Vitamin D deficiency and SARS-CoV-2 infection: Big-data analysis from March 2020 to March 2021. D-COVID study
et al., bioRxiv, doi:10.1101/2022.10.27.514012, Oct 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
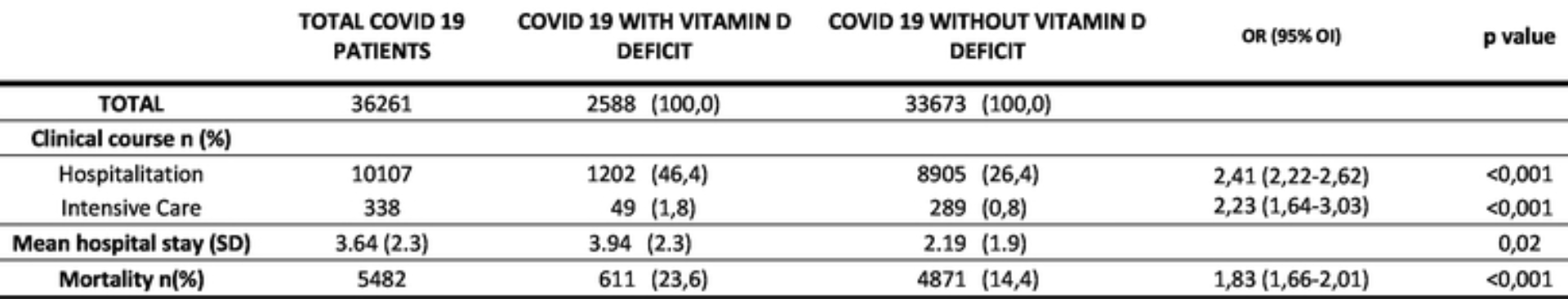
Retrospective free-text analysis of 143,157 COVID-19 patients, showing vitamin D deficiency associated with mortality, ICU admission, and hospitalization in unadjusted results.
This is the 146th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
This study is excluded in the after exclusion results of meta-analysis:
unadjusted results with no group details.
|
risk of death, 38.8% lower, RR 0.61, p < 0.001, high D levels 4,871 of 33,673 (14.5%), low D levels 611 of 2,588 (23.6%), NNT 11, inverted to make RR<1 favor high D levels, odds ratio converted to relative risk.
|
|
risk of ICU admission, 54.7% lower, RR 0.45, p < 0.001, high D levels 289 of 33,673 (0.9%), low D levels 49 of 2,588 (1.9%), NNT 97, inverted to make RR<1 favor high D levels, odds ratio converted to relative risk.
|
|
risk of hospitalization, 43.0% lower, RR 0.57, p < 0.001, high D levels 8,905 of 33,673 (26.4%), low D levels 1,202 of 2,588 (46.4%), NNT 5.0, inverted to make RR<1 favor high D levels, odds ratio converted to relative risk.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Álvarez et al., 28 Oct 2022, retrospective, Spain, preprint, 1 author, study period March 2020 - March 2021.
Contact: noemi.anguita@salud.madrid.org.
Vitamin D deficiency and SARS‑CoV‑2 infection: Big-data analysis from March 2020 to March 2021. D-COVID study
doi:10.1101/2022.10.27.514012
Background: Vitamin D has been proposed to have immunomodulatory functions and therefore play a role in coronavirus infection . However, there is no conclusive evidence on its impact on COVID-19 infection and evolution. Objective: To study the association between COVID-19 infection and vitamin D deficiency in patients of a terciary university hospital. To investigate the clinical evolution and prognosis of patients with COVID-19 and vitamin D deficiency. Methods: Using big-data analytics and artificial intelligence through the SAVANA Manager clinical platform, we analysed clinical data from patients with COVID-19 atended in a terciary university hospital from March 2020 to March 2021. Results: Of the 143.157 analysed patients, 36.261 subjects had COVID-19 infection (25.33%); during this period; of these 2588 had vitamin D deficiency (7.14%). Among subjects with COVID-19 and vitamin D deficiency, there was a higher proportion of women OR 1.45 [95% CI 1.33-1.57], adults older than 80 years OR 2.63 [95%CI 2.38-2.91], people living in nursing homes OR 2.88 [95%CI 2.95-3.45] and walking dependence OR 3.45 [95%CI 2.85-4.26]. Regarding clinical course, a higher number of subjects with COVID-19 and vitamin D deficiency required hospitalitation OR 2.41 [95%CI 2.22-2-61], intensive unit care (ICU) OR 2.22 [95% CI 1.64-3.02], had a longer mean hospital stay 3.94 (2.29) p=0.02 and higher mortality OR 1.82 [95%CI 1.66-2.01].) Conclusion: Low serum 25 (OH) Vitamin-D level was significantly associated with a worse clinical evolution and prognosis of COVID-19 infection. We found a higher proportion of institutionalised and dependent people over 80 years of age among patients with COVID-19 and vitamin D deficiency.
DECLARATIONS
Competing interests: Benavent Nuñez M, Parralejo Jimenez A, López Yepes G report that the y are employees at Medsavana. There are no other financial competing interests regarding this paper. Funding: There are no non-financial competing interests.
References
Baeza-Yates, Ribeiro-Neto, Modern Information Retrieval
Benson, Principles of Health Interoperability HL7 and SNOMED
Charan, Goyal, Saxena, Yadav, Vitamin D for prevention of respiratory tract infections: A systematic review and meta-analysis, Journal of Pharmacology and Pharmacotherapeutics, doi:10.4103/0976-500X.103685
Crafa, Cannarella, Condorelli, Mongioì, Barbagallo et al., Influence of 25-hydroxy-cholecalciferol levels on SARS-CoV-2 infection and COVID-19 severity: A systematic review and meta-analysis, EClinicalMedicine, doi:10.1016/j.eclinm.2021.100967
Diaz-Curiel, Cabello, Arboiro-Pinel, Mansur, Heili-Frades et al., The relationship between 25(OH) vitamin D levels and COVID-19 onset and disease course in Spanish patients, Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2021.105928
Driggin, Madhavan, Gupta, The role of vitamin D in cardiovascular disease and COVID-19, Reviews in Endocrine and Metabolic Disorders, doi:10.1007/s11154-021-09674-w
Ebadi, Montano-Loza, Perspective: improving vitamin D status in the management of COVID-19, European Journal of Clinical Nutrition, doi:10.1038/s41430-020-0661-0
González-Molero, Morcillo, Valdes, Pérez, Valero et al., Vitamin D deficiency in Spain: a population-based cohort study 1 Vitamin D deficiency in Spain: a population-based cohort study, European Journal of Clinical Nutrition, doi:10.1038/ejcn.2010.265ï
Holick, Medical Progress Vitamin D Deficiency, N Engl J Med
Israel, Cicurel, Feldhamer, Stern, Dror et al., Vitamin D deficiency is associated with higher risks for SARS-CoV-2 infection and COVID-19 severity: a retrospective case-control study, Internal and Emergency Medicine, doi:10.1007/s11739-021-02902-w
Laird, Rhodes, Kenny, Vitamin D and Inflammation: Potential Implications for Severity of Covid-19, Ir Med J
Larrosa, Gratacòs, Vaqueiro, Prat, Campos et al., Valoración del tratamiento sustitutivo, Revista Medicina clínica, doi:10.1016/S0025-7753(01)72195-1
Lips, Cashman, Lamberg-Allardt, Bischoff-Ferrari, Obermayer-Pietsch et al., Current Vitamin D status in European and Middle East countries and strategies to prevent Vitamin D deficiency: A position statement of the European Calcified Tissue Society, European Journal of Endocrinology, doi:10.1530/EJE-18-0736
Mateo-Pascual, Julián-Viñals, Alarcón-Alarcón, Castell-Alcalá, Ictoria et al., Vitamin D deficiency in a cohort over 65 years: prevalence and association with sociodemographic and health factors, Revista Española de Geriatría y Gerontología, doi:10.1016/j.regg.2013.11.004
Merzon, Tworowski, Gorohovski, Vinker, Golan Cohen et al., Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study, FEBS Journal, doi:10.1111/febs.15495
Panagiotou, Tee, Ihsan, Athar, Marchitelli et al., Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity, Clinical Endocrinology, doi:10.1111/cen.14276
Sabetta, Depetrillo, Cipriani, Smardin, Burns et al., Serum 25-hydroxyvitamin D and the incidence of acute viral respiratory tract infections in healthy adults, PLoS ONE, doi:10.1371/journal.pone.0011088
Sabetta, Depetrillo, Cipriani, Smardin, Burns et al., Serum 25-hydroxyvitamin D and the incidence of acute viral respiratory tract infections in healthy adults, PLoS ONE, doi:10.1371/journal.pone.0011088
Von Elm, Altman, Egger, Pocock, Gøtzsche et al., The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies, International Journal of Surgery, doi:10.1016/j.ijsu.2014.07.013
Xu, Baylink, Chen, Reeves, Xiao et al., The importance of Vitamin D metabolism as a potential prophylactic, immunoregulatory and neuroprotective treatment for COVID-19, Journal of Translational Medicine, doi:10.1186/s12967-020-02488-5
Ye, Tang, Liao, Shaw, Deng et al., Does Serum Vitamin D Level Affect COVID-19 Infection and Its Severity?-A Case-Control Study, Journal of the American College of Nutrition, doi:10.1080/07315724.2020.1826005
DOI record:
{
"DOI": "10.1101/2022.10.27.514012",
"URL": "http://dx.doi.org/10.1101/2022.10.27.514012",
"abstract": "<jats:p>Methods: Using big-data analytics and artificial intelligence through the SAVANA Manager clinical platform, we analysed clinical data from patients with COVID-19 atended in a terciary university hospital from March 2020 to March 2021. Results: Of the 143.157 analysed patients, 36.261 subjects had COVID-19 infection (25.33%); during this period; of these 2588 had vitamin D deficiency (7.14%). Among subjects with COVID-19 and vitamin D deficiency, there was a higher proportion of women OR 1.45 [95% CI 1.33-1.57], adults older than 80 years OR 2.63 [95%CI 2.38-2.91], people living in nursing homes OR 2.88 [95%CI 2.95-3.45] and walking dependence OR 3.45 [95%CI 2.85-4.26]. Regarding clinical course, a higher number of subjects with COVID-19 and vitamin D deficiency required hospitalitation OR 2.41 [95%CI 2.22-2-61], intensive unit care (ICU) OR 2.22 [95% CI 1.64-3.02], had a longer mean hospital stay 3.94 (2.29) p=0.02 and higher mortality OR 1.82 [95%CI 1.66-2.01].) Conclusion: Low serum 25 (OH) Vitamin-D level was significantly associated with a worse clinical evolution and prognosis of COVID-19 infection. We found a higher proportion of institutionalised and dependent people over 80 years of age among patients with COVID-19 and vitamin D deficiency.</jats:p>",
"accepted": {
"date-parts": [
[
2022,
10,
27
]
]
},
"author": [
{
"ORCID": "http://orcid.org/0000-0002-8753-7040",
"affiliation": [],
"authenticated-orcid": false,
"family": "Anguita",
"given": "Noemi",
"sequence": "first"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
10,
28
]
],
"date-time": "2022-10-28T14:10:11Z",
"timestamp": 1666966211000
},
"deposited": {
"date-parts": [
[
2022,
10,
28
]
],
"date-time": "2022-10-28T14:10:11Z",
"timestamp": 1666966211000
},
"group-title": "Pathology",
"indexed": {
"date-parts": [
[
2022,
10,
29
]
],
"date-time": "2022-10-29T05:03:18Z",
"timestamp": 1667019798160
},
"institution": [
{
"name": "bioRxiv"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
10,
28
]
]
},
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2022.10.27.514012",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2022,
10,
28
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2022,
10,
28
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "http://biorxiv.org/lookup/doi/10.1101/2022.10.27.514012"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "Vitamin D deficiency and SARS-CoV-2 infection: Big-data analysis from March 2020 to March 2021. D-COVID study",
"type": "posted-content"
}
