Does Serum Vitamin D Level Affect COVID-19 Infection and Its Severity? A Case-Control Study
et al., Journal of the American College of Nutrition, doi:10.1080/07315724.2020.182600, Oct 2020
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Case control study in China comparing 62 patients with 80 healthy controls showing vitamin D deficiency is a risk factor for COVID-19, especially for severe/critical cases.
This is the 20th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments1.
|
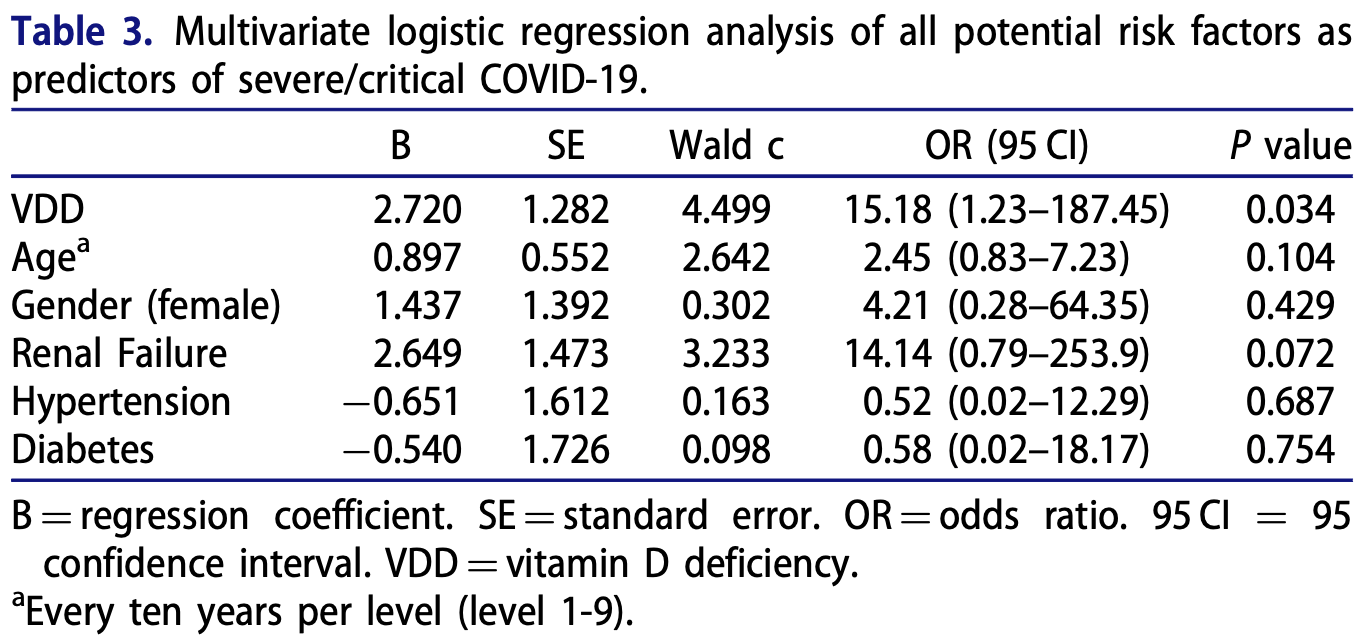
risk of severe/critical COVID-19, 93.4% lower, RR 0.07, p = 0.03, high D levels 2 of 36 (5.6%), low D levels 8 of 26 (30.8%), NNT 4.0, adjusted per study, inverted to make RR<1 favor high D levels, >50nmol/L.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ye et al., 13 Oct 2020, retrospective, China, peer-reviewed, 18 authors.
Does Serum Vitamin D Level Affect COVID-19 Infection and Its Severity?-A Case-Control Study
Journal of the American College of Nutrition, doi:10.1080/07315724.2020.1826005
Background: As effective medication to treat COVID-19 is currently unavailable, preventive remedies may be particularly important. Objective: To examine the relationship between serum 25-hydroxy vitamin D (25(OH)D) level and COVID-19 infection, its severity, and its clinical case characteristics. Methods: This case-control study compared serum 25(OH)D levels and rates of vitamin D deficiency (VDD) between 80 healthy controls and 62 patients diagnosed with COVID-19 and admitted to Guangxi People's Hospital, China, 2/16/2020-3/16/2020. Cases were categorized into asymptomatic, mild/moderate, and severe/critical disease. Logistic regression analysis was conducted to examine the associations between 25(OH)D level, or VDD, and case status/severity of COVID-19 while controlling for demographics and comorbidities. A threshold level of vitamin D for conveying COVID-19 risk was estimated. Results: Severe/critical COVID-19 cases were significantly older and had higher percentages of comorbidity (renal failure) compared to mild cases. The serum 25(OH)D concentration in COVID-19 patient was much lower than that in healthy control. And 25(OH)D level was the lowest in severe/ critical cases, compared with mild cases. In further, significantly higher rates of VDD were found in COVID-19 cases (41.9%) compared to healthy controls (11.1%). And VDD was the greatest in severe/critical cases (80%), compared with mild cases (36%). These statistically significant associations remained even after controlling for demographics and comorbidities. A potential threshold of 25(OH)D (41.19 nmol/L) to protect against COVID-19 was identified. Conclusion: Elderly and people with comorbidities were susceptible to severe COVID-19 infection. VDD was a risk factor for COVID-19, especially for severe/critical cases. While further confirmation is needed, vitamin D supplementation may have prevention or treatment potential for COVID-19 disease.
Authors' contributions K. Ye, S. Lin, F. Xu. Designed research; F.Tang, X.Liao, G. Huang, C. Chen, N. Tang conducted research; H. Xiao, X. Liao performed statistical analysis; F. Tang, X. Liao, M. Deng wrote the paper; Z. Qin, X. Peng, X. Liu, L. Ning, B. Wang, M. Li, J. Yang provided essential technical and material support; F. Xu, S. Lin, J. Yang, K. Ye had primary responsibility for final content. All authors read and approved the final manuscript.
Disclosure statement All authors have no conflict of interest.
ORCID Bangqin Wang http://orcid.org/0000-0002-1592-7074
References
Alquaiz, Kazi, Fouda, Alyousefi, Age and gender differences in the prevalence and correlates of vitamin D deficiency, Arch Osteoporos, doi:10.1007/s11657-018-0461-5
Chen, Zhou, Dong, Qu, Gong et al., Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study, Lancet
Contreras-Manzano, Villalpando, Garcia-Diaz, Flores-Aldana, Cardiovascular risk factors and their association with Vitamin D deficiency in Mexican women of reproductive age, Nutrients, doi:10.3390/nu11061211
D'antiga, Coronaviruses and immunosuppressed patients. The facts during the third epidemic, Liver Transplant, doi:10.1002/LT.25756
D'avolio, Avataneo, Manca, Cusato, Nicol O et al., 25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients, doi:10.3390/nu12051359
Esposito, Lelii, Vitamin D and respiratory tract infections in childhood, BMC Infect Dis, doi:10.1186/s12879-015-1196-1
Gallagher, Sai, Templin, Smith, Dose response to vitamin D supplementation in postmenopausal women: a randomized trial, Ann Intern Med, doi:10.7326/0003-4819-156-6-201203200-00005
Grasselli, Zangrillo, Zanella, Antonelli, Cabrini et al., Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy, Jama, doi:10.1001/jama.2020.5394
Gruber-Bzura, Vitamin D and influenza-prevention or therapy?, Int J Mol Sci
Guan, Ni, Hu, Liang, Ou et al., Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med, doi:10.1056/NEJMoa2002032?articleTools=true
Hastie, Mackay, Ho, Celis-Morales, Katikireddi et al., Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metabolic Syndrome, doi:10.1016/j.dsx.2020.04.050
Haugen, Chandyo, Ulak, Mathisen, Basnet et al., 25-Hydroxy-Vitamin D concentration is not affected by severe or non-severe pneumonia, or inflammation, in young children, Nutrients, doi:10.3390/nu9010052
Holick, Binkley, Bischoff-Ferrari, Gordon, Hanley et al., Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline, J Clin Endocrinol Metab, doi:10.1210/jc.2011-0385
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin Exp Res, doi:10.1007/s40520-020-01570-8
Laaksi, Ruohola, Mattila, Auvinen, Ylikomi et al., Vitamin D supplementation for the prevention of acute respiratory tract infection: a randomized, double-blinded trial among young Finnish men, J Infect Dis, doi:10.1086/654881
Laird, Rhodes, Kenny, Vitamin D and inflammation: Potential implications for severity of Covid-19, Ir Med J
Levey, Stevens, Schmid, Zhang, Castro et al., A new equation to estimate glomerular filtration rate, Ann Intern Med, doi:10.7326/0003-4819-150-9-200905050-00006
Liu, Stenger, Li, Wenzel, Tan et al., Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response, Science, doi:10.1126/science.1123933
Mamani, Muceli, Basir, Vasheghani, Poorolajal, Association between serum concentration of 25-hydroxyvitamin D and community-acquired pneumonia: a casecontrol study, IJGM, doi:10.2147/IJGM.S149049
Mangin, Sinha, Fincher, Inflammation and vitamin D: the infection connection, Inflamm Res, doi:10.1007/s00011-014-0755-z
Mathyssen, Gayan-Ramirez, Bouillon, Janssens, Vitamin D supplementation in respiratory diseases: evidence from randomized controlled trials, Pol Arch Intern Med, doi:10.20452/pamw.4134
Mcnally, Leis, Matheson, Karuananyake, Sankaran et al., Vitamin D deficiency in young children with severe acute lower respiratory infection, Pediatr Pulmonol, doi:10.1002/ppul.21089
Merzon, Tworowski, Gorohovski, Vinker, Cohen et al., Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study, FEBS J
Munshi, Hussein, Toraih, Elshazli, Jardak et al., Vitamin D insufficiency as a potential culprit in critical COVID-19 patients, J Med Virol
Nhco, The guidelines for the diagnosis and treatment of COVID-19
Panagiotou, Tee, Ihsan, Athar, Marchitelli et al., Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalised with COVID-19 are associated with greater disease severity, Clin Endocrinol, doi:10.1111/cen.14276
Talebi, Nejad, Yaseri, Hadadi, Association of vitamin D status with the severity and mortality of communityacquired pneumonia in Iran during 2016-2017: A Prospective Cohort Study, Rep Biochem Mol Biol
Vo, Koppel, Espinola, Mansbach, Celedon et al., Vitamin D status at the time of hospitalization for bronchiolitis and its association with disease severity, J Pediatr, doi:10.1016/j.jpeds.2018.07.097
Wang, Hu, Hu, Zhu, Liu et al., Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China, Jama, doi:10.1001/jama.2020.1585
Weiss, Murdoch, Clinical course and mortality risk of severe COVID-19, Lancet, doi:10.1016/S0140-6736(20)30633-4
Wu, Liao, Xia, Li, Li et al., Vitamin D receptor negatively regulates bacterial-stimulated NF-kappaB activity in intestine, Am J Pathol, doi:10.2353/ajpath.2010.090998
Wu, Mcgoogan, Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention, Jama, doi:10.1001/jama.2020.2648
Zheng, Gao, Wang, Song, Liu et al., Functional exhaustion of antiviral lymphocytes in COVID-19 patients, Cell Mol Immunol, doi:10.1038/s41423-020-0402-2
Zhu, Chen, Li, Yang, Liu et al., Associations of vitamin D with novel and traditional anthropometric indices according to age and sex: a cross-sectional study in central southern China, Eat Weight Disord
Zhu, Zhang, Li, Yang, Song et al., A novel coronavirus from patients with pneumonia in China, 2019, N Engl J Med, doi:10.1056/NEJMoa2001017
