The influence of physical activity level on the length of stay in hospital in older men survivors of COVID-19
et al., Sport Sciences for Health, doi:10.1007/s11332-022-00948-7, Jun 2022
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 39 hospitalized COVID-19 survivors >60 years old, showing shorter hospitalization for patients with active lifestyles before COVID-19 symptoms.
|
risk of ICU admission, 80.2% lower, RR 0.20, p = 0.06, high activity levels 1 of 14 (7.1%), low activity levels 9 of 25 (36.0%), NNT 3.5.
|
|
risk of miscellaneous, 40.5% lower, RR 0.60, p = 0.48, high activity levels 3 of 14 (21.4%), low activity levels 9 of 25 (36.0%), NNT 6.9, CT abnormalities >50%.
|
|
risk of miscellaneous, 72.5% lower, RR 0.27, p = 0.04, high activity levels 2 of 14 (14.3%), low activity levels 13 of 25 (52.0%), NNT 2.7, CT abnormalities 25-50%.
|
|
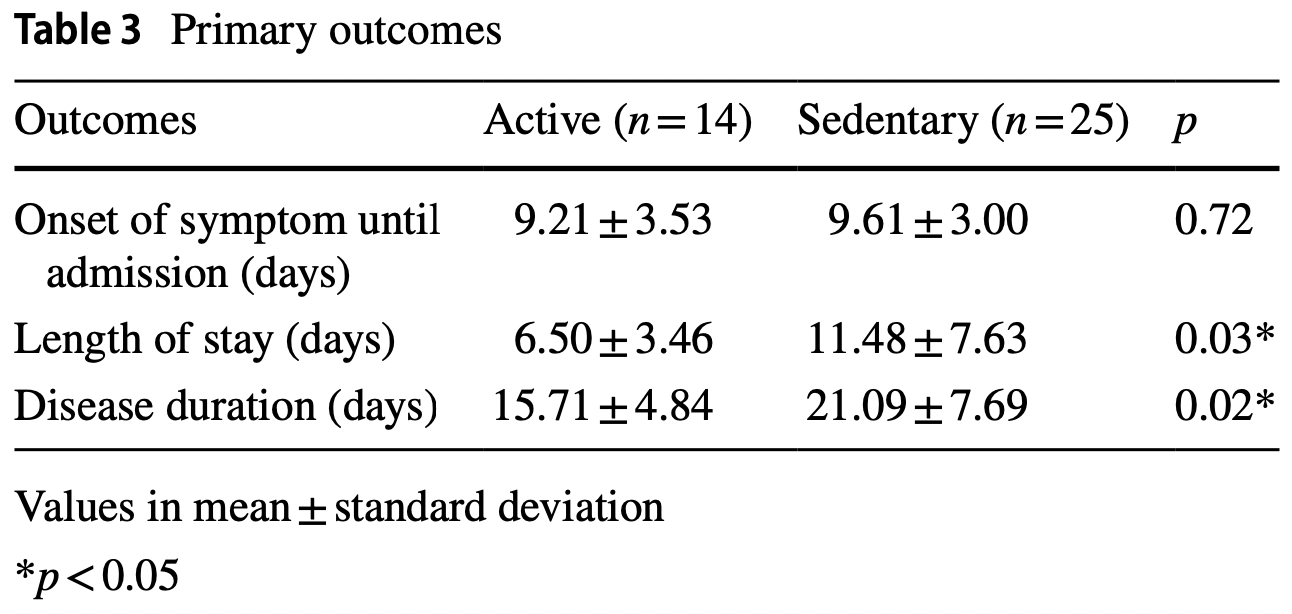
hospitalization time, 43.4% lower, relative time 0.57, p = 0.03, high activity levels 14, low activity levels 25.
|
|
miscellaneous, 25.5% lower, relative time 0.74, p = 0.02, high activity levels 14, low activity levels 25.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Antunes et al., 11 Jun 2022, retrospective, Brazil, peer-reviewed, survey, 5 authors, study period September 2020 - December 2020.
Contact: antunes.edher@gmail.com.
The influence of physical activity level on the length of stay in hospital in older men survivors of COVID-19
Sport Sciences for Health, doi:10.1007/s11332-022-00948-7
The purpose of this study was to verify the influence of physical activity level on the length of hospital stay in older men recovered from COVID-19. In total, 126 older men diagnosed with COVID-19 were admitted to the hospital between September and December 2020. Among them, 70 survived, of which 39 older men were included in the study. Within 30 days after discharge, patients answered the International Physical Activity Questionnaire to measure their physical activity level through phone contact, with questions corresponding to the week before symptom onset. Clinical and laboratorial data from admission, days between onset of symptoms and admission, length of stay, computed tomography abnormalities, and the need for the intensive care unit were collected. The groups (active × sedentary) were compared using the Student t test or Mann-Whitney test for quantitative data and chi-square test was used for categorical data. There is no difference between the groups in characteristics of admission (p > 0.05), except by potassium level. Active older men had a shorter length of stay (6.50 ± 3.46 vs 11.48 ± 7.63 days; p = 0.03), disease duration (15.71 ± 4.84 vs 21.09 ± 7.69 days; p = 0.02), and lower frequency of lung damage when compared to their sedentary counterparts. In conclusion, being physically active prior to infection can attenuate length of hospital stay in older men with COVID-19.
Declarations Conflict of interest The authors report no conflict of interest. Ethical approval This study was conducted in accordance with the recommendations from the Declaration of Helsinki.
Informed consent All participants provided informed consent prior to their participation. Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Brasil, Vigilância dos fatores de risco e proteção para doenças crônicas por inquérito telefônico: estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteção de doenças crônicas nas capitais dos 26 estados brasileiros e no Distrito Federal em
Campos, Costa, Pulmonary repercussions caused by the new Coronaviruses (COVID-19) and the use of invasive mechanical ventilation, J Health Biol Sci
Castañeda-Babarro, Arbillaga-Etxarri, Gutiérrez-Santamaría, Physical activity change during COVID-19 confinement, Int J Environ Res Public Health
Chu, Akl, Duda, Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis, Lancet
Cleland, Ferguson, Ellis, Validity of the International Physical Activity Questionnaire (IPAQ) for assessing moderate-to-vigorous physical activity and sedentary behavior of older adults in the United Kingdom, BMC Med Res Methodol
Costa, Costa, Barbosa-Filho, Vc, Influence of social distancing on the physical activity level during the COVID-19 pandemic, Rev Bras Ativ Fís Saúde
Echeverría-Esnal, Martin-Ontiyuelo, Navarrete-Rouco, Azithromycin in the treatment of COVID-19: a review, Expert Rev Anti Infect Ther
Fiuza-Laces, Santos-Lozano, Joyner, Exercise benefits in cardiovascular disease: beyond attenuation of traditional risk factors, Nat Rev Cardiol
Grande, Keogh, Silva, Exercise versus no exercise for the occurrence, severity, and duration of acute respiratory infections (Review), Cochrane Database Syst Rev, doi:10.1002/14651858.cd010596.pub.3
Hallal, Gomez, Parra, Lessons learned after 10 years of IPAQ use in Brazil and Colombia, J Phys Act Health
Hammer, Kivimaki, Gale, Batty, Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: a community-based cohort study of 387,109 adults in UK, Brain, Behav Immun
Hu, Huang, Yin, The cytokine storm and COVID-19, J Med Virol
Huang, Wang, Li, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Jahangiry, Farhangi, Shab-Bidar, Web-based physical activity interventions: a systematic review and metaanalysis of randomized controlled trials, Public Health
Javanmardi, Keshavarzi, Akbari, Prevalence of underlying diseases in died cases of COVID-19: a systematic review and meta-analysis, PLoS ONE
Kannan, Ali, Sheeza, COVID-19 (novel coronavirus 2019)-recent trends, Eur Rev Med Pharmacol Sci
Langsetmo, Bats, Cawthon, The association between objectively measured physical activity and subsequent health care utilization in older men, J Gerontol A Biol Sci Med Sci
Lee, Lee, Sy, Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study, Br J Sports Med, doi:10.1136/bjsports-2021-104203
Marino, Vargas, Skein, Metabolic and inflammatory health in SARS-CoV-2 and the potential role for habitual exercise in reducing disease severity, Inflamm Res, doi:10.1007/s00011-021-01517-3
Marques, Gheller, Physical activity during the COVID-19 pandemic: a survey with adults in Northern Brazil, Rev Bras Ativ Fís Saúde
Matias, Dominski, The COVID-19 pandemic challenges physical activity with two emerging paradigms, Rev Bras Ativ Fís Saúde
Matsudo, Araujo, Matsudo, International Physical Activity Questionnaire (IPAQ): study of validity and reliability in Brazil, Rev Bras Ativ Fís Saúde
Mesas, Redondo, Bueno, Predictors of in-hospital COVID-19 mortality: a comprehensive systematic review and meta-analysis exploring differences by age, sex and health conditions, PLoS ONE
Pedersen, Saltin, Exercise as medicine-evidence for prescribing exercise as therapy in 26 different chronic disease, Scand J Med Sci Sports
Peçanha, Goessler, Roschel, Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease, Am J Physiol Heart Circ Physiol
Pinto, Goessler, Fernandes, No independent associations between physical activity and clinical outcomes among hospitalized patients with moderate to severe COVID-19, J Sport Health Sci
Sallis, Young, Tartof, Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48440 adult patients, Br J Sports Med, doi:10.1136/bjsports-2021-104080
Simpson, Kay, Abbara, Radiological society of North America expert consensus document on reporting chest CT findings related to COVID-19: endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA, Cardiothorac Imaging
Siu, Campitelli, Kwong, Physical activity and Influenza-Coded outpatients visits, a population-based cohort study, PLoS ONE
Sjostrom, Ainsworth, Bauman, Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ)-short and long forms
Souza, Motta-Santos, Soares, Association of physical activity levels and the prevalence of COVID-19-associated hospitalization, J Sci Med Sport
Suzuki, Chronic inflammation as an immunological abnormality and effectiveness of exercise, Biomolecules
Tavakol, Ghannadi, Tabesh, Relationship between physical activity, healthy lifestyle and COVID-19 disease severity; a cross-sectional study, doi:10.1007/s10389-020-01468-9
Thompson, Joy, Jaworski, Exercise is Medicine, Am J Lifestyle Med
Udensi, Tchounwou, Potassium homeostasis, oxidative stress, and human disease, Int J Clin Exp Physiol
Woolcott, Ashe, Miller, Does physical activity reduce seniors' need for healthcare? A study of 24281 Canadians, Br J Sports Med
Yang, Zheng, Gou, Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis, Int J Infect Dis
Zheng, Peng, Xu, Risk factors of critical and mortal COVID-19 cases: a systematic literature review and meta-analysis, J Infect
DOI record:
{
"DOI": "10.1007/s11332-022-00948-7",
"ISSN": [
"1824-7490",
"1825-1234"
],
"URL": "http://dx.doi.org/10.1007/s11332-022-00948-7",
"alternative-id": [
"948"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "10 September 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "6 April 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "11 June 2022"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Conflict of interest",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "The authors report no conflict of interest."
},
{
"group": {
"label": "Ethical approval",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "This study was conducted in accordance with the recommendations from the Declaration of Helsinki."
},
{
"group": {
"label": "Informed consent",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "All participants provided informed consent prior to their participation."
},
{
"label": "Free to read",
"name": "free",
"value": "This content has been made available to all."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-0024-1563",
"affiliation": [],
"authenticated-orcid": false,
"family": "Antunes",
"given": "E. L.",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-1307-5039",
"affiliation": [],
"authenticated-orcid": false,
"family": "Costa",
"given": "B. M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4250-6416",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sochodolak",
"given": "R. C.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7324-4450",
"affiliation": [],
"authenticated-orcid": false,
"family": "Vargas",
"given": "L. M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8174-8501",
"affiliation": [],
"authenticated-orcid": false,
"family": "Okuno",
"given": "N. M.",
"sequence": "additional"
}
],
"container-title": "Sport Sciences for Health",
"container-title-short": "Sport Sci Health",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2022,
6,
11
]
],
"date-time": "2022-06-11T07:02:37Z",
"timestamp": 1654930957000
},
"deposited": {
"date-parts": [
[
2022,
6,
11
]
],
"date-time": "2022-06-11T08:09:43Z",
"timestamp": 1654934983000
},
"funder": [
{
"DOI": "10.13039/501100002322",
"doi-asserted-by": "publisher",
"name": "Coordenação de Aperfeiçoamento de Pessoal de Nível Superior"
}
],
"indexed": {
"date-parts": [
[
2022,
7,
8
]
],
"date-time": "2022-07-08T19:38:47Z",
"timestamp": 1657309127737
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
6,
11
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.springer.com/tdm",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
6,
11
]
],
"date-time": "2022-06-11T00:00:00Z",
"timestamp": 1654905600000
}
},
{
"URL": "https://www.springer.com/tdm",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
6,
11
]
],
"date-time": "2022-06-11T00:00:00Z",
"timestamp": 1654905600000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s11332-022-00948-7.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s11332-022-00948-7/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s11332-022-00948-7.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1007",
"published": {
"date-parts": [
[
2022,
6,
11
]
]
},
"published-online": {
"date-parts": [
[
2022,
6,
11
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"author": "C Huang",
"doi-asserted-by": "publisher",
"first-page": "497",
"journal-title": "Lancet",
"key": "948_CR1",
"unstructured": "Huang C, Wang Y, Li X et al (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395:497–506",
"volume": "395",
"year": "2020"
},
{
"author": "S Kannan",
"first-page": "2006",
"journal-title": "Eur Rev Med Pharmacol Sci",
"key": "948_CR2",
"unstructured": "Kannan S, Ali PSS, Sheeza A et al (2020) COVID-19 (novel coronavirus 2019)—recent trends. Eur Rev Med Pharmacol Sci 24:2006–2011",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.12662/2317-3076jhbs.v8i1.3185.p1-3.2020",
"author": "NG Campos",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Health Biol Sci",
"key": "948_CR3",
"unstructured": "Campos NG, Costa RF (2020) Pulmonary repercussions caused by the new Coronaviruses (COVID-19) and the use of invasive mechanical ventilation. J Health Biol Sci 8:1–3",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)31142-9",
"author": "DK Chu",
"doi-asserted-by": "publisher",
"first-page": "1973",
"journal-title": "Lancet",
"key": "948_CR4",
"unstructured": "Chu DK, Akl EA, Duda S et al (2020) Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet 395:1973–1987",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.12820/rbafs.25e0123",
"author": "CLA Costa",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Rev Bras Ativ Fís Saúde",
"key": "948_CR5",
"unstructured": "Costa CLA, Costa TM, Barbosa-Filho VC et al (2020) Influence of social distancing on the physical activity level during the COVID-19 pandemic. Rev Bras Ativ Fís Saúde 25:1–6",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.12820/rbafs.25e0151",
"author": "M Marques",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Rev Bras Ativ Fís Saúde",
"key": "948_CR6",
"unstructured": "Marques M, Gheller R, Henrique N et al (2020) Physical activity during the COVID-19 pandemic: a survey with adults in Northern Brazil. Rev Bras Ativ Fís Saúde 25:1–8",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.1152/ajpheart.00268.2020",
"author": "T Peçanha",
"doi-asserted-by": "publisher",
"first-page": "1441",
"journal-title": "Am J Physiol Heart Circ Physiol",
"key": "948_CR7",
"unstructured": "Peçanha T, Goessler KF, Roschel H et al (2020) Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am J Physiol Heart Circ Physiol 318:1441–1446",
"volume": "318",
"year": "2020"
},
{
"key": "948_CR8",
"unstructured": "Vigitel Brasil (2019) Vigilância dos fatores de risco e proteção para doenças crônicas por inquérito telefônico: estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteção de doenças crônicas nas capitais dos 26 estados brasileiros e no Distrito Federal em 2019. Ministério da Saúde, Secretaria de Vigilância em Saúde (BR)"
},
{
"DOI": "10.1177/1559827620912192",
"author": "WT Thompson",
"doi-asserted-by": "publisher",
"first-page": "511",
"journal-title": "Am J Lifestyle Med",
"key": "948_CR9",
"unstructured": "Thompson WT, Joy E, Jaworski CA et al (2020) Exercise is Medicine. Am J Lifestyle Med 14:511–523",
"volume": "14",
"year": "2020"
},
{
"author": "K Suzuki",
"first-page": "1",
"journal-title": "Biomolecules",
"key": "948_CR10",
"unstructured": "Suzuki K (2019) Chronic inflammation as an immunological abnormality and effectiveness of exercise. Biomolecules 223:1–11",
"volume": "223",
"year": "2019"
},
{
"author": "E Siu",
"first-page": "1",
"journal-title": "PLoS ONE",
"key": "948_CR11",
"unstructured": "Siu E, Campitelli MA, Kwong JC (2012) Physical activity and Influenza-Coded outpatients visits, a population-based cohort study. PLoS ONE 7:1–7",
"volume": "7",
"year": "2012"
},
{
"DOI": "10.1038/s41569-018-0065-1",
"author": "C Fiuza-Laces",
"doi-asserted-by": "publisher",
"first-page": "731",
"journal-title": "Nat Rev Cardiol",
"key": "948_CR12",
"unstructured": "Fiuza-Laces C, Santos-Lozano A, Joyner M et al (2018) Exercise benefits in cardiovascular disease: beyond attenuation of traditional risk factors. Nat Rev Cardiol 15:731–743",
"volume": "15",
"year": "2018"
},
{
"DOI": "10.1111/sms.12581",
"author": "BK Pedersen",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Scand J Med Sci Sports",
"key": "948_CR13",
"unstructured": "Pedersen BK, Saltin B (2015) Exercise as medicine—evidence for prescribing exercise as therapy in 26 different chronic disease. Scand J Med Sci Sports 25:1–72",
"volume": "25",
"year": "2015"
},
{
"DOI": "10.1371/journal.pone.0241265",
"author": "F Javanmardi",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "PLoS ONE",
"key": "948_CR14",
"unstructured": "Javanmardi F, Keshavarzi A, Akbari A et al (2020) Prevalence of underlying diseases in died cases of COVID-19: a systematic review and meta-analysis. PLoS ONE 15:1–13",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.03.017",
"author": "J Yang",
"doi-asserted-by": "publisher",
"first-page": "91",
"journal-title": "Int J Infect Dis",
"key": "948_CR15",
"unstructured": "Yang J, Zheng Y, Gou X et al (2020) Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis 94:91–95",
"volume": "94",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0241742",
"author": "AE Mesas",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "PLoS ONE",
"key": "948_CR16",
"unstructured": "Mesas AE, Redondo IC, Bueno CA et al (2020) Predictors of in-hospital COVID-19 mortality: a comprehensive systematic review and meta-analysis exploring differences by age, sex and health conditions. PLoS ONE 15:1–23",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2020.01.023",
"author": "Z Zheng",
"doi-asserted-by": "publisher",
"first-page": "17",
"journal-title": "J Infect",
"key": "948_CR17",
"unstructured": "Zheng Z, Peng F, Xu B et al (2020) Risk factors of critical and mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect 81:17–25",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.1016/j.bbi.2020.05.059",
"author": "M Hammer",
"doi-asserted-by": "publisher",
"first-page": "184",
"journal-title": "Brain, Behav Immun",
"key": "948_CR18",
"unstructured": "Hammer M, Kivimaki M, Gale CR, Batty G, D, (2020) Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: a community-based cohort study of 387,109 adults in UK. Brain, Behav Immun 87:184–187",
"volume": "87",
"year": "2020"
},
{
"DOI": "10.1136/bjsports-2021-104080",
"author": "R Sallis",
"doi-asserted-by": "publisher",
"journal-title": "Br J Sports Med",
"key": "948_CR19",
"unstructured": "Sallis R, Young DR, Tartof ST et al (2021) Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48440 adult patients. Br J Sports Med. https://doi.org/10.1136/bjsports-2021-104080",
"year": "2021"
},
{
"DOI": "10.1016/j.jsams.2021.05.011",
"author": "FR Souza",
"doi-asserted-by": "publisher",
"first-page": "913",
"journal-title": "J Sci Med Sport",
"key": "948_CR20",
"unstructured": "Souza FR, Motta-Santos D, Soares DS et al (2021) Association of physical activity levels and the prevalence of COVID-19-associated hospitalization. J Sci Med Sport 24:913–918",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1016/j.jshs.2021.08.001",
"author": "AJ Pinto",
"doi-asserted-by": "publisher",
"first-page": "690",
"journal-title": "J Sport Health Sci",
"key": "948_CR21",
"unstructured": "Pinto AJ, Goessler KF, Fernandes AL et al (2021) No independent associations between physical activity and clinical outcomes among hospitalized patients with moderate to severe COVID-19. J Sport Health Sci 10:690–696",
"volume": "10",
"year": "2021"
},
{
"author": "S Matsudo",
"first-page": "5",
"journal-title": "Rev Bras Ativ Fís Saúde",
"key": "948_CR22",
"unstructured": "Matsudo S, Araujo T, Matsudo V et al (2001) International Physical Activity Questionnaire (IPAQ): study of validity and reliability in Brazil. Rev Bras Ativ Fís Saúde 6:5–18",
"volume": "6",
"year": "2001"
},
{
"DOI": "10.1123/jpah.7.s2.s259",
"author": "PC Hallal",
"doi-asserted-by": "publisher",
"first-page": "259",
"journal-title": "J Phys Act Health",
"key": "948_CR23",
"unstructured": "Hallal PC, Gomez LF, Parra DC et al (2010) Lessons learned after 10 years of IPAQ use in Brazil and Colombia. J Phys Act Health 7:259–264",
"volume": "7",
"year": "2010"
},
{
"key": "948_CR24",
"unstructured": "Sjostrom M, Ainsworth B, Bauman A et al (2005) Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ)—short and long forms"
},
{
"author": "S Simpson",
"first-page": "1",
"journal-title": "Cardiothorac Imaging",
"key": "948_CR25",
"unstructured": "Simpson S, Kay FU, Abbara S et al (2020) Radiological society of North America expert consensus document on reporting chest CT findings related to COVID-19: endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Cardiothorac Imaging 2:1–10",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.1136/bjsm.2008.057216",
"author": "JC Woolcott",
"doi-asserted-by": "publisher",
"first-page": "902",
"journal-title": "Br J Sports Med",
"key": "948_CR26",
"unstructured": "Woolcott JC, Ashe MC, Miller MC et al (2010) Does physical activity reduce seniors’ need for healthcare? A study of 24281 Canadians. Br J Sports Med 44:902–904",
"volume": "44",
"year": "2010"
},
{
"DOI": "10.1093/gerona/glx191",
"author": "L Langsetmo",
"doi-asserted-by": "publisher",
"first-page": "820",
"journal-title": "J Gerontol A Biol Sci Med Sci",
"key": "948_CR27",
"unstructured": "Langsetmo L, Bats AM, Cawthon PM et al (2019) The association between objectively measured physical activity and subsequent health care utilization in older men. J Gerontol A Biol Sci Med Sci 74:820–826",
"volume": "74",
"year": "2019"
},
{
"DOI": "10.1002/14651858.cd010596.pub.3",
"author": "AJ Grande",
"doi-asserted-by": "publisher",
"journal-title": "Cochrane Database Syst Rev",
"key": "948_CR28",
"unstructured": "Grande AJ, Keogh J, Silva V et al (2020) Exercise versus no exercise for the occurrence, severity, and duration of acute respiratory infections (Review). Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.cd010596.pub.3",
"year": "2020"
},
{
"DOI": "10.1007/s10389-020-01468-9",
"author": "Z Tavakol",
"doi-asserted-by": "publisher",
"journal-title": "Z Gesundh Wiss",
"key": "948_CR29",
"unstructured": "Tavakol Z, Ghannadi S, Tabesh MR et al (2021) Relationship between physical activity, healthy lifestyle and COVID-19 disease severity; a cross-sectional study. Z Gesundh Wiss. https://doi.org/10.1007/s10389-020-01468-9",
"year": "2021"
},
{
"DOI": "10.1513/AnnalsATS.202002-183OC",
"author": "B Assouline",
"doi-asserted-by": "publisher",
"journal-title": "Ann Am Thorac Soc",
"key": "948_CR30",
"unstructured": "Assouline B, Cools E, Schorer R et al (2020) Preoperative exercise training to prevent postoperative pulmonary complications in adults undergoing major surgery: a systematic review and meta-analysis with trial sequential analysis. Ann Am Thorac Soc. https://doi.org/10.1513/AnnalsATS.202002-183OC",
"year": "2020"
},
{
"DOI": "10.1111/ijn.12134",
"author": "JG Hoogerdujin",
"doi-asserted-by": "publisher",
"first-page": "106",
"journal-title": "Int J Nurs Pract",
"key": "948_CR31",
"unstructured": "Hoogerdujin JG, Grobbee DE, Schuurmans MJ (2014) Prevention of functional decline in older hospitalized patients, nurses should play a key role in safe and adequate care. Int J Nurs Pract 20:106–113",
"volume": "20",
"year": "2014"
},
{
"DOI": "10.1093/gerona/63.10.1076",
"author": "P Kortebein",
"doi-asserted-by": "publisher",
"first-page": "1076",
"journal-title": "J Gerontol A Biol Sci Med Sci",
"key": "948_CR32",
"unstructured": "Kortebein P, Symons TB, Ferrando A et al (2008) Functional impact of 10 days of bed rest in healthy older adults. J Gerontol A Biol Sci Med Sci 63:1076–1081",
"volume": "63",
"year": "2008"
},
{
"DOI": "10.1111/j.1532-5415.2009.02393.x",
"author": "CJ Brown",
"doi-asserted-by": "publisher",
"first-page": "1660",
"journal-title": "J Am Geriatr Soc",
"key": "948_CR33",
"unstructured": "Brown CJ, Redden DT, Flood KL et al (2009) The underrecognized epidemic of low mobility during hospitalization of older adults. J Am Geriatr Soc 57:1660–1665",
"volume": "57",
"year": "2009"
},
{
"DOI": "10.1097/SLA.0b013e3181cf811d",
"author": "CP Snowden",
"doi-asserted-by": "publisher",
"first-page": "531",
"journal-title": "Ann Surg",
"key": "948_CR34",
"unstructured": "Snowden CP, Prentis J, Anderson HL et al (2010) Submaximal cardiopulmonary exercise testing predicts complications and hospital length of stay in patients undergoing major elective surgery. Ann Surg 251:531–535",
"volume": "251",
"year": "2010"
},
{
"DOI": "10.1097/SLA.0b013e31828dbac2",
"author": "CP Snowden",
"doi-asserted-by": "publisher",
"first-page": "999",
"journal-title": "Ann Surg",
"key": "948_CR35",
"unstructured": "Snowden CP, Prentis J, Jacques B et al (2013) Cardiorespiratory fitness predicts mortality and hospital length of stay after major elective surgery in older people. Ann Surg 257:999–1004",
"volume": "257",
"year": "2013"
},
{
"DOI": "10.1111/bju.12895",
"author": "S Tolchard",
"doi-asserted-by": "publisher",
"first-page": "554",
"journal-title": "BJU Int",
"key": "948_CR36",
"unstructured": "Tolchard S, Angell J, Pyke M et al (2015) Cardiopulmonary reserve as determined by cardiopulmonary exercise testing correlates with length of stay and predicts complications after radical cystectomy. BJU Int 115:554–561",
"volume": "115",
"year": "2015"
},
{
"DOI": "10.1093/icvts/ivw152",
"author": "RS Garcia",
"doi-asserted-by": "publisher",
"first-page": "486",
"journal-title": "Interact Cardiovasc Thorac Surg",
"key": "948_CR37",
"unstructured": "Garcia RS, Brage MIY, Moolhuyzen EG et al (2016) Functional and postoperative outcomes after preoperative exercise training in patients with lung cancer: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg 23:486–497",
"volume": "23",
"year": "2016"
},
{
"DOI": "10.4314/ahs.v18i1.16",
"author": "SMA El-Kader",
"doi-asserted-by": "publisher",
"first-page": "120",
"journal-title": "Afr Health Sci",
"key": "948_CR38",
"unstructured": "El-Kader SMA, Al-Shreef FM (2018) Inflammatory cytokines and immune system modulation by aerobic versus resisted exercise training for elderly. Afr Health Sci 18:120–131",
"volume": "18",
"year": "2018"
},
{
"DOI": "10.1016/j.jshs.2018.09.009",
"author": "DC Nieman",
"doi-asserted-by": "publisher",
"first-page": "201",
"journal-title": "J Sport Health Sci",
"key": "948_CR39",
"unstructured": "Nieman DC, Wentz LM (2019) The compelling link between physical activity and the body’s defense system. J Sport Health Sci 8:201–217",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.3389/fimmu.2018.02187",
"author": "M Sellami",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Front Immunol",
"key": "948_CR40",
"unstructured": "Sellami M, Gasmi M, Denham J et al (2018) Effects of acute and chronic exercise on immunological parameters in the elderly aged: can physical activity counteract the effects of aging? Front Immunol 9:1–17",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1016/bs.pmbts.2015.08.001",
"author": "RJ Simpson",
"doi-asserted-by": "publisher",
"first-page": "355",
"journal-title": "Prog Mol Biol Transl Sci",
"key": "948_CR41",
"unstructured": "Simpson RJ, Kunz H, Agha N et al (2015) Exercise and the regulation of immune functions. Prog Mol Biol Transl Sci 135:355–380",
"volume": "135",
"year": "2015"
},
{
"DOI": "10.1016/S2468-2667(17)30075-0",
"author": "M Elovainio",
"doi-asserted-by": "publisher",
"first-page": "260",
"journal-title": "Lance Public Health",
"key": "948_CR42",
"unstructured": "Elovainio M, Hakulinen C, Pulkki-Raback L et al (2017) Contribuition of risk factors to excess mortality in isolated and lonely individuals: an analysis of data from the UK Biobank cohort study. Lance Public Health 6:260–266",
"volume": "6",
"year": "2017"
},
{
"DOI": "10.3390/jpm10030080",
"author": "AO Ferreira",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Pers Med",
"key": "948_CR43",
"unstructured": "Ferreira AO, Polonini HC, Dijkers ECF (2020) Postulated adjuvant therapeutic strategies for COVID-19. J Pers Med 10:1–33",
"volume": "10",
"year": "2020"
},
{
"author": "X Yao",
"first-page": "2015",
"journal-title": "Vaccine",
"key": "948_CR44",
"unstructured": "Yao X, Hamilton RG, Wen N et al (2011) Frailty is associated with impairment of vaccine-induced antibody response and increase in post-vaccination influenza infection in community-dwelling older adults. Vaccine 23:2015–2021",
"volume": "23",
"year": "2011"
},
{
"DOI": "10.3389/fphys.2021.675778",
"author": "LU Pagan",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Front Physiol",
"key": "948_CR45",
"unstructured": "Pagan LU, Gomes MJ, Damatto RL et al (2021) Aerobic exercise during advance stage of uncontrolled arterial hypertension. Front Physiol 12:1–10",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1111/jch.12597",
"author": "TP Paula",
"doi-asserted-by": "publisher",
"first-page": "895",
"journal-title": "J Clin Hypertens",
"key": "948_CR46",
"unstructured": "Paula TP, Viana LV, Neto ATZ et al (2015) Effects of the DASH diet and walking on blood pressure in patients with type 2 diabetes and uncontrolled hypertension: a randomized controlled trial. J Clin Hypertens 17:895–901",
"volume": "17",
"year": "2015"
},
{
"DOI": "10.2147/DMSO.S262289",
"author": "AD Wake",
"doi-asserted-by": "publisher",
"first-page": "2909",
"journal-title": "Diabetes Metab Syndr Obes",
"key": "948_CR47",
"unstructured": "Wake AD (2020) Antidiabetic effects of physical activity: how it helps to control type 2 diabetes. Diabetes Metab Syndr Obes 13:2909–2923",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1177/0004563220922255",
"author": "G Lippi",
"doi-asserted-by": "publisher",
"first-page": "262",
"journal-title": "Ann Clin Biochem",
"key": "948_CR48",
"unstructured": "Lippi G, South AM, Henry BM (2020) Electrolyte imbalances in patients with severe coronavirus disease 2019 (COVID-19). Ann Clin Biochem 57:262–265",
"volume": "57",
"year": "2020"
},
{
"author": "UK Udensi",
"first-page": "111",
"journal-title": "Int J Clin Exp Physiol",
"key": "948_CR49",
"unstructured": "Udensi UK, Tchounwou PB (2017) Potassium homeostasis, oxidative stress, and human disease. Int J Clin Exp Physiol 43:111–122",
"volume": "43",
"year": "2017"
},
{
"DOI": "10.1056/NEJMoa2021436",
"author": "Recovery Collaborative Group",
"doi-asserted-by": "publisher",
"first-page": "693",
"journal-title": "N Engl J Med",
"key": "948_CR50",
"unstructured": "Recovery Collaborative Group (2021) Dexamethasone in hospitalized patients with COVID-19—preliminary report. N Engl J Med 384:693–704",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1080/14787210.2020.1813024",
"author": "D Echeverría-Esnal",
"doi-asserted-by": "publisher",
"first-page": "147",
"journal-title": "Expert Rev Anti Infect Ther",
"key": "948_CR51",
"unstructured": "Echeverría-Esnal D, Martin-Ontiyuelo C, Navarrete-Rouco ME et al (2021) Azithromycin in the treatment of COVID-19: a review. Expert Rev Anti Infect Ther 19:147–163",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1136/bjsports-2021-104203",
"author": "SW Lee",
"doi-asserted-by": "publisher",
"journal-title": "Br J Sports Med",
"key": "948_CR52",
"unstructured": "Lee SW, Lee J, Moon SY et al (2021) Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study. Br J Sports Med. https://doi.org/10.1136/bjsports-2021-104203",
"year": "2021"
},
{
"DOI": "10.1002/jmv.26232",
"author": "B Hu",
"doi-asserted-by": "publisher",
"first-page": "250",
"journal-title": "J Med Virol",
"key": "948_CR53",
"unstructured": "Hu B, Huang S, Yin L (2021) The cytokine storm and COVID-19. J Med Virol 93:250–256",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1007/s00011-021-01517-3",
"author": "FE Marino",
"doi-asserted-by": "publisher",
"journal-title": "Inflamm Res",
"key": "948_CR54",
"unstructured": "Marino FE, Vargas NT, Skein M et al (2021) Metabolic and inflammatory health in SARS-CoV-2 and the potential role for habitual exercise in reducing disease severity. Inflamm Res. https://doi.org/10.1007/s00011-021-01517-3",
"year": "2021"
},
{
"DOI": "10.12820/rbafs.25e0113",
"author": "TS Matias",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Rev Bras Ativ Fís Saúde",
"key": "948_CR55",
"unstructured": "Matias TS, Dominski FH (2020) The COVID-19 pandemic challenges physical activity with two emerging paradigms. Rev Bras Ativ Fís Saúde 25:1–6",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.1016/j.puhe.2017.06.005",
"author": "L Jahangiry",
"doi-asserted-by": "publisher",
"first-page": "36",
"journal-title": "Public Health",
"key": "948_CR56",
"unstructured": "Jahangiry L, Farhangi MA, Shab-Bidar S et al (2017) Web-based physical activity interventions: a systematic review and meta-analysis of randomized controlled trials. Public Health 152:36–46",
"volume": "152",
"year": "2017"
},
{
"DOI": "10.1186/s12874-018-0642-3",
"author": "C Cleland",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "BMC Med Res Methodol",
"key": "948_CR57",
"unstructured": "Cleland C, Ferguson S, Ellis G et al (2018) Validity of the International Physical Activity Questionnaire (IPAQ) for assessing moderate-to-vigorous physical activity and sedentary behavior of older adults in the United Kingdom. BMC Med Res Methodol 18:1–12",
"volume": "18",
"year": "2018"
},
{
"author": "A Castañeda-Babarro",
"first-page": "1",
"journal-title": "Int J Environ Res Public Health",
"key": "948_CR58",
"unstructured": "Castañeda-Babarro A, Arbillaga-Etxarri A, Gutiérrez-Santamaría B et al (2021) Physical activity change during COVID-19 confinement. Int J Environ Res Public Health 17:1–10",
"volume": "17",
"year": "2021"
}
],
"reference-count": 58,
"references-count": 58,
"relation": {},
"resource": {
"primary": {
"URL": "https://link.springer.com/10.1007/s11332-022-00948-7"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Orthopedics and Sports Medicine"
],
"subtitle": [],
"title": "The influence of physical activity level on the length of stay in hospital in older men survivors of COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy"
}
