Angiotensin converting enzyme 2 gene expression and markers of oxidative stress are correlated with disease severity in patients with COVID-19
et al., Molecular Biology Reports, doi:10.1007/s11033-023-08515-0, May 2023
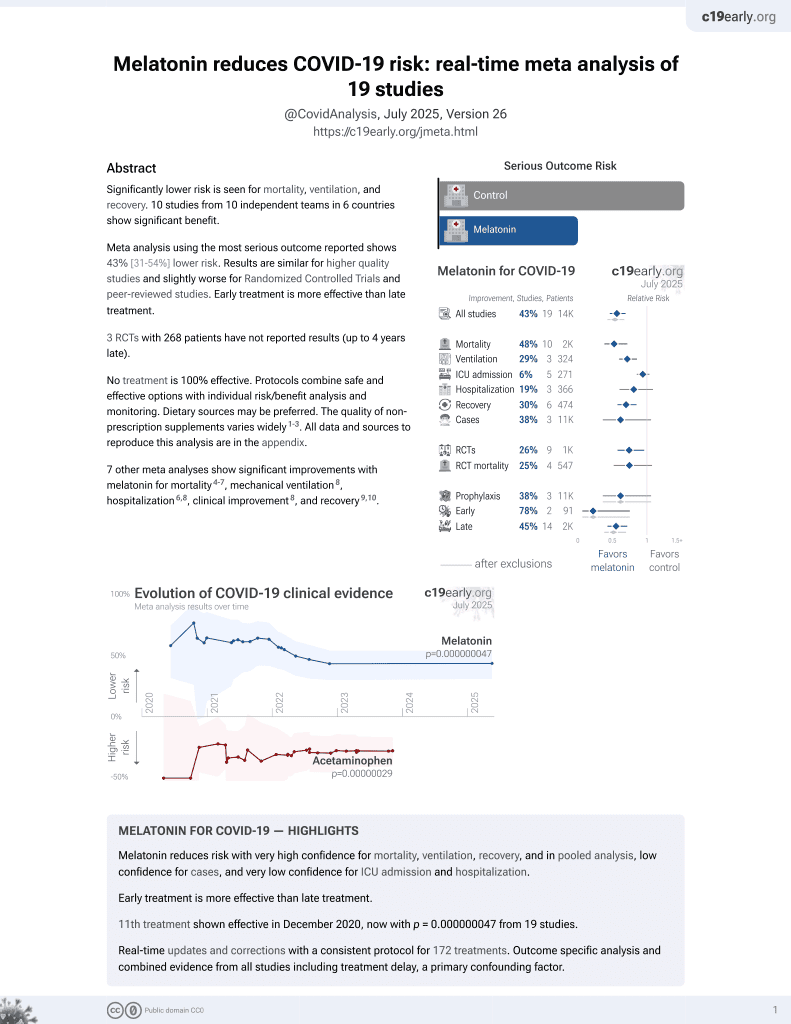
Melatonin for COVID-19
12th treatment shown to reduce risk in
December 2020, now with p = 0.0000000099 from 19 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
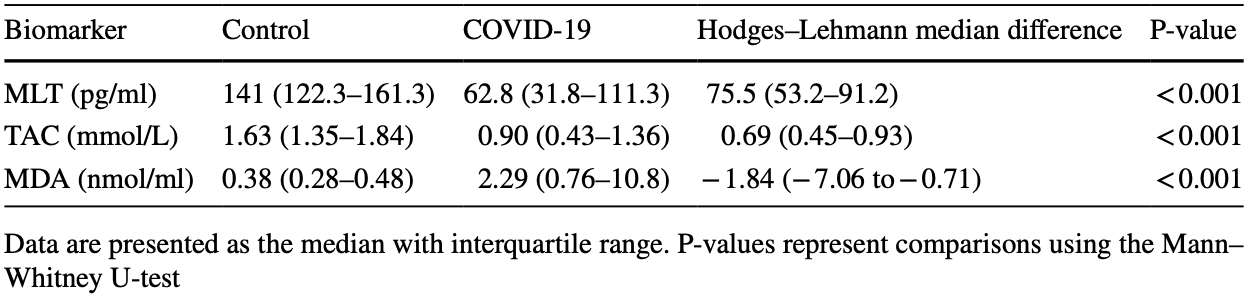
Analysis of 40 COVID-19 ICU patients and 40 matched healthy controls, showing significantly lower melatonin levels in COVID-19 patients.
Alobaidy et al., 24 May 2023, Egypt, peer-reviewed, mean age 60.7, 6 authors, study period September 2021 - March 2022.
Contact: elmissiry@mans.edu.eg, aiothman@mans.edu.eg, afraaalmkhtar@std.mans.edu.eg, dr_mona_elhelali@mans.edu.eg, maggieelsied@mans.edu.eg, rashasamirtaha@gmail.com.
Angiotensin converting enzyme 2 gene expression and markers of oxidative stress are correlated with disease severity in patients with COVID-19
Molecular Biology Reports, doi:10.1007/s11033-023-08515-0
Background Oxidative stress is thought to play a significant role in the pathogenesis and severity of COVID-19. Additionally, angiotensin converting enzyme 2 (ACE2) expression may predict the severity and clinical course of COVID-19. Accordingly, the aim of the present study was to evaluate the association of oxidative stress and ACE2 expression with the clinical severity in patients with COVID-19.
Methods and results The present study comprised 40 patients with COVID-19 and 40 matched healthy controls, recruited between September 2021 and March 2022. ACE 2 expression levels were measured using Hera plus SYBR Green qPCR kits with GAPDH used as an internal control. Serum melatonin (MLT) levels, serum malondialdehyde (MDA) levels, and total antioxidant capacity (TAC) were estimated using ELISA. The correlations between the levels of the studied markers and clinical indicators of disease severity were evaluated. Significantly, lower expression of ACE2 was observed in COVID-19 patients compared to controls. Patients with COVID-19 had lower serum levels of TAC and MLT but higher serum levels of MDA compared to normal controls. Serum MDA levels were correlated with diastolic blood pressure (DBP), Glasgow coma scale (GCS) scores, and serum potassium levels. Serum MLT levels were positively correlated with DBP, mean arterial pressure (MAP), respiratory rate, and serum potassium levels. TAC was correlated with GCS, mean platelet volume, and serum creatinine levels. Serum MLT levels were significantly lower in patients treated with remdesivir and inotropes. Receiver operating characteristic curve analysis demonstrates that all markers had utility in discriminating COVID-19 patients from healthy controls. Conclusions Increased oxidative stress and increased ACE2 expression were correlated with disease severity and poor outcomes in hospitalized patients with COVID-19 in the present study. Melatonin supplementation may provide a utility as an adjuvant therapy in decreasing disease severity and death in COVID-19 patients.
Author contributions All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by ASA, MEE, MEA, RSS, AIO, MAEM. The first draft of the manuscript was written and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. Funding Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Data availability All data generated or analyzed during this study are included in this published article.
Declarations Conflict of interest The authors declare that they have no conflict of interest to declare.
Ethics approval The study protocol was carried according to Institutional Ethics Committee of Mansoura University, Egypt (approval number sci-Z-ph-2021-60) which performed in compliance with the ethical guidelines outlined in the 1964 Helsinki Declaration. Patients have signed informed consent form.
Consent to participate Not applicable.
Consent to publish Not applicable. Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Biancatelli, Berrill, Mohammed, Marik, Melatonin for the treatment of sepsis: the scientific rationale, J Thorac Dis, doi:10.21037/jtd.2019.12.85
Camini, Da, Caetano, Almeida, De et al., Implications of oxidative stress on viral pathogenesis, Arch Virol, doi:10.1007/s00705-016-3187-y
Chuang, Shiesh, Chi, Tu, Hor et al., Serum total antioxidant capacity reflects severity of illness in patients with severe sepsis, Crit Care, doi:10.1186/cc4826
Cook, Ausiello, Functional ACE2 deficiency leading to angiotensin imbalance in the pathophysiology of COVID-19, Rev Endocr Metab Disord, doi:10.1007/s11154-021-09663-z
Cunnane, Manku, Oka, Horrobin, Enhanced vascular reactivity to various vasoconstrictor agents following pinealectomy in the rat: role of melatonin, Can J Physiol Pharmacol, doi:10.1139/y80-049
Darif, Hammi, Kihel, Idrissi, Guessous et al., The pro-inflammatory cytokines in COVID-19 pathogenesis: what goes wrong?, Microb Pathog, doi:10.1016/j.micpath.2021.104799
De Las, Giménez, Ferder, Manucha, Lahera, Implications of oxidative stress and potential role of mitochondrial dysfunction in COVID-19: therapeutic effects of vitamin D, Antioxidants, doi:10.3390/antiox9090897
Delgado-Roche, Mesta, Oxidative stress as key player in severe acute respiratory syndrome coronavirus (SARS-CoV) infection, Arch Med Res, doi:10.1016/j.arcmed.2020.04.019
El-Missiry, El-Missiry, Othman, Melatonin is a potential adjuvant to improve clinical outcomes in individuals with obesity and diabetes with coexistence of Covid-19, Eur J Pharmacol, doi:10.1016/j.ejphar.2020.173329
El-Missiry, Othman, Melatonin is a potential adjuvant to improve clinical outcomes in individuals with obesity and diabetes with coexistence of Covid-19, Eur J Pharmacol, doi:10.1016/j.ejphar.2020.173329
El-Sokkary, Reiter, Cuzzocrea, Caputi, Hassanein et al., Role of melatonin in reduction of lipid peroxidation and peroxynitrite formation in non-septic shock induced by zymosan, Shock, doi:10.1097/00024382-199911000-00009
Gheblawi, Viveiros, Nguyen, Zhong, Turner et al., Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system: celebrating the 20th anniversary of the discovery of ACE2, Circ Res, doi:10.1161/circresaha.120.317015
Giovannini, Chiarla, Giuliante, Pallavicini, Vellone et al., Serum uric acid, creatinine, and the assessment of antioxidant capacity in critical illness, Crit Care, doi:10.1186/cc5008
Herwig, Tsokos, Hermanns, Kirkpatrick, Müller, Vascular endothelial cadherin expression in lung specimens of patients with sepsis-induced acute respiratory distress syndrome and endothelial cell cultures, Pathobiology, doi:10.1159/000347062
Hoffmann, Kleine-Weber, Schroeder, Krüger, Herrler et al., SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and Is blocked by a clinically proven protease inhibitor, Cell, doi:10.1016/j.cell.2020.02.052
Hu, Huang, Yin, The cytokine storm and COVID-19, J Med Virol, doi:10.1002/jmv.26232
Ivanov, Bartosch, Isaguliants, Oxidative stress in infection and consequent disease, Oxid Med Cell Longev, doi:10.1155/2017/3496043
Jackson, Farzan, Chen, Choe, Mechanisms of SARS-CoV-2 entry into cells, Nat Rev Mol Cell Biol, doi:10.1038/s41580-021-00418-x
Karkhanei, Ghane, Mehri, Evaluation of oxidative stress level: total antioxidant capacity, total oxidant status and glutathione activity in patients with COVID-19, New Microbes New Infect, doi:10.1016/j.nmni.2021.100897
Kerekes, Arkossy, Altorjay, Huszka, Kappelmayer et al., Evaluation of hemostatic changes and blood antioxidant capacity in acute and chronic pancreatitis, Hepatogastroenterology
Kim, Kim, Ryu, Kim, Park et al., Reactive oxygen species induce antiviral innate immune response through IFN-λ regulation in human nasal epithelial cells, Am J Respir Cell Mol Biol, doi:10.1165/rcmb.2013-0003OC
Korniluk, Koper-Lenkiewicz, Kamińska, Kemona, Dymicka-Piekarska, Mean platelet volume (MPV): new perspectives for an old marker in the course and prognosis of inflammatory conditions, Mediators Inflamm, doi:10.1155/2019/9213074
Krause, Geary, Doolen, Duckles, Melatonin and cardiovascular function, Adv Exp Med Biol
Kuba, Imai, Rao, Gao, Guo et al., A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury, Nat Med, doi:10.1038/nm1267
Lan, Ge, Yu, Shan, Zhou et al., Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor, Nature, doi:10.1038/s41586-020-2180-5
Lippi, Henry, Favaloro, Mean platelet volume predicts severe COVID-19 illness, Semin Thromb Hemost, doi:10.1055/s-0041-1727283
Liu, Li, Long, Zeng, Gao et al., Bilirubin levels as potential indicators of disease severity in coronavirus disease patients: a retrospective cohort study, Front Med (Lausanne), doi:10.3389/fmed.2020.598870
Lorente, Martín, Almeida, Abreu-González, Ferreres et al., Association between serum total antioxidant capacity and mortality in severe septic patients, J Crit Care, doi:10.1016/j.jcrc.2014.09.012
Mariappan, Manoharan, Shanmugam, Rao, Pillai, Potential biomarkers for the early prediction of SARS-COV-2 disease outcome, Microb Pathog, doi:10.1016/j.micpath.2021.105057
Mariappan, Ranganadin, Shanmugam, Rao, Pillai, Early shedding of membrane-bounded ACE2 could be an indicator for disease severity in SARS-CoV-2, Biochimie, doi:10.1016/j.biochi.2022.06.005
Mariappan, Rr, Pillai, Angiotensin-converting enzyme 2: a protective factor in regulating disease virulence of SARS-COV-2, IUBMB Life, doi:10.1002/iub.2391
Mehri, Rahbar, Ghane, Souri, Esfahani, Changes in oxidative markers in COVID-19 patients, Arch Med Res, doi:10.1016/j.arcmed.2021.06.004
Mehta, Mcauley, Brown, Sanchez, Tattersall et al., COVID-19: consider cytokine storm syndromes and immunosuppression, Lancet, doi:10.1016/s0140-6736(20)30628-0
Morgan, Liu, Crosstalk of reactive oxygen species and NF-κB signaling, Cell Res, doi:10.1038/cr.2010.178
Mp, COVID-19 infection and oxidative stress: an under-explored approach for prevention and treatment?, Pan Afr Med J, doi:10.11604/pamj.2020.35.2.22877
Muhammad, Kani, Iliya, Muhammad, Binji et al., Deficiency of antioxidants and increased oxidative stress in COVID-19 patients: a cross-sectional comparative study in Jigawa, Northwestern Nigeria SAGE Open Med, doi:10.1177/2050312121991246
Nanduri, Yuan, Kumar, Semenza, Prabhakar, Transcriptional responses to intermittent hypoxia, Respir Physiol Neurobiol, doi:10.1016/j.resp.2008.07.006
Neoptolemos, Kemppainen, Mayer, Fitzpatrick, Raraty et al., Early prediction of severity in acute pancreatitis by urinary trypsinogen activation peptide: a multicentre study, Lancet, doi:10.1016/s0140-6736(00)02327-8
Oostwoud, Gunasinghe, Seow, Ye, Selemidis et al., Apocynin and ebselen reduce influenza A virus-induced lung inflammation in cigarette smoke-exposed mice, Sci Rep, doi:10.1038/srep20983
Ozdinc, Oz, Ozdemir, Kilic, Karakaya et al., Melatonin: is it an effective antioxidant for pulmonary contusion?, J Surg Res, doi:10.1016/j.jss.2016.05.020
Pagliaro, Penna, ACE/ACE2 ratio: a key also in 2019 coronavirus disease (Covid-19, Front Med (Lausanne), doi:10.3389/fmed.2020.00335
Paliogiannis, Zinellu, Bilirubin levels in patients with mild and severe Covid-19: a pooled analysis, Liver Int, doi:10.1111/liv.14477
Rabaan, Sh, Muhammad, Khan, Sule et al., Role of inflammatory cytokines in COVID-19 patients: a review on molecular mechanisms, immune functions immunopathology and immunomodulatory drugs to counter cytokine storm, Vaccines, doi:10.3390/vaccines9050436
Rieder, Wirth, Pollmeier, Jeserich, Goller et al., Serum ACE2, angiotensin II, and aldosterone levels are unchanged in patients with COVID-19, Am J Hypertens, doi:10.1093/ajh/hpaa169
Schmittgen, Livak, Analyzing real-time PCR data by the comparative C(T) method, Nat Protoc, doi:10.1038/nprot.2008.73
Shemies, Nagy, Younis, Sheashaa, Renal replacement therapy for critically ill patients with COVID-19-associated acute kidney injury: a review of current knowledge, Ther Apher Dial, doi:10.1111/1744-9987.13723
Shereen, Khan, Kazmi, Bashir, Siddique, COVID-19 infection: origin, transmission, and characteristics of human coronaviruses, J Adv Res, doi:10.1016/j.jare.2020.03.005
Sies, Stahl, Sundquist, Antioxidant functions of vitamins. Vitamins E and C, beta-carotene, and other carotenoids, Ann N Y Acad Sci, doi:10.1111/j.1749-6632.1992.tb17085.x
Ucar, Korkmaz, Reiter, Yaren, Oter et al., Melatonin alleviates lung damage induced by the chemical warfare agent nitrogen mustard, Toxicol Lett, doi:10.1016/j.toxlet.2007.07.005
Van Boheemen, De Graaf, Lauber, Bestebroer, Raj et al., Genomic characterization of a newly discovered coronavirus associated with acute respiratory distress syndrome in humans, doi:10.1128/mBio.00473-12
Vieira, Nery, Martins, Jabour, Dias et al., Downregulation of membrane-bound angiotensin converting enzyme 2 (ACE2) receptor has a pivotal role in COVID-19 immunopathology, Curr Drug Targets, doi:10.2174/1389450121666201020154033
Yaghoubi, Youssefi, Azad, Farzad, Yavari et al., Total antioxidant capacity as a marker of severity of COVID-19 infection: possible prognostic and therapeutic clinical application, J Med Virol, doi:10.1002/jmv.27500
Yan, Zhang, Li, Xia, Guo et al., Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2, Science, doi:10.1126/science.abb2762
Zein, Raffaello, Effect of colchicine on mortality in patients with COVID-19-a systematic review and meta-analysis, Diabetes Metab Syndr, doi:10.1016/j.dsx.2022.102395
Zhang, Li, Niu, ACE2 and COVID-19 and the resulting ARDS, Postgrad Med J, doi:10.1136/postgradmedj-2020-137935
Zhong, Peng, Mean platelet volume/platelet count ratio predicts severe pneumonia of COVID-19, J Clin Lab Anal, doi:10.1002/jcla.23607
Zhu, Zheng, Liu, Comparison of COVID-19 and lung cancer via reactive oxygen species signaling, Front Oncol, doi:10.3389/fonc.2021.708263
DOI record:
{
"DOI": "10.1007/s11033-023-08515-0",
"ISSN": [
"0301-4851",
"1573-4978"
],
"URL": "http://dx.doi.org/10.1007/s11033-023-08515-0",
"abstract": "<jats:title>Abstract</jats:title><jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>Oxidative stress is thought to play a significant role in the pathogenesis and severity of COVID-19. Additionally, angiotensin converting enzyme 2 (ACE2) expression may predict the severity and clinical course of COVID-19. Accordingly, the aim of the present study was to evaluate the association of oxidative stress and ACE2 expression with the clinical severity in patients with COVID-19.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Methods and results</jats:title>\n <jats:p>The present study comprised 40 patients with COVID-19 and 40 matched healthy controls, recruited between September 2021 and March 2022. ACE 2 expression levels were measured using Hera plus SYBR Green qPCR kits with GAPDH used as an internal control. Serum melatonin (MLT) levels, serum malondialdehyde (MDA) levels, and total antioxidant capacity (TAC) were estimated using ELISA. The correlations between the levels of the studied markers and clinical indicators of disease severity were evaluated. Significantly, lower expression of ACE2 was observed in COVID-19 patients compared to controls. Patients with COVID-19 had lower serum levels of TAC and MLT but higher serum levels of MDA compared to normal controls. Serum MDA levels were correlated with diastolic blood pressure (DBP), Glasgow coma scale (GCS) scores, and serum potassium levels. Serum MLT levels were positively correlated with DBP, mean arterial pressure (MAP), respiratory rate, and serum potassium levels. TAC was correlated with GCS, mean platelet volume, and serum creatinine levels. Serum MLT levels were significantly lower in patients treated with remdesivir and inotropes. Receiver operating characteristic curve analysis demonstrates that all markers had utility in discriminating COVID-19 patients from healthy controls.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Conclusions</jats:title>\n <jats:p>Increased oxidative stress and increased ACE2 expression were correlated with disease severity and poor outcomes in hospitalized patients with COVID-19 in the present study. Melatonin supplementation may provide a utility as an adjuvant therapy in decreasing disease severity and death in COVID-19 patients.</jats:p>\n </jats:sec>",
"alternative-id": [
"8515"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "22 January 2023"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "10 May 2023"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "24 May 2023"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Conflict of interest",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "The authors declare that they have no conflict of interest to declare."
},
{
"group": {
"label": "Ethics approval",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "The study protocol was carried according to Institutional Ethics Committee of Mansoura University, Egypt (approval number sci-Z-ph-2021–60) which performed in compliance with the ethical guidelines outlined in the 1964 Helsinki Declaration. Patients have signed informed consent form."
},
{
"group": {
"label": "Consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "Not applicable."
},
{
"group": {
"label": "Consent to publish",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 5,
"value": "Not applicable."
}
],
"author": [
{
"affiliation": [],
"family": "Alobaidy",
"given": "Afraa S. H.",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-8612-4247",
"affiliation": [],
"authenticated-orcid": false,
"family": "Elhelaly",
"given": "Mona",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2012-9154",
"affiliation": [],
"authenticated-orcid": false,
"family": "Amer",
"given": "Maggie E.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0770-8023",
"affiliation": [],
"authenticated-orcid": false,
"family": "Shemies",
"given": "Rasha S.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8624-1259",
"affiliation": [],
"authenticated-orcid": false,
"family": "Othman",
"given": "Azza I.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4566-0497",
"affiliation": [],
"authenticated-orcid": false,
"family": "El-Missiry",
"given": "Mohamed A.",
"sequence": "additional"
}
],
"container-title": "Molecular Biology Reports",
"container-title-short": "Mol Biol Rep",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2023,
5,
24
]
],
"date-time": "2023-05-24T06:02:06Z",
"timestamp": 1684908126000
},
"deposited": {
"date-parts": [
[
2023,
5,
24
]
],
"date-time": "2023-05-24T06:12:28Z",
"timestamp": 1684908748000
},
"funder": [
{
"DOI": "10.13039/501100009367",
"doi-asserted-by": "crossref",
"name": "Mansoura University"
}
],
"indexed": {
"date-parts": [
[
2023,
5,
25
]
],
"date-time": "2023-05-25T04:14:47Z",
"timestamp": 1684988087920
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
5,
24
]
]
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
5,
24
]
],
"date-time": "2023-05-24T00:00:00Z",
"timestamp": 1684886400000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
5,
24
]
],
"date-time": "2023-05-24T00:00:00Z",
"timestamp": 1684886400000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s11033-023-08515-0.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s11033-023-08515-0/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s11033-023-08515-0.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1007",
"published": {
"date-parts": [
[
2023,
5,
24
]
]
},
"published-online": {
"date-parts": [
[
2023,
5,
24
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1016/j.jare.2020.03.005",
"author": "MA Shereen",
"doi-asserted-by": "publisher",
"first-page": "91",
"journal-title": "J Adv Res",
"key": "8515_CR1",
"unstructured": "Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R (2020) COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res 24:91–98. https://doi.org/10.1016/j.jare.2020.03.005",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1128/mBio.00473-12",
"doi-asserted-by": "publisher",
"key": "8515_CR2",
"unstructured": "van Boheemen S, de Graaf M, Lauber C, Bestebroer TM, Raj VS, Zaki AM, Osterhaus AD, Haagmans BL, Gorbalenya AE, Snijder EJ, Fouchier RA (2012) Genomic characterization of a newly discovered coronavirus associated with acute respiratory distress syndrome in humans. mBio. doi: https://doi.org/10.1128/mBio.00473-12"
},
{
"DOI": "10.1038/s41580-021-00418-x",
"author": "CB Jackson",
"doi-asserted-by": "publisher",
"first-page": "3",
"journal-title": "Nat Rev Mol Cell Biol",
"key": "8515_CR3",
"unstructured": "Jackson CB, Farzan M, Chen B, Choe H (2022) Mechanisms of SARS-CoV-2 entry into cells. Nat Rev Mol Cell Biol 23:3–20. https://doi.org/10.1038/s41580-021-00418-x",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"author": "M Hoffmann",
"doi-asserted-by": "publisher",
"first-page": "271",
"journal-title": "Cell",
"key": "8515_CR4",
"unstructured": "Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, Müller MA, Drosten C, Pöhlmann S (2020) SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and Is blocked by a clinically proven protease inhibitor. Cell 181:271-280.e8. https://doi.org/10.1016/j.cell.2020.02.052",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2180-5",
"author": "J Lan",
"doi-asserted-by": "publisher",
"first-page": "215",
"journal-title": "Nature",
"key": "8515_CR5",
"unstructured": "Lan J, Ge J, Yu J, Shan S, Zhou H, Fan S, Zhang Q, Shi X, Wang Q, Zhang L, Wang X (2020) Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature 581:215–220. https://doi.org/10.1038/s41586-020-2180-5",
"volume": "581",
"year": "2020"
},
{
"DOI": "10.1161/circresaha.120.317015",
"author": "WK Gheblawi",
"doi-asserted-by": "publisher",
"first-page": "1456",
"journal-title": "Circ Res",
"key": "8515_CR6",
"unstructured": "Gheblawi WK, Viveiros A, Nguyen Q, Zhong JC, Turner AJ, Raizada MK, Grant MB, Oudit GY (2020) Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system: celebrating the 20th anniversary of the discovery of ACE2. Circ Res 126:1456–1474. https://doi.org/10.1161/circresaha.120.317015",
"volume": "126",
"year": "2020"
},
{
"DOI": "10.1038/cr.2010.178",
"author": "MJ Morgan",
"doi-asserted-by": "publisher",
"first-page": "103",
"journal-title": "Cell Res",
"key": "8515_CR7",
"unstructured": "Morgan MJ, Liu ZG (2011) Crosstalk of reactive oxygen species and NF-κB signaling. Cell Res 21:103–115. https://doi.org/10.1038/cr.2010.178",
"volume": "21",
"year": "2011"
},
{
"DOI": "10.1165/rcmb.2013-0003OC",
"author": "HJ Kim",
"doi-asserted-by": "publisher",
"first-page": "855",
"journal-title": "Am J Respir Cell Mol Biol",
"key": "8515_CR8",
"unstructured": "Kim HJ, Kim CH, Ryu JH, Kim MJ, Park CY, Lee JM, Holtzman MJ, Yoon JH (2013) Reactive oxygen species induce antiviral innate immune response through IFN-λ regulation in human nasal epithelial cells. Am J Respir Cell Mol Biol 49:855–865. https://doi.org/10.1165/rcmb.2013-0003OC",
"volume": "49",
"year": "2013"
},
{
"DOI": "10.1155/2017/3496043",
"author": "AV Ivanov",
"doi-asserted-by": "publisher",
"first-page": "3496043",
"journal-title": "Oxid Med Cell Longev",
"key": "8515_CR9",
"unstructured": "Ivanov AV, Bartosch B, Isaguliants MG (2017) Oxidative stress in infection and consequent disease. Oxid Med Cell Longev 2017:3496043. https://doi.org/10.1155/2017/3496043",
"volume": "2017",
"year": "2017"
},
{
"DOI": "10.1038/srep20983",
"author": "LC Oostwoud",
"doi-asserted-by": "publisher",
"first-page": "20983",
"journal-title": "Sci Rep",
"key": "8515_CR10",
"unstructured": "Oostwoud LC, Gunasinghe P, Seow HJ, Ye JM, Selemidis S, Bozinovski S, Vlahos R (2016) Apocynin and ebselen reduce influenza A virus-induced lung inflammation in cigarette smoke-exposed mice. Sci Rep 6:20983. https://doi.org/10.1038/srep20983",
"volume": "6",
"year": "2016"
},
{
"DOI": "10.1097/00024382-199911000-00009",
"author": "GH El-Sokkary",
"doi-asserted-by": "publisher",
"first-page": "402",
"journal-title": "Shock",
"key": "8515_CR11",
"unstructured": "El-Sokkary GH, Reiter RJ, Cuzzocrea S, Caputi AP, Hassanein AF, Tan DX (1999) Role of melatonin in reduction of lipid peroxidation and peroxynitrite formation in non-septic shock induced by zymosan. Shock 12:402–408. https://doi.org/10.1097/00024382-199911000-00009",
"volume": "12",
"year": "1999"
},
{
"DOI": "10.1016/j.toxlet.2007.07.005",
"author": "M Ucar",
"doi-asserted-by": "publisher",
"first-page": "124",
"journal-title": "Toxicol Lett",
"key": "8515_CR12",
"unstructured": "Ucar M, Korkmaz A, Reiter RJ, Yaren H, Oter S, Kurt B, Topal T (2007) Melatonin alleviates lung damage induced by the chemical warfare agent nitrogen mustard. Toxicol Lett 173:124–131. https://doi.org/10.1016/j.toxlet.2007.07.005",
"volume": "173",
"year": "2007"
},
{
"DOI": "10.1016/j.arcmed.2021.06.004",
"author": "F Mehri",
"doi-asserted-by": "publisher",
"first-page": "843",
"journal-title": "Arch Med Res",
"key": "8515_CR13",
"unstructured": "Mehri F, Rahbar AH, Ghane ET, Souri B, Esfahani M (2021) Changes in oxidative markers in COVID-19 patients. Arch Med Res 52:843–849. https://doi.org/10.1016/j.arcmed.2021.06.004",
"volume": "52",
"year": "2021"
},
{
"DOI": "10.3390/vaccines9050436",
"author": "AA Rabaan",
"doi-asserted-by": "publisher",
"journal-title": "Vaccines (Basel)",
"key": "8515_CR14",
"unstructured": "Rabaan AA, Al-Ahmed SH, Muhammad J, Khan A, Sule AA, Tirupathi R, Mutair AA, Alhumaid S, Al-Omari A, Dhawan M, Tiwari R, Sharun K, Mohapatra RK, Mitra S, Bilal M, Alyami SA, Emran TB, Moni MA, Dhama K (2021) Role of inflammatory cytokines in COVID-19 patients: a review on molecular mechanisms, immune functions immunopathology and immunomodulatory drugs to counter cytokine storm. Vaccines (Basel). https://doi.org/10.3390/vaccines9050436",
"year": "2021"
},
{
"DOI": "10.1016/j.micpath.2021.104799",
"author": "D Darif",
"doi-asserted-by": "publisher",
"first-page": "104799",
"journal-title": "Microb Pathog",
"key": "8515_CR15",
"unstructured": "Darif D, Hammi I, Kihel A, El Idrissi SI, Guessous F, Akarid K (2021) The pro-inflammatory cytokines in COVID-19 pathogenesis: what goes wrong? Microb Pathog 153:104799. https://doi.org/10.1016/j.micpath.2021.104799",
"volume": "153",
"year": "2021"
},
{
"DOI": "10.1159/000347062",
"author": "MC Herwig",
"doi-asserted-by": "publisher",
"first-page": "245",
"journal-title": "Pathobiology",
"key": "8515_CR16",
"unstructured": "Herwig MC, Tsokos M, Hermanns MI, Kirkpatrick CJ, Müller AM (2013) Vascular endothelial cadherin expression in lung specimens of patients with sepsis-induced acute respiratory distress syndrome and endothelial cell cultures. Pathobiology 80:245–251. https://doi.org/10.1159/000347062",
"volume": "80",
"year": "2013"
},
{
"DOI": "10.1016/j.resp.2008.07.006",
"author": "J Nanduri",
"doi-asserted-by": "publisher",
"first-page": "277",
"journal-title": "Respir Physiol Neurobiol",
"key": "8515_CR17",
"unstructured": "Nanduri J, Yuan G, Kumar GK, Semenza GL, Prabhakar NR (2008) Transcriptional responses to intermittent hypoxia. Respir Physiol Neurobiol 164:277–281. https://doi.org/10.1016/j.resp.2008.07.006",
"volume": "164",
"year": "2008"
},
{
"DOI": "10.1016/s0140-6736(20)30628-0",
"author": "P Mehta",
"doi-asserted-by": "publisher",
"first-page": "1033",
"journal-title": "Lancet",
"key": "8515_CR18",
"unstructured": "Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ (2020) COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 395:1033–1034. https://doi.org/10.1016/s0140-6736(20)30628-0",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26232",
"author": "B Hu",
"doi-asserted-by": "publisher",
"first-page": "250",
"journal-title": "J Med Virol",
"key": "8515_CR19",
"unstructured": "Hu B, Huang S, Yin L (2021) The cytokine storm and COVID-19. J Med Virol 93:250–256. https://doi.org/10.1002/jmv.26232",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1111/1744-9987.13723",
"author": "RS Shemies",
"doi-asserted-by": "publisher",
"first-page": "15",
"journal-title": "Ther Apher Dial",
"key": "8515_CR20",
"unstructured": "Shemies RS, Nagy E, Younis D, Sheashaa H (2022) Renal replacement therapy for critically ill patients with COVID-19-associated acute kidney injury: a review of current knowledge. Ther Apher Dial 26:15–23. https://doi.org/10.1111/1744-9987.13723",
"volume": "26",
"year": "2022"
},
{
"DOI": "10.1016/j.ejphar.2020.173329",
"author": "ZMA El-Missiry",
"doi-asserted-by": "publisher",
"first-page": "173329",
"journal-title": "Eur J Pharmacol",
"key": "8515_CR21",
"unstructured": "El-Missiry ZMA, Othman AI (2020) Melatonin is a potential adjuvant to improve clinical outcomes in individuals with obesity and diabetes with coexistence of Covid-19. Eur J Pharmacol 882:173329. https://doi.org/10.1016/j.ejphar.2020.173329",
"volume": "882",
"year": "2020"
},
{
"DOI": "10.1038/nprot.2008.73",
"author": "TD Schmittgen",
"doi-asserted-by": "publisher",
"first-page": "1101",
"journal-title": "Nat Protoc",
"key": "8515_CR22",
"unstructured": "Schmittgen TD, Livak KJ (2008) Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc 3:1101–1108. https://doi.org/10.1038/nprot.2008.73",
"volume": "3",
"year": "2008"
},
{
"DOI": "10.1007/s00705-016-3187-y",
"author": "FC Camini",
"doi-asserted-by": "publisher",
"first-page": "907",
"journal-title": "Arch Virol",
"key": "8515_CR23",
"unstructured": "Camini FC, da Silva Caetano CC, Almeida LT, de Brito Magalhães CL (2017) Implications of oxidative stress on viral pathogenesis. Arch Virol 162:907–917. https://doi.org/10.1007/s00705-016-3187-y",
"volume": "162",
"year": "2017"
},
{
"DOI": "10.3390/antiox9090897",
"author": "HN de Las",
"doi-asserted-by": "publisher",
"journal-title": "Antioxidants (Basel)",
"key": "8515_CR24",
"unstructured": "de Las HN, Martín Giménez VM, Ferder L, Manucha W, Lahera V (2020) Implications of oxidative stress and potential role of mitochondrial dysfunction in COVID-19: therapeutic effects of vitamin D. Antioxidants (Basel). https://doi.org/10.3390/antiox9090897",
"year": "2020"
},
{
"DOI": "10.3389/fonc.2021.708263",
"author": "Z Zhu",
"doi-asserted-by": "publisher",
"first-page": "708263",
"journal-title": "Front Oncol",
"key": "8515_CR25",
"unstructured": "Zhu Z, Zheng Z, Liu J (2021) Comparison of COVID-19 and lung cancer via reactive oxygen species signaling. Front Oncol 11:708263. https://doi.org/10.3389/fonc.2021.708263",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.11604/pamj.2020.35.2.22877",
"author": "MP Ntyonga-Pono",
"doi-asserted-by": "publisher",
"first-page": "12",
"journal-title": "Pan Afr Med J",
"key": "8515_CR26",
"unstructured": "Ntyonga-Pono MP (2020) COVID-19 infection and oxidative stress: an under-explored approach for prevention and treatment? Pan Afr Med J 35:12. https://doi.org/10.11604/pamj.2020.35.2.22877",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1177/2050312121991246",
"author": "Y Muhammad",
"doi-asserted-by": "publisher",
"first-page": "205031212199124",
"journal-title": "Northwestern Nigeria SAGE Open Med",
"key": "8515_CR27",
"unstructured": "Muhammad Y, Kani YA, Iliya S, Muhammad JB, Binji A, El-Fulaty Ahmad A, Kabir MB, Umar Bindawa K, Ahmed A (2021) Deficiency of antioxidants and increased oxidative stress in COVID-19 patients: a cross-sectional comparative study in Jigawa. Northwestern Nigeria SAGE Open Med 9:2050312121991246. https://doi.org/10.1177/2050312121991246",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1126/science.abb2762",
"author": "R Yan",
"doi-asserted-by": "publisher",
"first-page": "1444",
"journal-title": "Science",
"key": "8515_CR28",
"unstructured": "Yan R, Zhang Y, Li Y, Xia L, Guo Y, Zhou Q (2020) Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science 367:1444–1448. https://doi.org/10.1126/science.abb2762",
"volume": "367",
"year": "2020"
},
{
"DOI": "10.1038/nm1267",
"author": "K Kuba",
"doi-asserted-by": "publisher",
"first-page": "875",
"journal-title": "Nat Med",
"key": "8515_CR29",
"unstructured": "Kuba K, Imai Y, Rao S, Gao H, Guo F, Guan B, Huan Y, Yang P, Zhang Y, Deng W, Bao L, Zhang B, Liu G, Wang Z, Chappell M, Liu Y, Zheng D, Leibbrandt A, Wada T, Slutsky AS, Liu D, Qin C, Jiang C, Penninger JM (2005) A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med 11:875–879. https://doi.org/10.1038/nm1267",
"volume": "11",
"year": "2005"
},
{
"DOI": "10.1016/j.biochi.2022.06.005",
"author": "V Mariappan",
"doi-asserted-by": "publisher",
"first-page": "139",
"journal-title": "Biochimie",
"key": "8515_CR30",
"unstructured": "Mariappan V, Ranganadin P, Shanmugam L, Rao SR, Balakrishna Pillai A (2022) Early shedding of membrane-bounded ACE2 could be an indicator for disease severity in SARS-CoV-2. Biochimie 201:139–147. https://doi.org/10.1016/j.biochi.2022.06.005",
"volume": "201",
"year": "2022"
},
{
"DOI": "10.1002/iub.2391",
"author": "V Mariappan",
"doi-asserted-by": "publisher",
"first-page": "2533",
"journal-title": "IUBMB Life",
"key": "8515_CR31",
"unstructured": "Mariappan V, S RR and Balakrishna Pillai A, (2020) Angiotensin-converting enzyme 2: a protective factor in regulating disease virulence of SARS-COV-2. IUBMB Life 72:2533–2545. https://doi.org/10.1002/iub.2391",
"volume": "72",
"year": "2020"
},
{
"DOI": "10.1093/ajh/hpaa169",
"author": "M Rieder",
"doi-asserted-by": "publisher",
"first-page": "278",
"journal-title": "Am J Hypertens",
"key": "8515_CR32",
"unstructured": "Rieder M, Wirth L, Pollmeier L, Jeserich M, Goller I, Baldus N, Schmid B, Busch HJ, Hofmann M, Kern W, Bode C, Duerschmied D, Lother A (2021) Serum ACE2, angiotensin II, and aldosterone levels are unchanged in patients with COVID-19. Am J Hypertens 34:278–281. https://doi.org/10.1093/ajh/hpaa169",
"volume": "34",
"year": "2021"
},
{
"DOI": "10.1136/postgradmedj-2020-137935",
"author": "X Zhang",
"doi-asserted-by": "publisher",
"first-page": "403",
"journal-title": "Postgrad Med J",
"key": "8515_CR33",
"unstructured": "Zhang X, Li S, Niu S (2020) ACE2 and COVID-19 and the resulting ARDS. Postgrad Med J 96:403–407. https://doi.org/10.1136/postgradmedj-2020-137935",
"volume": "96",
"year": "2020"
},
{
"DOI": "10.2174/1389450121666201020154033",
"author": "C Vieira",
"doi-asserted-by": "publisher",
"first-page": "254",
"journal-title": "Curr Drug Targets",
"key": "8515_CR34",
"unstructured": "Vieira C, Nery L, Martins L, Jabour L, Dias R, Simões ESAC (2021) Downregulation of membrane-bound angiotensin converting enzyme 2 (ACE2) receptor has a pivotal role in COVID-19 immunopathology. Curr Drug Targets 22:254–281. https://doi.org/10.2174/1389450121666201020154033",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1007/s11154-021-09663-z",
"author": "JR Cook",
"doi-asserted-by": "publisher",
"first-page": "151",
"journal-title": "Rev Endocr Metab Disord",
"key": "8515_CR35",
"unstructured": "Cook JR, Ausiello J (2022) Functional ACE2 deficiency leading to angiotensin imbalance in the pathophysiology of COVID-19. Rev Endocr Metab Disord 23:151–170. https://doi.org/10.1007/s11154-021-09663-z",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.3389/fmed.2020.00335",
"author": "P Pagliaro",
"doi-asserted-by": "publisher",
"first-page": "335",
"journal-title": "Front Med (Lausanne)",
"key": "8515_CR36",
"unstructured": "Pagliaro P, Penna C (2020) ACE/ACE2 ratio: a key also in 2019 coronavirus disease (Covid-19)? Front Med (Lausanne) 7:335. https://doi.org/10.3389/fmed.2020.00335",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.3389/fmed.2020.598870",
"author": "Z Liu",
"doi-asserted-by": "publisher",
"first-page": "598870",
"journal-title": "Front Med (Lausanne)",
"key": "8515_CR37",
"unstructured": "Liu Z, Li J, Long W, Zeng W, Gao R, Zeng G, Chen D, Wang S, Li Q, Hu D, Guo L, Li Z, Wu X (2020) Bilirubin levels as potential indicators of disease severity in coronavirus disease patients: a retrospective cohort study. Front Med (Lausanne) 7:598870. https://doi.org/10.3389/fmed.2020.598870",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1111/liv.14477",
"author": "P Paliogiannis",
"doi-asserted-by": "publisher",
"first-page": "1787",
"journal-title": "Liver Int",
"key": "8515_CR38",
"unstructured": "Paliogiannis P, Zinellu A (2020) Bilirubin levels in patients with mild and severe Covid-19: a pooled analysis. Liver Int 40:1787–1788. https://doi.org/10.1111/liv.14477",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.1016/j.jss.2016.05.020",
"author": "S Ozdinc",
"doi-asserted-by": "publisher",
"first-page": "445",
"journal-title": "J Surg Res",
"key": "8515_CR39",
"unstructured": "Ozdinc S, Oz G, Ozdemir C, Kilic I, Karakaya Z, Bal A, Koken T, Solak O (2016) Melatonin: is it an effective antioxidant for pulmonary contusion? J Surg Res 204:445–451. https://doi.org/10.1016/j.jss.2016.05.020",
"volume": "204",
"year": "2016"
},
{
"DOI": "10.1016/j.nmni.2021.100897",
"author": "B Karkhanei",
"doi-asserted-by": "publisher",
"first-page": "100897",
"journal-title": "New Microbes New Infect",
"key": "8515_CR40",
"unstructured": "Karkhanei B, Talebi Ghane E, Mehri F (2021) Evaluation of oxidative stress level: total antioxidant capacity, total oxidant status and glutathione activity in patients with COVID-19. New Microbes New Infect 42:100897. https://doi.org/10.1016/j.nmni.2021.100897",
"volume": "42",
"year": "2021"
},
{
"DOI": "10.1002/jmv.27500",
"author": "N Yaghoubi",
"doi-asserted-by": "publisher",
"first-page": "1558",
"journal-title": "J Med Virol",
"key": "8515_CR41",
"unstructured": "Yaghoubi N, Youssefi M, Jabbari Azad F, Farzad F, Yavari Z, Zahedi Avval F (2022) Total antioxidant capacity as a marker of severity of COVID-19 infection: possible prognostic and therapeutic clinical application. J Med Virol 94:1558–1565. https://doi.org/10.1002/jmv.27500",
"volume": "94",
"year": "2022"
},
{
"DOI": "10.1186/cc5008",
"author": "I Giovannini",
"doi-asserted-by": "publisher",
"first-page": "421",
"journal-title": "Crit Care",
"key": "8515_CR42",
"unstructured": "Giovannini I, Chiarla C, Giuliante F, Pallavicini F, Vellone M, Ardito F, Nuzzo G (2006) Serum uric acid, creatinine, and the assessment of antioxidant capacity in critical illness. Crit Care 10:421. https://doi.org/10.1186/cc5008",
"volume": "10",
"year": "2006"
},
{
"DOI": "10.1186/cc4826",
"author": "CC Chuang",
"doi-asserted-by": "publisher",
"first-page": "R36",
"journal-title": "Crit Care",
"key": "8515_CR43",
"unstructured": "Chuang CC, Shiesh SC, Chi CH, Tu YF, Hor LI, Shieh CC, Chen MF (2006) Serum total antioxidant capacity reflects severity of illness in patients with severe sepsis. Crit Care 10:R36. https://doi.org/10.1186/cc4826",
"volume": "10",
"year": "2006"
},
{
"DOI": "10.1016/j.jcrc.2014.09.012",
"author": "L Lorente",
"doi-asserted-by": "publisher",
"first-page": "217.e7",
"journal-title": "J Crit Care",
"key": "8515_CR44",
"unstructured": "Lorente L, Martín MM, Almeida T, Abreu-González P, Ferreres J, Solé-Violán J, Labarta L, Díaz C, Jiménez A (2015) Association between serum total antioxidant capacity and mortality in severe septic patients. J Crit Care 30:217.e7–12. https://doi.org/10.1016/j.jcrc.2014.09.012",
"volume": "30",
"year": "2015"
},
{
"DOI": "10.1155/2019/9213074",
"author": "A Korniluk",
"doi-asserted-by": "publisher",
"first-page": "9213074",
"journal-title": "Mediators Inflamm",
"key": "8515_CR45",
"unstructured": "Korniluk A, Koper-Lenkiewicz OM, Kamińska J, Kemona H, Dymicka-Piekarska V (2019) Mean platelet volume (MPV): new perspectives for an old marker in the course and prognosis of inflammatory conditions. Mediators Inflamm 2019:9213074. https://doi.org/10.1155/2019/9213074",
"volume": "2019",
"year": "2019"
},
{
"DOI": "10.1016/s0140-6736(00)02327-8",
"author": "JP Neoptolemos",
"doi-asserted-by": "publisher",
"first-page": "1955",
"journal-title": "Lancet",
"key": "8515_CR46",
"unstructured": "Neoptolemos JP, Kemppainen EA, Mayer JM, Fitzpatrick JM, Raraty MG, Slavin J, Beger HG, Hietaranta AJ, Puolakkainen PA (2000) Early prediction of severity in acute pancreatitis by urinary trypsinogen activation peptide: a multicentre study. Lancet 355:1955–1960. https://doi.org/10.1016/s0140-6736(00)02327-8",
"volume": "355",
"year": "2000"
},
{
"author": "L Kerekes",
"first-page": "1746",
"journal-title": "Hepatogastroenterology",
"key": "8515_CR47",
"unstructured": "Kerekes L, Arkossy P, Altorjay I, Huszka M, Kappelmayer J, Tóth P, Szentkereszty Z, Sápy P (2001) Evaluation of hemostatic changes and blood antioxidant capacity in acute and chronic pancreatitis. Hepatogastroenterology 48:1746–1749",
"volume": "48",
"year": "2001"
},
{
"DOI": "10.1055/s-0041-1727283",
"author": "G Lippi",
"doi-asserted-by": "publisher",
"first-page": "456",
"journal-title": "Semin Thromb Hemost",
"key": "8515_CR48",
"unstructured": "Lippi G, Henry BM, Favaloro EJ (2021) Mean platelet volume predicts severe COVID-19 illness. Semin Thromb Hemost 47:456–459. https://doi.org/10.1055/s-0041-1727283",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.1002/jcla.23607",
"author": "Q Zhong",
"doi-asserted-by": "publisher",
"first-page": "e23607",
"journal-title": "J Clin Lab Anal",
"key": "8515_CR49",
"unstructured": "Zhong Q, Peng J (2021) Mean platelet volume/platelet count ratio predicts severe pneumonia of COVID-19. J Clin Lab Anal 35:e23607. https://doi.org/10.1002/jcla.23607",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2022.102395",
"author": "A Zein",
"doi-asserted-by": "publisher",
"first-page": "102395",
"journal-title": "Diabetes Metab Syndr",
"key": "8515_CR50",
"unstructured": "Zein A, Raffaello WM (2022) Effect of colchicine on mortality in patients with COVID-19—a systematic review and meta-analysis. Diabetes Metab Syndr 16:102395. https://doi.org/10.1016/j.dsx.2022.102395",
"volume": "16",
"year": "2022"
},
{
"DOI": "10.1016/j.ejphar.2020.173329",
"author": "MA El-Missiry",
"doi-asserted-by": "publisher",
"first-page": "173329",
"journal-title": "Eur J Pharmacol",
"key": "8515_CR51",
"unstructured": "El-Missiry MA, El-Missiry ZMA, Othman AI (2020) Melatonin is a potential adjuvant to improve clinical outcomes in individuals with obesity and diabetes with coexistence of Covid-19. Eur J Pharmacol 882:173329. https://doi.org/10.1016/j.ejphar.2020.173329",
"volume": "882",
"year": "2020"
},
{
"DOI": "10.21037/jtd.2019.12.85",
"author": "RML Colunga Biancatelli",
"doi-asserted-by": "publisher",
"first-page": "S54",
"journal-title": "J Thorac Dis",
"key": "8515_CR52",
"unstructured": "Colunga Biancatelli RML, Berrill M, Mohammed YH, Marik PE (2020) Melatonin for the treatment of sepsis: the scientific rationale. J Thorac Dis 12:S54-s65. https://doi.org/10.21037/jtd.2019.12.85",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1111/j.1749-6632.1992.tb17085.x",
"author": "H Sies",
"doi-asserted-by": "publisher",
"first-page": "7",
"journal-title": "Ann N Y Acad Sci",
"key": "8515_CR53",
"unstructured": "Sies H, Stahl W, Sundquist AR (1992) Antioxidant functions of vitamins. Vitamins E and C, beta-carotene, and other carotenoids. Ann N Y Acad Sci 669:7–20. https://doi.org/10.1111/j.1749-6632.1992.tb17085.x",
"volume": "669",
"year": "1992"
},
{
"DOI": "10.1016/j.arcmed.2020.04.019",
"author": "L Delgado-Roche",
"doi-asserted-by": "publisher",
"first-page": "384",
"journal-title": "Arch Med Res",
"key": "8515_CR54",
"unstructured": "Delgado-Roche L, Mesta F (2020) Oxidative stress as key player in severe acute respiratory syndrome coronavirus (SARS-CoV) infection. Arch Med Res 51:384–387. https://doi.org/10.1016/j.arcmed.2020.04.019",
"volume": "51",
"year": "2020"
},
{
"DOI": "10.1139/y80-049",
"author": "SC Cunnane",
"doi-asserted-by": "publisher",
"first-page": "287",
"journal-title": "Can J Physiol Pharmacol",
"key": "8515_CR55",
"unstructured": "Cunnane SC, Manku MS, Oka M, Horrobin DF (1980) Enhanced vascular reactivity to various vasoconstrictor agents following pinealectomy in the rat: role of melatonin. Can J Physiol Pharmacol 58:287–293. https://doi.org/10.1139/y80-049",
"volume": "58",
"year": "1980"
},
{
"DOI": "10.1007/0-306-46814-X_32",
"author": "DN Krause",
"doi-asserted-by": "publisher",
"first-page": "299",
"journal-title": "Adv Exp Med Biol",
"key": "8515_CR56",
"unstructured": "Krause DN, Geary GG, Doolen S, Duckles SP (1999) Melatonin and cardiovascular function. Adv Exp Med Biol 460:299–310",
"volume": "460",
"year": "1999"
},
{
"DOI": "10.1016/j.micpath.2021.105057",
"author": "V Mariappan",
"doi-asserted-by": "publisher",
"first-page": "105057",
"journal-title": "Microb Pathog",
"key": "8515_CR57",
"unstructured": "Mariappan V, Manoharan PS, Shanmugam L, Rao SR, Pillai AB (2021) Potential biomarkers for the early prediction of SARS-COV-2 disease outcome. Microb Pathog 158:105057. https://doi.org/10.1016/j.micpath.2021.105057",
"volume": "158",
"year": "2021"
}
],
"reference-count": 57,
"references-count": 57,
"relation": {},
"resource": {
"primary": {
"URL": "https://link.springer.com/10.1007/s11033-023-08515-0"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Genetics",
"Molecular Biology",
"General Medicine"
],
"subtitle": [],
"title": "Angiotensin converting enzyme 2 gene expression and markers of oxidative stress are correlated with disease severity in patients with COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy"
}