Association Between Vitamin D Levels and COVID-19 Infection in Children: A Case-Control Study
et al., Turkish Archives of Pediatrics, doi:10.5152/turkarchpediatr.2023.22217, Apr 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 73 COVID-19 and 76 healthy pediatric patients in Turkey, showing significantly lower vitamin D levels in COVID-19 patients.
This is the 172nd of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
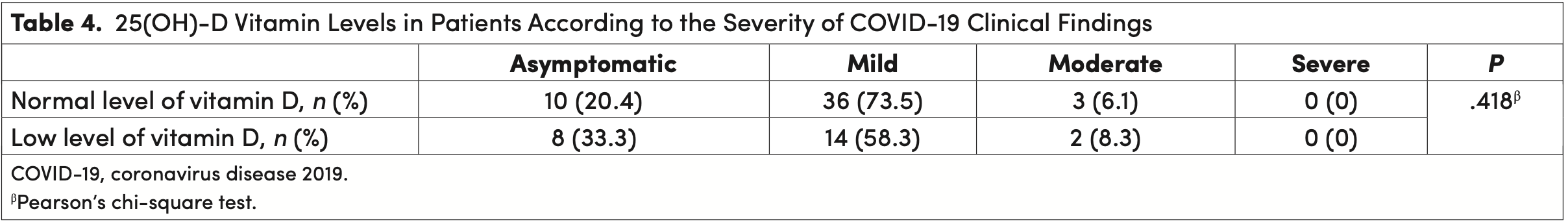
risk of moderate/severe case, 26.5% lower, RR 0.73, p = 1.00, high D levels (≥20ng/mL) 3 of 49 (6.1%), low D levels (<20ng/mL) 2 of 24 (8.3%), NNT 45.
|
|
risk of case, 33.4% lower, OR 0.67, p = 0.23, high D levels (≥20ng/mL) 41 of 73 (56.2%) cases,
50 of 76 (65.8%) controls, NNT 9.9, case control OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Bayrak et al., 5 Apr 2023, retrospective, Turkey, peer-reviewed, mean age 19.0, 8 authors, study period November 2020 - January 2021.
Contact: hrnbyrk@gmail.com.
Association Between Vitamin D Levels and COVID-19 Infection in Children: A Case-Control Study
Turkish Archives of Pediatrics, doi:10.5152/turkarchpediatr.2023.22217
Objective: Coronavirus disease 2019 (COVID-19) infection is seen in all age groups, and its symptoms are very variable. The course of the disease can be asymptomatic or mortal. In pediatric patients, vitamin D is thought to be protective against (COVID-19) with its immunomodulator, antiviral, anti-inflammatory, and epithelial integrity properties. Our aim is to investigate the relationship between (COVID-19) infection and vitamin D level.
Materials and Methods: We included (COVID-19) patients between 1 month and 18 years of age and healthy control groups. We compared epidemiological, clinical, laboratory, and imaging findings in patients. Results: One hundred forty-nine patients were evaluated in our study. Seventy-three (49%) of them were (COVID-19)-positive patients and 76 (51%) of them were healthy control group. The mean 25(OH)-D vitamin level was 15.80 ng/mL (5-41.56) in (COVID-19) patients and 21.51 ng/mL (5-69.80) in the control group. Vitamin D level was shown to be statistically significantly lower in coronavirus disease 2019 patients (P < .001). It was observed that myalgia was more common in patients with low 25(OH)-D levels (P < .048).
Conclusion: Our study is one of the rare studies examining the relationship between (COVID-19) and 25(OH)-D vitamins in the pediatric age group. Children with (COVID-19) have a lower 25(OH)-D vitamin level than the control group.
Ethics Committee Approval: Ethical committee approval was received from the Ethics Committee of University of Health Sciences University (Approval No: 2020-493). Informed Consent: Informed consent was obtained from the patient's family, who agreed to take part in the study. Peer-review: Externally peer-reviewed.
References
Carpagnano, Lecce, Quaranta, Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19, J Endocrinol Invest, doi:10.1007/s40618-020-01370-x
Dalvi, Ramraje, Patil, Hegde, Yeram, Study of IL-6 and vitamin D3 in patients of pulmonary tuberculosis, Indian J Tuberc, doi:10.1016/j.ijtb.2018.05.018
Dong, Mo, Hu, Epidemiology of COVID-19 among children in China, Pediatrics, doi:10.1542/peds.2020-0702
Esposito, Lelii, Vitamin D and respiratory tract infections in childhood, BMC Infect Dis, doi:10.1186/s12879-015-1196-1
Gombart, Borregaard, Koeffler, Human cathelicidin antimicrobial peptide (CAMP) gene is a direct target of the vitamin D receptor and is strongly up-regulated in myeloid cells by 1,25-dihydroxyvitamin D3, FASEB J, doi:10.1096/fj.04-3284com
Grant, Lahore, Mcdonnell, Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients, doi:10.3390/nu12040988
Greiller, Martineau, Modulation of the immune response to respiratory viruses by vitamin D, Nutrients, doi:10.3390/nu7064240
Gül, Gür, Erener Ercan, Can, The effect of vitamin D prophylaxis on 25-OH vitamin D levels in children, Turk Arch Pediatr, doi:10.5152/TurkArchPediatr.2021.21166
Holick, The vitamin D deficiency pandemic: approaches for diagnosis, treatment and prevention, Rev Endocr Metab Disord, doi:10.1007/s11154-017-9424-1
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin Exp Res, doi:10.1007/s40520-020-01570-8
Jain, Parsanathan, Can vitamin D and L-cysteine co-supplementation reduce 25(OH)-Vitamin D Deficiency and the Mortality Associated with COVID-19 in African Americans?, J Am Coll Nutr, doi:10.1080/07315724.2020.1789518
Jolliffe, Camargo, Jr, Sluyter, Vitamin D supplementation to prevent acute respiratory infections: a systematic review and meta-analysis of aggregate data from randomised controlled trials, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00051-6
Kakodkar, Kaka, Baig, A comprehensive literature review on the clinical presentation, and management of the pandemic coronavirus disease 2019 (COVID-19), Cureus, doi:10.7759/cureus.7560
Kara, Ekiz, Ricci, Kara, Chang et al., Scientific Strabismus' or two related pandemics: coronavirus disease and vitamin D deficiency, Br J Nutr, doi:10.1017/S0007114520001749
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS One, doi:10.1371/journal.pone.0239252
Khayznikov, Hemachrandra, Pandit, Kumar, Wang et al., Statin intolerance because of myalgia, myositis, myopathy, or myonecrosis can in most cases be safely resolved by vitamin D supplementation, N Am J Med Sci, doi:10.4103/1947-2714.153919
Kurnik, Hochman, Vesterman-Landes, Muscle pain and serum creatine kinase are not associated with low serum 25(OH) vitamin D levels in patients receiving statins, Clin Endocrinol (Oxf), doi:10.1111/j.1365-2265.2011.04321.x
Köse, Korelasyon Ve, Regresyon Analizi
Lechien, Chiesa-Estomba, Place, Clinical and epidemiological characteristics of 1420 European patients with mildto-moderate coronavirus disease 2019, J Intern Med, doi:10.1111/joim.13089
Li, Huang, Wang, COVID-19 patients' clinical characteristics, discharge rate, and fatality rate of meta-analysis, J Med Virol, doi:10.1002/jmv.25757
Li, Tian, Wang, The prevalence of vitamin D deficiency among schoolchildren: a cohort study from Xinxiang, China, J Pediatr Endocrinol Metab, doi:10.1515/jpem-2014-0250
Lu, Zhang, Ma, Link between community-acquired pneumonia and vitamin D levels in older patients
López, Gerber, Leonard, Xie, Schinnar et al., Children with lower respiratory tract infections and serum 25-hydroxyvitamin D3 levels: a case-control study, Pediatr Pulmonol, doi:10.1002/ppul.23439
Manion, Hullsiek, Wilson, Vitamin D deficiency is associated with IL-6 levels and monocyte activation in HIV-infected persons, PLoS One, doi:10.1371/journal.pone.0175517
Martineau, Jolliffe, Greenberg, Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis, Health Technol Assess, doi:10.3310/hta23020
Meltzer, Best, Zhang, Vokes, Arora et al., Association of vitamin D status and other clinical characteristics with COVID-19 test results, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.19722
Merzon, Tworowski, Gorohovski, Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study, FEBS Journal, doi:10.1111/febs.15495
Misra, Pacaud, Petryk, Collett-Solberg, Kappy, Drug and Therapeutics Committee of the Lawson Wilkins Pediatric Endocrine Society. Vitamin D deficiency in children and its management: review of current knowledge and recommendations, Pediatrics, doi:10.1542/peds.2007-1894
Parri, Lenge, Cantoni, COVID-19 in 17 Italian pediatric emergency departments, Pediatrics, doi:10.1542/peds.2020-1235
Pennisi, Bartolo, Malaguarnera, Bella, Lanza et al., Vitamin D serum levels in patients with statininduced musculoskeletal pain, Dis Markers, doi:10.1155/2019/3549402
Poudel-Tandukar, Poudel, Jimba, Kobayashi, Johnson et al., Serum 25-hydroxyvitamin d levels and C-reactive protein in persons with human immunodeficiency virus infection, AIDS Res Hum Retrovir, doi:10.1089/AID.2012.0120
Scott, Gronowski, Reid, Holick, Thadhani et al., Vitamin D: the more we know, the less we know, Clin Chem, doi:10.1373/clinchem.2014.222521
Shen, Yang, Wang, Diagnosis, treatment, and prevention of 2019 novel coronavirus infection in children: experts' consensus statement, World J Pediatr, doi:10.1007/s12519-020-00343-7
Sinha, Calfee, Cherian, Prevalence of phenotypes of acute respiratory distress syndrome in critically ill patients with COVID-19: a prospective observational study, Lancet Respir Med, doi:10.1016/S2213-2600(20)30366-0
Tiosano, Abrams, Weisman, Lessons learned from hereditary 1,25-dihydroxyvitamin D-resistant rickets patients on vitamin D functions, J Nutr, doi:10.1093/jn/nxaa380
Vankadari, Wilce, Emerging WuHan (COVID-19) coronavirus: glycan shield and structure prediction of spike glycoprotein and its interaction with human CD26, Emerg Microbes Infect, doi:10.1080/22221751.2020.1739565
Wang, Liu, Zhao, Clinical characteristics of 80 hospitalized frontline medical workers infected with COVID-19 in Wuhan, China, J Hosp Infect, doi:10.1016/j.jhin.2020.04.019
Worldometer, None
Yılmaz, Şen, Is vitamin D deficiency a risk factor for COVID-19 in children?, Pediatr Pulmonol, doi:10.1002/ppul.25106
Zhou, Luo, Qin, The association between vitamin D deficiency and community-acquired pneumonia: a meta-analysis of observational studies, Med (Baltim), doi:10.1097/MD.0000000000017252
Zimmermann, Curtis, Why is COVID-19 less severe in children? A review of the proposed mechanisms underlying the age-related difference in severity of SARS-CoV-2 infections, Arch Dis Child, doi:10.1136/archdischild-2020-320338
DOI record:
{
"DOI": "10.5152/turkarchpediatr.2023.22217",
"URL": "http://dx.doi.org/10.5152/turkarchpediatr.2023.22217",
"author": [
{
"affiliation": [],
"family": "Bayrak",
"given": "Harun",
"sequence": "first"
},
{
"affiliation": [],
"name": "Department of General Pediatrics, University of Health Sciences Gulhane Faculty of Medicine, Ankara, Turkey",
"sequence": "first"
},
{
"affiliation": [],
"family": "Ozturk",
"given": "Didem",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bolat",
"given": "Ahmet",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Unay",
"given": "Bulent",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Department of General Pediatrics, University of Health Sciences Gulhane Faculty of Medicine, Ankara, Turkey",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Department of General Pediatrics, University of Health Sciences Gulhane Faculty of Medicine, Ankara, Turkey",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Department of General Pediatrics, University of Health Sciences Gulhane Faculty of Medicine, Ankara, Turkey;Department of Pediatric Neurology, University of Health Sciences Gulhane Faculty of Medicine, Ankara, Turkey",
"sequence": "additional"
}
],
"container-title": "Turkish Archives of Pediatrics",
"container-title-short": "Turk Arch Pediatr",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
4,
5
]
],
"date-time": "2023-04-05T11:31:40Z",
"timestamp": 1680694300000
},
"deposited": {
"date-parts": [
[
2023,
4,
5
]
],
"date-time": "2023-04-05T11:31:42Z",
"timestamp": 1680694302000
},
"indexed": {
"date-parts": [
[
2023,
4,
6
]
],
"date-time": "2023-04-06T05:04:28Z",
"timestamp": 1680757468099
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
4,
5
]
]
},
"member": "3111",
"original-title": [],
"prefix": "10.5152",
"published": {
"date-parts": [
[
2023,
4,
5
]
]
},
"published-online": {
"date-parts": [
[
2023,
4,
5
]
]
},
"publisher": "AVES YAYINCILIK A.Ş.",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://turkarchpediatr.org/en/association-between-vitamin-d-levels-and-covid-19-infection-in-children-a-case-control-study-131483"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Water Science and Technology",
"Aquatic Science",
"Oceanography",
"Geometry and Topology",
"Statistics and Probability",
"Algebra and Number Theory",
"Analysis",
"General Medicine",
"Computer Networks and Communications",
"Hardware and Architecture",
"Software",
"General Medicine",
"Political Science and International Relations",
"Sociology and Political Science",
"Sociology and Political Science",
"Cultural Studies",
"Marketing",
"Medicine (miscellaneous)",
"Experimental and Cognitive Psychology"
],
"subtitle": [],
"title": "Association Between Vitamin D Levels and COVID-19 Infection in Children: A Case-Control Study",
"type": "journal-article"
}
