "178",
"year": "2020"
},
{
"DOI": "10.1371/journal.ppat.1001176",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.12"
},
{
"DOI": "10.1001/jama.286.14.1754",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.13"
},
{
"DOI": "10.7326/0003-4819-150-9-200905050-00006",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.14"
},
{
"DOI": "10.1159/000339789",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.15"
},
{
"article-title": "KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney Disease-Mineral and bone disorder (CKD-MBD)",
"first-page": "S1",
"journal-title": "Kidney Int Suppl",
"key": "2021040819050964000_11.4.e042549.16",
"volume": "113",
"year": "2009"
},
{
"DOI": "10.1007/s00134-012-2682-1",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.17"
},
{
"DOI": "10.21037/jtd.2017.09.14",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.18"
},
{
"DOI": "10.1016/j.kint.2020.03.005",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.19"
},
{
"DOI": "10.1016/j.jaci.2020.04.006",
"doi-asserted-by": "crossref",
"key": "2021040819050964000_11.4.e042549.20",
"unstructured": "Li X , Xu S , Yu M . Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol 2020."
},
{
"DOI": "10.1097/MCC.0b013e328344b446",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.21"
},
{
"DOI": "10.1186/cc9355",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.22"
},
{
"DOI": "10.1097/00003246-200008000-00012",
"article-title": "Effect of norepinephrine on the outcome of septic shock",
"author": "Martin",
"doi-asserted-by": "crossref",
"first-page": "2758",
"journal-title": "Crit Care Med",
"key": "2021040819050964000_11.4.e042549.23",
"volume": "28",
"year": "2000"
},
{
"DOI": "10.1007/s00134-013-3186-3",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.24"
},
{
"DOI": "10.1097/01.CCM.0000065188.87029.C3",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.25"
},
{
"DOI": "10.1016/j.pcad.2020.04.008",
"article-title": "The impact of 2019 novel coronavirus on heart injury: a systematic review and meta-analysis",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "518",
"journal-title": "Prog Cardiovasc Dis",
"key": "2021040819050964000_11.4.e042549.26",
"volume": "63",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30216-2",
"article-title": "COVID-19 cytokine storm: the interplay between inflammation and coagulation",
"author": "Jose",
"doi-asserted-by": "crossref",
"first-page": "e46",
"journal-title": "Lancet Respir Med",
"key": "2021040819050964000_11.4.e042549.27",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1097/CCM.0000000000002737",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.28"
},
{
"DOI": "10.3389/fmicb.2017.01041",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.29"
},
{
"DOI": "10.1016/j.jinf.2020.05.022",
"article-title": "Cardiac troponins predict mortality in patients with COVID-19: a meta-analysis of adjusted risk estimates",
"author": "Vrsalovic",
"doi-asserted-by": "crossref",
"first-page": "e99",
"journal-title": "J Infect",
"key": "2021040819050964000_11.4.e042549.30",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.1128/MMBR.05015-11",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.31"
},
{
"DOI": "10.1378/chest.108.5.1303",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.32"
},
{
"DOI": "10.1136/thoraxjnl-2013-204367",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.33"
},
{
"DOI": "10.1016/j.autrev.2020.102573",
"article-title": "COVID-19 gone bad: a new character in the spectrum of the hyperferritinemic syndrome?",
"author": "Colafrancesco",
"doi-asserted-by": "crossref",
"journal-title": "Autoimmun Rev",
"key": "2021040819050964000_11.4.e042549.34",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1021/jm0601856",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.35"
},
{
"DOI": "10.5582/bst.2020.01047",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.36"
},
{
"key": "2021040819050964000_11.4.e042549.37"
},
{
"DOI": "10.1056/NEJMoa2012410",
"article-title": "Observational study of hydroxychloroquine in hospitalized patients with Covid-19",
"author": "Geleris",
"doi-asserted-by": "crossref",
"first-page": "2411",
"journal-title": "N Engl J Med",
"key": "2021040819050964000_11.4.e042549.38",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2019014",
"article-title": "Hydroxychloroquine with or without azithromycin in mild-to-moderate Covid-19",
"author": "Cavalcanti",
"doi-asserted-by": "crossref",
"first-page": "2041",
"journal-title": "N Engl J Med Overseas Ed",
"key": "2021040819050964000_11.4.e042549.39",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa478",
"doi-asserted-by": "crossref",
"key": "2021040819050964000_11.4.e042549.40",
"unstructured": "Bhimraj A , Morgan RL , Shumaker AH . Infectious diseases Society of America guidelines on the treatment and management of patients with COVID-19. Clin Infect Dis 2020."
},
{
"DOI": "10.1177/2050312118807615",
"article-title": "Vitamin C supplementation in the critically ill: a systematic review and meta-analysis",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "205031211880761",
"journal-title": "SAGE Open Med",
"key": "2021040819050964000_11.4.e042549.41",
"volume": "6",
"year": "2018"
},
{
"DOI": "10.1016/j.nut.2017.07.009",
"article-title": "Zinc and selenium status in critically ill patients according to severity stratification",
"author": "Cirino Ruocco",
"doi-asserted-by": "crossref",
"first-page": "85",
"journal-title": "Nutrition",
"key": "2021040819050964000_11.4.e042549.42",
"volume": "45",
"year": "2018"
},
{
"DOI": "10.4103/0972-5229.198324",
"article-title": "Zinc supplementation in adult mechanically ventilated trauma patients is associated with decreased occurrence of ventilator-associated pneumonia: a secondary analysis of a prospective, observational study",
"author": "Hasanzadeh Kiabi",
"doi-asserted-by": "crossref",
"first-page": "34",
"journal-title": "Indian J Crit Care Med",
"key": "2021040819050964000_11.4.e042549.43",
"volume": "21",
"year": "2017"
},
{
"DOI": "10.2174/138945009789108792",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.44"
},
{
"DOI": "10.1007/s40618-020-01253-1",
"article-title": "COVID-19 outbreak and steroids administration: are patients treated for Sars-Cov-2 at risk of adrenal insufficiency?",
"author": "Scaroni",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "J Endocrinol Invest",
"key": "2021040819050964000_11.4.e042549.45",
"volume": "43",
"year": "2020"
},
{
"key": "2021040819050964000_11.4.e042549.46",
"unstructured": "Dexamethasone in hospitalized patients with Covid-19 — preliminary report. N Engl J Med 2020."
},
{
"DOI": "10.1056/NEJMoa2007764",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.47"
},
{
"DOI": "10.1002/jmv.25801",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.48"
},
{
"DOI": "10.1002/jmv.25964",
"doi-asserted-by": "crossref",
"key": "2021040819050964000_11.4.e042549.49",
"unstructured": "Alattar R , Ibrahim TBH , Shaar SH . Tocilizumab for the treatment of severe coronavirus disease 2019. J Med Virol 2020."
},
{
"DOI": "10.1016/j.ejim.2020.05.021",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.50"
},
{
"key": "2021040819050964000_11.4.e042549.51",
"unstructured": "Salazar E , Perez KK , Ashraf M . Treatment of coronavirus disease 2019 (COVID-19) patients with convalescent plasma. Am J Pathol 2020."
},
{
"article-title": "Early safety indicators of COVID-19 convalescent plasma in 5,000 patients",
"author": "Joyner",
"journal-title": "medRxiv",
"key": "2021040819050964000_11.4.e042549.52",
"year": "2020"
},
{
"DOI": "10.1093/aje/kwk052",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.53"
},
{
"DOI": "10.1186/s12874-016-0267-3.",
"doi-asserted-by": "publisher",
"key": "2021040819050964000_11.4.e042549.54"
}
],
"reference-count": 54,
"references-count": 54,
"relation": {},
"resource": {
"primary": {
"URL": "https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2020-042549"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Clinical characteristics of hospitalised patients with COVID-19 and the impact on mortality: a single-network, retrospective cohort study from Pennsylvania state",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "11"
}
gadhiya