Dampening of the respiratory cytokine storm is promoted by inhaled budesonide in patients with early COVID-19
et al., medRxiv, doi:10.1101/2021.10.26.21265512, Oct 2021
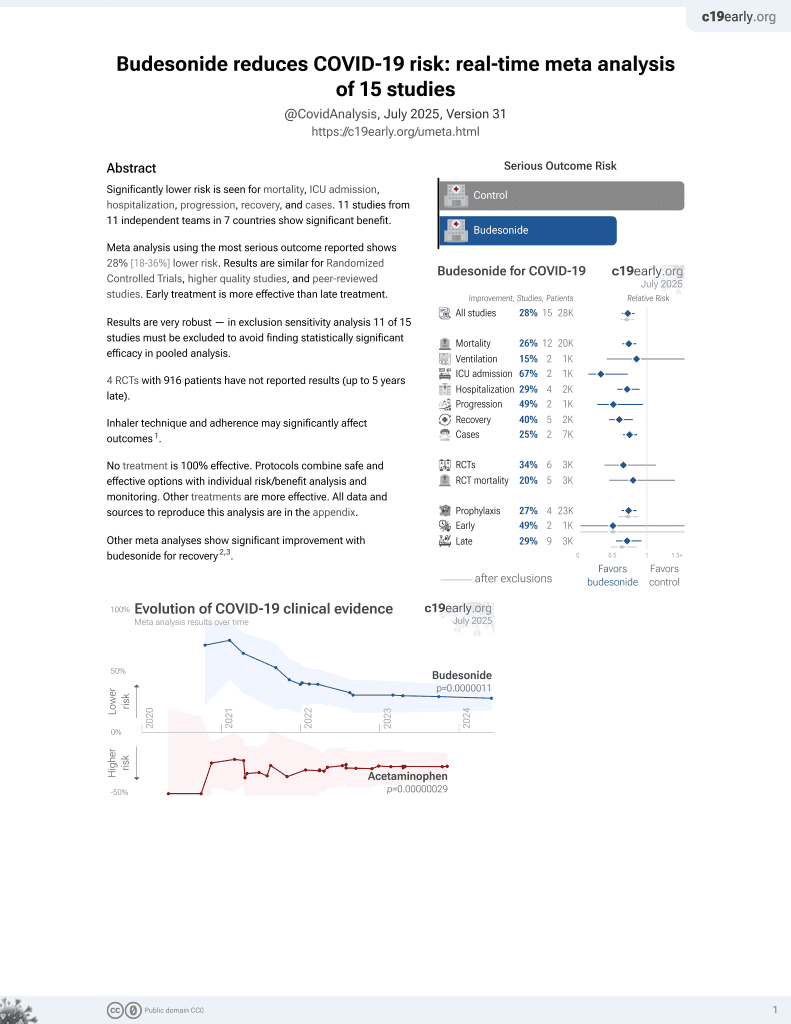
Budesonide for COVID-19
28th treatment shown to reduce risk in
September 2021, now with p = 0.0000042 from 14 studies, recognized in 10 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Analysis of inflammatory mediators in the nasal mucosa of patients in the STOIC1 trial and a cohort of SARS-CoV-2 negative controls, showing that budesonide treatment decreased IL-33 and IFN-γ, implying a reduction in epithelial damage and dampening of the interferon response. Treatment also increased CCL17 concentrations, suggesting improved T-cell response.
Baker et al., 27 Oct 2021, preprint, 10 authors.
Dampening of the respiratory cytokine storm is promoted by inhaled budesonide in patients with early COVID-19
doi:10.1101/2021.10.26.21265512
Vaccinations against SARS-CoV-2 are effective in COVID-19. However, with limited vaccine access, vaccine hesitancy and variant breakthroughs, there is still a need for effective and safe early treatments. Two community-based clinical trials of the inhaled corticosteroid, budesonide, have recently been published showing and improvement in patients with COVID-19 treated early with budesonide 1,2 . To understand mechanistically how budesonide was beneficial, inflammatory mediators were assessed in the nasal mucosa of patients recruited to the Steroids in COVID (STOIC 1 ) trial and a cohort of SARS-CoV-2 negative individuals. Here we show that in early COVID-19, elevation in viral response proteins and Th1 and Th2 inflammation occurs. Longitudinal sampling in the natural course of COVID-19 showed persistently high interferon levels and elevated concentrations of the eosinophil chemokine, CCL11. In patients who deteriorate, the initial nasal mucosal signal is characterised by a marked suppression of the early inflammatory response, with reduced concentrations of interferon and inflammatory cytokines, but elevated eosinophil chemokines. Systemic inflammation remained altered in COVID-19 patients, implying that even after symptom resolution, changes in immunological mediators do not resolve. Budesonide treatment decreased IL-33 and IFN-γ, implying a reduction in epithelial damage and dampening of the interferon response. Budesonide treatment also increased CCL17 concentrations, suggesting an improved T-cell response; and significantly alters inflammatory pathways giving further insight into how this treatment can accelerate patient recovery. . This finding has now been replicated in a large Phase 3 efficacy trial 2 , but has yet to attract global adoption. The mechanism for how ICS can improve early COVID-19 infection is however currently unknown. Here, we report the nasal mucosal inflammatory response in patients with early COVID-19 disease and examine the evolution of inflammation in the natural course of COVID-19. We also identify how inflammation in the airway can predict illness severity and investigate the effect of inhaled budesonide upon the respiratory mucosa in early COVID-19 disease. Finally, we show using network analysis how inhaled budesonide can resolve the exaggerated inflammatory response seen in early COVID-19 infection and promote resolution to health.
Methods
Study design and participants STOIC was a randomised, open-label, parallel group, phase 2 clinical intervention trial. Participants aged 18 and over with early COVID-19 symptoms (defined as new onset of cough and/or fever and/or anosmia for less than 7 days) were randomised to receive usual care (UC), namely as required anti-pyretics, or inhaled budesonide (BUD) at a dose of 800μg twice a day plus usual care (see supplement figure S1 ). Participants were seen at home at randomisation day 0 (visit 1), day 7 (visit 2), and day 14 (visit 3) by a research nurse to obtain consent, provide inhalers and collect nasal absorption samples and nasopharyngeal swabs which were self-performed. At day 28 (visit 4), whole
Nasal mucosal sampling Nasal mucosal sampling was self-performed by all participants as previously described
37 . Briefly, samples of the nasal mucosal lining fluid were collected by placing a Nasosorption™ FX•I device (Hunt Developments UK Ltd) consisting of a synthetic absorptive matrix strip against the inferior turbinate for a duration of 1 minute. The sample was then eluted in 500 μL of PBS, 1% bovine serum albumin (BSA) (w/v), 1% Triton X-100 (v/v), and 0.05% sodium azide (w/v) (Sigma-Aldrich, UK) and stored at -80°C.
Isolation of serum
References
Bafadhel, Acute exacerbations of chronic obstructive pulmonary disease: identification of biologic clusters and their biomarkers, Am J Respir Crit Care Med, doi:10.1164/rccm.201104-0597OC
Bafadhel, Pavord, Russell, Eosinophils in COPD: just another biomarker?, Lancet Respir Med, doi:10.1016/S2213-2600(17)30217-5
Barnes, Inhaled Corticosteroids, Pharmaceuticals, doi:10.3390/ph3030514
Blondel, Guillaume, Lambiotte, Lefebvre, Fast unfolding of communities in large networks, Journal of Statistical Mechanics: Theory and Experiment, doi:10.1088/1742-5468/2008/10/p10008
Bloom, Risk of adverse outcomes in patients with underlying respiratory conditions admitted to hospital with COVID-19: a national, multicentre prospective cohort study using the ISARIC WHO Clinical Characterisation Protocol UK, Lancet Respir Med, doi:10.1016/S2213-2600(21)00013-8
Chua, COVID-19 severity correlates with airway epithelium-immune cell interactions identified by single-cell analysis, Nature Biotechnology, doi:10.1038/s41587-020-0602-4
Farr, Altered microRNA expression in COVID-19 patients enables identification of SARS-CoV-2 infection, PLoS Pathog, doi:10.1371/journal.ppat.1009759
Finney, Inhaled corticosteroids downregulate the SARS-CoV-2 receptor ACE2 in COPD through suppression of type I interferon, The Journal of allergy and clinical immunology, doi:10.1016/j.jaci.2020.09.034
Gleich, Mechanisms of eosinophil-associated inflammation, J Allergy Clin Immunol, doi:10.1067/mai.2000.105712
Guan, Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis, Eur Respir J, doi:10.1183/13993003.00547-2020
Guo-Parke, Linden, Weldon, Kidney, Taggart, Mechanisms of Virus-Induced Airway Immunity Dysfunction in the Pathogenesis of COPD Disease, Progression, and Exacerbation, Frontiers in Immunology, doi:10.3389/fimmu.2020.01205
Hadjadj, Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients, Science, doi:10.1126/science.abc6027
Han, Profiling serum cytokines in COVID-19 patients reveals IL-6 and IL-10 are disease severity predictors, Emerging Microbes & Infections, doi:10.1080/22221751.2020.1770129
Hoffmann, SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor, Cell, doi:10.1016/j.cell.2020.02.052
Iyengar, Jain, Vaishya, Ish, Long COVID-19: an emerging pandemic in itself, Adv Respir Med, doi:10.5603/ARM.a2021.0040
Lee, Ashkar, The Dual Nature of Type I and Type II Interferons, Frontiers in Immunology, doi:10.3389/fimmu.2018.02061
Leist, Schäfer, Martinez, Cell and animal models of SARS-CoV-2 pathogenesis and immunity, Disease Models & Mechanisms, doi:10.1242/dmm.046581
Liao, Single-cell landscape of bronchoalveolar immune cells in patients with COVID-19, Nature Medicine, doi:10.1038/s41591-020-0901-9
Lucas, Longitudinal analyses reveal immunological misfiring in severe COVID-19, Nature, doi:10.1038/s41586-020-2588-y
Marchenko, Pastur, Распределение собственных значений в некоторых ансамблях случайных матриц
Mason, Thoughts on the alveolar phase of COVID-19, American Journal of Physiology-Lung Cellular and Molecular Physiology, doi:10.1152/ajplung.00126.2020
Message, Johnston, The immunology of virus infection in asthma, European Respiratory Journal, doi:10.1183/09031936.01.00228701
Milne, Inhaled corticosteroids downregulate SARS-CoV-2-related genes in COPD: results from a randomised controlled trial, Eur Respir J, doi:10.1183/13993003.00130-2021
Morton, Distinct clinical and immunological profiles of patients with evidence of SARS-CoV-2 infection in sub-Saharan Africa, Nature communications, doi:10.1038/s41467-021-23267-w
Murira, Lamarre, Type-I Interferon Responses: From Friend to Foe in the Battle against Chronic Viral Infection, Frontiers in Immunology, doi:10.3389/fimmu.2016.00609
Papi, Infections and airway inflammation in chronic obstructive pulmonary disease severe exacerbations, Am J Respir Crit Care Med, doi:10.1164/rccm.200506-859OC
Peluso, Long-term SARS-CoV-2-specific immune and inflammatory responses in individuals recovering from COVID-19 with and without post-acute symptoms, Cell Rep, doi:10.1016/j.celrep.2021.109518
Ramakrishnan, Inhaled budesonide in the treatment of early COVID-19 (STOIC): a phase 2, open-label, randomised controlled trial, Lancet Respir Med, doi:10.1016/s2213-2600(21)00160-0
Rogliani, Lauro, Di Daniele, Chetta, Calzetta, Reduced risk of COVID-19 hospitalization in asthmatic and COPD patients: a benefit of inhaled corticosteroids?, Expert Rev Respir Med, doi:10.1080/17476348.2021.1850275
Rouse, Sehrawat, Immunity and immunopathology to viruses: what decides the outcome?, Nature Reviews Immunology, doi:10.1038/nri2802
Saris, Distinct cellular immune profiles in the airways and blood of critically ill patients with COVID-19, Thorax, doi:10.1136/thoraxjnl-2020-216256
Scheller, Chalaris, Garbers, Rose-John, ADAM17: a molecular switch to control inflammation and tissue regeneration, Trends in Immunology, doi:10.1016/j.it.2011.05.005
Sudre, Attributes and predictors of long COVID, Nature Medicine, doi:10.1038/s41591-021-01292-y
Tan, Viruses in asthma exacerbations, Curr Opin Pulm Med, doi:10.1097/01.mcp.0000146781.11092.0d
Thwaites, Inflammatory profiles across the spectrum of disease reveal a distinct role for GM-CSF in severe COVID-19, Sci Immunol, doi:10.1126/sciimmunol.abg9873
Valle, An inflammatory cytokine signature predicts COVID-19 severity and survival, Nature medicine, doi:10.1038/s41591-020-1051-9
Vareille, Kieninger, Edwards, Regamey, The airway epithelium: soldier in the fight against respiratory viruses, Clin Microbiol Rev, doi:10.1128/CMR.00014-10
Yamaya, Nishimura, Nadine, Kubo, Nagatomi, Formoterol and budesonide inhibit rhinovirus infection and cytokine production in primary cultures of human tracheal epithelial cells, Respir Investig, doi:10.1016/j.resinv.2014.03.004
Yu, Inhaled budesonide for COVID-19 in people at high risk of complications in the community in the UK (PRINCIPLE): a randomised, controlled, open-label, adaptive platform trial, Lancet, doi:10.1016/S0140-6736(21)01744-X
Zhou, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
DOI record:
{
"DOI": "10.1101/2021.10.26.21265512",
"URL": "http://dx.doi.org/10.1101/2021.10.26.21265512",
"abstract": "<jats:title>Summary</jats:title><jats:p>Vaccinations against SARS-CoV-2 are effective in COVID-19. However, with limited vaccine access, vaccine hesitancy and variant breakthroughs, there is still a need for effective and safe early treatments. Two community-based clinical trials of the inhaled corticosteroid, budesonide, have recently been published showing and improvement in patients with COVID-19 treated early with budesonide<jats:sup>1,2</jats:sup>. To understand mechanistically how budesonide was beneficial, inflammatory mediators were assessed in the nasal mucosa of patients recruited to the Steroids in COVID (STOIC<jats:sup>1</jats:sup>) trial and a cohort of SARS-CoV-2 negative individuals. Here we show that in early COVID-19, elevation in viral response proteins and Th1 and Th2 inflammation occurs. Longitudinal sampling in the natural course of COVID-19 showed persistently high interferon levels and elevated concentrations of the eosinophil chemokine, CCL11. In patients who deteriorate, the initial nasal mucosal signal is characterised by a marked suppression of the early inflammatory response, with reduced concentrations of interferon and inflammatory cytokines, but elevated eosinophil chemokines. Systemic inflammation remained altered in COVID-19 patients, implying that even after symptom resolution, changes in immunological mediators do not resolve. Budesonide treatment decreased IL-33 and IFN-γ, implying a reduction in epithelial damage and dampening of the interferon response. Budesonide treatment also increased CCL17 concentrations, suggesting an improved T-cell response; and significantly alters inflammatory pathways giving further insight into how this treatment can accelerate patient recovery.</jats:p><jats:sec><jats:title>Abstract Figure</jats:title><jats:fig id=\"ufig1\" position=\"float\" fig-type=\"figure\" orientation=\"portrait\"><jats:graphic xmlns:xlink=\"http://www.w3.org/1999/xlink\" xlink:href=\"21265512v1_ufig1\" position=\"float\" orientation=\"portrait\" /></jats:fig></jats:sec>",
"accepted": {
"date-parts": [
[
2021,
10,
27
]
]
},
"author": [
{
"affiliation": [],
"family": "Baker",
"given": "Jonathan R",
"sequence": "first"
},
{
"affiliation": [],
"family": "Mahdi",
"given": "Mahdi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nicolau",
"given": "Dan V",
"sequence": "additional",
"suffix": "Jr."
},
{
"ORCID": "http://orcid.org/0000-0002-3003-7918",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ramakrishnan",
"given": "Sanjay",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5122-4018",
"affiliation": [],
"authenticated-orcid": false,
"family": "Barnes",
"given": "Peter J",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Simpson",
"given": "Jodie L",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7032-6239",
"affiliation": [],
"authenticated-orcid": false,
"family": "Cass",
"given": "Steven P",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3890-7201",
"affiliation": [],
"authenticated-orcid": false,
"family": "Russell",
"given": "Richard EK",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Donnelly",
"given": "Louise E",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9993-2478",
"affiliation": [],
"authenticated-orcid": false,
"family": "Bafadhel",
"given": "Mona",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
10,
29
]
],
"date-time": "2021-10-29T14:55:17Z",
"timestamp": 1635519317000
},
"deposited": {
"date-parts": [
[
2021,
10,
29
]
],
"date-time": "2021-10-29T14:55:21Z",
"timestamp": 1635519321000
},
"group-title": "Infectious Diseases (except HIV/AIDS)",
"indexed": {
"date-parts": [
[
2022,
3,
31
]
],
"date-time": "2022-03-31T12:47:50Z",
"timestamp": 1648730870091
},
"institution": [
{
"name": "medRxiv"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2021,
10,
27
]
]
},
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2021.10.26.21265512",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2021,
10,
27
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2021,
10,
27
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference": [
{
"DOI": "10.1016/s22132600(21)00160-0",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.1"
},
{
"DOI": "10.1016/S0140-6736(21)01744-X",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.2"
},
{
"DOI": "10.1242/dmm.046581",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.3"
},
{
"DOI": "10.1016/j.celrep.2021.109518",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.4"
},
{
"DOI": "10.1371/journal.ppat.1009759",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.5"
},
{
"DOI": "10.1038/nri2802",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.6"
},
{
"DOI": "10.1183/09031936.01.00228701",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.7"
},
{
"DOI": "10.3389/fimmu.2020.01205",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.8"
},
{
"DOI": "10.1097/01.mcp.0000146781.11092.0d",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.9"
},
{
"DOI": "10.1164/rccm.200506-859OC",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.10"
},
{
"DOI": "10.1164/rccm.201104-0597OC",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.11"
},
{
"DOI": "10.1183/13993003.00547-2020",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.12"
},
{
"DOI": "10.1080/17476348.2021.1850275",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.13"
},
{
"DOI": "10.1016/S2213-2600(21)00013-8",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.14"
},
{
"DOI": "10.1038/s41467-021-23267-w",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.15"
},
{
"DOI": "10.1038/s41586-020-2588-y",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.16"
},
{
"DOI": "10.1038/s41591-020-0901-9",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.17"
},
{
"DOI": "10.1038/s41587-020-0602-4",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.18"
},
{
"DOI": "10.1080/22221751.2020.1770129",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.19"
},
{
"DOI": "10.1152/ajplung.00126.2020",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.20"
},
{
"DOI": "10.1128/CMR.00014-10",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.21"
},
{
"DOI": "10.1126/science.abc6027",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.22"
},
{
"DOI": "10.1067/mai.2000.105712",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.23"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.24"
},
{
"DOI": "10.1016/S2213-2600(17)30217-5",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.25"
},
{
"DOI": "10.5603/ARM.a2021.0040",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.26"
},
{
"DOI": "10.1136/thoraxjnl-2020-216256",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.27"
},
{
"DOI": "10.1038/s41591-021-01292-y",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.28"
},
{
"DOI": "10.3389/fimmu.2018.02061",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.29"
},
{
"DOI": "10.3389/fimmu.2016.00609",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.30"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.31"
},
{
"DOI": "10.1016/j.jaci.2020.09.034",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.32"
},
{
"DOI": "10.1183/13993003.001302021",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.33"
},
{
"DOI": "10.1016/j.resinv.2014.03.004",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.34"
},
{
"DOI": "10.3390/ph3030514",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.35"
},
{
"DOI": "10.1016/j.it.2011.05.005",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.36"
},
{
"DOI": "10.3791/56413",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.37"
},
{
"DOI": "10.1126/sciimmunol.abg9873",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.38"
},
{
"DOI": "10.1038/s41591-020-1051-9",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.39"
},
{
"article-title": "Распределение собственных значений в некоторых ансамблях случайных матриц” [Distribution of eigenvalues for some sets of random matrices]",
"first-page": "507",
"journal-title": "Mat. Sb",
"key": "2021102907550968000_2021.10.26.21265512v1.40",
"volume": "72",
"year": "1967"
},
{
"DOI": "10.1088/1742-5468/2008/10/p10008",
"doi-asserted-by": "publisher",
"key": "2021102907550968000_2021.10.26.21265512v1.41"
}
],
"reference-count": 41,
"references-count": 41,
"relation": {},
"resource": {
"primary": {
"URL": "http://medrxiv.org/lookup/doi/10.1101/2021.10.26.21265512"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"subtype": "preprint",
"title": "Dampening of the respiratory cytokine storm is promoted by inhaled budesonide in patients with early COVID-19",
"type": "posted-content"
}