Survival analysis based on body mass index in patients with COVID-19 admitted to the intensive care unit of Amir Al-Momenin Hospital in Arak – 2021
et al., Obesity Medicine, doi:10.1016/j.obmed.2022.100420, May 2022
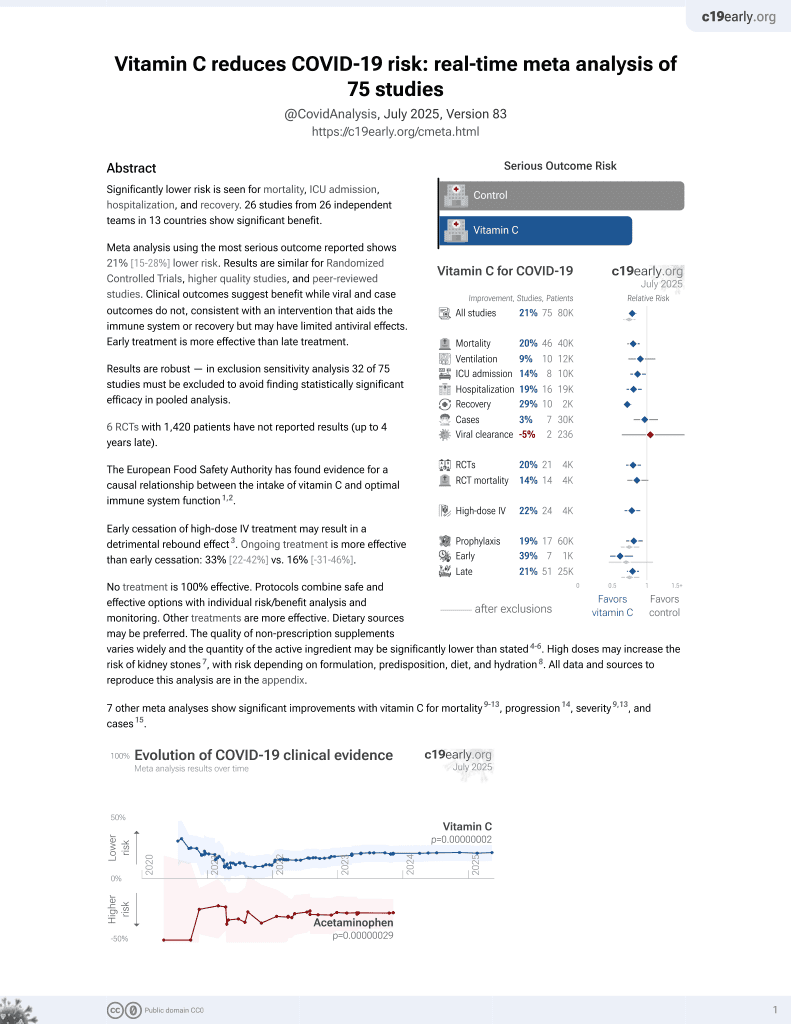
Vitamin C for COVID-19
6th treatment shown to reduce risk in
September 2020, now with p = 0.000000068 from 74 studies, recognized in 22 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 193 ICU patients in Iran, showing no significant difference with vitamin C treatment.
This is the 47th of 74 COVID-19 controlled studies for vitamin C, which collectively show efficacy with p=0.000000068.
21 studies are RCTs, which show efficacy with p=0.0012.
This study is excluded in the after exclusion results of meta-analysis:
very late stage, ICU patients.
|
risk of death, 4.0% lower, HR 0.96, p = 0.86, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Zangeneh et al., 13 May 2022, retrospective, Iran, peer-reviewed, 3 authors, dosage not specified.
Contact: mor.zangene62@gmail.com, touraj1416@gmail.com, a.sharifi1983@gmail.com, a_sharifi@goums.ac.ir.
Survival analysis based on body mass index in patients with Covid-19 admitted to the intensive care unit of Amir Al-Momenin Hospital in Arak – 2021
Obesity Medicine, doi:10.1016/j.obmed.2022.100420
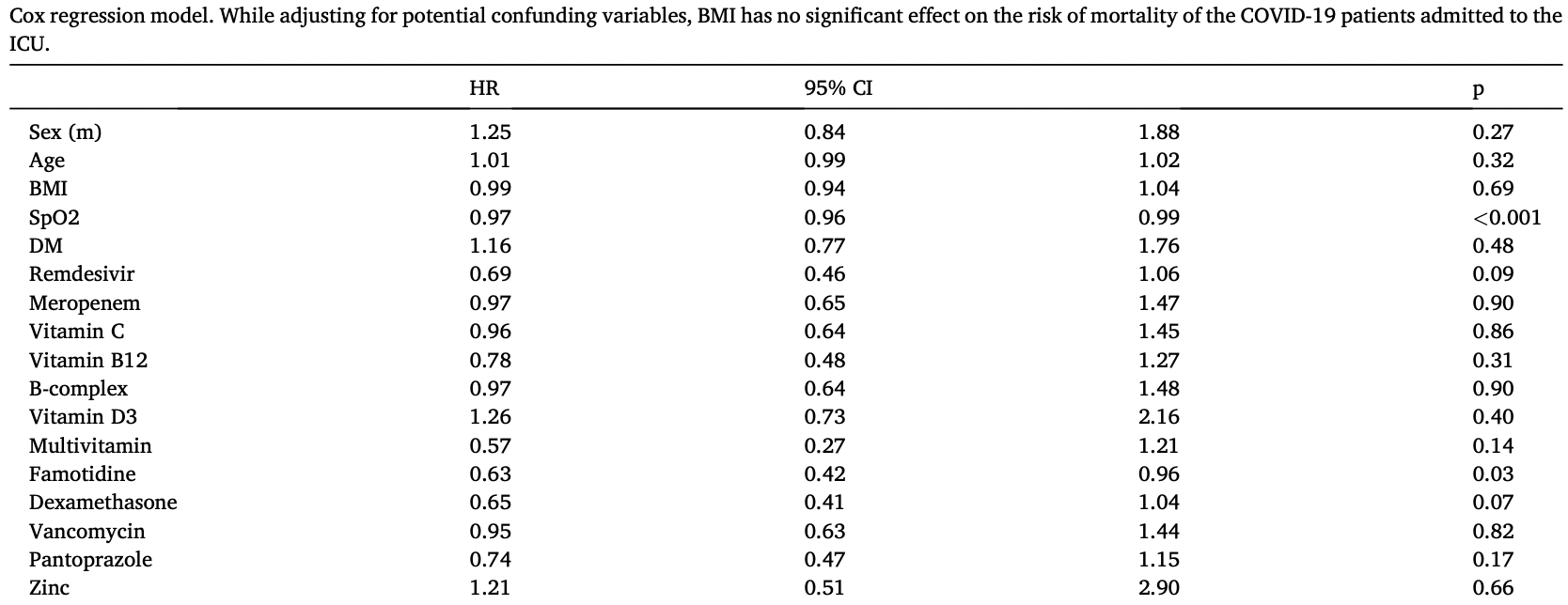
Introduction: The potential risk of obesity on the severity of COVID-19 has been proposed. The main purpose of this study was to investigate the effect of BMI on the survival rate of COVID-19 patients admitted to the ICU. Methods & materials: Patients with COVID-19 admitted to ICU were included. Gender, height, weight, BMI, age, underlying disease status, prescribed drugs and nutritional supplements, and clinical and laboratory parameters at the beginning of admission were recorded. Death or discharge from the ICU and the days elapsed to these events were also reviewed and recorded. Data analysis was performed using the Cox regression model. Results: assessing 193 patients showed that BMI was not related to the survival rate even after adjusting for other potential confounding variables. It was shown that arterial oxygen saturation and taking Famotidine were the significant factors determining the time to event in these patients.
Conclusion: The BMI at the time of ICU admission has no effect on survival rate and time to event in COVID-19 infected patients admitted to ICU.
Declaration of competing interest None.
References
Abbas, Fathy, Fawzy, Salem, Shawky et al., Obesity and susceptibility to severe outcomes following respiratory viral infection, Obes. Med
Andersen, Murphy, Fernandez, Impact of obesity and metabolic syndrome on immunity, Adv. Nutr
Brennan, Nadella, Zhao, Dima, Jordan-Martin et al., Oral famotidine versus placebo in non-hospitalised patients with COVID-19: a randomised, double-blind, data-intense, phase 2 clinical trial, Gut
Cheng, Can early and high intravenous dose of vitamin C prevent and treat coronavirus disease 2019 (COVID-19)?, Med. Drug Discov
Chiu, Shen, Lo, Chiu, Chen et al., Effect of famotidine on hospitalized patients with COVID-19: a systematic review and metaanalysis, PLoS One
Chowdhury, Alam, Rabbi, Rahman, Reza, Does higher body mass index increase COVID-19 severity? A systematic review and metaanalysis, Obes. Med
De Almeida Brasiel, The key role of zinc in elderly immunity: a possible approach in the COVID-19 crisis, Clin. Nutr. ESPEN
De Siqueira, Almeida, Zica, Brum, Barcelo et al., Impact of obesity on hospitalizations and mortality, due to COVID-19: a systematic review, Obes. Res. Clin. Pract
Emami, Akbari, Basirat, Zare, Javanmardi et al., The role of comorbidities on mortality of COVID-19 in patients with diabetes, Obes. Med
Fresán, Guevara, Elía, Albéniz, Burgui et al., Independent role of severe obesity as a risk factor for COVID-19 hospitalization: a Spanish population-based cohort study, Obesity
Giacomelli, Ridolfo, Milazzo, Oreni, Bernacchia et al., 30-day mortality in patients hospitalized with COVID-19 during the first wave of the Italian epidemic: a prospective cohort study, Pharmacol. Res
Grasselli, Zangrillo, Zanella, Antonelli, Cabrini et al., Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy, JAMA
Houdek, Griffin, Ferguson, Wunder, Morbid obesity increases the risk of postoperative wound complications, infection, and repeat surgical procedures following upper extremity limb salvage surgery for soft tissue sarcoma, Hand (N Y)
Huang, Lu, Huang, Wang, Ling et al., Obesity in patients with COVID-19: a systematic review and meta-analysis, Obes. Res. Clin. Pract
Huang, Wang, Zheng, Liu, Chen et al., Letter to the Editor: obesity hypoventilation syndrome and severe COVID-19, Metabolism
Kang, Mortality rate of infection with COVID-19 in Korea from the perspective of underlying disease, Disaster Med. Public Health Prep
Li, Li, Zhang, Wang, Lighter et al., Obesity in patients younger than 60 Years is a risk factor for COVID-19 hospital admission, Infect. Dis. Poverty
Loffredo, Lucero, Chen, O'connell, Bergqvist et al., The in-vitro effect of famotidine on sars-cov-2 proteases and virus replication, Sci. Rep
Louie, Acosta, Samuel, Schechter, Vugia et al., A novel risk factor for a novel virus: obesity and 2009 pandemic influenza A (H1N1), Clin. Infect. Dis
Mizumoto, Kagaya, Zarebski, Chowell, Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Euro Surveill
Muscogiuri, Pugliese, Barrea, Savastano, Colao, Changes in human dendritic cell number and function in severe obesity may contribute to increased susceptibility to viral infection, Metabol. Clin
Palaiodimos, Kokkinidis, Li, Karamanis, Ognibene et al., Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, Metabolism
Pranata, Lim, Yonas, Vania, Lukito et al., Body mass index and outcome in patients with COVID-19: a dose-response metaanalysis, Diabetes Metab
Rojas-Osornio, Cruz-Hernandez, Drago-Serrano, Campos-Rodriguez, Immunity to influenza: impact of obesity, Obes. Res. Clin. Pract
Ruan, Yang, Wang, Jiang, Song, Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China, Intensive Care Med
Rychter, Zawada, Ratajczak, Dobrowolska, Krela-Kazmierczak, Should patients with obesity be more afraid of COVID-19?, Obes. Rev
Sartaj Sohrab, Atkinson, Alawi, Azhar, Viral infection and obesity: current status and future prospective, Curr. Drug Metabol
Sattar, Mcinnes, Mcmurray, Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanisms, Circulation
Shrestha, Charkviani, Musurakis, Kansakar, Devkota et al., Type 2 diabetes is associated with increased risk of critical respiratory illness in patients COVID-19 in a community hospital, Obes. Med
Skalny, Rink, Ajsuvakova, Aschner, Gritsenko et al., Zinc and respiratory tract infections: perspectives for COVID-19, Int. J. Mol. Med
Sureshchandra, Marshall, Messaoudi, Impact of pregravid obesity on maternal and fetal immunity: fertile grounds for reprogramming, J. Leukoc. Biol
Wu, Mcgoogan, Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention, JAMA
Yates, Razieh, Zaccardi, Davies, Khunti, Obesity and risk of COVID-19: analysis of UK biobank, Prim. Care Diabetes
DOI record:
{
"DOI": "10.1016/j.obmed.2022.100420",
"ISSN": [
"2451-8476"
],
"URL": "http://dx.doi.org/10.1016/j.obmed.2022.100420",
"alternative-id": [
"S245184762200032X"
],
"article-number": "100420",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Survival analysis based on body mass index in patients with Covid-19 admitted to the intensive care unit of Amir Al-Momenin Hospital in Arak – 2021"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Obesity Medicine"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.obmed.2022.100420"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2022 Elsevier Ltd. All rights reserved."
}
],
"author": [
{
"affiliation": [],
"family": "Zangeneh",
"given": "Morteza",
"sequence": "first"
},
{
"affiliation": [],
"family": "Valeh",
"given": "Touraj",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sharifi",
"given": "Amrollah",
"sequence": "additional"
}
],
"container-title": "Obesity Medicine",
"container-title-short": "Obesity Medicine",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.com.au",
"clinicalkey.es",
"clinicalkey.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2022,
5,
11
]
],
"date-time": "2022-05-11T07:56:22Z",
"timestamp": 1652255782000
},
"deposited": {
"date-parts": [
[
2022,
5,
17
]
],
"date-time": "2022-05-17T17:58:34Z",
"timestamp": 1652810314000
},
"funder": [
{
"DOI": "10.13039/501100007113",
"award": [
"3837"
],
"doi-asserted-by": "publisher",
"name": "Arak University of Medical Sciences"
}
],
"indexed": {
"date-parts": [
[
2022,
5,
17
]
],
"date-time": "2022-05-17T18:41:41Z",
"timestamp": 1652812901804
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
6
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
6,
1
]
],
"date-time": "2022-06-01T00:00:00Z",
"timestamp": 1654041600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S245184762200032X?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S245184762200032X?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "100420",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2022,
6
]
]
},
"published-print": {
"date-parts": [
[
2022,
6
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/j.obmed.2020.100250",
"article-title": "The mutual effects of COVID-19 and obesity",
"author": "Abbas",
"doi-asserted-by": "crossref",
"first-page": "100250",
"journal-title": "Obes. Med.",
"key": "10.1016/j.obmed.2022.100420_bib1",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1136/thoraxjnl-2012-203009",
"article-title": "Obesity and susceptibility to severe outcomes following respiratory viral infection",
"author": "Almond",
"doi-asserted-by": "crossref",
"first-page": "684",
"issue": "7",
"journal-title": "Thorax",
"key": "10.1016/j.obmed.2022.100420_bib2",
"volume": "68",
"year": "2013"
},
{
"DOI": "10.3945/an.115.010207",
"article-title": "Impact of obesity and metabolic syndrome on immunity",
"author": "Andersen",
"doi-asserted-by": "crossref",
"first-page": "66",
"issue": "1",
"journal-title": "Adv. Nutr.",
"key": "10.1016/j.obmed.2022.100420_bib3",
"volume": "7",
"year": "2016"
},
{
"DOI": "10.1136/gutjnl-2022-326952",
"article-title": "Oral famotidine versus placebo in non-hospitalised patients with COVID-19: a randomised, double-blind, data-intense, phase 2 clinical trial",
"author": "Brennan",
"doi-asserted-by": "crossref",
"first-page": "879",
"issue": "5",
"journal-title": "Gut",
"key": "10.1016/j.obmed.2022.100420_bib4",
"volume": "71",
"year": "2022"
},
{
"DOI": "10.1016/j.medidd.2020.100028",
"article-title": "Can early and high intravenous dose of vitamin C prevent and treat coronavirus disease 2019 (COVID-19)?",
"author": "Cheng",
"doi-asserted-by": "crossref",
"first-page": "100028",
"journal-title": "Med. Drug Discov.",
"key": "10.1016/j.obmed.2022.100420_bib5",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0259514",
"article-title": "Effect of famotidine on hospitalized patients with COVID-19: a systematic review and meta-analysis",
"author": "Chiu",
"doi-asserted-by": "crossref",
"issue": "11",
"journal-title": "PLoS One",
"key": "10.1016/j.obmed.2022.100420_bib6",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1016/j.obmed.2021.100340",
"article-title": "Does higher body mass index increase COVID-19 severity? A systematic review and meta-analysis",
"author": "Chowdhury",
"doi-asserted-by": "crossref",
"first-page": "100340",
"journal-title": "Obes. Med.",
"key": "10.1016/j.obmed.2022.100420_bib7",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.1016/j.clnesp.2020.06.003",
"article-title": "The key role of zinc in elderly immunity: a possible approach in the COVID-19 crisis",
"author": "de Almeida Brasiel",
"doi-asserted-by": "crossref",
"first-page": "65",
"journal-title": "Clin. Nutr. ESPEN",
"key": "10.1016/j.obmed.2022.100420_bib8",
"volume": "38",
"year": "2020"
},
{
"DOI": "10.1016/j.orcp.2020.07.005",
"article-title": "Impact of obesity on hospitalizations and mortality, due to COVID-19: a systematic review",
"author": "de Siqueira",
"doi-asserted-by": "crossref",
"first-page": "398",
"issue": "5",
"journal-title": "Obes. Res. Clin. Pract.",
"key": "10.1016/j.obmed.2022.100420_bib9",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.obmed.2021.100352",
"article-title": "The role of comorbidities on mortality of COVID-19 in patients with diabetes",
"author": "Emami",
"doi-asserted-by": "crossref",
"first-page": "100352",
"journal-title": "Obes. Med.",
"key": "10.1016/j.obmed.2022.100420_bib10",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1016/j.nut.2020.110948",
"article-title": "Vitamin C as prophylaxis and adjunctive medical treatment for COVID-19?",
"author": "Feyaerts",
"doi-asserted-by": "crossref",
"first-page": "110948",
"journal-title": "Nutrition",
"key": "10.1016/j.obmed.2022.100420_bib11",
"volume": "79",
"year": "2020"
},
{
"DOI": "10.1002/oby.23029",
"article-title": "Independent role of severe obesity as a risk factor for COVID-19 hospitalization: a Spanish population-based cohort study",
"author": "Fresán",
"doi-asserted-by": "crossref",
"first-page": "29",
"issue": "1",
"journal-title": "Obesity",
"key": "10.1016/j.obmed.2022.100420_bib12",
"volume": "29",
"year": "2021"
},
{
"DOI": "10.1016/j.phrs.2020.104931",
"article-title": "30-day mortality in patients hospitalized with COVID-19 during the first wave of the Italian epidemic: a prospective cohort study",
"author": "Giacomelli",
"doi-asserted-by": "crossref",
"first-page": "104931",
"journal-title": "Pharmacol. Res.",
"key": "10.1016/j.obmed.2022.100420_bib13",
"volume": "158",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.5394",
"article-title": "Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy",
"author": "Grasselli",
"doi-asserted-by": "crossref",
"first-page": "1574",
"issue": "16",
"journal-title": "JAMA",
"key": "10.1016/j.obmed.2022.100420_bib14",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1177/1558944718797336",
"article-title": "Morbid obesity increases the risk of postoperative wound complications, infection, and repeat surgical procedures following upper extremity limb salvage surgery for soft tissue sarcoma",
"author": "Houdek",
"doi-asserted-by": "crossref",
"first-page": "114",
"issue": "1",
"journal-title": "Hand (N Y).",
"key": "10.1016/j.obmed.2022.100420_bib15",
"volume": "14",
"year": "2019"
},
{
"DOI": "10.1016/j.metabol.2020.154249",
"article-title": "Letter to the Editor: obesity hypoventilation syndrome and severe COVID-19",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "154249",
"journal-title": "Metabolism",
"key": "10.1016/j.obmed.2022.100420_bib16",
"volume": "108",
"year": "2020"
},
{
"DOI": "10.1016/j.metabol.2020.154378",
"article-title": "Obesity in patients with COVID-19: a systematic review and meta-analysis",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "154378",
"journal-title": "Metabolism",
"key": "10.1016/j.obmed.2022.100420_bib17",
"volume": "113",
"year": "2020"
},
{
"DOI": "10.1016/j.orcp.2020.07.002",
"article-title": "Obesity and mortality of COVID-19. Meta-analysis",
"author": "Hussain",
"doi-asserted-by": "crossref",
"first-page": "295",
"issue": "4",
"journal-title": "Obes. Res. Clin. Pract.",
"key": "10.1016/j.obmed.2022.100420_bib18",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1017/dmp.2020.60",
"article-title": "Mortality rate of infection with COVID-19 in Korea from the perspective of underlying disease",
"author": "Kang",
"doi-asserted-by": "crossref",
"first-page": "384",
"issue": "3",
"journal-title": "Disaster Med. Public Health Prep.",
"key": "10.1016/j.obmed.2022.100420_bib19",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1186/s40249-020-00662-x",
"article-title": "Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "45",
"issue": "1",
"journal-title": "Infect. Dis. Poverty",
"key": "10.1016/j.obmed.2022.100420_bib20",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa415",
"article-title": "Obesity in patients younger than 60 Years is a risk factor for COVID-19 hospital admission",
"author": "Lighter",
"doi-asserted-by": "crossref",
"first-page": "896",
"issue": "15",
"journal-title": "Clin. Infect. Dis.",
"key": "10.1016/j.obmed.2022.100420_bib21",
"volume": "71",
"year": "2020"
},
{
"DOI": "10.1038/s41598-021-84782-w",
"article-title": "The in-vitro effect of famotidine on sars-cov-2 proteases and virus replication",
"author": "Loffredo",
"doi-asserted-by": "crossref",
"first-page": "5433",
"issue": "1",
"journal-title": "Sci. Rep.",
"key": "10.1016/j.obmed.2022.100420_bib22",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1093/cid/ciq152",
"article-title": "A novel risk factor for a novel virus: obesity and 2009 pandemic influenza A (H1N1)",
"author": "Louie",
"doi-asserted-by": "crossref",
"first-page": "301",
"issue": "3",
"journal-title": "Clin. Infect. Dis.",
"key": "10.1016/j.obmed.2022.100420_bib23",
"volume": "52",
"year": "2011"
},
{
"DOI": "10.2807/1560-7917.ES.2020.25.10.2000180",
"article-title": "Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020",
"author": "Mizumoto",
"doi-asserted-by": "crossref",
"first-page": "2000180",
"issue": "10",
"journal-title": "Euro Surveill.",
"key": "10.1016/j.obmed.2022.100420_bib24",
"volume": "25",
"year": "2020"
},
{
"article-title": "Experimental. Commentary: obesity: the “Achilles heel” for COVID-19?",
"author": "Muscogiuri",
"journal-title": "Metabol. Clin.",
"key": "10.1016/j.obmed.2022.100420_bib25",
"volume": "108",
"year": "2020"
},
{
"DOI": "10.1038/ijo.2013.16",
"article-title": "Changes in human dendritic cell number and function in severe obesity may contribute to increased susceptibility to viral infection",
"author": "O'Shea",
"doi-asserted-by": "crossref",
"first-page": "1510",
"issue": "11",
"journal-title": "Int. J. Obes.",
"key": "10.1016/j.obmed.2022.100420_bib26",
"volume": "37",
"year": "2013"
},
{
"DOI": "10.1016/j.metabol.2020.154262",
"article-title": "Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York",
"author": "Palaiodimos",
"doi-asserted-by": "crossref",
"first-page": "154262",
"journal-title": "Metabolism",
"key": "10.1016/j.obmed.2022.100420_bib27",
"volume": "108",
"year": "2020"
},
{
"DOI": "10.1016/j.diabet.2020.07.005",
"article-title": "Body mass index and outcome in patients with COVID-19: a dose-response meta-analysis",
"author": "Pranata",
"doi-asserted-by": "crossref",
"first-page": "101178",
"issue": "2",
"journal-title": "Diabetes Metab.",
"key": "10.1016/j.obmed.2022.100420_bib28",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.1016/j.orcp.2019.05.003",
"article-title": "Immunity to influenza: impact of obesity",
"author": "Rojas-Osornio",
"doi-asserted-by": "crossref",
"first-page": "419",
"issue": "5",
"journal-title": "Obes. Res. Clin. Pract.",
"key": "10.1016/j.obmed.2022.100420_bib29",
"volume": "13",
"year": "2019"
},
{
"DOI": "10.1007/s00134-020-05991-x",
"article-title": "Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China",
"author": "Ruan",
"doi-asserted-by": "crossref",
"first-page": "846",
"issue": "5",
"journal-title": "Intensive Care Med.",
"key": "10.1016/j.obmed.2022.100420_bib30",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1111/obr.13083",
"article-title": "Should patients with obesity be more afraid of COVID-19?",
"author": "Rychter",
"doi-asserted-by": "crossref",
"issue": "9",
"journal-title": "Obes. Rev.",
"key": "10.1016/j.obmed.2022.100420_bib31",
"volume": "21",
"year": "2020"
},
{
"article-title": "Viral infection and obesity: current status and future prospective",
"author": "Sartaj Sohrab",
"first-page": "798",
"issue": "9",
"journal-title": "Curr. Drug Metabol.",
"key": "10.1016/j.obmed.2022.100420_bib32",
"volume": "18",
"year": "2017"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.047659",
"article-title": "Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanisms",
"author": "Sattar",
"doi-asserted-by": "crossref",
"first-page": "4",
"issue": "1",
"journal-title": "Circulation",
"key": "10.1016/j.obmed.2022.100420_bib33",
"volume": "142",
"year": "2020"
},
{
"DOI": "10.1016/j.obmed.2020.100316",
"article-title": "Type 2 diabetes is associated with increased risk of critical respiratory illness in patients COVID-19 in a community hospital",
"author": "Shrestha",
"doi-asserted-by": "crossref",
"first-page": "100316",
"journal-title": "Obes. Med.",
"key": "10.1016/j.obmed.2022.100420_bib34",
"volume": "22",
"year": "2021"
},
{
"article-title": "Zinc and respiratory tract infections: perspectives for COVID-19",
"author": "Skalny",
"first-page": "17",
"issue": "1",
"journal-title": "Int. J. Mol. Med.",
"key": "10.1016/j.obmed.2022.100420_bib35",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1002/JLB.3RI0619-181R",
"article-title": "Impact of pregravid obesity on maternal and fetal immunity: fertile grounds for reprogramming",
"author": "Sureshchandra",
"doi-asserted-by": "crossref",
"first-page": "1035",
"issue": "5",
"journal-title": "J. Leukoc. Biol.",
"key": "10.1016/j.obmed.2022.100420_bib36",
"volume": "106",
"year": "2019"
},
{
"DOI": "10.1001/jama.2020.2648",
"article-title": "Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "1239",
"issue": "13",
"journal-title": "JAMA",
"key": "10.1016/j.obmed.2022.100420_bib37",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1016/j.pcd.2020.05.011",
"article-title": "Obesity and risk of COVID-19: analysis of UK biobank",
"author": "Yates",
"doi-asserted-by": "crossref",
"first-page": "566",
"issue": "5",
"journal-title": "Prim. Care Diabetes",
"key": "10.1016/j.obmed.2022.100420_bib38",
"volume": "14",
"year": "2020"
}
],
"reference-count": 38,
"references-count": 38,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S245184762200032X"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Public Health, Environmental and Occupational Health",
"Endocrinology, Diabetes and Metabolism",
"Internal Medicine"
],
"subtitle": [],
"title": "Survival analysis based on body mass index in patients with Covid-19 admitted to the intensive care unit of Amir Al-Momenin Hospital in Arak – 2021",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "32"
}
zangeneh