Effect of common maintenance drugs on the risk and severity of COVID-19 in elderly patients
et al., PLoS ONE, doi:10.1371/journal.pone.0266922, Oct 2021 (preprint)
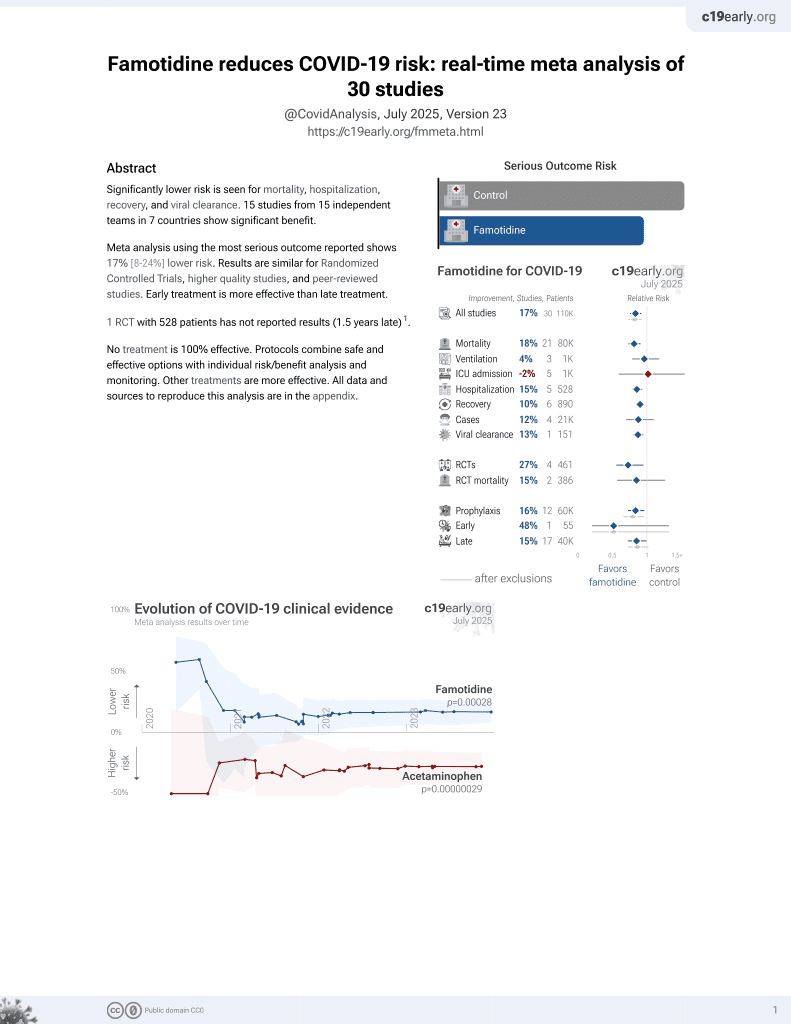
Famotidine for COVID-19
28th treatment shown to reduce risk in
October 2021, now with p = 0.00028 from 30 studies, recognized in 2 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
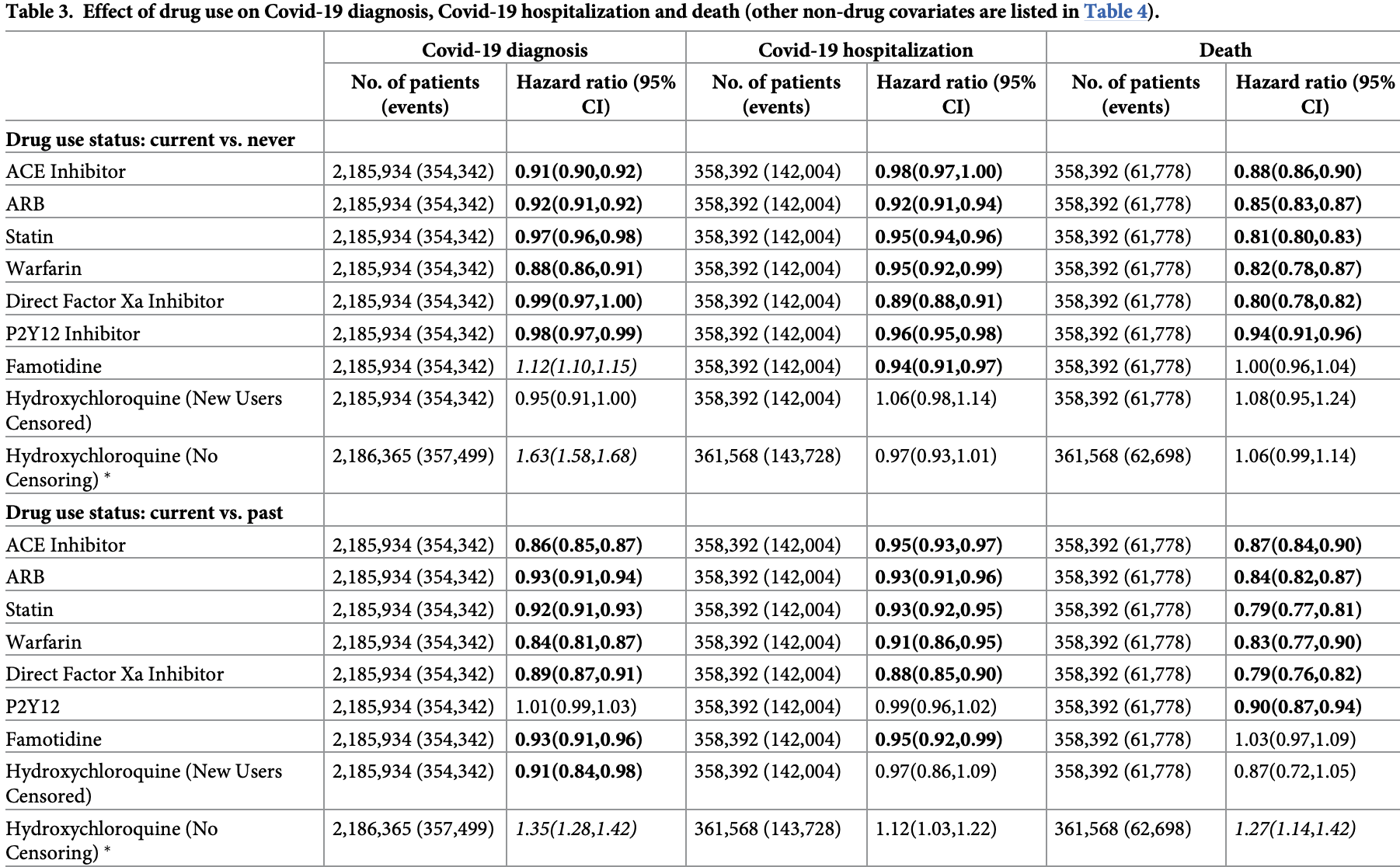
Retrospective database analysis of 374,229 patients in the USA, showing higher cases, lower hospitalizations, and no change in mortality with famotidine use.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
This study is excluded in the after exclusion results of meta-analysis:
not fully adjusting for the different baseline risk of systemic autoimmune patients.
Study covers HCQ and famotidine.
|
risk of death, no change, HR 1.00, p = 1.00, vs. never used.
|
|
risk of hospitalization, 6.0% lower, HR 0.94, p < 0.001, vs. never used.
|
|
risk of case, 12.0% higher, HR 1.12, p < 0.001, vs. never used.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Fung et al., 1 Oct 2021, retrospective, population-based cohort, USA, peer-reviewed, 6 authors.
Effect of common maintenance drugs on the risk and severity of COVID-19 in elderly patients
PLOS ONE, doi:10.1371/journal.pone.0266922
Background Maintenance drugs are used to treat chronic conditions. Several classes of maintenance drugs have attracted attention because of their potential to affect susceptibility to and severity of COVID-19.
Methods Using claims data on 20% random sample of Part D Medicare enrollees from April to December 2020, we identified patients diagnosed with COVID-19. Using a nested case-control design, non-COVID-19 controls were identified by 1:5 matching on age, race, sex, dualeligibility status, and geographical region. We identified usage of angiotensin-converting enzyme inhibitors (ACEI), angiotensin-receptor blockers (ARB), statins, warfarin, direct factor Xa inhibitors, P2Y12 inhibitors, famotidine and hydroxychloroquine based on Medicare prescription claims data. Using extended Cox regression models with time-varying propensity score adjustment we examined the independent effect of each study drug on contracting COVID-19. For severity of COVID-19, we performed extended Cox regressions on all COVID-19 patients, using COVID-19-related hospitalization and all-cause mortality as outcomes. Covariates included gender, age, race, geographic region, low-income indicator, and co-morbidities. To compensate for indication bias related to the use of hydroxychloroquine for the prophylaxis or treatment of COVID-19, we censored patients who only started on hydroxychloroquine in 2020.
Results Up to December 2020, our sample contained 374,229 Medicare patients over 65 who were diagnosed with COVID-19. Among the COVID-19 patients, 278,912 (74.6%) were on at least one study drug. The three most common study drugs among COVID-19 patients were statins 187,374 (50.1%), ACEI 97,843 (26.2%) and ARB 83,290 (22.3%). For all three outcomes (diagnosis, hospitalization and death), current users of ACEI, ARB,
References
Arshad, Treatment with hydroxychloroquine, azithromycin, and combination in patients hospitalized with COVID-19, Int J Infect Dis, doi:10.1016/j.ijid.2020.06.099
Azzato, Prevalent cases in observational studies of cancer survival: do they bias hazard ratio estimates?, Br J Cancer, doi:10.1038/sj.bjc.6605062
Barochiner, Martinez, Use of inhibitors of the renin-angiotensin system in hypertensive patients and COVID-19 severity: A systematic review and meta-analysis, J Clin Pharm Ther, doi:10.1111/jcpt.13246
Bikdeli, COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review, J Am Coll Cardiol, doi:10.1016/j.jacc.2020.04.031
Bourinbaiar, Fruhstorfer, The effect of histamine type 2 receptor antagonists on human immunodeficiency virus (HIV) replication: identification of a new class of antiviral agents, Life Sci, doi:10.1016/s0024-3205%2896%2900553-x
Bozkurt, Kovacs, Harrington, Joint HFSA/ACC/AHA Statement Addresses Concerns Re: Using RAAS Antagonists in COVID-19, J Card Fail, doi:10.1016/j.cardfail.2020.04.013
Csizmadi, Collet, Boivin, Bias and Confounding in Pharmacoepidemiology
Cubeddu, Seamon, Statin withdrawal: clinical implications and molecular mechanisms, Pharmacotherapy, doi:10.1592/phco.26.9.1288
Cui, Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia, J Thromb Haemost, doi:10.1111/jth.14830
Elshafei, RAAS, ACE2 and COVID-19; a mechanistic review, Saudi J Biol Sci, doi:10.1016/j.sjbs.2021.07.003
Ernster, Nested case-control studies, Prev Med, doi:10.1006/pmed.1994.1093
Ferrario, Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2, Hydroxychloroquine (No Censoring) �, doi:10.1161/CIRCULATIONAHA.104.510461
Fontelo, A review of thromboembolic events in hospitalized COVID-19 patients, Thromb J, doi:10.1186/s12959-021-00298-3
Fosbol, Association of Angiotensin-Converting Enzyme Inhibitor or Angiotensin Receptor Blocker Use With COVID-19 Diagnosis and Mortality, JAMA, doi:10.1001/jama.2020.11301
Freedberg, Famotidine Use Is Associated With Improved Clinical Outcomes in Hospitalized COVID-19 Patients: A Propensity Score Matched Retrospective Cohort Study, Gastroenterology, doi:10.1053/j.gastro.2020.05.053
Guo, Zhu, Decreased Mortality of COVID-19 With Renin-Angiotensin-Aldosterone System Inhibitors Therapy in Patients With Hypertension: A Meta-Analysis, Hypertension, doi:10.1161/HYPERTENSIONAHA.120.15572
Health Organization, COVID-19 and the use of angiotensin-converting enzyme inhibitors and receptor blockers-Scientific Brief
Hoffmann, SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor, Cell, doi:10.1016/j.cell.2020.02.052
Inama, Coronavirus disease 2019 infection in patients with recent cardiac surgery: does chronic anticoagulant therapy have a protective effect?, J Cardiovasc Med, doi:10.2459/JCM.0000000000001066
Janowitz, Famotidine use and quantitative symptom tracking for COVID-19 in non-hospitalised patients: a case series, Gut, doi:10.1136/gutjnl-2020-321852
Keyaerts, In vitro inhibition of severe acute respiratory syndrome coronavirus by chloroquine, Biochem Biophys Res Commun, doi:10.1016/j.bbrc.2004.08.085
Klok, Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis, Thromb Res, doi:10.1016/j.thromres.2020.04.041
Li, Association of Renin-Angiotensin System Inhibitors With Severity or Risk of Death in Patients With Hypertension Hospitalized for Coronavirus Disease 2019 (COVID-19) Infection in Wuhan, China, JAMA Cardiol, doi:10.1001/jamacardio.2020.1624
Mancia, Renin-Angiotensin-Aldosterone System Blockers and the Risk of Covid-19, N Engl J Med, doi:10.1056/NEJMoa2006923
Pal, Statin use and clinical outcomes in patients with COVID-19: An updated systematic review and meta-analysis, Postgrad Med J, doi:10.1136/postgradmedj-2020-139172
Pawlos, COVID-19: Direct and Indirect Mechanisms of Statins, Int J Mol Sci, doi:10.3390/ijms22084177
Permana, In-hospital use of statins is associated with a reduced risk of mortality in coronavirus-2019 (COVID-19): systematic review and meta-analysis, Pharmacol Rep, doi:10.1007/s43440-021-00233-3
Pourhoseingholi, Baghestani, Vahedi, How to control confounding effects by statistical analysis, Gastroenterol Hepatol Bed Bench
Reynolds, Renin-Angiotensin-Aldosterone System Inhibitors and Risk of Covid-19, N Engl J Med, doi:10.1056/NEJMoa2008975
Rico-Mesa, The Role of Anticoagulation in COVID-19-Induced Hypercoagulability, Curr Cardiol Rep, doi:10.1007/s11886-020-01328-8
Rodrigues-Diez, Statins: Could an old friend help in the fight against COVID-19?, Br J Pharmacol, doi:10.1111/bph.15166
Rosenbaum, Rubin, The Central Role of the Propensity Score in Observational Studies for Causal Effects, Biometrika
Rossi, Protective role of chronic treatment with direct oral anticoagulants in elderly patients affected by interstitial pneumonia in COVID-19 era, Eur J Intern Med, doi:10.1016/j.ejim.2020.06.006
Russo, Clinical impact of pre-admission antithrombotic therapy in hospitalized patients with COVID-19: A multicenter observational study, Pharmacol Res, doi:10.1016/j.phrs.2020.104965
Sinha, Balayla, Hydroxychloroquine and COVID-19, Postgrad Med J, doi:10.1136/postgradmedj-2020-137785
Sivaloganathan, Ladikou, Chevassut, COVID-19 mortality in patients on anticoagulants and antiplatelet agents, Br J Haematol, doi:10.1111/bjh.16968
Soler, Pharmacologic modulation of ACE2 expression, Curr Hypertens Rep, doi:10.1007/s11906-008-0076-0
Tang, Abnormal coagulation parameters are associated with prognosis in patients with novel coronavirus pneumonia, J Thromb Haemost, doi:10.1111/jth.14768
Tremblay, Impact of anticoagulation prior to COVID-19 infection: a propensity score-matched cohort study, Blood, doi:10.1182/blood.2020006941
Vaduganathan, Renin-Angiotensin-Aldosterone System Inhibitors in Patients with Covid-19, N Engl J Med, doi:10.1056/NEJMsr2005760
Verity, Estimates of the severity of coronavirus disease 2019: a model-based analysis, Lancet Infect Dis, doi:10.1016/S1473-3099%2820%2930243-7
Vincent, Chloroquine is a potent inhibitor of SARS coronavirus infection and spread, Virol J, doi:10.1186/1743-422X-2-69
Williamson, Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Wu, Analysis of therapeutic targets for SARS-CoV-2 and discovery of potential drugs by computational methods, Acta Pharm Sin B, doi:10.1016/j.apsb.2020.02.008
Wyss, Use of Time-Dependent Propensity Scores to Adjust Hazard Ratio Estimates in Cohort Studies with Differential Depletion of Susceptibles, Epidemiology, doi:10.1097/EDE.0000000000001107
Zhang, Coagulopathy and Antiphospholipid Antibodies in Patients with Covid-19, N Engl J Med, doi:10.1056/NEJMc2007575
DOI record:
{
"DOI": "10.1371/journal.pone.0266922",
"ISSN": [
"1932-6203"
],
"URL": "http://dx.doi.org/10.1371/journal.pone.0266922",
"abstract": "<jats:sec id=\"sec001\">\n<jats:title>Background</jats:title>\n<jats:p>Maintenance drugs are used to treat chronic conditions. Several classes of maintenance drugs have attracted attention because of their potential to affect susceptibility to and severity of COVID-19.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec002\">\n<jats:title>Methods</jats:title>\n<jats:p>Using claims data on 20% random sample of Part D Medicare enrollees from April to December 2020, we identified patients diagnosed with COVID-19. Using a nested case-control design, non-COVID-19 controls were identified by 1:5 matching on age, race, sex, dual-eligibility status, and geographical region. We identified usage of angiotensin-converting enzyme inhibitors (ACEI), angiotensin-receptor blockers (ARB), statins, warfarin, direct factor Xa inhibitors, P2Y12 inhibitors, famotidine and hydroxychloroquine based on Medicare prescription claims data. Using extended Cox regression models with time-varying propensity score adjustment we examined the independent effect of each study drug on contracting COVID-19. For severity of COVID-19, we performed extended Cox regressions on all COVID-19 patients, using COVID-19-related hospitalization and all-cause mortality as outcomes. Covariates included gender, age, race, geographic region, low-income indicator, and co-morbidities. To compensate for indication bias related to the use of hydroxychloroquine for the prophylaxis or treatment of COVID-19, we censored patients who only started on hydroxychloroquine in 2020.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec003\">\n<jats:title>Results</jats:title>\n<jats:p>Up to December 2020, our sample contained 374,229 Medicare patients over 65 who were diagnosed with COVID-19. Among the COVID-19 patients, 278,912 (74.6%) were on at least one study drug. The three most common study drugs among COVID-19 patients were statins 187,374 (50.1%), ACEI 97,843 (26.2%) and ARB 83,290 (22.3%). For all three outcomes (diagnosis, hospitalization and death), current users of ACEI, ARB, statins, warfarin, direct factor Xa inhibitors and P2Y12 inhibitors were associated with reduced risks, compared to never users. Famotidine did not show consistent significant effects. Hydroxychloroquine did not show significant effects after censoring of recent starters.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec004\">\n<jats:title>Conclusion</jats:title>\n<jats:p>Maintenance use of ACEI, ARB, warfarin, statins, direct factor Xa inhibitors and P2Y12 inhibitors was associated with reduction in risk of acquiring COVID-19 and dying from it.</jats:p>\n</jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0003-0593-5377",
"affiliation": [],
"authenticated-orcid": true,
"family": "Fung",
"given": "Kin Wah",
"sequence": "first"
},
{
"affiliation": [],
"family": "Baik",
"given": "Seo H.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Baye",
"given": "Fitsum",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zheng",
"given": "Zhaonian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Huser",
"given": "Vojtech",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McDonald",
"given": "Clement J.",
"sequence": "additional"
}
],
"container-title": "PLOS ONE",
"container-title-short": "PLoS ONE",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.plosone.org"
]
},
"created": {
"date-parts": [
[
2022,
4,
18
]
],
"date-time": "2022-04-18T17:27:56Z",
"timestamp": 1650302876000
},
"deposited": {
"date-parts": [
[
2022,
4,
18
]
],
"date-time": "2022-04-18T17:28:41Z",
"timestamp": 1650302921000
},
"editor": [
{
"affiliation": [],
"family": "Mogi",
"given": "Masaki",
"sequence": "first"
}
],
"funder": [
{
"DOI": "10.13039/100000092",
"award": [
"Intramural research program"
],
"doi-asserted-by": "publisher",
"name": "U.S. National Library of Medicine"
}
],
"indexed": {
"date-parts": [
[
2023,
10,
4
]
],
"date-time": "2023-10-04T10:32:07Z",
"timestamp": 1696415527413
},
"is-referenced-by-count": 7,
"issue": "4",
"issued": {
"date-parts": [
[
2022,
4,
18
]
]
},
"journal-issue": {
"issue": "4",
"published-online": {
"date-parts": [
[
2022,
4,
18
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/publicdomain/zero/1.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
4,
18
]
],
"date-time": "2022-04-18T00:00:00Z",
"timestamp": 1650240000000
}
}
],
"link": [
{
"URL": "https://dx.plos.org/10.1371/journal.pone.0266922",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "340",
"original-title": [],
"page": "e0266922",
"prefix": "10.1371",
"published": {
"date-parts": [
[
2022,
4,
18
]
]
},
"published-online": {
"date-parts": [
[
2022,
4,
18
]
]
},
"publisher": "Public Library of Science (PLoS)",
"reference": [
{
"DOI": "10.1161/CIRCULATIONAHA.104.510461",
"article-title": "Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2",
"author": "C.M. Ferrario",
"doi-asserted-by": "crossref",
"first-page": "2605",
"issue": "20",
"journal-title": "Circulation",
"key": "pone.0266922.ref001",
"volume": "111",
"year": "2005"
},
{
"DOI": "10.1007/s11906-008-0076-0",
"article-title": "Pharmacologic modulation of ACE2 expression",
"author": "M.J. Soler",
"doi-asserted-by": "crossref",
"first-page": "410",
"issue": "5",
"journal-title": "Curr Hypertens Rep",
"key": "pone.0266922.ref002",
"volume": "10",
"year": "2008"
},
{
"DOI": "10.1038/nature02145",
"article-title": "Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus",
"author": "W. Li",
"doi-asserted-by": "crossref",
"first-page": "450",
"issue": "6965",
"journal-title": "Nature",
"key": "pone.0266922.ref003",
"volume": "426",
"year": "2003"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"article-title": "SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor",
"author": "M. Hoffmann",
"doi-asserted-by": "crossref",
"first-page": "271",
"issue": "2",
"journal-title": "Cell",
"key": "pone.0266922.ref004",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1001/jamacardio.2020.1624",
"article-title": "Association of Renin-Angiotensin System Inhibitors With Severity or Risk of Death in Patients With Hypertension Hospitalized for Coronavirus Disease 2019 (COVID-19) Infection in Wuhan, China",
"author": "J. Li",
"doi-asserted-by": "crossref",
"first-page": "825",
"issue": "7",
"journal-title": "JAMA Cardiol",
"key": "pone.0266922.ref005",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1056/NEJMsr2005760",
"article-title": "Renin-Angiotensin-Aldosterone System Inhibitors in Patients with Covid-19",
"author": "M. Vaduganathan",
"doi-asserted-by": "crossref",
"first-page": "1653",
"issue": "17",
"journal-title": "N Engl J Med",
"key": "pone.0266922.ref006",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2006923",
"article-title": "Renin-Angiotensin-Aldosterone System Blockers and the Risk of Covid-19",
"author": "G. Mancia",
"doi-asserted-by": "crossref",
"first-page": "2431",
"issue": "25",
"journal-title": "N Engl J Med",
"key": "pone.0266922.ref007",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.11301",
"article-title": "Association of Angiotensin-Converting Enzyme Inhibitor or Angiotensin Receptor Blocker Use With COVID-19 Diagnosis and Mortality",
"author": "E.L. Fosbol",
"doi-asserted-by": "crossref",
"first-page": "168",
"issue": "2",
"journal-title": "JAMA",
"key": "pone.0266922.ref008",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2008975",
"article-title": "Renin-Angiotensin-Aldosterone System Inhibitors and Risk of Covid-19",
"author": "H.R. Reynolds",
"doi-asserted-by": "crossref",
"first-page": "2441",
"issue": "25",
"journal-title": "N Engl J Med",
"key": "pone.0266922.ref009",
"volume": "382",
"year": "2020"
},
{
"article-title": "Decreased Mortality of COVID-19 With Renin-Angiotensin-Aldosterone System Inhibitors Therapy in Patients With Hypertension: A Meta-Analysis",
"author": "X. Guo",
"first-page": "e13",
"issue": "2",
"journal-title": "Hypertension",
"key": "pone.0266922.ref010",
"volume": "76",
"year": "2020"
},
{
"article-title": "Use of inhibitors of the renin-angiotensin system in hypertensive patients and COVID-19 severity: A systematic review and meta-analysis",
"author": "J. Barochiner",
"journal-title": "J Clin Pharm Ther",
"key": "pone.0266922.ref011",
"year": "2020"
},
{
"key": "pone.0266922.ref012",
"unstructured": "Efficacy of Captopril in Covid-19 Patients With Severe Acute Respiratory Syndrome (SARS) CoV-2 Pneumonia (CAPTOCOVID) [clinical trial]. https://clinicaltrials.gov/ct2/show/NCT04355429."
},
{
"key": "pone.0266922.ref013",
"unstructured": "Angiotensin Converting Enzyme Inhibitors in Treatment of Covid 19 [clinical trial]. https://clinicaltrials.gov/ct2/show/NCT04345406."
},
{
"key": "pone.0266922.ref014",
"unstructured": "Valsartan for Prevention of Acute Respiratory Distress Syndrome in Hospitalized Patients With SARS-COV-2 (COVID-19) Infection Disease [clinical trial]. https://clinicaltrials.gov/ct2/show/NCT04335786."
},
{
"DOI": "10.1111/bph.15166",
"article-title": "Statins: Could an old friend help in the fight against COVID-19?",
"author": "R.R. Rodrigues-Diez",
"doi-asserted-by": "crossref",
"first-page": "4873",
"issue": "21",
"journal-title": "Br J Pharmacol",
"key": "pone.0266922.ref015",
"volume": "177",
"year": "2020"
},
{
"DOI": "10.3390/ijms22084177",
"article-title": "COVID-19: Direct and Indirect Mechanisms of Statins",
"author": "A. Pawlos",
"doi-asserted-by": "crossref",
"issue": "8",
"journal-title": "Int J Mol Sci",
"key": "pone.0266922.ref016",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1007/s43440-021-00233-3",
"article-title": "In-hospital use of statins is associated with a reduced risk of mortality in coronavirus-2019 (COVID-19): systematic review and meta-analysis",
"author": "H. Permana",
"doi-asserted-by": "crossref",
"first-page": "769",
"issue": "3",
"journal-title": "Pharmacol Rep",
"key": "pone.0266922.ref017",
"volume": "73",
"year": "2021"
},
{
"article-title": "Statin use and clinical outcomes in patients with COVID-19: An updated systematic review and meta-analysis",
"author": "R. Pal",
"journal-title": "Postgrad Med J",
"key": "pone.0266922.ref018",
"year": "2021"
},
{
"DOI": "10.1111/jth.14768",
"article-title": "Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia",
"author": "N. Tang",
"doi-asserted-by": "crossref",
"first-page": "844",
"issue": "4",
"journal-title": "J Thromb Haemost",
"key": "pone.0266922.ref019",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1016/j.jacc.2020.04.031",
"article-title": "COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review",
"author": "B. Bikdeli",
"doi-asserted-by": "crossref",
"first-page": "2950",
"issue": "23",
"journal-title": "J Am Coll Cardiol",
"key": "pone.0266922.ref020",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1056/NEJMc2007575",
"article-title": "Coagulopathy and Antiphospholipid Antibodies in Patients with Covid-19",
"author": "Y. Zhang",
"doi-asserted-by": "crossref",
"first-page": "e38",
"issue": "17",
"journal-title": "N Engl J Med",
"key": "pone.0266922.ref021",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1111/jth.14830",
"article-title": "Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia",
"author": "S. Cui",
"doi-asserted-by": "crossref",
"first-page": "1421",
"issue": "6",
"journal-title": "J Thromb Haemost",
"key": "pone.0266922.ref022",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1016/j.thromres.2020.04.041",
"article-title": "Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis",
"author": "F.A. Klok",
"doi-asserted-by": "crossref",
"first-page": "148",
"journal-title": "Thromb Res",
"key": "pone.0266922.ref023",
"volume": "191",
"year": "2020"
},
{
"DOI": "10.1007/s11886-020-01328-8",
"article-title": "The Role of Anticoagulation in COVID-19-Induced Hypercoagulability",
"author": "J.S. Rico-Mesa",
"doi-asserted-by": "crossref",
"first-page": "53",
"issue": "7",
"journal-title": "Curr Cardiol Rep",
"key": "pone.0266922.ref024",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1182/blood.2020006941",
"article-title": "Impact of anticoagulation prior to COVID-19 infection: a propensity score-matched cohort study",
"author": "D. Tremblay",
"doi-asserted-by": "crossref",
"first-page": "144",
"issue": "1",
"journal-title": "Blood",
"key": "pone.0266922.ref025",
"volume": "136",
"year": "2020"
},
{
"DOI": "10.1016/j.phrs.2020.104965",
"article-title": "Clinical impact of pre-admission antithrombotic therapy in hospitalized patients with COVID-19: A multicenter observational study",
"author": "V. Russo",
"doi-asserted-by": "crossref",
"first-page": "104965",
"journal-title": "Pharmacol Res",
"key": "pone.0266922.ref026",
"volume": "159",
"year": "2020"
},
{
"article-title": "COVID-19 mortality in patients on anticoagulants and antiplatelet agents",
"author": "H. Sivaloganathan",
"journal-title": "Br J Haematol",
"key": "pone.0266922.ref027",
"year": "2020"
},
{
"DOI": "10.2459/JCM.0000000000001066",
"article-title": "Coronavirus disease 2019 infection in patients with recent cardiac surgery: does chronic anticoagulant therapy have a protective effect?",
"author": "G. Inama",
"doi-asserted-by": "crossref",
"first-page": "765",
"issue": "10",
"journal-title": "J Cardiovasc Med (Hagerstown)",
"key": "pone.0266922.ref028",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1016/j.ejim.2020.06.006",
"article-title": "Protective role of chronic treatment with direct oral anticoagulants in elderly patients affected by interstitial pneumonia in COVID-19 era",
"author": "R. Rossi",
"doi-asserted-by": "crossref",
"first-page": "158",
"journal-title": "Eur J Intern Med",
"key": "pone.0266922.ref029",
"volume": "77",
"year": "2020"
},
{
"DOI": "10.1016/j.apsb.2020.02.008",
"article-title": "Analysis of therapeutic targets for SARS-CoV-2 and discovery of potential drugs by computational methods",
"author": "C. Wu",
"doi-asserted-by": "crossref",
"first-page": "766",
"issue": "5",
"journal-title": "Acta Pharm Sin B",
"key": "pone.0266922.ref030",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1016/S0024-3205(96)00553-X",
"article-title": "The effect of histamine type 2 receptor antagonists on human immunodeficiency virus (HIV) replication: identification of a new class of antiviral agents",
"author": "A.S. Bourinbaiar",
"doi-asserted-by": "crossref",
"first-page": "PL 365",
"issue": "23",
"journal-title": "Life Sci",
"key": "pone.0266922.ref031",
"volume": "59",
"year": "1996"
},
{
"DOI": "10.1136/gutjnl-2020-321852",
"article-title": "Famotidine use and quantitative symptom tracking for COVID-19 in non-hospitalised patients: a case series",
"author": "T. Janowitz",
"doi-asserted-by": "crossref",
"first-page": "1592",
"issue": "9",
"journal-title": "Gut",
"key": "pone.0266922.ref032",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1053/j.gastro.2020.05.053",
"article-title": "Famotidine Use Is Associated With Improved Clinical Outcomes in Hospitalized COVID-19 Patients: A Propensity Score Matched Retrospective Cohort Study",
"author": "D.E. Freedberg",
"doi-asserted-by": "crossref",
"first-page": "1129",
"issue": "3",
"journal-title": "Gastroenterology",
"key": "pone.0266922.ref033",
"volume": "159",
"year": "2020"
},
{
"DOI": "10.1016/j.bbrc.2004.08.085",
"article-title": "In vitro inhibition of severe acute respiratory syndrome coronavirus by chloroquine",
"author": "E. Keyaerts",
"doi-asserted-by": "crossref",
"first-page": "264",
"issue": "1",
"journal-title": "Biochem Biophys Res Commun",
"key": "pone.0266922.ref034",
"volume": "323",
"year": "2004"
},
{
"DOI": "10.1186/1743-422X-2-69",
"article-title": "Chloroquine is a potent inhibitor of SARS coronavirus infection and spread",
"author": "M.J. Vincent",
"doi-asserted-by": "crossref",
"first-page": "69",
"journal-title": "Virol J",
"key": "pone.0266922.ref035",
"volume": "2",
"year": "2005"
},
{
"DOI": "10.1136/postgradmedj-2020-137785",
"article-title": "Hydroxychloroquine and COVID-19",
"author": "N. Sinha",
"doi-asserted-by": "crossref",
"first-page": "550",
"issue": "1139",
"journal-title": "Postgrad Med J",
"key": "pone.0266922.ref036",
"volume": "96",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.06.099",
"article-title": "Treatment with hydroxychloroquine, azithromycin, and combination in patients hospitalized with COVID-19",
"author": "S. Arshad",
"doi-asserted-by": "crossref",
"first-page": "396",
"journal-title": "Int J Infect Dis",
"key": "pone.0266922.ref037",
"volume": "97",
"year": "2020"
},
{
"key": "pone.0266922.ref038",
"unstructured": "Research Data Assistance Center (ResDAC). CMS Virtual Research Data Center (VRDC). https://www.resdac.org/cms-virtual-research-data-center-vrdc."
},
{
"key": "pone.0266922.ref039",
"unstructured": "The Chronic Condition Warehouse. Chronic Conditions Data Warehouse: CCW Chronic Condition Algorithms. https://www.ccwdata.org/web/guest/condition-categories."
},
{
"DOI": "10.1006/pmed.1994.1093",
"article-title": "Nested case-control studies",
"author": "V.L. Ernster",
"doi-asserted-by": "crossref",
"first-page": "587",
"issue": "5",
"journal-title": "Prev Med",
"key": "pone.0266922.ref040",
"volume": "23",
"year": "1994"
},
{
"DOI": "10.1038/sj.bjc.6605062",
"article-title": "Prevalent cases in observational studies of cancer survival: do they bias hazard ratio estimates?",
"author": "E.M. Azzato",
"doi-asserted-by": "crossref",
"first-page": "1806",
"issue": "11",
"journal-title": "Br J Cancer",
"key": "pone.0266922.ref041",
"volume": "100",
"year": "2009"
},
{
"DOI": "10.1093/biomet/70.1.41",
"article-title": "The Central Role of the Propensity Score in Observational Studies for Causal Effects",
"author": "P.R. Rosenbaum",
"doi-asserted-by": "crossref",
"first-page": "41",
"journal-title": "Biometrika",
"key": "pone.0266922.ref042",
"volume": "70",
"year": "1983"
},
{
"DOI": "10.1097/EDE.0000000000001107",
"article-title": "Use of Time-Dependent Propensity Scores to Adjust Hazard Ratio Estimates in Cohort Studies with Differential Depletion of Susceptibles",
"author": "R. Wyss",
"doi-asserted-by": "crossref",
"first-page": "82",
"issue": "1",
"journal-title": "Epidemiology",
"key": "pone.0266922.ref043",
"volume": "31",
"year": "2020"
},
{
"key": "pone.0266922.ref044",
"unstructured": "Centers for Disease Control and Prevention. COVID-19 Response. COVID-19 Case Surveillance Public Data Access, Summary, and Limitations. 2020; https://data.cdc.gov/Case-Surveillance/COVID-19-Case-Surveillance-Public-Use-Data/vbim-akqf."
},
{
"DOI": "10.1016/j.sjbs.2021.07.003",
"article-title": "RAAS, ACE2 and COVID-19; a mechanistic review",
"author": "A. Elshafei",
"doi-asserted-by": "crossref",
"first-page": "6465",
"issue": "11",
"journal-title": "Saudi J Biol Sci",
"key": "pone.0266922.ref045",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1016/j.cardfail.2020.04.013",
"article-title": "Joint HFSA/ACC/AHA Statement Addresses Concerns Re: Using RAAS Antagonists in COVID-19",
"author": "B. Bozkurt",
"doi-asserted-by": "crossref",
"first-page": "370",
"issue": "5",
"journal-title": "J Card Fail",
"key": "pone.0266922.ref046",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.15557/PiMR.2020.0023",
"doi-asserted-by": "crossref",
"key": "pone.0266922.ref047",
"unstructured": "World Health Organization. COVID-19 and the use of angiotensin-converting enzyme inhibitors and receptor blockers—Scientific Brief. 2020; https://www.who.int/news-room/commentaries/detail/covid-19-and-the-use-of-angiotensin-converting-enzyme-inhibitors-and-receptor-blockers."
},
{
"DOI": "10.1186/s12959-021-00298-3",
"article-title": "A review of thromboembolic events in hospitalized COVID-19 patients",
"author": "P. Fontelo",
"doi-asserted-by": "crossref",
"first-page": "47",
"issue": "1",
"journal-title": "Thromb J",
"key": "pone.0266922.ref048",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"article-title": "Factors associated with COVID-19-related death using OpenSAFELY",
"author": "E.J. Williamson",
"doi-asserted-by": "crossref",
"first-page": "430",
"issue": "7821",
"journal-title": "Nature",
"key": "pone.0266922.ref049",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1016/j.ijchy.2021.100088",
"article-title": "COVID-19 morbidity and mortality associated with angiotensin-converting enzyme inhibitors or angiotensin receptor blockers use among 14,129 patients with hypertension from a US integrated healthcare system",
"author": "J. An",
"doi-asserted-by": "crossref",
"first-page": "100088",
"journal-title": "Int J Cardiol Hypertens",
"key": "pone.0266922.ref050",
"volume": "9",
"year": "2021"
},
{
"key": "pone.0266922.ref051",
"unstructured": "Administration on Aging—U.S. Department of Health and Human Services. 2018 Profile of Older Americans. https://acl.gov/aging-and-disability-in-america/data-and-research/profile-older-americans."
},
{
"DOI": "10.1002/9780470059876.ch47",
"author": "I. Csizmadi",
"doi-asserted-by": "crossref",
"first-page": "791",
"key": "pone.0266922.ref052",
"volume-title": "Pharmacoepidemiology",
"year": "2006"
},
{
"DOI": "10.1592/phco.26.9.1288",
"article-title": "Statin withdrawal: clinical implications and molecular mechanisms",
"author": "L.X. Cubeddu",
"doi-asserted-by": "crossref",
"first-page": "1288",
"issue": "9",
"journal-title": "Pharmacotherapy",
"key": "pone.0266922.ref053",
"volume": "26",
"year": "2006"
},
{
"article-title": "How to control confounding effects by statistical analysis",
"author": "M.A. Pourhoseingholi",
"first-page": "79",
"issue": "2",
"journal-title": "Gastroenterol Hepatol Bed Bench",
"key": "pone.0266922.ref054",
"volume": "5",
"year": "2012"
},
{
"DOI": "10.1016/S1473-3099(20)30243-7",
"article-title": "Estimates of the severity of coronavirus disease 2019: a model-based analysis",
"author": "R. Verity",
"doi-asserted-by": "crossref",
"first-page": "669",
"issue": "6",
"journal-title": "Lancet Infect Dis",
"key": "pone.0266922.ref055",
"volume": "20",
"year": "2020"
}
],
"reference-count": 55,
"references-count": 55,
"relation": {},
"resource": {
"primary": {
"URL": "https://dx.plos.org/10.1371/journal.pone.0266922"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "Effect of common maintenance drugs on the risk and severity of COVID-19 in elderly patients",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1371/journal.pone.corrections_policy",
"volume": "17"
}
fung