Saying No to SARS-CoV-2: the potential of nitric oxide in the treatment of COVID-19 pneumonia
et al., Medical Gas Research, doi:10.4103/2045-9912.385414, Nov 2023
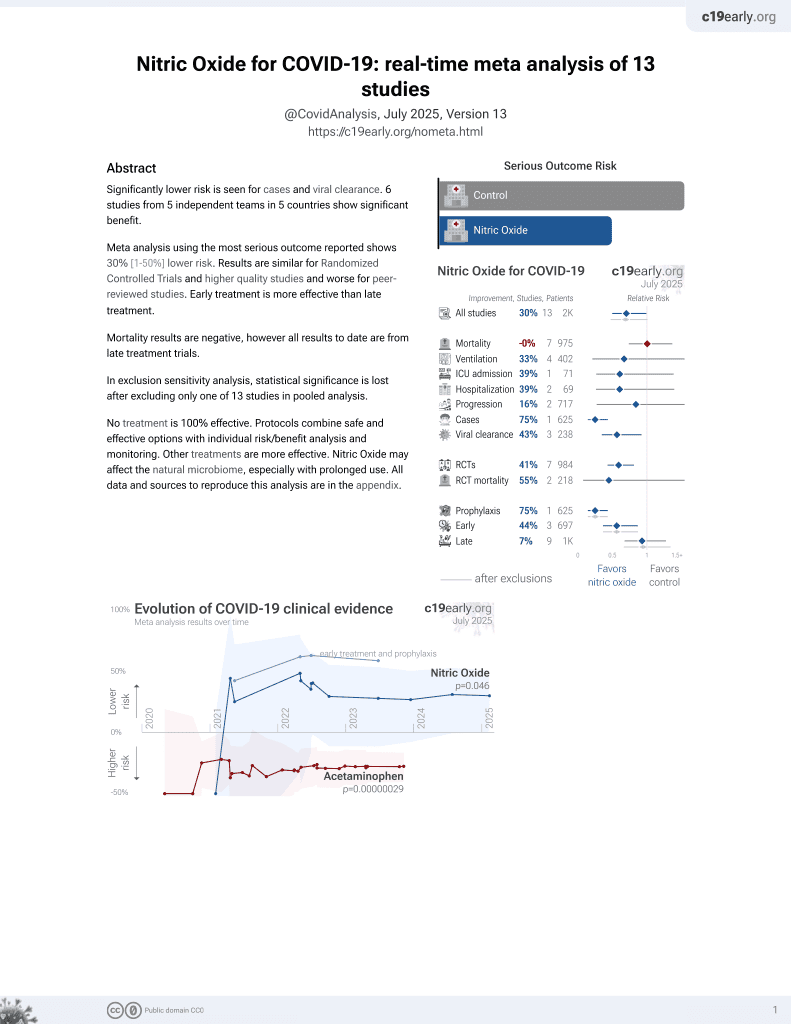
43rd treatment shown to reduce risk in
June 2022, now with p = 0.012 from 12 studies, recognized in 10 countries.
Lower risk for cases and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Review of nitric oxide (NO) in the treatment of COVID-19. Authors summarizes evidence from in vitro studies suggesting NO has direct antiviral effects against SARS-CoV-2 as well as immune modulating and pulmonary protective effects. Small preliminary clinical trials of inhaled NO have shown mixed results for improving oxygenation in COVID-19 pneumonia patients. Of note, NO nasal spray developed by SaNOtize has received regulatory approval in several countries based on evidence it can reduce viral load in mild COVID-19 infection. Authors note that more research is needed to increase the clinical evidence and determine optimal dosing, administration method, and safety.
1.
Wright et al., Nitric Oxide in the Treatment of COVID‐19: Nasal Sprays, Inhalants and Nanoparticles, Biochemistry Research International, doi:10.1155/bri/8846903.
2.
Zhang et al., Saying No to SARS-CoV-2: the potential of nitric oxide in the treatment of COVID-19 pneumonia, Medical Gas Research, doi:10.4103/2045-9912.385414.
3.
Zhao et al., Inhaled nitric oxide: can it serve as a savior for COVID-19 and related respiratory and cardiovascular diseases?, Frontiers in Microbiology, doi:10.3389/fmicb.2023.1277552.
4.
Yamasaki et al., Pleiotropic Functions of Nitric Oxide Produced by Ascorbate for the Prevention and Mitigation of COVID-19: A Revaluation of Pauling’s Vitamin C Therapy, Microorganisms, doi:10.3390/microorganisms11020397.
Zhang et al., 1 Nov 2023, peer-reviewed, 4 authors.
Contact: 1020071789@cpu.edu.cn.
Saying No to SARS-CoV-2: the potential of nitric oxide in the treatment of COVID-19 pneumonia
Medical Gas Research, doi:10.4103/2045-9912.385414
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been spreading around the world since 2019. Coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2 was declared as a pandemic by the World Health Organization in March 2020. As of September 2022, it has infected more than 607 million people worldwide and claimed the lives of more than 6.5 million people. The pandemic shows no signs of slowing down and the recent emergence of more transmissible variants (Delta and Omicron) fuels a surge of infections around the world, posing a significant threat to public health as well as a tremendous social and economic burden worldwide. SARS-CoV-2 is an RNA virus closely related to SARS-CoV with 79% genetic similarity, 1 belonging to the beta-coronavirus genus. The possible modes of transmission for SARS-CoV-2 include contact, respiratory droplets, fomite, faecal-oral, mother-to-child, and animal-to-human transmission. The virus invades cells through the binding between the S protein on its surface and the host-cell receptor angiotensin-converting enzyme 2 (ACE2), which is widely distributed in various tissues and immune cells in human bodies. 2 The clinical manifestations of SARS-CoV-2 infection include fever, cough, fatigue, pneumonia, local inflammation, severe or critical disseminated intravascular coagulation, acute respiratory distress syndrome (ARDS), hypotension and multiple organ failures, some of which may eventually lead to death. 3 Nitric oxide (NO) is a signaling molecule produced from L-arginine catalyzed by NO synthase in mammalian cells. It was first discovered as an endothelium-derived relaxing factor that can activate guanylate cyclase to produce the second messenger cyclic guanosine monophosphate, finally leading to vasodilation. [4] [5] [6] The biological role of NO also involves S-nitrosation of proteins whereby NO or its derivative interacts with the thiol group of cysteine residue to form S-nitrosothiol. This post-translational modification affects countless cellular processes in physiology and pathophysiology, including the regulation of virus replication. 7, 8 Moreover, NO can cause nitration of proteins, lipids, and DNA through peroxynitrite, which is generated by the reaction of NO with superoxide anion radical, affecting various cellular processes. 9 Many studies have reported that NO plays a direct or indirect role in fighting against harmful viruses, including respiratory viruses, such as SARS-CoV-2, 10 severe acute respiratory syndrome coronavirus, 11 and influenza virus, 12 as well as non-respiratory viruses such as human papillomavirus, 13 herpes simplex virus-1 14 and porcine circovirus type 2. 15 The potential role of NO in the treatment of SARS-CoV-2 has been revealed by increasing basic and clinical studies. What's even more encouraging is the urgent approval of NO nasal spray (NONS) for the treatment of COVID-19 pneumonia in Israel, Bahrain, Thailand and Indonesia. NONS is administered
Author contributions JC designed the manuscript. HZ, CZ and WH collected literature and wrote the manuscript. JC polished the language for the manuscript. All authors read and approved the final manuscript.
Conflicts of interest The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Data availability statement No additional data are available.
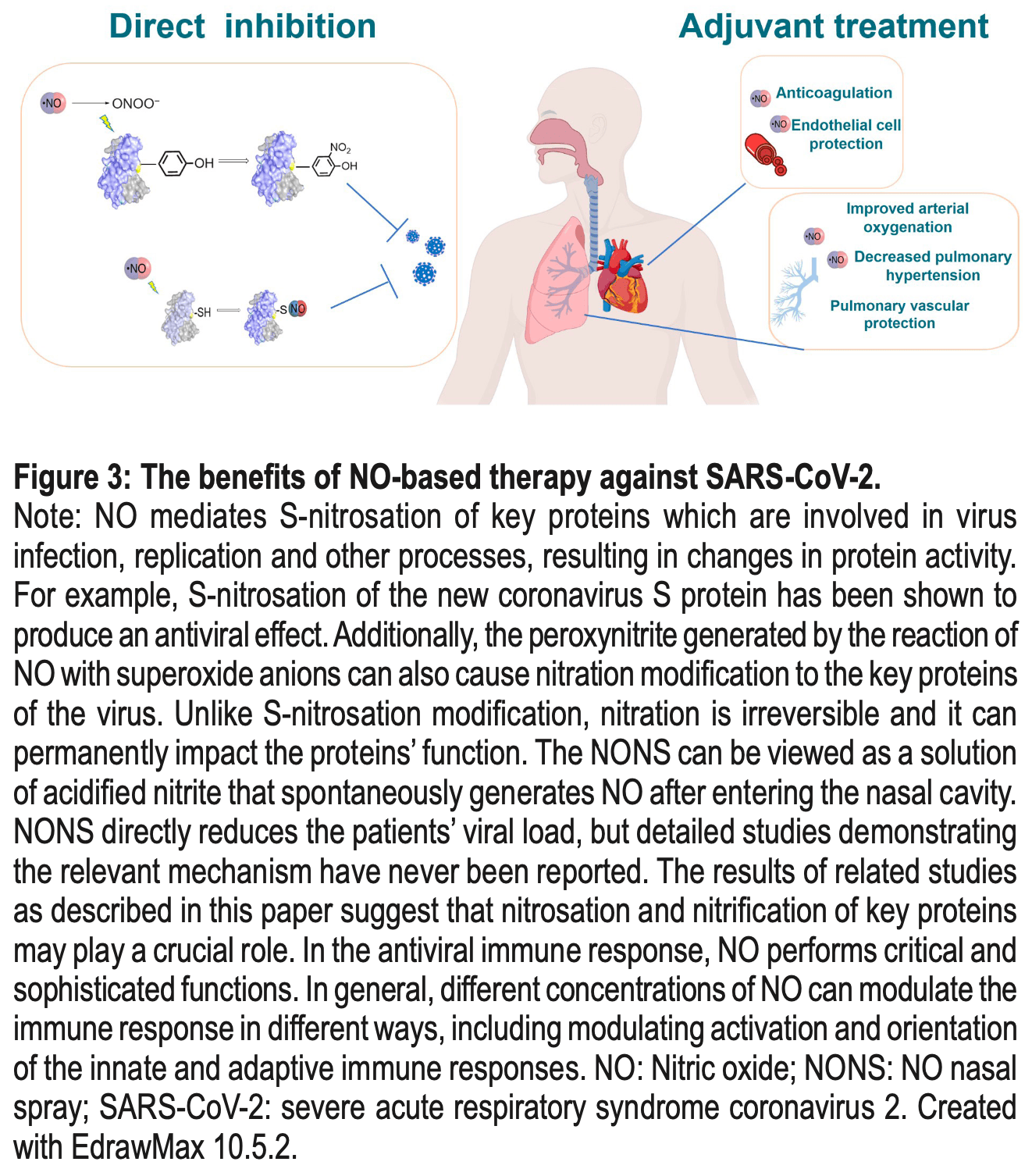
Open access statement This is an open access journal, and articles are distributed under the terms of the Creative Commons AttributionNonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms. Note: NO mediates S-nitrosation of key proteins which are involved in virus infection, replication and other processes, resulting in changes in protein activity. For example, S-nitrosation of the new coronavirus S protein has been shown to produce an antiviral effect. Additionally, the peroxynitrite generated by the reaction of NO with superoxide anions can also cause nitration modification to the key proteins of the virus. Unlike S-nitrosation modification, nitration is irreversible and it can permanently impact the proteins' function. The NONS can be viewed as a solution of acidified nitrite that spontaneously generates NO after entering the nasal cavity. NONS directly..
References
Ackermann, Verleden, Kuehnel, Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19, N Engl J Med
Akaberi, Krambrich, Ling, Mitigation of the replication of SARS-CoV-2 by nitric oxide in vitro, Redox Biol
Akaike, Maeda, Nitric oxide and virus infection, Immunology
Akaike, Noguchi, Ijiri, Pathogenesis of influenza virusinduced pneumonia: involvement of both nitric oxide and oxygen radicals, Proc Natl Acad Sci U S A
Akerström, Gunalan, Keng, Tan, Mirazimi, Dual effect of nitric oxide on SARS-CoV replication: viral RNA production and palmitoylation of the S protein are affected, Virology
Akerström, Mousavi-Jazi, Klingström, Leijon, Lundkvist et al., Nitric oxide inhibits the replication cycle of severe acute respiratory syndrome coronavirus, J Virol
Akuta, Zaki, Yoshitake, Okamoto, Akaike, Nitrative stress through formation of 8-nitroguanosine: insights into microbial pathogenesis, Nitric Oxide
Andersen, Rambaut, Lipkin, Holmes, Garry, The proximal origin of SARS-CoV-2, Nat Med
Ashour, Elsayed, Elmorsy, Harb, Hypothesis: the potential therapeutic role of nicorandil in COVID-19, Clin Exp Pharmacol Physiol
Bi, Reiss, Inhibition of vesicular stomatitis virus infection by nitric oxide, J Virol
Chen, Guo, Wang, Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records, Lancet
Chen, Liu, Gao, Inhalation of nitric oxide in the treatment of severe acute respiratory syndrome: a rescue trial in Beijing, Clin Infect Dis
Chen, Wu, Chen, Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study, BMJ
Colasanti, Persichini, Venturini, Ascenzi, S-nitrosylation of viral proteins: molecular bases for antiviral effect of nitric oxide, IUBMB Life
Croen, Evidence for antiviral effect of nitric oxide. Inhibition of herpes simplex virus type 1 replication, J Clin Invest
Cymerys, Kowalczyk, Mikołajewicz, Słońska, Krzyżowska, Nitric oxide influences HSV-1-induced neuroinflammation, Oxid Med Cell Longev
De Souza, Silva, De, Rocha, Nitric oxide synthase expression correlates with death in an experimental mouse model of dengue with CNS involvement, Virol J
Fakhr, Fenza, Gianni, Inhaled high dose nitric oxide is a safe and effective respiratory treatment in spontaneous breathing hospitalized patients with COVID-19 pneumonia, Nitric Oxide
Fakhr, Wiegand, Pinciroli, High concentrations of nitric oxide inhalation therapy in pregnant patients with severe coronavirus disease 2019 (COVID-19), Obstet Gynecol
Ferrari, Santini, Protti, Inhaled nitric oxide in mechanically ventilated patients with COVID-19, J Crit Care
Goldstein, Lue, Padma-Nathan, Rosen, Steers et al., Oral sildenafil in the treatment of erectile dysfunction. Sildenafil Study Group, N Engl J Med
Goshi, Zhou, He, Nitric oxide detection methods in vitro and in vivo, Med Gas Res
Guan, Seet, Kennedy, Does eNOS derived nitric oxide protect the young from severe COVID-19 complications?, Ageing Res Rev
Harris, Buller, Karupiah, Gamma interferon-induced, nitric oxide-mediated inhibition of vaccinia virus replication, J Virol
Hess, Patterson, Smith, Skene, Neuronal growth cone collapse and inhibition of protein fatty acylation by nitric oxide, Nature
Heuts, Ubben, Banks-Gonzales, Nitric oxide ventilation improves recirculation and right ventricular function during veno-venous extracorporeal membrane oxygenation in a COV-ID-19 patient, J Cardiothorac Vasc Anesth
Hoffmann, Kleine-Weber, Schroeder, SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor, Cell
Huang, Fu, Zhang, Nitric oxide donor-based cancer therapy: advances and prospects, J Med Chem
Huang, Li, Brighton, Carson, Becker et al., 3-nitrotyrosine attenuates respiratory syncytial virus infection in human bronchial epithelial cell line, Am J Physiol Lung Cell Mol Physiol
Iba, Connors, Levy, The coagulopathy, endotheliopathy, and vasculitis of COVID-19, Inflamm Res
Ignarro, Buga, Wood, Byrns, Chaudhuri, Endothelium-derived relaxing factor produced and released from artery and vein is nitric oxide, Proc Natl Acad Sci U S A
Ischiropoulos, Biological tyrosine nitration: a pathophysiological function of nitric oxide and reactive oxygen species, Arch Biochem Biophys
Isidori, Giannetta, Pofi, Targeting the NO-cGMP-PDE5 pathway in COVID-19 infection. The DEDALO project, Andrology
Karupiah, Chen, Mahalingam, Nathan, Macmicking, Rapid interferon gamma-dependent clearance of influenza A virus and protection from consolidating pneumonitis in nitric oxide synthase 2-deficient mice, J Exp Med
Karupiah, Xie, Buller, Nathan, Duarte et al., Inhibition of viral replication by interferon-gamma-induced nitric oxide synthase, Science
Klingström, Akerström, Hardestam, Nitric oxide and peroxynitrite have different antiviral effects against hantavirus replication and free mature virions, Eur J Immunol
Lam, Van Heerden, Blott, Roberts, Ilett, The selective pulmonary vasodilatory effect of inhaled DETA/NO, a novel nitric oxide donor, in ARDS-a pilot human trial, J Crit Care
Lei, Su, Dong, Protocol of a randomized controlled trial testing inhaled nitric oxide in mechanically ventilated patients with severe acute respiratory syndrome in COVID-19, medRxiv, doi:10.1101/2020.03.09.20033530
Li, Wang, Xu, Synthesis and biological evaluation of nitric oxide-releasing hybrids from gemcitabine and phenylsulfonyl furoxans as anti-tumor agents, Med Chem Commun
Libby, Lüscher, COVID-19 is, in the end, an endothelial disease, Eur Heart J
Lisi, Zelikin, Chandrawati, Nitric oxide to fight viral infections, Adv Sci (Weinh)
Liu, Wen, Xiao, He, Nitric oxide-generating compound GSNO suppresses porcine circovirus type 2 infection in vitro and in vivo, BMC Vet Res
Longobardo, Montanari, Shulman, Benhalim, Singer et al., Inhaled nitric oxide minimally improves oxygenation in COVID-19 related acute respiratory distress syndrome, Br J Anaesth
Lotz, Muellenbach, Meybohm, Effects of inhaled nitric oxide in COVID-19-induced ARDS -Is it worthwhile?, Acta Anaesthesiol Scand
Maclean, Wei, Huang, Ua, Chan et al., Mice lacking inducible nitric-oxide synthase are more susceptible to herpes simplex virus infection despite enhanced Th1 cell responses, J Gen Virol
Meier, Stapleton, Hofferber, Haworth, Kachman et al., Quantification of nitric oxide concentration using single-walled carbon nanotube sensors, Nanomaterials
Milara, Escrivá, Ortiz, Vascular effects of sildenafil in patients with pulmonary fibrosis and pulmonary hypertension: an ex vivo/in vitro study, Eur Respir J
Miller, Miller, Mcmullin, A phase I clinical study of inhaled nitric oxide in healthy adults, J Cyst Fibros
Miyazawa, Immunopathogenesis of SARS-CoV-2-induced pneumonia: lessons from influenza virus infection, Inflamm Regen
Mostafa, Could oral phosphodiesterase 5 inhibitors have a potential adjuvant role in combating COVID-19 infection?, Sex Med Rev
Murad, Cyclic guanosine monophosphate as a mediator of vasodilation, J Clin Invest
Niedbala, Wei, Campbell, Thomson, Komai-Koma et al., Nitric oxide preferentially induces type 1 T cell differentiation by selectively up-regulating IL-12 receptor beta 2 expression via cGMP, Proc Natl Acad Sci U S A
Nishimura, Hess, Kacmarek, Ritz, Hurford, Nitrogen dioxide production during mechanical ventilation with nitric oxide in adults. Effects of ventilator internal volume, air versus nitrogen dilution, minute ventilation, and inspired oxygen fraction, Anesthesiology
Noureddine, Altara, Fan, Yabluchanskiy, Booz et al., Impact of the renin-angiotensin system on the endothelium in vascular dementia: unresolved issues and future perspectives, Int J Mol Sci
Novella, Dantas, Segarra, Medina, Hermenegildo, Vascular aging in women: is estrogen the fountain of youth?, Front Physiol
Oh, Nakamura, Beutler, Targeted protein S-nitrosylation of ACE2 inhibits SARS-CoV-2 infection, Nat Chem Biol
Palmer, Ferrige, Moncada, Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor, Nature
Perrone, Belser, Wadford, Katz, Tumpey, Inducible nitric oxide contributes to viral pathogenesis following highly pathogenic influenza virus infection in mice, J Infect Dis
Persichini, Colasanti, Fraziano, Nitric oxide inhibits the HIV-1 reverse transcriptase activity, Biochem Biophys Res Commun
Ray, R-107 shows promise in early study for pah linked to CO-VID-19
Regev-Shoshani, Vimalanathan, Mcmullin, Road, Av-Gay et al., Gaseous nitric oxide reduces influenza infectivity in vitro, Nitric Oxide
Reichenbach, Momi, Gresele, Nitric oxide and its antithrombotic action in the cardiovascular system, Curr Drug Targets Cardiovasc Haematol Disord
Rimmelzwaan, Baars, De Lijster, Fouchier, Osterhaus, Inhibition of influenza virus replication by nitric oxide, J Virol
Rogosnitzky, Okediji, Koman, Cepharanthine: a review of the antiviral potential of a Japanese-approved alopecia drug in CO-VID-19, Pharmacol Rep
Rossaint, Falke, López, Slama, Pison et al., Inhaled nitric oxide for the adult respiratory distress syndrome, N Engl J Med
Sanders, Siekierski, Porter, Richards, Proud, Nitric oxide inhibits rhinovirus-induced cytokine production and viral replication in a human respiratory epithelial cell line, J Virol
Saura, Zaragoza, Mcmillan, An antiviral mechanism of nitric oxide: inhibition of a viral protease, Immunity
Shang, Ye, Shi, Structural basis of receptor recognition by SARS-CoV-2, Nature
Siddiqi, Libby, Ridker, COVID-19 -A vascular disease, Trends Cardiovasc Med
South, Diz, Chappell, COVID-19, ACE2, and the cardiovascular consequences, Am J Physiol Heart Circ Physiol
Stefano, Esch, Kream, Potential immunoregulatory and antiviral/SARS-CoV-2 activities of nitric oxide, Med Sci Monit
Stomberski, Hess, Stamler, Protein S-nitrosylation: determinants of specificity and enzymatic regulation of S-nitrosothiol-based signaling, Antioxid Redox Signal
Tavazzi, Pozzi, Mongodi, Dammassa, Romito et al., Inhaled nitric oxide in patients admitted to intensive care unit with COVID-19 pneumonia, Crit Care
Teuwen, Geldhof, Pasut, Carmeliet, COVID-19: the vasculature unleashed, Nat Rev Immunol
Torre, Pugliese, Speranza, Role of nitric oxide in HIV-1 infection: friend or foe?, Lancet Infect Dis
Uehara, Bde, Brito, Role of nitric oxide in immune responses against viruses: beyond microbicidal activity, Inflamm Res
Wan, Shang, Graham, Baric, Li, Receptor recognition by the novel coronavirus from wuhan: an analysis based on decade-long structural studies of SARS coronavirus, J Virol
Winchester, John, Jabbar, John, Clinical efficacy of nitric oxide nasal spray (NONS) for the treatment of mild COVID-19 infection, J Infect
Wu, Tackle the free radicals damage in COVID-19, Nitric Oxide
Yang, Xie, Tu, Fu, Xu et al., The signal pathways and treatment of cytokine storm in COVID-19, Signal Transduct Target Ther
Yang, Yu, Xu, Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study, Lancet Respir Med
Yao, Wang, Yao, Yao, Abnormal expressions of inflammatory-related mediators and inhibition of fat metabolism in mice infected with influenza a virus, Pak J Pharm Sci
Yu, Sun, Liu, Nitric oxide inhibits the transcription of E6 gene of human papillomavirus, Acta Virol
Zisman, Schwarz, A controlled trial of sildenafil in advanced idiopathic pulmonary fibrosis, N Engl J Med
DOI record:
{
"DOI": "10.4103/2045-9912.385414",
"ISSN": [
"2045-9912"
],
"URL": "http://dx.doi.org/10.4103/2045-9912.385414",
"alternative-id": [
"385414"
],
"author": [
{
"affiliation": [],
"family": "Zhang",
"given": "Honghua",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Chen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hua",
"given": "Wenyan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Jing",
"sequence": "additional"
}
],
"container-title": "Medical Gas Research",
"container-title-short": "Med Gas Res",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
9,
8
]
],
"date-time": "2023-09-08T05:36:16Z",
"timestamp": 1694151376000
},
"deposited": {
"date-parts": [
[
2023,
9,
18
]
],
"date-time": "2023-09-18T07:12:45Z",
"timestamp": 1695021165000
},
"indexed": {
"date-parts": [
[
2023,
9,
19
]
],
"date-time": "2023-09-19T14:31:11Z",
"timestamp": 1695133871743
},
"is-referenced-by-count": 0,
"issue": "2",
"issued": {
"date-parts": [
[
2024
]
]
},
"journal-issue": {
"issue": "2",
"published-print": {
"date-parts": [
[
2024
]
]
}
},
"language": "en",
"member": "2581",
"original-title": [],
"page": "0",
"prefix": "10.4103",
"published": {
"date-parts": [
[
2024
]
]
},
"published-print": {
"date-parts": [
[
2024
]
]
},
"publisher": "Medknow",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://journals.lww.com/10.4103/2045-9912.385414"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Anesthesiology and Pain Medicine",
"Neuroscience (miscellaneous)"
],
"subtitle": [],
"title": "Saying No to SARS-CoV-2: the potential of nitric oxide in the treatment of COVID-19 pneumonia",
"type": "journal-article",
"volume": "14"
}