COVID-19: a vascular nightmare unfolding
et al., Frontiers in Immunology, doi:10.3389/fimmu.2025.1593885, NCT04360824, Aug 2025
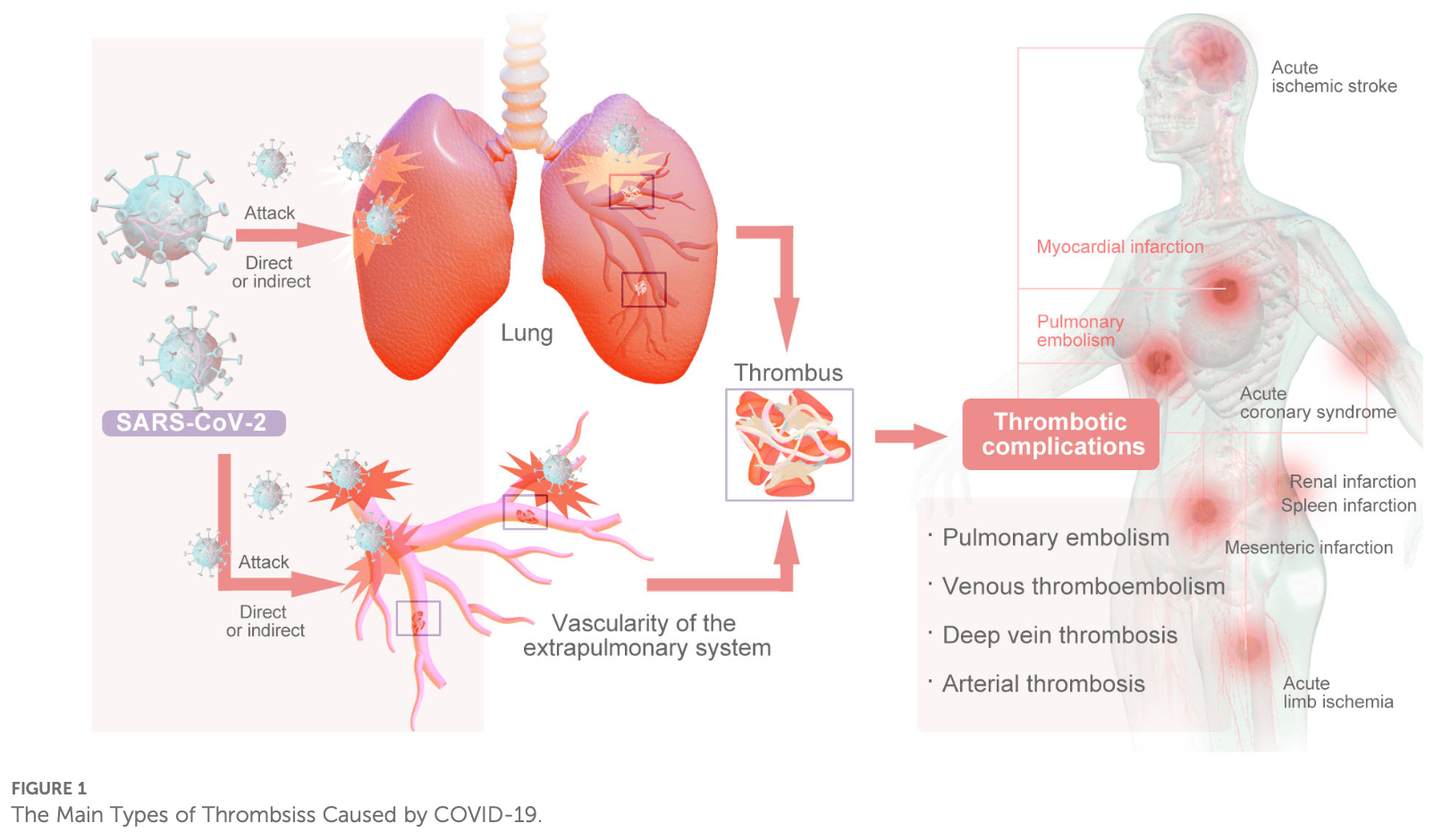
Review of thrombotic complications in COVID-19 patients and anticoagulation strategies. Authors note that COVID-19 induces a prethrombotic state with thrombosis rates of 21% overall, including deep vein thrombosis (20%), pulmonary embolism (8%), and arterial thrombosis (5%), with significantly higher rates in critically ill patients. The mechanisms involve vascular endothelial injury through SARS-CoV-2 binding to ACE-2 receptors, inflammatory cytokine storms with elevated IL-6 and TNF-α, complement system activation, neutrophil extracellular trap formation, and platelet hyperactivation that can persist for at least 40 days post-recovery.
Yin et al., 1 Aug 2025, multiple countries, peer-reviewed, 9 authors, trial NCT04360824 (history).
Contact: bianyuan567@126.com, 550909237@qq.com, yummylia@163.com.
COVID-19: a vascular nightmare unfolding
Frontiers in Immunology, doi:10.3389/fimmu.2025.1593885
The emergence of COVID-19 has been associated with an increased risk of arteriovenous thrombosis, with immune inflammation playing a significant role in the pathogenesis of thrombosis. Numerous drug-related clinical trials have been undertaken to prevent thrombosis, and guidelines for its prevention and treatment are continuously evolving as our understanding of the disease progresses. This article provides a comprehensive review of the mechanisms underlying thrombosis in COVID-19 patients, as well as the advancements in clinical trials and guidelines for thrombosis prevention with pharmacological interventions.
Author contributions QY: Writingoriginal draft, Writingreview & editing, Conceptualization, Methodology. YH: Methodology, Writingoriginal draft, Writingreview & editing. HW: Writing -
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abd Razak, Ismail, Aziz, Suddin, Azzeri et al., Post-COVID syndrome prevalence: a systematic review and meta-analysis, BMC Public Health, doi:10.1186/s12889-024-19264-5
Afshar, Pirzaman, Hosseinzadeh, Babazadeh, Taghizadeh Moghadam et al., Anticoagulant therapy in COVID-19: A narrative review, Clin Transl Sci, doi:10.1111/cts.13569
Afzali, Noris, Lambrecht, Kemper, The state of complement in COVID-19, Nat Rev Immunol, doi:10.1038/s41577-021-00665-1
Ajaz, Mcphail, Singh, Mujib, Trovato et al., Oxidative stress and inflammation in COVID-19-associated sepsis: the potential role of anti-oxidant therapy in avoiding disease progression, American Journal of Physiology-cell Physiology, doi:10.3390/antiox9100936
Ali, Ibrahim, Multi-factorial mechanism behind COVID-19 related thrombosis, Med Arch, doi:10.5455/medarh.2022.76.62-65
Althaus, Marini, Zlamal, Pelzl, Singh et al., Antibodyinduced procoagulant platelets in severe COVID-19 infection, Blood, doi:10.1182/blood.2020008762
Althaus, Zlamal, Bakchoul, Antibody-mediated platelet activation in COVID-19: A coincidence or a new mechanism of the dysregulated coagulation system?, J Thromb Haemost, doi:10.1111/jth.15275
Avdonin, Blinova, Serkova, Komleva, Avdonin, Immunity and coagulation in COVID-19, Int J Mol Sci, doi:10.3390/ijms252011267
Ayyoub, Dhillon, Tura-Ceide, Genetics of long COVID: exploring the molecular drivers of persistent pulmonary vascular disease symptoms, Infect Dis Rep, doi:10.3390/idr17010015
Bagheri, Alipour, Yousefi, Jalalian, Moghimi et al., Prevalence of thromboembolic events, including venous thromboembolism and arterial thrombosis, in patients with COVID-19: A systematic review with meta-analysis, J Tehran Heart Cent, doi:10.18502/jthc.v18i3.14110
Ballering, Van Zon, Hartman, Rosmalen, Corona Research, Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study, Lancet, doi:10.1016/S0140-6736(22)01214-4
Barco, Voci, Held, Sebastian, Bingisser et al., Enoxaparin for primary thromboprophylaxis in symptomatic outpatients with COVID-19 (OVID): a randomised, open-label, parallel-group, multicentre, phase 3 trial, Lancet Haematol, doi:10.1016/S2352-3026(22)00175-2
Becker, Sexton, Smyth, COVID-19 and biomarkers of thrombosis: focus on von Willebrand factor and extracellular vesicles, J Thromb Thrombolysis, doi:10.1007/s11239-021-02544-x
Bikdeli, Talasaz, Rashidi, Bakhshandeh, Rafiee et al., Intermediate-dose versus standard-dose prophylactic anticoagulation in patients with COVID-19 admitted to the intensive care unit: 90-day results from the INSPIRATION randomized trial, Thromb Haemost, doi:10.1055/a-1485-2372
Bohula, Berg, Lopes, Connors, Babar et al., Anticoagulation and antiplatelet therapy for prevention of venous and arterial thrombotic events in critically ill patients with COVID-19: COVID-PACT, Circulation, doi:10.1161/CIRCULATIONAHA.122.061533
Bonaventura, Vecchiéa, Dagna, Martinod, Dixon et al., Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19, Nat Rev Immunol, doi:10.1038/s41577-021-00536-9
Brown, Vaughan, Prothrombotic effects of angiotensin, Advances in Internal Medicine
Burn, Duarte-Salles, Fernandez-Bertolin, Reyes, Kostka et al., Venous or arterial thrombosis and deaths among COVID-19 cases: a European network cohort study, Lancet Infect Dis, doi:10.1016/S1473-3099(22)00223-7
Cappellano, Raineri, Rolla, Giordano, Puricelli et al., Circulating platelet-derived extracellular vesicles are a hallmark of sars-cov-2 infection, Circulation, doi:10.3390/cells10010085
Cervia-Hasler, Brüningk, Hoch, Fan, Muzio et al., Persistent complement dysregulation with signs of thromboinflammation in active Long Covid, Science, doi:10.1126/science.adg7942
Cesta, Zippoli, Marsiglia, Gavioli, Cremonesi et al., Neutrophil activation and neutrophil extracellular traps (NETs) in COVID-19 ARDS and immunothrombosis, Eur J Immunol, doi:10.1002/eji.202250010
Chan, Vanhoutte, Hypoxia, vascular smooth muscles and endothelium, Acta Pharm Sin B, doi:10.1016/j.apsb.2012.12.007
Charles, Ploplis, COVID-19 induces cytokine storm and dysfunctional he mostasi s, C urr Dr ug T argets, doi:10.2174/1389450124666221025102929
Chen, Wang, Zhu, Coagulation disorders and thrombosis in COVID-19 patients and a possible mechanism involving endothelial cells: A review, Aging Dis, doi:10.14336/AD.2021.0704
Chevassut, Hunt, Pavord, VITT, COVID-19 and the Expert Haematology Panel: The story of how the UK responded to emerging cases of vaccine-induced immune thrombocytopenia and thrombosis during the vaccination programme, Clin Med (Lond), doi:10.7861/clinmed.2021-0488
Comer, Cullivan, Szklanna, Weiss, Cullen et al., COVID-19 induces a hyperactive phenotype in circulating platelets, PloS Biol, doi:10.1371/journal.pbio.3001109
Connors, Levy, COVID-19 and its implications for thrombosis and anticoagulation, Blood, doi:10.1182/blood.2020006000
Conway, Pryzdial, Complement contributions to COVID-19, Curr Opin Hematol, doi:10.1097/MOH.0000000000000724
Cuker, Tseng, Nieuwlaat, Angchaisuksiri, Blair et al., American Society of Hematology 2021 guidelines on the use of anticoagulation for thromboprophylaxis in patients with COVID-19, Blood Adv, doi:10.1182/bloodadvances.2020003763
Dai, Xin, Kong, Ding, Fang, Effectiveness and safety of extended thromboprophylaxis in post-discharge patients with COVID-19: A systematic review and meta-analysis, Thromb Res, doi:10.1016/j.thromres.2022.11.019
Eltayeb, Adilovićm, Golzardi, Hromic-Jahjefendića, Rubio-Casillas et al., Intrinsic factors behind long COVID: exploring the role of nucleocapsid protein in thrombosis, PeerJ, doi:10.7717/peerj.19429
Enochs, Colpo, Couture, Baskin, Cahuiche et al., The contribution of neutrophil extracellular traps to coagulopathy in patients with COVID-19-related thrombosis, Viruses, doi:10.3390/v16111677
Fogarty, Ward, Townsend, Karampini, Elliott et al., Sustained VWF-ADAMTS-13 axis imbalance and endotheliopathy in long COVID syndrome is related to immune dysfunction, J Thromb Haemost, doi:10.1111/jth.15830
Galland, Thoreau, Delrue, Neuwirth, Stepanian et al., White blood count, D-dimers, and ferritin levels as predictive factors of pulmonary embolism suspected upon admission in noncritically ill COVID-19 patients: The French multicenter CLOTVID retrospective study, Eur J Haematol, doi:10.1042/BCJ20220016
Ge, Yu, Guo, Li, Ye et al., Complement and complement regulatory proteins are upregulated in lungs of COVID-19 patients, Pathol Res Pract, doi:10.1016/j.prp.2023.154519
Gianni, Goldin, Ngu, Zafeiropoulos, Geropoulos et al., Complement-mediated microvascular injury and thrombosis in the pathogenesis of severe COVID-19: A review, World J Exp Med, doi:10.5493/wjem.v12.i4.53
Goonewardena, Chen, Tate, Grushko, Damodaran et al., Monocyte-mediated thrombosis linked to circulating tissue factor and immune paralysis in COVID-19, Arterioscler Thromb Vasc Biol, doi:10.1161/ATVBAHA.122.318721
Goshua, Pine, Meizlish, Chang, Zhang et al., Endotheliopathy in COVID-19-associated coagulopathy: evidence from a singlecentre, cross-sectional study, Lancet Haematol, doi:10.1016/S2352-3026(20)30216-7
Greenhalgh, Sivan, Perlowski, Nikolich, Long COVID: a clinical update, Lancet, doi:10.1016/S0140-6736(24)01136-X
Greinacher, Thiele, Warkentin, Weisser, Kyrle et al., Thrombotic Thrombocytopenia after ChAdOx1 nCov-19 Vaccination, N Engl J Med, doi:10.1056/NEJMe2106315
Guervilly, Bonifay, Burtey, Sabatier, Cauchois et al., Different potential of extracellular vesicles to support thrombin generation: contributions of phosphatidylserine, tissue factor, and cellular origin, Blood Adv, doi:10.1038/s41598-017-03262-2
Guglielmetti, Quaglia, Sainaghi, Castello, Vaschetto et al., Four years into the pandemic, managing COVID-19 patients with acute coagulopathy: what have we learned?, J Thromb Haemost, doi:10.1542/peds.2022-056726
Gupta, Acharya, Keerti, Common coagulopathies associated with COVID-19 patients, Cureus, doi:10.7759/cureus.38067
Gupta, Zhao, Evans, The stimulation of thrombosis by hypoxia, Thromb Res, doi:10.1016/j.thromres.2019.07.013
Guzik, Mohiddin, Dimarco, Patel, Savvatis et al., COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options, Cardiovasc Res, doi:10.1093/cvr/cvaa106
Hanff, Mohareb, Giri, Cohen, Chirinos, Thrombosis in COVID-19, Am J Hematol, doi:10.1002/ajh.25982
He, Blomback, Wallen, COVID-19: Not a thrombotic disease but a thromboinflammatory disease, Ups J Med Sci, doi:10.48101/ujms.v129.9863
He, Cao, Thalin, Svensson, Blomback et al., The clotting trigger is an important determinant for the coagulation pathway in vivo or in vitro-inference from data review, Semin Thromb Hemost, doi:10.1055/s-0040-1718888
Heidari, Naeimzadeh, Fallahi, Savardashtaki, Razban et al., The role of tissue factor in signaling pathways of pathological conditions and angiogenesis, Curr Mol Med, doi:10.2174/0115665240258746230919165935
Hendaus, Jomha, From COVID-19 to clot: the involvement of the complement system, J Biomol Struct Dyn, doi:10.1080/07391102.2020.1832919
Hess, Hsia, Carroll, Nehler, Ruf et al., Novel tissue factor inhibition for thromboprophylaxis in COVID-19: primary results of the ASPEN-COVID-19 trial, Arterioscler Thromb Vasc Biol, doi:10.1161/ATVBAHA.122.318748
Hippensteel, Lariviere, Colbert, Langouët-Astriécj, Schmidt, Heparin as a therapy for COVID-19: current evidence and future possibilities, American Journal of Physiology-lung Cellular And Molecular Physiology, doi:10.1152/ajplung.00199.2020
Houghton, Wysokinski, Casanegra, Padrnos, Shah et al., Risk of venous thromboembolism after COVID-19 vaccination, Journal of Thrombosis And Haemostasis, doi:10.1111/jth.15725
Ibrahim, Eilenberg, Neumayer, Brostjan, Neutrophil extracellular traps in cardiovascular and aortic disease: A narrative review on molecular mechanisms and therapeutic targeting, Int J Mol Sci, doi:10.3390/ijms25073983
Ishiguro, Matsuo, Fujii, Takayanagi, Acute thrombotic vascular events complicating influenza-associated pneumonia, Respir Med Case Rep, doi:10.1016/j.rmcr.2019.100884
Jara-Palomares, Bikdeli, Jimenez, Muriel, Demelo-Rodriguez et al., Risk of recurrence after discontinuing anticoagulation in patients with COVID-19-associated venous thromboembolism: a prospective multicentre cohort study, EClinicalMedicine, doi:10.1016/j.eclinm.2024.102659
Jevtic, Nazy, The COVID complex: A review of platelet activation and immune complexes in COVID-19, Front Immunol, doi:10.3389/fimmu.2022.807934
Kaiser, Leunig, Pekayvaz, Popp, Joppich et al., Selfsustaining IL-8 loops drive a prothrombotic neutrophil phenotype in severe COVID-19, JCI Insight, doi:10.1172/jci.insight.150862
Kang, Peng, Yan, Al-Badriyeh, Lee et al., Direct oral anticoagulants versus low-molecular-weight heparin in patients with cancer-associated venous thrombosis: a cost-effectiveness analysis, J Pharm Policy Pract, doi:10.1080/20523211.2024.2375269
Khan, Shamma, Kazmi, Altuhami, Ahmed et al., Hypoxia-induced complement dysregulation is associated with microvascular impairments in mouse tracheal transplants, J Transl Med, doi:10.1186/s12967-020-02305-z
Kim, Kim, Kim, Yun, Lee et al., Effectiveness of pfizer-bioNTech and moderna vaccines against COVID-19 among hospitalized adults aged ≥65 years -United States, january-march 2021, MMWR Morb Mortal Wkly Rep, doi:10.1055/s-0041-1727284
Klok, Kruip, Van Der Meer, Arbous, Gommers et al., Incidence of thrombotic complications in critically ill ICU patients with COVID-19, Thromb Res, doi:10.1016/j.thromres.2020.04.013
Laverdure, Sperlich, Fox, Nh, Sørvoll et al., Refractory immune TTP following Pfizer-BioNTech COVID-19 vaccine successfully salvaged with caplacizumab, New England Journal of Medicine, doi:10.1056/NEJMoa2104882
Lee, Jang, Choi, Joh, Kim et al., Comparison of safety and efficacy between therapeutic or intermediate versus prophylactic anticoagulation for thrombosis in COVID-19 patients: a systematic review and meta-analysis, J Thromb Thrombolysis, doi:10.1007/s11239-022-02643-3
Levi, Der Poll, Coagulation and sepsis, Thromb Res, doi:10.1016/j.thromres.2016.11.007
Levi, Thachil, Iba, Levy, Coagulation abnormalities and thrombosis in patients with COVID-19, Lancet Haematol, doi:10.1016/S2352-3026(20)30145-9
Li, Zhang, Zhang, Gu, Huang, Neutrophils in COVID-19: recent insights and advances, Virol J, doi:10.1186/s12985-023-02116-w
Louis, Saad, Vijayakumar, Ilyas, Kokkirala et al., The cardiovascular manifestations of COVID-19, Cardiol Clin, doi:10.1016/j.ccl.2022.03.001
Ma, Willey, The interplay between inflammation and thrombosis in COVID-19: Mechanisms, therapeutic strategies, and challenges, Thromb Update, doi:10.1016/j.tru.2022.100117
Ma, Yang, Huang, Lui, Endothelial contribution to COVID-19: an update on mechanisms and therapeutic implications, J Mol Cell Cardiol, doi:10.1016/j.yjmcc.2021.11.010
Mackman, Tissue factor and COVID-19 associated thrombosis, Arterioscler Thromb Vasc Biol, doi:10.1161/ATVBAHA.123.320144
Manne, Munzer, Badolia, Walker-Allgaier, Campbell et al., PDK1 governs thromboxane generation and thrombosis in platelets by regulating activation of Raf1 in the MAPK pathway, J Thromb Haemost, doi:10.1111/jth.14005
Marchetti, COVID-19-driven endothelial damage: complement, HIF-1, and ABL2 are potential pathways of damage and targets for cure, Ann Hematol, doi:10.1007/s00277-020-04138-8
Mayadas, Cullere, Lowell, The multifaceted functions of neutrophils, Annu Rev Pathology: Mech Dis, doi:10.1146/annurev-pathol-020712-164023
Middleton, He, Denorme, Campbell, Ng et al., Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome, Blood, doi:10.1182/blood.2020007008
Millington-Burgess, Harper, A double-edged sword: antibody-mediated procoagulant platelets in COVID-19, Platelets, doi:10.1080/09537104.2021.1912315
Moness, Mousa, Mousa, Adel, Ibrahim et al., Risk of cardiovascular disease in double heterozygous carriers and homozygous carriers of F5 R506Q (factor V Leiden) and F2 (prothrombin) G20210A: a retrospective family cohort study, British Journal of Haematology, doi:10.1111/j.1365-2141.2010.08529.x
Moores, Tritschler, Brosnahan, Carrier, Collen et al., Thromboprophylaxis and Management of Anticoagulation in Hospitalized Patients with COVID-19, Pulmonary Embolism & Pulmonary Vascular Diseases Group of the Chinese Thoracic Society, Pulmonary Embolism & Pulmonary Vascular Disease Working Committee of Chinese Association of Chest Physicians, National Cooperation Group on Prevention & Treatment of Pulmonary Embolism & Pulmonary Vascular Disease and National Program Office for Prevention Treatment of Pulmonary Embolism & Deep Vein Thrombosis, China Grade Center. Practice guidelines of thromboprophylaxis and management of anticoagulation in hospitalized patients with COVID-19, Chin Med J, doi:10.3760/cma.j.cn112137-2023-01-20-00115
Moores, Tritschler, Brosnahan, Carrier, Collen et al., Thromboprophylaxis in patients with COVID-19: A brief update to the CHEST guideline and expert panel report, Chest, doi:10.1016/j.chest.2022.02.006
Murad, Paracha, Nisar, Unravelling the impact of SARS-CoV-2 on hemostatic and complement systems: a systems immunology perspective, Front Immunol, doi:10.3389/fimmu.2024.1457324
Nara, Shimizu, Yamamoto, Nakamizo, Hayakawa et al., Prolonged platelet hyperactivity after COVID-19 infection, Br J Haematol, doi:10.1111/bjh.19125
Netea, Rovina, Akinosoglou, Antoniadou, Antonakos, Complex immune dysregulation in COVID-19 patients with severe respiratory failure, Cell Host Microbe, doi:10.1016/j.chom.2020.04.009
Nicolai, Kaiser, Stark, Thromboinflammation in long COVID-the elusive key to postinfection sequelae?, J Thromb Haemost, doi:10.1016/j.jtha.2023.04.039
Othman, Zaki, Isa, Ming, Zulkifly, A systematic review of thromboembolic complications and outcomes in hospitalised COVID-19 patients, BMC Infect Dis, doi:10.1186/s12879-024-09374-1
Patel, Zhong, Grant, Oudit, Role of the ACE2/angiotensin 1-7 axis of the renin-angiotensin system in heart failure, Circulation research, doi:10.1161/CIRCRESAHA.116.307708
Pavord, Scully, Hunt, Lester, Bagot et al., Clinical features of vaccine-induced immune thrombocytopenia and thrombosis, N Engl J Med, doi:10.1056/NEJMoa2109908
Pelzl, Singh, Funk, Witzemann, Marini et al., Antibodymediated procoagulant platelet formation in COVID-19 is AKT dependent, J Thromb Haemost, doi:10.1111/jth.15587
Perico, Benigni, Remuzzi, SARS-CoV-2 and the spike protein in endotheliopathy, Trends Microbiol, doi:10.1016/j.tim.2023.06.004
Petry, Shoykhet, Weiser, Griesbaum, Dezfouli et al., SARS-CoV-2 S1 protein induces IgG-mediated platelet activation and is prevented by 1.8-cineole, BioMed Pharmacother, doi:10.1016/j.biopha.2025.118100
Potere, Garrad, Kanthi, Nisio, Kaplanski et al., NLRP3 inflammasome and interleukin-1 contributions to COVID-19-associated coagulopathy and immunothrombosis, Cardiovasc Res, doi:10.1093/cvr/cvad084
Qian, Zang, Zhang, Zheng, Qiu et al., Circulating extracellular vesicles from severe COVID-19 patients induce lung inflammation, mSphere, doi:10.1128/msphere.00764-24
Ramacciotti, Agati, Calderaro, Aguiar, Spyropoulos et al., Rivaroxaban versus no anticoagulation for post-discharge thromboprophylaxis after hospitalisation for COVID-19 (MICHELLE): an openlabel, multicentre, randomised, controlled trial, Lancet, doi:10.1016/S0140-6736(21)02392-8
Ramiro, Mostard, Magro-Checa, Van Dongen, Dormans et al., Historically controlled comparison of glucocorticoids with or without tocilizumab versus supportive care only in patients with COVID-19-associated cytokine storm syndrome: results of the CHIC study, Ann Rheum Dis, doi:10.1136/annrheumdis-2020-218479
Rosell, Havervall, Meijenfeldt, Hisada, Aguilera et al., Patients with COVID-19 have elevated levels of circulating extracellular vesicle tissue factor activity that is associated with severity and mortality-Brief report, Arteriosclerosis Thrombosis Vasc Biol, doi:10.1161/ATVBAHA.120.315547
Rubino, Imburgia, Bonura, Trizzino, Iaria et al., Thromboembolic events in patients with influenza: A scoping review, Viruses, doi:10.3390/v14122817
Ruf, Immune damage in long covid, Science, doi:10.1126/science.adn1077
Ryu, Yan, Montano, Sozmen, Dixit et al., Fibrin drives thromboinflammation and neuropathology in COVID-19, Nature, doi:10.1038/s41586-024-07873-4
Santoro, Nuñez-Gil, Vitale, Viana-Llamas, Romero et al., Aspirin therapy on prophylactic anticoagulation for patients hospitalized with COVID-19: A propensity score-matched cohort analysis of the HOPE-COVID-19 registry, Journal of the American Heart Association, doi:10.1093/eurheartj/ehac544.2715
Sastry, Cuomo, Muthusamy, COVID-19 and thrombosis: The role of hemodynamics, Thromb Res, doi:10.1016/j.thromres.2022.02.016
Savla, Prabhavalkar, Bhatt, Cytokine storm associated coagulation complications in COVID-19 patients: Pathogenesis and Management, Expert Rev Anti Infect Ther, doi:10.1080/14787210.2021.1915129
Sayyadi, Hassani, Shams, Dorgalaleh, Status of major hemostatic components in the setting of COVID-19: the effect on endothelium, platelets, coagulation factors, fibrinolytic system, and complement, Ann Hematol, doi:10.1007/s00277-023-05234-1
Schiavello, Vizio, Bosco, Pivetta, Mariano et al., Extracellular vesicles: new players in the mechanisms of sepsis-and COVID-19-related thromboinflammation, Int J Mol Sci, doi:10.3390/ijms24031920
Schieppati, Post-COVID-19 thrombotic sequelae: The potential role of persistent platelet hyperactivity, Br J Haematol, doi:10.1111/bjh.19159
Schmitt, Manolov, Morgenstern, Fleming, Heitmeier et al., Acute fibrinolysis shutdown occurs early in septic shock and is associated with increased morbidity and mortality: results of an observational pilot study, Ann Intensive Care, doi:10.1186/s13613-019-0499-6
Schulman, Arnold, Bradbury, Broxmeyer, Connors et al., Guidelines for diagnosis, prevention and treatment of COVID-19 in adults in China, J Thromb Haemost, doi:10.3760/cma.j.cn112137-20210112-00090
Sciaudone, Corkrey, Humphries, Koupenova, Platelets and SARS-coV-2 during COVID-19: immunity, thrombosis, and beyond, Circ Res, doi:10.1161/CIRCRESAHA.122.321930
Scully, Singh, Lown, Poles, Solomon et al., Pathologic Antibodies to Platelet Factor 4 after ChAdOx1 nCoV-19 Vaccination, N Engl J Med, doi:10.1056/NEJMoa2105385
Semo, Shomanova, Sindermann, Mohr, Evers et al., Persistent monocytic bioenergetic impairment and mitochondrial DNA damage in PASC patients with cardiovascular complications, Int J Mol Sci, doi:10.3390/ijms26104562
Serrano-Gonzalo, Meneńdez-Jandula, Franco-Garcıá, Arevalo-Vargas, Lahoz-Gil et al., Neutrophil extracellular traps and macrophage activation contibute to thrombosis and post-covid syndrome in SARS-CoV-2 infection, Front Immunol, doi:10.3389/fimmu.2025.1507167
Sholzberg, Tang, Negri, Rahhal, Kreuziger et al., Coagulopathy of hospitalised COVID-19: A Pragmatic Randomised Controlled Trial of Therapeutic Anticoagulation versus Standard Care as a Rapid Response to the COVID-19 Pandemic (RAPID COVID COAG -RAPID Trial): A structured summary of a study protocol for a randomised controlled trial, Trials, doi:10.1186/s13063-021-05076-0
Sholzberg, Tang, Rahhal, Alhamzah, Kreuziger, Effectiveness of therapeutic heparin versus prophylactic heparin on death, mechanical ventilation, or intensive care unit admission in moderately ill patients with covid-19 admitted to hospital: RAPID randomised clinical trial, N Engl J Med, doi:10.1056/NEJMoa2103417
Smadja, Mentzer, Fontenay, Laffan, Ackermann et al., COVID-19 is a systemic vascular hemopathy: insight for mechanistic and clinical aspects, Angiogenesis, doi:10.1007/s10456-021-09805-6
Solomon, Rosen, Treister, Bartov, Intravitreal suture: a complication of pterygium surgery, Ophthalmic Surg, doi:10.3928/1542-8877-19910101-16
Soriano, Murthy, Marshall, Relan, Diaz, A clinical case definition of post-COVID-19 condition by a Delphi consensus, Lancet Infect Dis, doi:10.1016/S1473-3099(21)00703-9
Soy, Keser, Atagunduz, Tabak, Atagunduz et al., Cytokine storm in COVID-19: pathogenesis and overview of anti-inflammatory agents used in treatment, Clin Rheumatol, doi:10.1007/s10067-020-05190-5
Spyropoulos, Goldin, Giannis, Diab, Wang et al., Efficacy and safety of therapeutic-dose heparin vs standard prophylactic or intermediate-dose heparins for thromboprophylaxis in high-risk hospitalized patients with COVID-19: the HEP-COVID randomized clinical trial, JAMA Intern Med, doi:10.1111/jth.15450
Stasi, Fallani, Voller, Silvestri, Treatment for COVID-19: an overview, Eur J Pharmacol, doi:10.1016/j.ejphar.2020.173644
Stone, Farkouh, Tinuoye, Dressler, Moreno, Therapeutic versus prophylactic anticoagulation for patients admitted to hospital with COVID-19 and elevated D-dimer concentration (ACTION): an open-label, multicentre, randomised, controlled trial, J Am Coll Cardiol, doi:10.1016/S0140-6736(21)01203-4
Sung, Sun, Tao, Hsieh, Inhibition of SARS-coV-2-mediated thromboinflammation by CLEC2.Fc, EMBO Mol Med, doi:10.15252/emmm.202216351
Szilveszter, Pal, Simon-Szabo, Oz, Moldovan et al., The management of COVID-19-related coagulopathy: A focus on the challenges of metabolic and vascular diseases, Int J Mol Sci, doi:10.3390/ijms241612782
Tang, Li, Wang, Sun, Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia, J Thromb Haemostasis, doi:10.1111/jth.14768
Taus, Salvagno, Cane, Fava, Mazzaferri et al., Platelets promote thromboinflammation in SARS-coV-2 pneumonia, Arterioscler Thromb Vasc Biol, doi:10.1161/ATVBAHA.120.315175
Teodoro, Rodrigues, Farnesi-De-Assuncao, Borges, Obata et al., Inflammatory response and activation of coagulation after COVID-19 infection, Viruses, doi:10.3390/v15040938
Theofilis, Sagris, Antonopoulos, Oikonomou, Tsioufis et al., Inflammatory mediators of platelet activation: focus on atherosclerosis and COVID-19, International Journal of Molecular Sciences, doi:10.3390/ijms222011170
Thierry, Salmon, Inflammation-, immunothrombosis,-and autoimmunefeedback loops may lead to persistent neutrophil self-stimulation in long COVID, J Med Virol, doi:10.1002/jmv.29887
Torabizadeh, Asfeh, Zayeri, Kazemi, Saki, Implications of complement imbalance in COVID-19: A molecular mechanistic discussion on the importance of complement balance, Iran J Immunol, doi:10.22034/iji.2023.97585.2522
Turner, Khan, Putrino, Woodcock, Kell et al., Long COVID: pathophysiological factors and abnormalities of coagulation, Trends Endocrinol Metab, doi:10.1016/j.tem.2023.03.002
Valencia, Lumpuy-Castillo, Magalhaes, Sanchez-Ferrer, Lorenzo et al., Mechanisms of endothelial activation, hypercoagulation and thrombosis in COVID-19: a link with diabetes mellitus, Cardiovasc Diabetol, doi:10.1186/s12933-023-02097-8
Varga, Flammer, Steiger, Haberecker, Andermatt et al., Endothelial cell infection and endotheliitis in COVID-19, Lancet, doi:10.1016/S0140-6736(20)30937-5
Vieceli, Sega, Fortini, Licastro, Monego et al., Serum from COVID-19 patients promotes endothelial cell dysfunction through protease-activated receptor 2, Inflammation Res, doi:10.1007/s00011-023-01823-y
Violi, Pignatelli, Cammisotto, Carnevale, Nocella, COVID-19 and thrombosis: Clinical features, mechanism of disease, and therapeutic implications, Kardiol Pol, doi:10.33963/KP.a2021.0154
Voci, Gotschi, Held, Bingisser, Colucci et al., Enoxaparin for outpatients with COVID-19: 90-day results from the randomised, open-label, parallel-group, multinational, phase III OVID trial, Thromb Res, doi:10.1016/j.thromres.2022.10.021
Weinberg, Sena, Chandel, Mitochondria in the regulation of innate and adaptive immunity, Immunity, doi:10.1016/j.immuni.2015.02.002
Weiss, Mostageer, Eichhorn, Huber, Egger et al., The fluorochrome-to-protein ratio is crucial for the flow cytometric detection of tissue factor on extracellular vesicles, Sci Rep, doi:10.1038/s41598-024-56841-5
Wolf, Khimani, Yoon, Gerhart, Endsley et al., The mechanistic basis linking cytokine storm to thrombosis in COVID-19, Thromb Update, doi:10.1016/j.tru.2022.100110
Wong, Wu, To, Lee, Lam et al., Tissue factor expression, extracellular vesicles, and thrombosis after infection with the respiratory viruses influenza A virus and coronavirus, Bmj-british Medical Journal, doi:10.1111/jth.15509
Xiao, Ellsworth, Qin, Emerging role of complement in COVID-19 and other respiratory virus diseases, Cell Mol Life Sci, doi:10.1007/s00018-024-05157-8
Xie, Xu, Bowe, Al-Aly, Long-term cardiovascular outcomes of COVID-19, Nat Med, doi:10.1038/s41591-022-01689-3
Xu, Ilyas, Weng, Endothelial dysfunction in COVID-19: an overview of evidence, biomarkers, mechanisms and potential therapies, Acta Pharmacol Sin, doi:10.1038/s41401-022-00998-0
Yin, Zhang, Liao, Huang, Wan et al., Potential anticoagulant of traditional chinese medicine and novel targets for anticoagulant drugs, Phytomedicine, doi:10.1016/j.phymed.2023.154880
Yu, Yuan, Chen, Chaturvedi, Braunstein et al., Direct activation of the alternative complement pathway by SARS-CoV-2 spike proteins is blocked by factor D inhibition, Blood, doi:10.1182/blood.2020008248
Zanini, Selleri, Roncati, Coppi, Nasi et al., Vascular "Long COVID": A new vessel disease?, Angiology, doi:10.1177/00033197231153204
Zhang, Liu, Wang, Yang, Li et al., SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19, J Hematol Oncol, doi:10.1186/s13045-020-00954-7
Zhu, Chen, Liu, NETosis and neutrophil extracellular traps in COVID-19: immunothrombosis and beyond, Front Immunol, doi:10.3389/fimmu.2022.838011
Zuin, Barco, Giannakoulas, Engelen, Hobohm et al., Risk of venous thromboembolic events after COVID-19 infection: a systematic review and metaanalysis, J Thromb Thrombolysis, doi:10.1007/s11239-022-02766-7
DOI record:
{
"DOI": "10.3389/fimmu.2025.1593885",
"ISSN": [
"1664-3224"
],
"URL": "http://dx.doi.org/10.3389/fimmu.2025.1593885",
"abstract": "<jats:p>The emergence of COVID-19 has been associated with an increased risk of arteriovenous thrombosis, with immune inflammation playing a significant role in the pathogenesis of thrombosis. Numerous drug-related clinical trials have been undertaken to prevent thrombosis, and guidelines for its prevention and treatment are continuously evolving as our understanding of the disease progresses. This article provides a comprehensive review of the mechanisms underlying thrombosis in COVID-19 patients, as well as the advancements in clinical trials and guidelines for thrombosis prevention with pharmacological interventions.</jats:p>",
"alternative-id": [
"10.3389/fimmu.2025.1593885"
],
"article-number": "1593885",
"author": [
{
"affiliation": [],
"family": "Yin",
"given": "Qinan",
"sequence": "first"
},
{
"affiliation": [],
"family": "Huang",
"given": "Youjin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wang",
"given": "Hulin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wang",
"given": "Yin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Huang",
"given": "Xuefei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Song",
"given": "Yujie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wang",
"given": "Yueyuan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Han",
"given": "Lizhu",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yuan",
"given": "Bian",
"sequence": "additional"
}
],
"container-title": "Frontiers in Immunology",
"container-title-short": "Front. Immunol.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2025,
8,
1
]
],
"date-time": "2025-08-01T05:33:27Z",
"timestamp": 1754026407000
},
"deposited": {
"date-parts": [
[
2025,
8,
1
]
],
"date-time": "2025-08-01T05:33:31Z",
"timestamp": 1754026411000
},
"funder": [
{
"DOI": "10.13039/501100012166",
"award": [
"2020YFC2005500"
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/501100012166",
"id-type": "DOI"
}
],
"name": "National Key Research and Development Program of China"
}
],
"indexed": {
"date-parts": [
[
2025,
8,
1
]
],
"date-time": "2025-08-01T06:10:05Z",
"timestamp": 1754028605520,
"version": "3.41.2"
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2025,
8,
1
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
8,
1
]
],
"date-time": "2025-08-01T00:00:00Z",
"timestamp": 1754006400000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fimmu.2025.1593885/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2025,
8,
1
]
]
},
"published-online": {
"date-parts": [
[
2025,
8,
1
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1016/j.tem.2023.03.002",
"article-title": "Long COVID: pathophysiological factors and abnormalities of coagulation",
"author": "Turner",
"doi-asserted-by": "publisher",
"journal-title": "Trends Endocrinol Metab",
"key": "B1",
"volume": "34",
"year": "2023"
},
{
"DOI": "10.1038/s41401-022-00998-0",
"article-title": "Endothelial dysfunction in COVID-19: an overview of evidence, biomarkers, mechanisms and potential therapies",
"author": "Xu",
"doi-asserted-by": "publisher",
"first-page": "695",
"journal-title": "Acta Pharmacol Sin",
"key": "B2",
"volume": "44",
"year": "2023"
},
{
"DOI": "10.1182/blood.2020006000",
"article-title": "COVID-19 and its implications for thrombosis and anticoagulation",
"author": "Connors",
"doi-asserted-by": "publisher",
"journal-title": "Blood",
"key": "B3",
"volume": "135",
"year": "2020"
},
{
"DOI": "10.1002/ajh.25982",
"article-title": "Thrombosis in COVID-19",
"author": "Hanff",
"doi-asserted-by": "publisher",
"journal-title": "Am J Hematol",
"key": "B4",
"volume": "95",
"year": "2020"
},
{
"DOI": "10.33963/KP.a2021.0154",
"article-title": "COVID-19 and thrombosis: Clinical features, mechanism of disease, and therapeutic implications",
"author": "Violi",
"doi-asserted-by": "publisher",
"journal-title": "Kardiol Pol",
"key": "B5",
"volume": "79",
"year": "2021"
},
{
"DOI": "10.1016/j.ccl.2022.03.001",
"article-title": "The cardiovascular manifestations of COVID-19",
"author": "Louis",
"doi-asserted-by": "publisher",
"journal-title": "Cardiol Clin",
"key": "B6",
"volume": "40",
"year": "2022"
},
{
"DOI": "10.1111/jth.14768",
"article-title": "Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia",
"author": "Tang",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Haemostasis",
"key": "B7",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1186/s12879-024-09374-1",
"article-title": "A systematic review of thromboembolic complications and outcomes in hospitalised COVID-19 patients",
"author": "Othman",
"doi-asserted-by": "publisher",
"first-page": "484",
"journal-title": "BMC Infect Dis",
"key": "B8",
"volume": "24",
"year": "2024"
},
{
"DOI": "10.18502/jthc.v18i3.14110",
"article-title": "Prevalence of thromboembolic events, including venous thromboembolism and arterial thrombosis, in patients with COVID-19: A systematic review with meta-analysis",
"author": "Bagheri",
"doi-asserted-by": "publisher",
"journal-title": "J Tehran Heart Cent",
"key": "B9",
"volume": "18",
"year": "2023"
},
{
"DOI": "10.1007/s11239-022-02766-7",
"article-title": "Risk of venous thromboembolic events after COVID-19 infection: a systematic review and meta-analysis",
"author": "Zuin",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Thrombolysis",
"key": "B10",
"volume": "55",
"year": "2023"
},
{
"DOI": "10.1016/S1473-3099(22)00223-7",
"article-title": "Venous or arterial thrombosis and deaths among COVID-19 cases: a European network cohort study",
"author": "Burn",
"doi-asserted-by": "publisher",
"journal-title": "Lancet Infect Dis",
"key": "B11",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1186/s12889-024-19264-5",
"article-title": "Post-COVID syndrome prevalence: a systematic review and meta-analysis",
"author": "Sk Abd Razak",
"doi-asserted-by": "publisher",
"first-page": "1785",
"journal-title": "BMC Public Health",
"key": "B12",
"volume": "24",
"year": "2024"
},
{
"DOI": "10.1016/j.eclinm.2024.102659",
"article-title": "Risk of recurrence after discontinuing anticoagulation in patients with COVID-19- associated venous thromboembolism: a prospective multicentre cohort study",
"author": "Jara-Palomares",
"doi-asserted-by": "publisher",
"first-page": "102659",
"journal-title": "EClinicalMedicine",
"key": "B13",
"volume": "73",
"year": "2024"
},
{
"DOI": "10.1055/s-0040-1718888",
"article-title": "The clotting trigger is an important determinant for the coagulation pathway in vivo or in vitro-inference from data review",
"author": "He",
"doi-asserted-by": "publisher",
"first-page": "63",
"journal-title": "Semin Thromb Hemost",
"key": "B14",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.1016/j.phymed.2023.154880",
"article-title": "Potential anticoagulant of traditional chinese medicine and novel targets for anticoagulant drugs",
"author": "Yin",
"doi-asserted-by": "publisher",
"first-page": "154880",
"journal-title": "Phytomedicine",
"key": "B15",
"volume": "116",
"year": "2023"
},
{
"DOI": "10.1016/S0140-6736(20)30937-5",
"article-title": "Endothelial cell infection and endotheliitis in COVID-19",
"author": "Varga",
"doi-asserted-by": "publisher",
"journal-title": "Lancet",
"key": "B16",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1186/s13045-020-00954-7",
"article-title": "SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "120",
"journal-title": "J Hematol Oncol",
"key": "B17",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1016/S2352-3026(20)30216-7",
"article-title": "Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study",
"author": "Goshua",
"doi-asserted-by": "publisher",
"journal-title": "Lancet Haematol",
"key": "B18",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1007/s10456-021-09805-6",
"article-title": "COVID-19 is a systemic vascular hemopathy: insight for mechanistic and clinical aspects",
"author": "Smadja",
"doi-asserted-by": "publisher",
"journal-title": "Angiogenesis",
"key": "B19",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1016/S2352-3026(20)30145-9",
"article-title": "Coagulation abnormalities and thrombosis in patients with COVID-19",
"author": "Levi",
"doi-asserted-by": "publisher",
"journal-title": "Lancet Haematol",
"key": "B20",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1161/ATVBAHA.122.318721",
"article-title": "Monocyte-mediated thrombosis linked to circulating tissue factor and immune paralysis in COVID-19",
"author": "Goonewardena",
"doi-asserted-by": "publisher",
"journal-title": "Arterioscler Thromb Vasc Biol",
"key": "B21",
"volume": "44",
"year": "2024"
},
{
"DOI": "10.1186/s12933-023-02097-8",
"article-title": "Mechanisms of endothelial activation, hypercoagulation and thrombosis in COVID-19: a link with diabetes mellitus",
"author": "Valencia",
"doi-asserted-by": "publisher",
"first-page": "75",
"journal-title": "Cardiovasc Diabetol",
"key": "B22",
"volume": "23",
"year": "2024"
},
{
"DOI": "10.5455/medarh.2022.76.62-65",
"article-title": "Multi-factorial mechanism behind COVID-19 related thrombosis",
"author": "Ali",
"doi-asserted-by": "publisher",
"journal-title": "Med Arch",
"key": "B23",
"volume": "76",
"year": "2022"
},
{
"DOI": "10.1016/j.tru.2022.100117",
"article-title": "The interplay between inflammation and thrombosis in COVID-19: Mechanisms, therapeutic strategies, and challenges",
"author": "Ma",
"doi-asserted-by": "publisher",
"first-page": "100117",
"journal-title": "Thromb Update",
"key": "B24",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.1016/j.yjmcc.2021.11.010",
"article-title": "Endothelial contribution to COVID-19: an update on mechanisms and therapeutic implications",
"author": "Ma",
"doi-asserted-by": "publisher",
"first-page": "69",
"journal-title": "J Mol Cell Cardiol",
"key": "B25",
"volume": "164",
"year": "2022"
},
{
"DOI": "10.1161/CIRCRESAHA.116.307708",
"article-title": "Role of the ACE2/angiotensin 1–7 axis of the renin–angiotensin system in heart failure",
"author": "Patel",
"doi-asserted-by": "publisher",
"journal-title": "Circulation research",
"key": "B26",
"volume": "118",
"year": "2016"
},
{
"article-title": "Prothrombotic effects of angiotensin",
"author": "Brown",
"journal-title": "Advances in Internal Medicine",
"key": "B27",
"volume": "45",
"year": "2000"
},
{
"DOI": "10.1016/j.tru.2022.100110",
"article-title": "The mechanistic basis linking cytokine storm to thrombosis in COVID-19",
"author": "Wolf",
"doi-asserted-by": "publisher",
"first-page": "100110",
"journal-title": "Thromb Update",
"key": "B28",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.1038/s41577-021-00536-9",
"article-title": "Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19",
"author": "Bonaventura",
"doi-asserted-by": "publisher",
"journal-title": "Nat Rev Immunol",
"key": "B29",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.2174/0115665240258746230919165935",
"article-title": "The role of tissue factor in signaling pathways of pathological conditions and angiogenesis",
"author": "Heidari",
"doi-asserted-by": "publisher",
"journal-title": "Curr Mol Med",
"key": "B30",
"volume": "24",
"year": "2023"
},
{
"DOI": "10.1161/ATVBAHA.123.320144",
"article-title": "Tissue factor and COVID-19 associated thrombosis",
"author": "Mackman",
"doi-asserted-by": "publisher",
"journal-title": "Arterioscler Thromb Vasc Biol",
"key": "B31",
"volume": "44",
"year": "2024"
},
{
"DOI": "10.1177/00033197231153204",
"article-title": "Vascular “Long COVID”: A new vessel disease",
"author": "Zanini",
"doi-asserted-by": "publisher",
"first-page": "8",
"journal-title": "Angiology",
"key": "B32",
"volume": "75",
"year": "2024"
},
{
"DOI": "10.1016/j.tim.2023.06.004",
"article-title": "SARS-CoV-2 and the spike protein in endotheliopathy",
"author": "Perico",
"doi-asserted-by": "publisher",
"first-page": "53",
"journal-title": "Trends Microbiol",
"key": "B33",
"volume": "32",
"year": "2024"
},
{
"DOI": "10.1016/j.thromres.2016.11.007",
"article-title": "Coagulation and sepsis",
"author": "Levi",
"doi-asserted-by": "publisher",
"first-page": "38",
"journal-title": "Thromb Res",
"key": "B34",
"volume": "149",
"year": "2017"
},
{
"DOI": "10.1186/s13613-019-0499-6",
"article-title": "Acute fibrinolysis shutdown occurs early in septic shock and is associated with increased morbidity and mortality: results of an observational pilot study",
"author": "Schmitt",
"doi-asserted-by": "publisher",
"first-page": "19",
"journal-title": "Ann Intensive Care",
"key": "B35",
"volume": "9",
"year": "2019"
},
{
"DOI": "10.1007/s00277-020-04138-8",
"article-title": "COVID-19-driven endothelial damage: complement, HIF-1, and ABL2 are potential pathways of damage and targets for cure",
"author": "Marchetti",
"doi-asserted-by": "publisher",
"journal-title": "Ann Hematol",
"key": "B36",
"volume": "99",
"year": "2020"
},
{
"DOI": "10.1007/s00011-023-01823-y",
"article-title": "Serum from COVID-19 patients promotes endothelial cell dysfunction through protease-activated receptor 2",
"author": "Vieceli Dalla Sega",
"doi-asserted-by": "publisher",
"journal-title": "Inflammation Res",
"key": "B37",
"volume": "73",
"year": "2024"
},
{
"DOI": "10.1111/cts.13569",
"article-title": "Anticoagulant therapy in COVID-19: A narrative review",
"author": "Mohseni Afshar",
"doi-asserted-by": "publisher",
"journal-title": "Clin Transl Sci",
"key": "B38",
"volume": "16",
"year": "2023"
},
{
"DOI": "10.1126/science.adg7942",
"article-title": "Persistent complement dysregulation with signs of thromboinflammation in active Long Covid",
"author": "Cervia-Hasler",
"doi-asserted-by": "publisher",
"journal-title": "Science",
"key": "B39",
"volume": "383",
"year": "2024"
},
{
"DOI": "10.1016/j.thromres.2022.02.016",
"article-title": "COVID-19 and thrombosis: The role of hemodynamics",
"author": "Sastry",
"doi-asserted-by": "publisher",
"journal-title": "Thromb Res",
"key": "B40",
"volume": "212",
"year": "2022"
},
{
"DOI": "10.14336/AD.2021.0704",
"article-title": "Coagulation disorders and thrombosis in COVID-19 patients and a possible mechanism involving endothelial cells: A review",
"author": "Chen",
"doi-asserted-by": "publisher",
"journal-title": "Aging Dis",
"key": "B41",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/j.jtha.2023.04.039",
"article-title": "Thromboinflammation in long COVID-the elusive key to postinfection sequelae",
"author": "Nicolai",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Haemost",
"key": "B42",
"volume": "21",
"year": "2023"
},
{
"DOI": "10.1111/jth.15830",
"article-title": "Sustained VWF-ADAMTS-13 axis imbalance and endotheliopathy in long COVID syndrome is related to immune dysfunction",
"author": "Fogarty",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Haemost",
"key": "B43",
"volume": "20",
"year": "2022"
},
{
"DOI": "10.1016/j.apsb.2012.12.007",
"article-title": "Hypoxia, vascular smooth muscles and endothelium",
"author": "Chan",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Acta Pharm Sin B",
"key": "B44",
"volume": "3",
"year": "2013"
},
{
"DOI": "10.1016/j.thromres.2019.07.013",
"article-title": "The stimulation of thrombosis by hypoxia",
"author": "Gupta",
"doi-asserted-by": "publisher",
"first-page": "77",
"journal-title": "Thromb Res",
"key": "B45",
"volume": "181",
"year": "2019"
},
{
"DOI": "10.1186/s12967-020-02305-z",
"article-title": "Hypoxia-induced complement dysregulation is associated with microvascular impairments in mouse tracheal transplants",
"author": "Khan",
"doi-asserted-by": "publisher",
"first-page": "147",
"journal-title": "J Transl Med",
"key": "B46",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1136/annrheumdis-2020-218479",
"article-title": "Historically controlled comparison of glucocorticoids with or without tocilizumab versus supportive care only in patients with COVID-19-associated cytokine storm syndrome: results of the CHIC study",
"author": "Ramiro",
"doi-asserted-by": "publisher",
"journal-title": "Ann Rheum Dis",
"key": "B47",
"volume": "79",
"year": "2020"
},
{
"DOI": "10.3928/1542-8877-19910101-16",
"article-title": "Intravitreal suture: a complication of pterygium surgery",
"author": "Solomon",
"doi-asserted-by": "publisher",
"journal-title": "Ophthalmic Surg",
"key": "B48",
"volume": "22",
"year": "1991"
},
{
"DOI": "10.1016/j.ejphar.2020.173644",
"article-title": "Treatment for COVID-19: an overview",
"author": "Stasi",
"doi-asserted-by": "publisher",
"first-page": "173644",
"journal-title": "Eur J Pharmacol",
"key": "B49",
"volume": "889",
"year": "2020"
},
{
"DOI": "10.1080/14787210.2021.1915129",
"article-title": "Cytokine storm associated coagulation complications in COVID-19 patients: Pathogenesis and Management",
"author": "Savla",
"doi-asserted-by": "publisher",
"journal-title": "Expert Rev Anti Infect Ther",
"key": "B50",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.3390/ijms252011267",
"article-title": "Immunity and coagulation in COVID-19",
"author": "Avdonin",
"doi-asserted-by": "publisher",
"journal-title": "Int J Mol Sci",
"key": "B51",
"volume": "25",
"year": "2024"
},
{
"DOI": "10.1007/s10067-020-05190-5",
"article-title": "Cytokine storm in COVID-19: pathogenesis and overview of anti-inflammatory agents used in treatment",
"author": "Soy",
"doi-asserted-by": "publisher",
"journal-title": "Clin Rheumatol",
"key": "B52",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.2174/1389450124666221025102929",
"article-title": "COVID-19 induces cytokine storm and dysfunctional hemostasis",
"author": "Charles",
"doi-asserted-by": "publisher",
"journal-title": "Curr Drug Targets",
"key": "B53",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1016/j.chom.2020.04.009",
"article-title": "Complex immune dysregulation in COVID-19 patients with severe respiratory failure",
"author": "Giamarellos-Bourboulis",
"doi-asserted-by": "publisher",
"first-page": "992",
"journal-title": "Cell Host Microbe",
"key": "B54",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.7759/cureus.38067",
"article-title": "Common coagulopathies associated with COVID-19 patients",
"author": "Gupta",
"doi-asserted-by": "publisher",
"journal-title": "Cureus",
"key": "B55",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.3390/ijms241612782",
"article-title": "The management of COVID-19-related coagulopathy: A focus on the challenges of metabolic and vascular diseases",
"author": "Szilveszter",
"doi-asserted-by": "publisher",
"journal-title": "Int J Mol Sci",
"key": "B56",
"volume": "24",
"year": "2023"
},
{
"DOI": "10.3390/v15040938",
"article-title": "Inflammatory response and activation of coagulation after COVID-19 infection",
"author": "Teodoro",
"doi-asserted-by": "publisher",
"journal-title": "Viruses",
"key": "B57",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1093/cvr/cvad084",
"article-title": "NLRP3 inflammasome and interleukin-1 contributions to COVID-19-associated coagulopathy and immunothrombosis",
"author": "Potere",
"doi-asserted-by": "publisher",
"journal-title": "Cardiovasc Res",
"key": "B58",
"volume": "119",
"year": "2023"
},
{
"DOI": "10.1097/MOH.0000000000000724",
"article-title": "Complement contributions to COVID-19",
"author": "Conway",
"doi-asserted-by": "publisher",
"journal-title": "Curr Opin Hematol",
"key": "B59",
"volume": "29",
"year": "2022"
},
{
"DOI": "10.1080/07391102.2020.1832919",
"article-title": "From COVID-19 to clot: the involvement of the complement system",
"author": "Hendaus",
"doi-asserted-by": "publisher",
"journal-title": "J Biomol Struct Dyn",
"key": "B60",
"volume": "40",
"year": "2022"
},
{
"DOI": "10.7717/peerj.19429",
"article-title": "Intrinsic factors behind long COVID: exploring the role of nucleocapsid protein in thrombosis",
"author": "Eltayeb",
"doi-asserted-by": "publisher",
"journal-title": "PeerJ",
"key": "B61",
"volume": "13",
"year": "2025"
},
{
"DOI": "10.1016/j.prp.2023.154519",
"article-title": "Complement and complement regulatory proteins are upregulated in lungs of COVID-19 patients",
"author": "Ge",
"doi-asserted-by": "publisher",
"first-page": "154519",
"journal-title": "Pathol Res Pract",
"key": "B62",
"volume": "247",
"year": "2023"
},
{
"DOI": "10.5493/wjem.v12.i4.53",
"article-title": "Complement-mediated microvascular injury and thrombosis in the pathogenesis of severe COVID-19: A review",
"author": "Gianni",
"doi-asserted-by": "publisher",
"first-page": "53",
"journal-title": "World J Exp Med",
"key": "B63",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1182/blood.2020008248",
"article-title": "Direct activation of the alternative complement pathway by SARS-CoV-2 spike proteins is blocked by factor D inhibition",
"author": "Yu",
"doi-asserted-by": "publisher",
"journal-title": "Blood",
"key": "B64",
"volume": "136",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2024.1457324",
"article-title": "Unravelling the impact of SARS-CoV-2 on hemostatic and complement systems: a systems immunology perspective",
"author": "Murad",
"doi-asserted-by": "publisher",
"journal-title": "Front Immunol",
"key": "B65",
"volume": "15",
"year": "2024"
},
{
"DOI": "10.1126/science.adn1077",
"article-title": "Immune damage in long covid",
"author": "Ruf",
"doi-asserted-by": "publisher",
"journal-title": "Science",
"key": "B66",
"volume": "383",
"year": "2024"
},
{
"DOI": "10.1002/eji.202250010",
"article-title": "Neutrophil activation and neutrophil extracellular traps (NETs) in COVID-19 ARDS and immunothrombosis",
"author": "Cesta",
"doi-asserted-by": "publisher",
"journal-title": "Eur J Immunol",
"key": "B67",
"volume": "53",
"year": "2023"
},
{
"DOI": "10.1038/s41577-021-00665-1",
"article-title": "The state of complement in COVID-19",
"author": "Afzali",
"doi-asserted-by": "publisher",
"first-page": "77",
"journal-title": "Nat Rev Immunol",
"key": "B68",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.22034/iji.2023.97585.2522",
"article-title": "Implications of complement imbalance in COVID-19: A molecular mechanistic discussion on the importance of complement balance",
"author": "Torabizadeh",
"doi-asserted-by": "publisher",
"journal-title": "Iran J Immunol",
"key": "B69",
"volume": "3",
"year": "2023"
},
{
"DOI": "10.1146/annurev-pathol-020712-164023",
"article-title": "The multifaceted functions of neutrophils",
"author": "Mayadas",
"doi-asserted-by": "publisher",
"first-page": "181",
"journal-title": "Annu Rev Pathology: Mech Dis",
"key": "B70",
"volume": "9",
"year": "2014"
},
{
"DOI": "10.3390/v16111677",
"article-title": "The contribution of neutrophil extracellular traps to coagulopathy in patients with COVID-19-related thrombosis",
"author": "Enochs",
"doi-asserted-by": "publisher",
"journal-title": "Viruses",
"key": "B71",
"volume": "16",
"year": "2024"
},
{
"DOI": "10.1002/jmv.29887",
"article-title": "Inflammation-, immunothrombosis,- and autoimmune-feedback loops may lead to persistent neutrophil self-stimulation in long COVID",
"author": "Thierry",
"doi-asserted-by": "publisher",
"journal-title": "J Med Virol",
"key": "B72",
"volume": "96",
"year": "2024"
},
{
"DOI": "10.3389/fimmu.2025.1507167",
"article-title": "Neutrophil extracellular traps and macrophage activation contibute to thrombosis and post-covid syndrome in SARS-CoV-2 infection",
"author": "Serrano-Gonzalo",
"doi-asserted-by": "publisher",
"journal-title": "Front Immunol",
"key": "B73",
"volume": "16",
"year": "2025"
},
{
"DOI": "10.15252/emmm.202216351",
"article-title": "Inhibition of SARS-coV-2-mediated thromboinflammation by CLEC2.Fc",
"author": "Sung",
"doi-asserted-by": "publisher",
"first-page": "e16351",
"journal-title": "EMBO Mol Med",
"key": "B74",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1007/s00018-024-05157-8",
"article-title": "Emerging role of complement in COVID-19 and other respiratory virus diseases",
"author": "Xiao",
"doi-asserted-by": "publisher",
"first-page": "94",
"journal-title": "Cell Mol Life Sci",
"key": "B75",
"volume": "81",
"year": "2024"
},
{
"DOI": "10.3390/ijms25073983",
"article-title": "Neutrophil extracellular traps in cardiovascular and aortic disease: A narrative review on molecular mechanisms and therapeutic targeting",
"author": "Ibrahim",
"doi-asserted-by": "publisher",
"journal-title": "Int J Mol Sci",
"key": "B76",
"volume": "25",
"year": "2024"
},
{
"DOI": "10.1172/jci.insight.150862",
"article-title": "Self-sustaining IL-8 loops drive a prothrombotic neutrophil phenotype in severe COVID-19",
"author": "Kaiser",
"doi-asserted-by": "publisher",
"journal-title": "JCI Insight",
"key": "B77",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1182/blood.2020007008",
"article-title": "Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome",
"author": "Middleton",
"doi-asserted-by": "publisher",
"journal-title": "Blood",
"key": "B78",
"volume": "136",
"year": "2020"
},
{
"DOI": "10.1186/s12985-023-02116-w",
"article-title": "Neutrophils in COVID-19: recent insights and advances",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "169",
"journal-title": "Virol J",
"key": "B79",
"volume": "20",
"year": "2023"
},
{
"DOI": "10.1007/s00277-023-05234-1",
"article-title": "Status of major hemostatic components in the setting of COVID-19: the effect on endothelium, platelets, coagulation factors, fibrinolytic system, and complement",
"author": "Sayyadi",
"doi-asserted-by": "publisher",
"journal-title": "Ann Hematol",
"key": "B80",
"volume": "102",
"year": "2023"
},
{
"DOI": "10.1161/CIRCRESAHA.122.321930",
"article-title": "Platelets and SARS-coV-2 during COVID-19: immunity, thrombosis, and beyond",
"author": "Sciaudone",
"doi-asserted-by": "publisher",
"journal-title": "Circ Res",
"key": "B81",
"volume": "132",
"year": "2023"
},
{
"DOI": "10.48101/ujms.v129.9863",
"article-title": "COVID-19: Not a thrombotic disease but a thromboinflammatory disease",
"author": "He",
"doi-asserted-by": "publisher",
"journal-title": "Ups J Med Sci",
"key": "B82",
"volume": "129",
"year": "2024"
},
{
"DOI": "10.1161/ATVBAHA.120.315175",
"article-title": "Platelets promote thromboinflammation in SARS-coV-2 pneumonia",
"author": "Taus",
"doi-asserted-by": "publisher",
"journal-title": "Arterioscler Thromb Vasc Biol",
"key": "B83",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.1111/bjh.19159",
"article-title": "Post-COVID-19 thrombotic sequelae: The potential role of persistent platelet hyperactivity",
"author": "Schieppati",
"doi-asserted-by": "publisher",
"journal-title": "Br J Haematol",
"key": "B84",
"volume": "204",
"year": "2024"
},
{
"DOI": "10.1111/bjh.19125",
"article-title": "Prolonged platelet hyperactivity after COVID-19 infection",
"author": "Nara",
"doi-asserted-by": "publisher",
"journal-title": "Br J Haematol",
"key": "B85",
"volume": "204",
"year": "2024"
},
{
"DOI": "10.3390/ijms222011170",
"article-title": "Inflammatory mediators of platelet activation: focus on atherosclerosis and COVID-19",
"author": "Theofilis",
"doi-asserted-by": "publisher",
"first-page": "11170",
"journal-title": "International Journal of Molecular Sciences",
"key": "B86",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1371/journal.pbio.3001109",
"article-title": "COVID-19 induces a hyperactive phenotype in circulating platelets",
"author": "Comer",
"doi-asserted-by": "publisher",
"journal-title": "PloS Biol",
"key": "B87",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1111/jth.14005",
"article-title": "PDK1 governs thromboxane generation and thrombosis in platelets by regulating activation of Raf1 in the MAPK pathway",
"author": "Manne",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Haemost",
"key": "B88",
"volume": "16",
"year": "2018"
},
{
"DOI": "10.1111/jth.15275",
"article-title": "Antibody-mediated platelet activation in COVID-19: A coincidence or a new mechanism of the dysregulated coagulation system",
"author": "Althaus",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Haemost",
"key": "B89",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2022.807934",
"article-title": "The COVID complex: A review of platelet activation and immune complexes in COVID-19",
"author": "Jevtic",
"doi-asserted-by": "publisher",
"journal-title": "Front Immunol",
"key": "B90",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/j.biopha.2025.118100",
"article-title": "SARS-CoV-2 S1 protein induces IgG-mediated platelet activation and is prevented by 1.8-cineole",
"author": "Petry",
"doi-asserted-by": "publisher",
"first-page": "118100",
"journal-title": "BioMed Pharmacother",
"key": "B91",
"volume": "187",
"year": "2025"
},
{
"DOI": "10.1080/09537104.2021.1912315",
"article-title": "A double-edged sword: antibody-mediated procoagulant platelets in COVID-19",
"author": "Millington-Burgess",
"doi-asserted-by": "publisher",
"journal-title": "Platelets",
"key": "B92",
"volume": "32",
"year": "2021"
},
{
"DOI": "10.1182/blood.2020008762",
"article-title": "Antibody-induced procoagulant platelets in severe COVID-19 infection",
"author": "Althaus",
"doi-asserted-by": "publisher",
"journal-title": "Blood",
"key": "B93",
"volume": "137",
"year": "2021"
},
{
"DOI": "10.1111/jth.15587",
"article-title": "Antibody-mediated procoagulant platelet formation in COVID-19 is AKT dependent",
"author": "Pelzl",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Haemost",
"key": "B94",
"volume": "20",
"year": "2022"
},
{
"DOI": "10.1007/s11239-021-02544-x",
"article-title": "COVID-19 and biomarkers of thrombosis: focus on von Willebrand factor and extracellular vesicles",
"author": "Becker",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Thrombolysis",
"key": "B95",
"volume": "52",
"year": "2021"
},
{
"DOI": "10.3390/ijms24031920",
"article-title": "Extracellular vesicles: new players in the mechanisms of sepsis- and COVID-19-related thromboinflammation",
"author": "Schiavello",
"doi-asserted-by": "publisher",
"journal-title": "Int J Mol Sci",
"key": "B96",
"volume": "24",
"year": "2023"
},
{
"DOI": "10.1128/msphere.00764-24",
"article-title": "Circulating extracellular vesicles from severe COVID-19 patients induce lung inflammation",
"author": "Qian",
"doi-asserted-by": "publisher",
"journal-title": "mSphere",
"key": "B97",
"volume": "9",
"year": "2024"
},
{
"DOI": "10.1161/ATVBAHA.120.315547",
"article-title": "Patients with COVID-19 have elevated levels of circulating extracellular vesicle tissue factor activity that is associated with severity and mortality—Brief report",
"author": "Rosell",
"doi-asserted-by": "publisher",
"journal-title": "Arteriosclerosis Thrombosis Vasc Biol",
"key": "B98",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.1182/bloodadvances.2020003308",
"article-title": "Dissemination of extreme levels of extracellular vesicles: tissue factor activity in patients with severe COVID-19",
"author": "Guervilly",
"doi-asserted-by": "publisher",
"journal-title": "Blood Adv",
"key": "B99",
"volume": "5",
"year": "2021"
},
{
"DOI": "10.1038/s41598-017-03262-2",
"article-title": "Different potential of extracellular vesicles to support thrombin generation: contributions of phosphatidylserine, tissue factor, and cellular origin",
"author": "Tripisciano",
"doi-asserted-by": "publisher",
"first-page": "6522",
"journal-title": "Sci Rep",
"key": "B100",
"volume": "7",
"year": "2017"
},
{
"DOI": "10.1038/s41598-024-56841-5",
"article-title": "The fluorochrome-to-protein ratio is crucial for the flow cytometric detection of tissue factor on extracellular vesicles",
"author": "Weiss",
"doi-asserted-by": "publisher",
"first-page": "6419",
"journal-title": "Sci Rep",
"key": "B101",
"volume": "14",
"year": "2024"
},
{
"DOI": "10.3390/cells10010085",
"article-title": "Circulating platelet-derived extracellular vesicles are a hallmark of sars-cov-2 infection",
"author": "Cappellano",
"doi-asserted-by": "publisher",
"first-page": "85",
"journal-title": "Circulation",
"key": "B102",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1186/s13054-020-03060-9",
"article-title": "War to the knife” against thromboinflammation to protect endothelial function of COVID-19 patients",
"author": "Guglielmetti",
"doi-asserted-by": "publisher",
"first-page": "365",
"journal-title": "Crit Care",
"key": "B103",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1016/j.jtha.2024.02.013",
"article-title": "Four years into the pandemic, managing COVID-19 patients with acute coagulopathy: what have we learned",
"author": "Iba",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Haemost",
"key": "B104",
"volume": "22",
"year": "2024"
},
{
"DOI": "10.1542/peds.2022-056726",
"article-title": "Enoxaparin thromboprophylaxis in children hospitalized for COVID-19: A phase 2 trial",
"author": "Sochet",
"doi-asserted-by": "publisher",
"journal-title": "Pediatrics",
"key": "B105",
"volume": "150",
"year": "2022"
},
{
"DOI": "10.1161/ATVBAHA.122.318748",
"article-title": "Novel tissue factor inhibition for thromboprophylaxis in COVID-19: primary results of the ASPEN-COVID-19 trial",
"author": "Hess",
"doi-asserted-by": "publisher",
"journal-title": "Arterioscler Thromb Vasc Biol",
"key": "B106",
"volume": "43",
"year": "2023"
},
{
"DOI": "10.1016/j.jacc.2023.02.041",
"article-title": "Randomized trial of anticoagulation strategies for noncritically ill patients hospitalized with COVID-19",
"author": "Stone",
"doi-asserted-by": "publisher",
"journal-title": "J Am Coll Cardiol",
"key": "B107",
"volume": "81",
"year": "2023"
},
{
"DOI": "10.1016/S0140-6736(21)01203-4",
"article-title": "Therapeutic versus prophylactic anticoagulation for patients admitted to hospital with COVID-19 and elevated D-dimer concentration (ACTION): an open-label, multicentre, randomised, controlled trial",
"author": "Lopes",
"doi-asserted-by": "publisher",
"journal-title": "Lancet",
"key": "B108",
"volume": "397",
"year": "2021"
},
{
"DOI": "10.1136/bmj.n2400",
"article-title": "Effectiveness of therapeutic heparin versus prophylactic heparin on death, mechanical ventilation, or intensive care unit admission in moderately ill patients with covid-19 admitted to hospital: RAPID randomised clinical trial",
"author": "Sholzberg",
"doi-asserted-by": "publisher",
"first-page": "n2400",
"journal-title": "Bmj",
"key": "B109",
"volume": "375",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2105911",
"article-title": "Therapeutic anticoagulation with heparin in noncritically ill patients with covid-19",
"author": "Investigators",
"doi-asserted-by": "publisher",
"first-page": "790",
"journal-title": "N Engl J Med",
"key": "B110",
"volume": "385",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2103417",
"article-title": "Therapeutic anticoagulation with heparin in critically ill patients with covid-19",
"author": "Investigators",
"doi-asserted-by": "publisher",
"journal-title": "N Engl J Med",
"key": "B111",
"volume": "385",
"year": "2021"
},
{
"DOI": "10.1161/CIRCULATIONAHA.122.061533",
"article-title": "Anticoagulation and antiplatelet therapy for prevention of venous and arterial thrombotic events in critically ill patients with COVID-19: COVID-PACT",
"author": "Bohula",
"doi-asserted-by": "publisher",
"journal-title": "Circulation",
"key": "B112",
"volume": "146",
"year": "2022"
},
{
"DOI": "10.1001/jamainternmed.2021.6203",
"article-title": "Efficacy and safety of therapeutic-dose heparin vs standard prophylactic or intermediate-dose heparins for thromboprophylaxis in high-risk hospitalized patients with COVID-19: the HEP-COVID randomized clinical trial",
"author": "Spyropoulos",
"doi-asserted-by": "publisher",
"journal-title": "JAMA Intern Med",
"key": "B113",
"volume": "181",
"year": "2021"
},
{
"DOI": "10.1016/j.thromres.2020.09.026",
"article-title": "Therapeutic versus prophylactic anticoagulation for severe COVID-19: A randomized phase II clinical trial (HESACOVID)",
"author": "Lemos",
"doi-asserted-by": "publisher",
"journal-title": "Thromb Res",
"key": "B114",
"volume": "196",
"year": "2020"
},
{
"DOI": "10.1111/jth.15450",
"article-title": "Standard prophylactic versus intermediate dose enoxaparin in adults with severe COVID-19: A multi-center, open-label, randomized controlled trial",
"author": "Perepu",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Haemost",
"key": "B115",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1055/a-1485-2372",
"article-title": "Intermediate-dose versus standard-dose prophylactic anticoagulation in patients with COVID-19 admitted to the intensive care unit: 90-day results from the INSPIRATION randomized trial",
"author": "Bikdeli",
"doi-asserted-by": "publisher",
"journal-title": "Thromb Haemost",
"key": "B116",
"volume": "122",
"year": "2022"
},
{
"DOI": "10.1016/j.thromres.2022.10.021",
"article-title": "Enoxaparin for outpatients with COVID-19: 90-day results from the randomised, open-label, parallel-group, multinational, phase III OVID trial",
"author": "Voci",
"doi-asserted-by": "publisher",
"journal-title": "Thromb Res",
"key": "B117",
"volume": "221",
"year": "2023"
},
{
"DOI": "10.1016/S2352-3026(22)00175-2",
"article-title": "Enoxaparin for primary thromboprophylaxis in symptomatic outpatients with COVID-19 (OVID): a randomised, open-label, parallel-group, multicentre, phase 3 trial",
"author": "Barco",
"doi-asserted-by": "publisher",
"journal-title": "Lancet Haematol",
"key": "B118",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1016/j.thromres.2022.11.019",
"article-title": "Effectiveness and safety of extended thromboprophylaxis in post-discharge patients with COVID-19: A systematic review and meta-analysis",
"author": "Dai",
"doi-asserted-by": "publisher",
"journal-title": "Thromb Res",
"key": "B119",
"volume": "221",
"year": "2023"
},
{
"DOI": "10.4266/acc.2022.01424",
"article-title": "Comparison of safety and efficacy between therapeutic or intermediate versus prophylactic anticoagulation for thrombosis in COVID-19 patients: a systematic review and meta-analysis",
"author": "Lee",
"doi-asserted-by": "publisher",
"journal-title": "Acute Crit Care",
"key": "B120",
"volume": "38",
"year": "2023"
},
{
"DOI": "10.1007/s11739-022-03159-7",
"article-title": "Efficacy and safety of two heparin regimens for prevention of venous thromboembolism in hospitalized patients with COVID-19: a meta-analysis",
"author": "Vedovati",
"doi-asserted-by": "publisher",
"journal-title": "Intern Emerg Med",
"key": "B121",
"volume": "18",
"year": "2023"
},
{
"DOI": "10.1007/s11239-022-02643-3",
"article-title": "Thromboembolic prevention and anticoagulant therapy during the COVID-19 pandemic: updated clinical guidance from the anticoagulation forum",
"author": "Barnes",
"doi-asserted-by": "publisher",
"first-page": "197",
"journal-title": "J Thromb Thrombolysis",
"key": "B122",
"volume": "54",
"year": "2022"
},
{
"DOI": "10.1016/j.jtha.2024.02.011",
"article-title": "2023 ISTH update of the 2022 ISTH guidelines for antithrombotic treatment in COVID-19",
"author": "Schulman",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Haemost",
"key": "B123",
"volume": "22",
"year": "2024"
},
{
"DOI": "10.3760/cma.j.cn112137-20210112-00090",
"article-title": "Guidelines for diagnosis, prevention and treatment of COVID-19 in adults in China",
"doi-asserted-by": "publisher",
"journal-title": "Chin Med J",
"key": "B124",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1182/bloodadvances.2020003763",
"article-title": "American Society of Hematology 2021 guidelines on the use of anticoagulation for thromboprophylaxis in patients with COVID-19",
"author": "Cuker",
"doi-asserted-by": "publisher",
"journal-title": "Blood Adv",
"key": "B125",
"volume": "5",
"year": "2021"
},
{
"key": "B126",
"volume-title": "Final coronavirus disease (COVID-19) treatment guidelines",
"year": "2024"
},
{
"DOI": "10.1016/j.chest.2022.02.006",
"article-title": "Thromboprophylaxis in patients with COVID-19: A brief update to the CHEST guideline and expert panel report",
"author": "Moores",
"doi-asserted-by": "publisher",
"journal-title": "Chest",
"key": "B127",
"volume": "162",
"year": "2022"
},
{
"DOI": "10.1016/j.chest.2020.05.559",
"article-title": "Prevention, diagnosis, and treatment of VTE in patients with coronavirus disease 2019: CHEST guideline and expert panel report",
"author": "Moores",
"doi-asserted-by": "publisher",
"journal-title": "Chest",
"key": "B128",
"volume": "158",
"year": "2020"
},
{
"DOI": "10.3760/cma.j.cn112137-2023-01-20-00115",
"article-title": "Practice guidelines of thromboprophylaxis and management of anticoagulation in hospitalized patients with COVID-19",
"doi-asserted-by": "publisher",
"journal-title": "Chin Med J",
"key": "B129",
"volume": "103",
"year": "2023"
},
{
"DOI": "10.1016/S0140-6736(22)01214-4",
"article-title": "Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study",
"author": "Ballering",
"doi-asserted-by": "publisher",
"journal-title": "Lancet",
"key": "B130",
"volume": "400",
"year": "2022"
},
{
"DOI": "10.1016/S0140-6736(24)01136-X",
"article-title": "Long COVID: a clinical update",
"author": "Greenhalgh",
"doi-asserted-by": "publisher",
"journal-title": "Lancet",
"key": "B131",
"volume": "404",
"year": "2024"
},
{
"DOI": "10.1038/s41591-022-01689-3",
"article-title": "Long-term cardiovascular outcomes of COVID-19",
"author": "Xie",
"doi-asserted-by": "publisher",
"journal-title": "Nat Med",
"key": "B132",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1016/S1473-3099(21)00703-9",
"article-title": "A clinical case definition of post-COVID-19 condition by a Delphi consensus",
"author": "Soriano",
"doi-asserted-by": "publisher",
"journal-title": "Lancet Infect Dis",
"key": "B133",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1093/cvr/cvaa106",
"article-title": "COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options",
"author": "Guzik",
"doi-asserted-by": "publisher",
"journal-title": "Cardiovasc Res",
"key": "B134",
"volume": "116",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2022.838011",
"article-title": "NETosis and neutrophil extracellular traps in COVID-19: immunothrombosis and beyond",
"author": "Zhu",
"doi-asserted-by": "publisher",
"journal-title": "Front Immunol",
"key": "B135",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.3390/ijms26104562",
"article-title": "Persistent monocytic bioenergetic impairment and mitochondrial DNA damage in PASC patients with cardiovascular complications",
"author": "Semo",
"doi-asserted-by": "publisher",
"journal-title": "Int J Mol Sci",
"key": "B136",
"volume": "26",
"year": "2025"
},
{
"DOI": "10.1016/j.immuni.2015.02.002",
"article-title": "Mitochondria in the regulation of innate and adaptive immunity",
"author": "Weinberg",
"doi-asserted-by": "publisher",
"journal-title": "Immunity",
"key": "B137",
"volume": "42",
"year": "2015"
},
{
"DOI": "10.1152/ajpcell.00426.2020",
"article-title": "Mitochondrial metabolic manipulation by SARS-CoV-2 in peripheral blood mononuclear cells of patients with COVID-19",
"author": "Ajaz",
"doi-asserted-by": "publisher",
"journal-title": "American Journal of Physiology-cell Physiology",
"key": "B138",
"volume": "320",
"year": "2021"
},
{
"DOI": "10.1016/j.biocel.2014.05.019",
"article-title": "Mitochondria in monocytes and macrophages-implications for translational and basic research",
"author": "Ravi",
"doi-asserted-by": "publisher",
"journal-title": "Int J Biochem Cell Biol",
"key": "B139",
"volume": "53",
"year": "2014"
},
{
"DOI": "10.1016/j.arcmed.2020.04.019",
"article-title": "Oxidative stress as key player in severe acute respiratory syndrome coronavirus (SARS-coV) infection",
"author": "Delgado-Roche",
"doi-asserted-by": "publisher",
"journal-title": "Arch Med Res",
"key": "B140",
"volume": "51",
"year": "2020"
},
{
"DOI": "10.3390/antiox9100936",
"article-title": "Oxidative stress and inflammation in COVID-19-associated sepsis: the potential role of anti-oxidant therapy in avoiding disease progression",
"author": "Beltrán-García",
"doi-asserted-by": "publisher",
"first-page": "936",
"journal-title": "Antioxidants",
"key": "B141",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.3390/idr17010015",
"article-title": "Genetics of long COVID: exploring the molecular drivers of persistent pulmonary vascular disease symptoms",
"author": "Ayyoub",
"doi-asserted-by": "publisher",
"first-page": "15",
"journal-title": "Infect Dis Rep",
"key": "B142",
"volume": "17",
"year": "2025"
},
{
"DOI": "10.1371/journal.pone.0296668",
"article-title": "Thrombophilia genetic mutations and their relation to disease severity among patients with COVID-19",
"author": "Moness",
"doi-asserted-by": "publisher",
"journal-title": "PloS One",
"key": "B143",
"volume": "19",
"year": "2024"
},
{
"DOI": "10.1111/j.1365-2141.2010.08529.x",
"article-title": "Risk of cardiovascular disease in double heterozygous carriers and homozygous carriers of F5 R506Q (factor V Leiden) and F2 (prothrombin) G20210A: a retrospective family cohort study",
"author": "Roach",
"doi-asserted-by": "publisher",
"journal-title": "British Journal of Haematology",
"key": "B144",
"volume": "153",
"year": "2011"
},
{
"DOI": "10.3947/ic.2022.0141",
"article-title": "Preliminary guidelines for the clinical evaluation and management of long COVID",
"author": "Kim",
"doi-asserted-by": "publisher",
"journal-title": "Infect Chemother",
"key": "B145",
"volume": "54",
"year": "2022"
},
{
"DOI": "10.3947/ic.2024.0024",
"article-title": "Updated clinical practice guidelines for the diagnosis and management of long COVID",
"author": "Seo",
"doi-asserted-by": "publisher",
"journal-title": "Infect Chemother",
"key": "B146",
"volume": "56",
"year": "2024"
},
{
"DOI": "10.1001/jamanetworkopen.2022.8526",
"article-title": "COVID-19 vaccination and estimated public health impact in california",
"author": "Tan",
"doi-asserted-by": "publisher",
"journal-title": "JAMA Netw Open",
"key": "B147",
"volume": "5",
"year": "2022"
},
{
"DOI": "10.15585/mmwr.mm7018e1",
"article-title": "Effectiveness of pfizer-bioNTech and moderna vaccines against COVID-19 among hospitalized adults aged ≥65 years - United States, january-march 2021",
"author": "Tenforde",
"doi-asserted-by": "publisher",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "B148",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.1055/s-0041-1727284",
"article-title": "Venous thromboembolism in patients discharged after COVID-19 hospitalization",
"author": "Engelen",
"doi-asserted-by": "publisher",
"journal-title": "Semin Thromb Hemost",
"key": "B149",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.1016/j.thromres.2020.04.013",
"article-title": "Incidence of thrombotic complications in critically ill ICU patients with COVID-19",
"author": "Klok",
"doi-asserted-by": "publisher",
"journal-title": "Thromb Res",
"key": "B150",
"volume": "191",
"year": "2020"
},
{
"DOI": "10.1186/s13063-021-05076-0",
"article-title": "Coagulopathy of hospitalised COVID-19: A Pragmatic Randomised Controlled Trial of Therapeutic Anticoagulation versus Standard Care as a Rapid Response to the COVID-19 Pandemic (RAPID COVID COAG - RAPID Trial): A structured summary of a study protocol for a randomised controlled trial",
"author": "Sholzberg",
"doi-asserted-by": "publisher",
"first-page": "202",
"journal-title": "Trials",
"key": "B151",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1111/jth.15725",
"article-title": "Risk of venous thromboembolism after COVID-19 vaccination",
"author": "Houghton",
"doi-asserted-by": "publisher",
"journal-title": "Journal of Thrombosis And Haemostasis",
"key": "B152",
"volume": "20",
"year": "2022"
},
{
"DOI": "10.1111/jth.15751",
"article-title": "Refractory immune TTP following Pfizer-BioNTech COVID-19 vaccine successfully salvaged with caplacizumab",
"author": "Laverdure",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Haemost",
"key": "B153",
"volume": "20",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa2104882",
"article-title": "Thrombosis and Thrombocytopenia after ChAdOx1 nCoV-19 Vaccination",
"author": "Schultz",
"doi-asserted-by": "publisher",
"journal-title": "New England Journal of Medicine",
"key": "B154",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2104840",
"article-title": "Thrombotic Thrombocytopenia after ChAdOx1 nCov-19 Vaccination",
"author": "Greinacher",
"doi-asserted-by": "publisher",
"journal-title": "N Engl J Med",
"key": "B155",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1056/NEJMe2106315",
"article-title": "SARS-coV-2 vaccine-induced immune thrombotic thrombocytopenia",
"author": "Cines",
"doi-asserted-by": "publisher",
"journal-title": "N Engl J Med",
"key": "B156",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2105385",
"article-title": "Pathologic Antibodies to Platelet Factor 4 after ChAdOx1 nCoV-19 Vaccination",
"author": "Scully",
"doi-asserted-by": "publisher",
"journal-title": "N Engl J Med",
"key": "B157",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(21)02392-8",
"article-title": "Rivaroxaban versus no anticoagulation for post-discharge thromboprophylaxis after hospitalisation for COVID-19 (MICHELLE): an open-label, multicentre, randomised, controlled trial",
"author": "Ramacciotti",
"doi-asserted-by": "publisher",
"journal-title": "Lancet",
"key": "B158",
"volume": "399",
"year": "2022"
},
{
"DOI": "10.1080/20523211.2024.2375269",
"article-title": "Direct oral anticoagulants versus low-molecular-weight heparin in patients with cancer-associated venous thrombosis: a cost-effectiveness analysis",
"author": "Kang",
"doi-asserted-by": "publisher",
"first-page": "2375269",
"journal-title": "J Pharm Policy Pract",
"key": "B159",
"volume": "17",
"year": "2024"
},
{
"DOI": "10.1056/NEJMoa2109908",
"article-title": "Clinical features of vaccine-induced immune thrombocytopenia and thrombosis",
"author": "Pavord",
"doi-asserted-by": "publisher",
"journal-title": "N Engl J Med",
"key": "B160",
"volume": "385",
"year": "2021"
},
{
"DOI": "10.7861/clinmed.2021-0488",
"article-title": "VITT, COVID-19 and the Expert Haematology Panel: The story of how the UK responded to emerging cases of vaccine-induced immune thrombocytopenia and thrombosis during the vaccination programme",
"author": "Chevassut",
"doi-asserted-by": "publisher",
"journal-title": "Clin Med (Lond)",
"key": "B161",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1016/j.rmcr.2019.100884",
"article-title": "Acute thrombotic vascular events complicating influenza-associated pneumonia",
"author": "Ishiguro",
"doi-asserted-by": "publisher",
"first-page": "100884",
"journal-title": "Respir Med Case Rep",
"key": "B162",
"volume": "28",
"year": "2019"
},
{
"DOI": "10.3390/v14122817",
"article-title": "Thromboembolic events in patients with influenza: A scoping review",
"author": "Rubino",
"doi-asserted-by": "publisher",
"journal-title": "Viruses",
"key": "B163",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1136/bmj.326.7403.1358",
"article-title": "Haematological manifestations in patients with severe acute respiratory syndrome: retrospective analysis",
"author": "Wong",
"doi-asserted-by": "publisher",
"journal-title": "Bmj-british Medical Journal",
"key": "B164",
"volume": "326",
"year": "2003"
},
{
"DOI": "10.1016/j.ahj.2020.10.075",
"article-title": "Thrombosis in hospitalized patients with viral respiratory infections versus COVID-19",
"author": "Smilowitz",
"doi-asserted-by": "publisher",
"journal-title": "Am Heart J",
"key": "B165",
"volume": "231",
"year": "2021"
},
{
"DOI": "10.1089/jir.2022.0029",
"article-title": "Comparing the cytokine storms of COVID-19 and pandemic influenza",
"author": "Pacheco-Hernández",
"doi-asserted-by": "publisher",
"journal-title": "J Interferon Cytokine Res",
"key": "B166",
"volume": "42",
"year": "2022"
},
{
"DOI": "10.1111/jth.15509",
"article-title": "Tissue factor expression, extracellular vesicles, and thrombosis after infection with the respiratory viruses influenza A virus and coronavirus",
"author": "Mackman",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Haemost",
"key": "B167",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1152/ajplung.00199.2020",
"article-title": "Heparin as a therapy for COVID-19: current evidence and future possibilities",
"author": "Hippensteel",
"doi-asserted-by": "publisher",
"journal-title": "American Journal of Physiology-lung Cellular And Molecular Physiology",
"key": "B168",
"volume": "319",
"year": "2020"
},
{
"DOI": "10.1093/eurheartj/ehac544.2715",
"article-title": "Aspirin therapy on prophylactic anticoagulation for patients hospitalized with COVID-19: A propensity score-matched cohort analysis of the HOPE-COVID-19 registry",
"author": "Santoro",
"doi-asserted-by": "publisher",
"journal-title": "Journal of the American Heart Association",
"key": "B169",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1111/ejh.13638",
"article-title": "White blood count, D-dimers, and ferritin levels as predictive factors of pulmonary embolism suspected upon admission in noncritically ill COVID-19 patients: The French multicenter CLOTVID retrospective study",
"author": "Galland",
"doi-asserted-by": "publisher",
"first-page": "190",
"journal-title": "Eur J Haematol",
"key": "B170",
"volume": "107",
"year": "2021"
},
{
"DOI": "10.1042/BCJ20220016",
"article-title": "A central role for amyloid fibrin microclots in long COVID/PASC: origins and therapeutic implications",
"author": "Kell",
"doi-asserted-by": "publisher",
"journal-title": "Biochem J",
"key": "B171",
"volume": "479",
"year": "2022"
},
{
"DOI": "10.1038/s41586-024-07873-4",
"article-title": "Fibrin drives thromboinflammation and neuropathology in COVID-19",
"author": "Ryu",
"doi-asserted-by": "publisher",
"journal-title": "Nature",
"key": "B172",
"volume": "633",
"year": "2024"
}
],
"reference-count": 172,
"references-count": 172,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fimmu.2025.1593885/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "COVID-19: a vascular nightmare unfolding",
"type": "journal-article",
"update-policy": "https://doi.org/10.3389/crossmark-policy",
"volume": "16"
}