Convalescent Plasma for COVID-19: A multicenter, randomized clinical trial
et al., medRxiv, doi:10.1101/2020.08.26.20182444, ConPlas-19, NCT04345523, Sep 2020
Early terminated RCT with 81 hospitalized patients, 38 treated with convalescent plasma, showing lower progression with treatment.
|
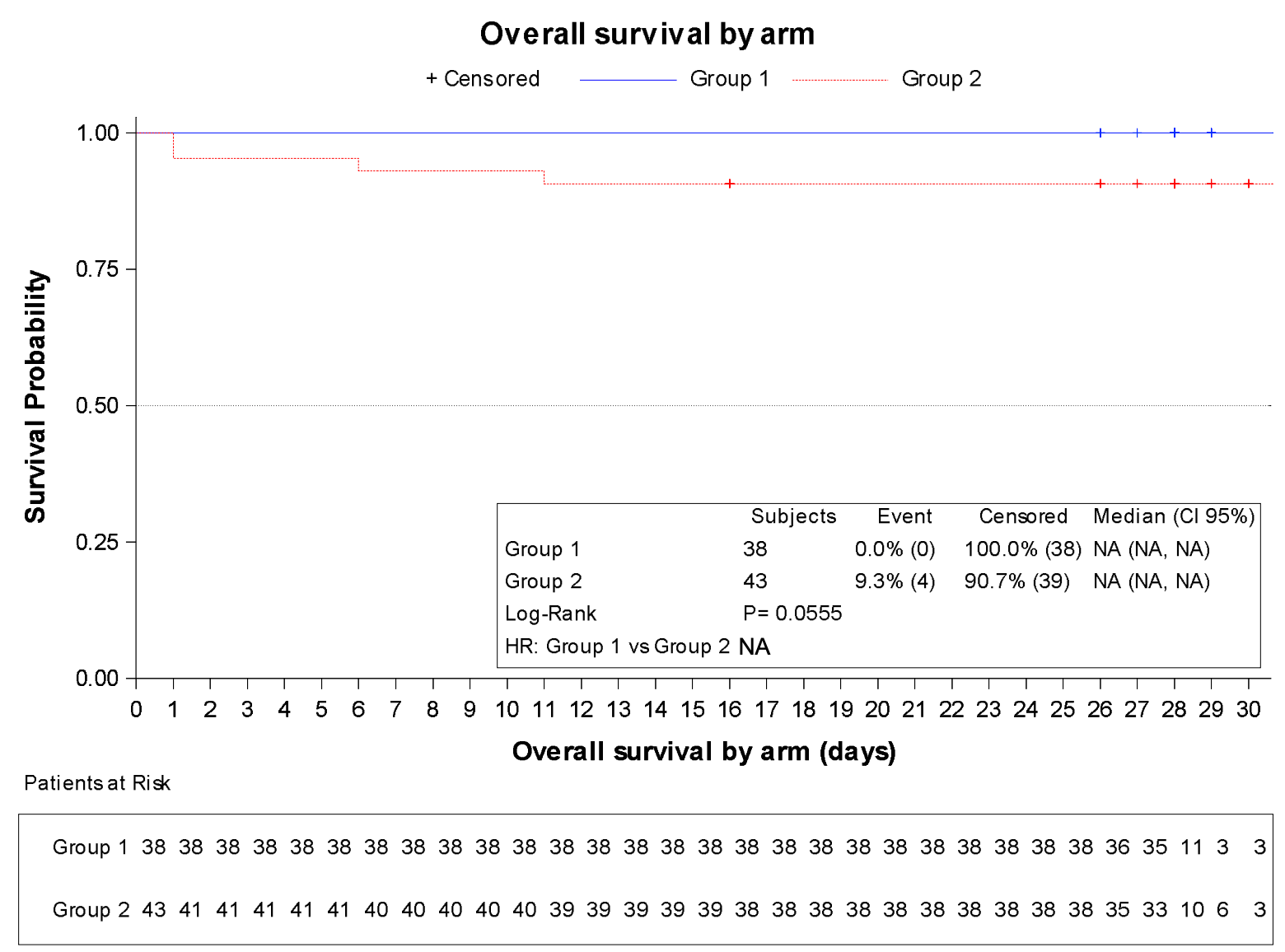
risk of death, 88.3% lower, RR 0.12, p = 0.12, treatment 0 of 38 (0.0%), control 4 of 43 (9.3%), NNT 11, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), day 29.
|
|
risk of progression, 93.0% lower, RR 0.07, p = 0.01, treatment 0 of 38 (0.0%), control 7 of 43 (16.3%), NNT 6.1, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), day 29, progression to categories 5-7.
|
|
risk of progression, 91.9% lower, RR 0.08, p = 0.03, treatment 0 of 38 (0.0%), control 6 of 43 (14.0%), NNT 7.2, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), day 15, progression to categories 5-7, primary outcome.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Avendaño-Solà et al., 29 Sep 2020, Randomized Controlled Trial, Spain, peer-reviewed, 38 authors, study period 4 April, 2020 - 10 July, 2020, average treatment delay 8.0 days, trial NCT04345523 (history) (ConPlas-19).
Convalescent Plasma for COVID-19: A multicenter, randomized clinical trial
doi:10.1101/2020.08.26.20182444
Background: Passive immunotherapy with convalescent plasma (CP) is a potential treatment for COVID-19 for which evidence from controlled clinical trials is lacking.
Methods: We conducted a multi-center, randomized clinical trial in patients hospitalized for COVID-19. All patients received standard of care treatment, including off-label use of marketed medicines, and were randomized 1:1 to receive one dose (250-300 mL) of CP from donors with IgG anti-SARS-CoV-2. The primary endpoint was the proportion of patients in categories 5, 6 or 7 of the COVID-19 ordinal scale at day 15.
Results: The trial was stopped after first interim analysis due to the fall in recruitment related to pandemic control. With 81 patients randomized, there were no patients progressing to mechanical ventilation or death among the 38 patients assigned to receive plasma (0%) versus 6 out of 43 patients (14%) progressing in control arm. Mortality rates were 0% vs 9.3% at days 15 and 29 for the active and control groups, respectively. No significant differences were found in secondary endpoints. At inclusion, patients had a median time of 8 days (IQR, 6-9) of symptoms and 49,4% of them were positive for anti-SARS-CoV-2 IgG antibodies.
Conclusions : Convalescent plasma could be superior to standard of care in avoiding progression to mechanical ventilation or death in hospitalized patients with COVID-19. The strong dependence of results on a limited number of events in the control group prevents drawing firm conclusions about CP efficacy from this trial. (Funded by Instituto de Salud Carlos III; NCT04345523). .
References
Beigel, Tomashek, Dodd, Remdesivir for the treatment of Covid-19 -preliminary report, N Engl J Med, doi:10.1056/NEJMoa2007764
Califf, Hernandez, Landray, Weighing the Benefits and Risks of Proliferating Observational Treatment Assessments.Observational Cacophony, Randomized Harmony, JAMA, doi:10.1001/jama.2020.13319
Cao, Wang, Wen, A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19, New England Journal of Medicine
Cavalcanti, Zampieri, Rosa, Hydroxychloroquine with or without Azithromycin in Mild-to-Moderate Covid-19, New England Journal of Medicine
Chen, Xiong, Bao, Shi, Convalescent plasma as a potential therapy for COVID-19, Lancet Infect Dis
Gharbharan, Jordans, Geurtsvankessel, Convalescent Plasma for COVID-19. A randomized clinical trial, Medrxiv
Joyner, Effect of Convalescent Plasma on Mortality among Hospitalized Patients with COVID-19: Initial Three-Month Experience, doi:10.1101/2020.08.12.20169359v1
Li, Zhang, Hu, Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial, JAMA. Published, doi:10.1001/jama.2020.10044
Mair-Jenkins, Saavedra-Campos, Baillie, The effectiveness of convalescent plasma and hyperimmune immunoglobulin for the treatment of severe acute respiratory infections of viral etiology: a systematic review and exploratory meta-analysis, J Infect Dis
Petkova, Antman, Troxel, Pooling Data From Individual Clinical Trials in the COVID-19 Era, JAMA Published Online, doi:10.1001/jama.2020.13042
DOI record:
{
"DOI": "10.1101/2020.08.26.20182444",
"URL": "http://dx.doi.org/10.1101/2020.08.26.20182444",
"abstract": "<jats:title>ABSTRACT</jats:title><jats:sec><jats:title>Background</jats:title><jats:p>Passive immunotherapy with convalescent plasma (CP) is a potential treatment for COVID-19 for which evidence from controlled clinical trials is lacking.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>We conducted a multi-center, randomized clinical trial in patients hospitalized for COVID-19. All patients received standard of care treatment, including off-label use of marketed medicines, and were randomized 1:1 to receive one dose (250-300 mL) of CP from donors with IgG anti-SARS-CoV-2. The primary endpoint was the proportion of patients in categories 5, 6 or 7 of the COVID-19 ordinal scale at day 15.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>The trial was stopped after first interim analysis due to the fall in recruitment related to pandemic control. With 81 patients randomized, there were no patients progressing to mechanical ventilation or death among the 38 patients assigned to receive plasma (0%) versus 6 out of 43 patients (14%) progressing in control arm. Mortality rates were 0% vs 9.3% at days 15 and 29 for the active and control groups, respectively. No significant differences were found in secondary endpoints. At inclusion, patients had a median time of 8 days (IQR, 6-9) of symptoms and 49,4% of them were positive for anti-SARS-CoV-2 IgG antibodies.</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>Convalescent plasma could be superior to standard of care in avoiding progression to mechanical ventilation or death in hospitalized patients with COVID-19. The strong dependence of results on a limited number of events in the control group prevents drawing firm conclusions about CP efficacy from this trial. (Funded by <jats:italic>Instituto de Salud Carlos III;</jats:italic><jats:ext-link xmlns:xlink=\"http://www.w3.org/1999/xlink\" ext-link-type=\"clintrialgov\" xlink:href=\"NCT04345523\">NCT04345523</jats:ext-link>).</jats:p></jats:sec>",
"accepted": {
"date-parts": [
[
2020,
9,
29
]
]
},
"author": [
{
"affiliation": [],
"family": "Avendaño-Solà",
"given": "C",
"sequence": "first"
},
{
"affiliation": [],
"family": "Ramos-Martínez",
"given": "A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Muñez-Rubio",
"given": "E",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ruiz-Antorán",
"given": "B",
"sequence": "additional"
},
{
"affiliation": [],
"family": "de Molina",
"given": "R Malo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Torres",
"given": "F",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fernández-Cruz",
"given": "A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Callejas-Díaz",
"given": "A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Calderón",
"given": "J",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Payares-Herrera",
"given": "C",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Salcedo",
"given": "I",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Romera",
"given": "I",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lora-Tamayo",
"given": "J",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mancheño-Losa",
"given": "M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Paciello",
"given": "ML",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Villegas",
"given": "C",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Estrada",
"given": "V",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Saez-Serrano",
"given": "I",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Porras-Leal",
"given": "ML",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jarilla-Fernández",
"given": "MC",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Paño-Pardo",
"given": "JR",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Moreno-Chulilla",
"given": "JA",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Arrieta-Aldea",
"given": "I",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bosch",
"given": "A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Belhassen-Garcia",
"given": "M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "López-Villar",
"given": "O",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ramos-Garrido",
"given": "A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Blanco",
"given": "L",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Madrigal-Sánchez",
"given": "ME",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Contreras",
"given": "E",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Muñiz-Díaz",
"given": "E",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Domingo-Morera",
"given": "JM",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Casas-Flecha",
"given": "I",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pérez-Olmeda",
"given": "M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Garcia-Pérez",
"given": "Javier",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alcamí",
"given": "J",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bueno",
"given": "JL",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Duarte",
"given": "RF",
"sequence": "additional"
},
{
"affiliation": [],
"name": "for the ConPlas-19 Study Group",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2020,
9,
1
]
],
"date-time": "2020-09-01T15:00:34Z",
"timestamp": 1598972434000
},
"deposited": {
"date-parts": [
[
2021,
2,
17
]
],
"date-time": "2021-02-17T22:11:15Z",
"timestamp": 1613599875000
},
"group-title": "Infectious Diseases (except HIV/AIDS)",
"indexed": {
"date-parts": [
[
2024,
1,
25
]
],
"date-time": "2024-01-25T05:24:26Z",
"timestamp": 1706160266511
},
"institution": [
{
"name": "medRxiv"
}
],
"is-referenced-by-count": 45,
"issued": {
"date-parts": [
[
2020,
9,
1
]
]
},
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2020.08.26.20182444",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2020,
9,
1
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2020,
9,
1
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference": [
{
"DOI": "10.1093/infdis/jiu396",
"doi-asserted-by": "publisher",
"key": "2021021307351449000_2020.08.26.20182444v3.1"
},
{
"DOI": "10.1056/NEJMoa2001282",
"article-title": "A Trial of Lopinavir–Ritonavir in Adults Hospitalized with Severe Covid-19",
"doi-asserted-by": "crossref",
"first-page": "1787",
"journal-title": "New England Journal of Medicine",
"key": "2021021307351449000_2020.08.26.20182444v3.2",
"volume": "382",
"year": "2020"
},
{
"key": "2021021307351449000_2020.08.26.20182444v3.3",
"unstructured": "Cavalcanti AB , Zampieri FG , Rosa RG , et al. Hydroxychloroquine with or without Azithromycin in Mild-to-Moderate Covid-19. New England Journal of Medicine 2020; published on July 23, 2020."
},
{
"DOI": "10.1056/NEJMoa2007764",
"doi-asserted-by": "publisher",
"key": "2021021307351449000_2020.08.26.20182444v3.4"
},
{
"key": "2021021307351449000_2020.08.26.20182444v3.5",
"unstructured": "RECOVERY Collaborative Group. Dexamethasone in Hospitalized Patients with Covid-19. New England Journal of Medicine 2020; published on July 17,2020."
},
{
"DOI": "10.1001/jama.2020.10044",
"doi-asserted-by": "publisher",
"key": "2021021307351449000_2020.08.26.20182444v3.6"
},
{
"key": "2021021307351449000_2020.08.26.20182444v3.7",
"unstructured": "Gharbharan A , Jordans C , GeurtsvanKessel C , et al. Convalescent Plasma for COVID-19. A randomized clinical trial. Medrxiv 2020: 2020.07.01.2013985 7v1."
},
{
"DOI": "10.1016/s1473-3099(20)30141-9",
"doi-asserted-by": "publisher",
"key": "2021021307351449000_2020.08.26.20182444v3.8"
},
{
"DOI": "10.1001/jama.2020.13319",
"doi-asserted-by": "publisher",
"key": "2021021307351449000_2020.08.26.20182444v3.9"
},
{
"key": "2021021307351449000_2020.08.26.20182444v3.10",
"unstructured": "European Commission. An EU programme of COVID-19 convalescent plasma collection and transfusion. Guidance on collection, testing, processing, storage, distribution and monitored use. Version 1.0 April 4 2020. Most updated version accessible at https://ec.europa.eu/health/blood_tissues_organs/covid-19_en."
},
{
"key": "2021021307351449000_2020.08.26.20182444v3.11",
"unstructured": "Center for Bio logics Evaluation and Research. Investigational COVID-19 Convalescent Plasma.Updated May 1, 2020. http://https://www.fda.gov/regulatory-information/search-fda-guidance-documents/investigational-covid-19-convalescent-plasma. Accessed August 22."
},
{
"key": "2021021307351449000_2020.08.26.20182444v3.12",
"unstructured": "Joyner MJ Effect of Convalescent Plasma on Mortality among Hospitalized Patients with COVID-19: Initial Three-Month Experience. https://www.medrxiv.org/content/10.1101/2020.08.12.20169359v1."
},
{
"DOI": "10.1001/jama.2020.13042",
"doi-asserted-by": "publisher",
"key": "2021021307351449000_2020.08.26.20182444v3.13"
}
],
"reference-count": 13,
"references-count": 13,
"relation": {},
"resource": {
"primary": {
"URL": "http://medrxiv.org/lookup/doi/10.1101/2020.08.26.20182444"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "Convalescent Plasma for COVID-19: A multicenter, randomized clinical trial",
"type": "posted-content"
}