Improving Nutritional Status Was Associated with Decreasing Disease Severity and Shortening of Negative Conversion Time of PCR Test in Non-ICU Patients with COVID-19
et al., Infection and Drug Resistance, doi:10.2147/idr.s409615, Jul 2023
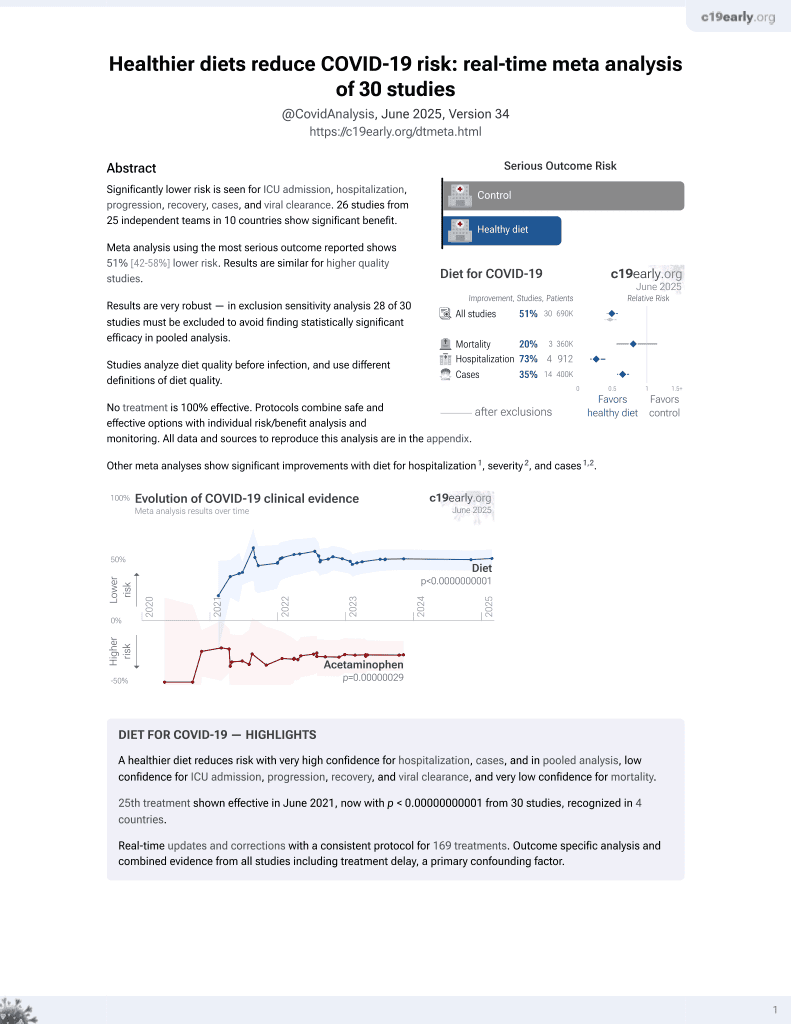
Diet for COVID-19
26th treatment shown to reduce risk in
June 2021, now with p < 0.00000000001 from 30 studies, recognized in 4 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 148 hospitalized COVID-19 patients in China, showing lower severity and faster viral clearance with improved nutrition.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments1.
|
risk of severe case, 45.0% lower, OR 0.55, p = 0.06, higher quality diet 81, lower quality diet 67, adjusted per study, MNA-SF >11 vs. ≤11, multivariable, RR approximated with OR.
|
|
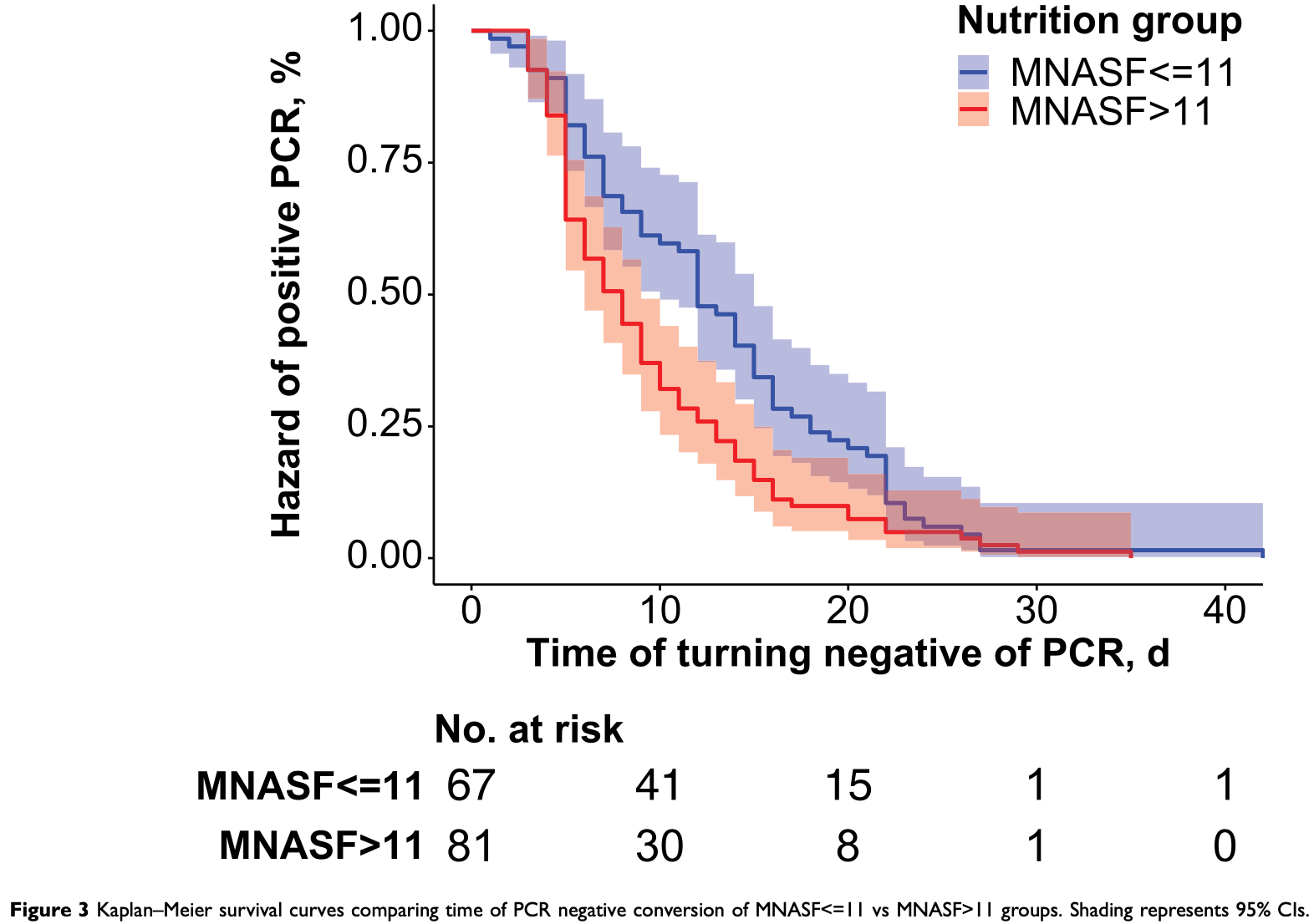
risk of no viral clearance, 31.5% lower, HR 0.68, p = 0.03, higher quality diet 81, lower quality diet 67, inverted to make HR<1 favor higher quality diet, MNA-SF >11 vs. ≤11, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Wang et al., 31 Jul 2023, retrospective, China, peer-reviewed, 9 authors, study period April 2022 - June 2022.
Contact: zjl12616@rjh.com.cn, bangliyong@163.com.
Improving Nutritional Status Was Associated with Decreasing Disease Severity and Shortening of Negative Conversion Time of PCR Test in Non-ICU Patients with COVID-19
Infection and Drug Resistance, doi:10.2147/idr.s409615
Background: Nutrition is an important prevention in old patients with COVID-19. However, in China, there are few studies on the correlation between nutrition and COVID-19. Methods: A total of 148 hospitalized COVID-19 (65.7 ± 16.0 [range: from 21 to 101] years old) patients were enrolled in this study. The information of demographic, biochemical results, vaccination doses, types of COVID-19, PCR test negative conversion time, and scores of Mini Nutritional Assessment Short Form (MNA-SF) for evaluating nutritional status were recorded. We first explored the relationships between MNA-SF performance and the severities of COVID-19 in the groups with non-vaccinated, vaccinated, and all the patients using multivariable ordinal logistic regression. Further, we explored the relationships between performance of MNA-SF and the time of negative conversion of PCR in the groups with non-vaccinated, vaccinated, and all the patients using COX proportional hazards survival regression. Results: Group of patients with malnutrition or at risk of malnutrition group was associated with older of the age, those who had not been vaccinated, in fewer people who were asymptomatic type and in more people who showed longer of the negative conversion time of PCR, lower of the BMI, and the lower of the hemoglobin level. Each additional increase of one point of MNA-SF was associated with a 17% decrease in the odds of a worse type of COVID-19 in all patients, and the significant result exists in non-vaccinated patients. One point increase of MNA-SF was associated with increased 11% of hazard ratios of turning negative of PCR and wellnourished group was associated with increased 46% of hazard ratio of turning negative of PCR. Conclusion: Higher nutrition is associated with less severity of COVID-19, especially in the non-vaccinated group. Higher nutrition is also associated with shorter time of turning negative of PCR in non-ICU COVID-19 patients.
Author Contributions All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure The authors declare no conflicts of interest in this work.
Dovepress
References
Agarwal, Busse, Innate and adaptive immunosenescence, Ann Allergy Asthma Immunol, doi:10.1016/j.anai.2009.11.009
Alexander, Tinkov, Strand, Alehagen, Skalny et al., Early nutritional interventions with zinc, selenium and Vitamin D for raising anti-viral resistance against progressive COVID-19, Nutrients, doi:10.3390/nu12082358
Antwi, Appiah, Oluwakuse, Abu, The nutrition-COVID-19 interplay: a review, Curr Nutr Rep, doi:10.1007/s13668-021-00380-2
Borsche, Glauner, Mendel, COVID-19 mortality risk correlates inversely with Vitamin D3 status, and a mortality rate close to zero could theoretically be achieved at 50 ng/mL 25(OH)D3: results of a systematic review and meta-analysis, Nutrients, doi:10.3390/nu13103596
Bosello, Vanzo, Obesity paradox and aging, Eat Weight Disord, doi:10.1007/s40519-019-00815-4
Calder, Nutrition and immunity: lessons for COVID-19, Eur J Clin Nutr, doi:10.1038/s41430-021-00949-8
Core, R: a language and environment for statistical computing
Galmés, Serra, Palou, Current state of evidence: influence of nutritional and nutrigenetic factors on immunity in the COVID-19 pandemic framework, Nutrients, doi:10.3390/nu12092738
Kacimi, Klouche-Djedid, Riffi, Determinants of COVID-19 vaccine engagement in Algeria: a population-based study with systematic review of studies from Arab countries of the MENA region, doi:10.3389/fpubh.2022.843449
Kaluźniak-Szymanowska, Krzymińska-Siemaszko, Lewandowicz, Deskur-Śmielecka, Stachnik et al., Diagnostic performance and accuracy of the MNA-SF against GLIM criteria in community-dwelling older adults from Poland, Nutrients, doi:10.3390/nu13072183
Kananen, Eriksdotter, Boström, Body mass index and mini nutritional assessment-short form as predictors of in-geriatric hospital mortality in older adults with COVID-19, Clin Nutr, doi:10.1016/j.clnu.2021.07.025
Kaur, Rasane, Singh, Nutritional interventions for elderly and considerations for the development of geriatric foods, Curr Aging Sci, doi:10.2174/1874609812666190521110548
Landi, Barillaro, Bellieni, The new challenge of geriatrics: saving frail older people from the Sars-COV-2 pandemic infection, J Nutr Health Aging, doi:10.1007/s12603-020-1356-x
Lange, Nakamura, Lifestyle factors in the prevention of COVID-19, Glob Health J, doi:10.1016/j.glohj.2020.11.002
Liu, Zhang, Mao, Wang, Hu, Clinical significance of nutritional risk screening for older adult patients with COVID-19, Eur J Clin Nutr, doi:10.1038/s41430-020-0659-7
Lochs, Allison, Meier, Introductory to the ESPEN guidelines on enteral nutrition: terminology, definitions and general topics, Clin Nutr, doi:10.1016/j.clnu.2006.02.007
Majumder, Minko, Recent developments on therapeutic and diagnostic approaches for COVID-19, AAPS J, doi:10.1208/s12248-020-00532-2
Pawelec, Larbi, Derhovanessian, Senescence of the human immune system, J Comp Pathol, doi:10.1016/j.jcpa.2009.09.005
Rubenstein, Harker, Salvà, Guigoz, Vellas, Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF), J Gerontol a Biol Sci Med Sci, doi:10.1093/gerona/56.6.M366
Silva, Lima, Sena-Evangelista, Marchioni, Cobucci et al., Nutritional risk screening tools for older adults with COVID-19: a systematic review, Nutrients, doi:10.3390/nu12102956
Tan, Wong, Tan, St, Knowledge, attitudes, and practices towards COVID-19 among undergraduates during emergency remote learning, Discov Soc Sci Health, doi:10.1007/s44155-022-00017-x
Tang, Luo, Zhao, Relationship between body mass index and arterial stiffness in a health assessment Chinese population, Medicine, doi:10.1097/MD.0000000000018793
Woolford, Angelo, Curtis, COVID-19 and associations with frailty and multimorbidity: a prospective analysis of UK Biobank participants, Aging Clin Exp Res, doi:10.1007/s40520-020-01653-6
Yang, Zhao, Deng, Pulse wave velocity is decreased with obesity in an elderly Chinese population, J Clin Hypertens, doi:10.1111/jch.13659
Zabetakis, Lordan, Norton, Tsoupras, COVID-19: the inflammation link and the role of nutrition in potential mitigation, Nutrients, doi:10.3390/nu12051466
Zhang, Gui, Cong, He, A modified nutrition risk screening 2002 predicts the risk of death among hospitalized patients with COVID-19, Clin Nutr ESPEN, doi:10.1016/j.clnesp.2022.09.018
Zhang, Wang, Ning, Ping, Protecting older people: a high priority during the COVID-19 pandemic, Lancet, doi:10.1016/S0140-6736(22)01530-6
DOI record:
{
"DOI": "10.2147/idr.s409615",
"ISSN": [
"1178-6973"
],
"URL": "http://dx.doi.org/10.2147/idr.s409615",
"author": [
{
"ORCID": "http://orcid.org/0000-0003-1610-1626",
"affiliation": [],
"authenticated-orcid": true,
"family": "Wang",
"given": "Xiaodan",
"sequence": "first"
},
{
"affiliation": [],
"family": "Deng",
"given": "Weiping",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhao",
"given": "Jiehui",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0009-0006-7290-1184",
"affiliation": [],
"authenticated-orcid": true,
"family": "Guo",
"given": "Yongchao",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lai",
"given": "Haifang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hu",
"given": "Yueliang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kang",
"given": "Wenyan",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7859-8936",
"affiliation": [],
"authenticated-orcid": true,
"family": "Li",
"given": "Yong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zuo",
"given": "Junli",
"sequence": "additional"
}
],
"container-title": "Infection and Drug Resistance",
"container-title-short": "IDR",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
7,
6
]
],
"date-time": "2023-07-06T07:45:57Z",
"timestamp": 1688629557000
},
"deposited": {
"date-parts": [
[
2023,
7,
6
]
],
"date-time": "2023-07-06T07:46:04Z",
"timestamp": 1688629564000
},
"indexed": {
"date-parts": [
[
2023,
7,
7
]
],
"date-time": "2023-07-07T04:23:26Z",
"timestamp": 1688703806008
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
7
]
]
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/3.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
7,
1
]
],
"date-time": "2023-07-01T00:00:00Z",
"timestamp": 1688169600000
}
}
],
"link": [
{
"URL": "https://www.dovepress.com/getfile.php?fileID=90984",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.dovepress.com/getfile.php?fileID=90984",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "301",
"original-title": [],
"page": "4443-4452",
"prefix": "10.2147",
"published": {
"date-parts": [
[
2023,
7
]
]
},
"published-online": {
"date-parts": [
[
2023,
7
]
]
},
"publisher": "Informa UK Limited",
"reference": [
{
"DOI": "10.1007/s44155-022-00017-x",
"author": "Tan",
"doi-asserted-by": "publisher",
"first-page": "13",
"journal-title": "Discov Soc Sci Health",
"key": "ref1",
"volume": "2",
"year": "2022"
},
{
"DOI": "10.1208/s12248-020-00532-2",
"author": "Majumder",
"doi-asserted-by": "publisher",
"first-page": "14",
"journal-title": "AAPS J",
"key": "ref2",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.3390/nu12102956",
"author": "Silva",
"doi-asserted-by": "publisher",
"first-page": "2956",
"journal-title": "Nutrients",
"key": "ref3",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1038/s41430-020-0659-7",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "876",
"journal-title": "Eur J Clin Nutr",
"key": "ref4",
"volume": "74",
"year": "2020"
},
{
"DOI": "10.1016/j.clnu.2006.02.007",
"author": "Lochs",
"doi-asserted-by": "publisher",
"first-page": "180",
"journal-title": "Clin Nutr",
"key": "ref5",
"volume": "25",
"year": "2006"
},
{
"DOI": "10.1007/s13668-021-00380-2",
"author": "Antwi",
"doi-asserted-by": "publisher",
"first-page": "364",
"journal-title": "Curr Nutr Rep",
"key": "ref6",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.3390/nu12092738",
"author": "Galmés",
"doi-asserted-by": "publisher",
"first-page": "2738",
"journal-title": "Nutrients",
"key": "ref7",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1093/gerona/56.6.M366",
"author": "Rubenstein",
"doi-asserted-by": "publisher",
"first-page": "M366",
"journal-title": "J Gerontol a Biol Sci Med Sci",
"key": "ref8",
"volume": "56",
"year": "2001"
},
{
"DOI": "10.3390/nu13072183",
"author": "Kaluźniak-Szymanowska",
"doi-asserted-by": "publisher",
"first-page": "2183",
"journal-title": "Nutrients",
"key": "ref9",
"volume": "13",
"year": "2021"
},
{
"key": "ref10",
"unstructured": "R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2022. Available from: https://www.R-project.org/. Accessed June 20, 2023."
},
{
"DOI": "10.2174/1874609812666190521110548",
"author": "Kaur",
"doi-asserted-by": "publisher",
"first-page": "15",
"journal-title": "Curr Aging Sci",
"key": "ref11",
"volume": "12",
"year": "2019"
},
{
"DOI": "10.1016/j.jcpa.2009.09.005",
"author": "Pawelec",
"doi-asserted-by": "publisher",
"first-page": "S39",
"journal-title": "J Comp Pathol",
"key": "ref12",
"volume": "142",
"year": "2010"
},
{
"DOI": "10.1016/j.anai.2009.11.009",
"author": "Agarwal",
"doi-asserted-by": "publisher",
"first-page": "183",
"journal-title": "Ann Allergy Asthma Immunol",
"key": "ref13",
"volume": "104",
"year": "2010"
},
{
"DOI": "10.1016/j.clnu.2021.07.025",
"author": "Kananen",
"doi-asserted-by": "publisher",
"first-page": "2973",
"journal-title": "Clin Nutr",
"key": "ref14",
"volume": "41",
"year": "2022"
},
{
"DOI": "10.1016/j.clnesp.2022.09.018",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "365",
"journal-title": "Clin Nutr ESPEN",
"key": "ref15",
"volume": "52",
"year": "2022"
},
{
"DOI": "10.1038/s41430-021-00949-8",
"author": "Calder",
"doi-asserted-by": "publisher",
"first-page": "1309",
"journal-title": "Eur J Clin Nutr",
"key": "ref16",
"volume": "75",
"year": "2021"
},
{
"DOI": "10.1007/s40520-020-01653-6",
"author": "Woolford",
"doi-asserted-by": "publisher",
"first-page": "1897",
"journal-title": "Aging Clin Exp Res",
"key": "ref17",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1007/s12603-020-1356-x",
"author": "Landi",
"doi-asserted-by": "publisher",
"first-page": "466",
"journal-title": "J Nutr Health Aging",
"key": "ref18",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1111/jch.13659",
"author": "Yang",
"doi-asserted-by": "publisher",
"first-page": "1379",
"journal-title": "J Clin Hypertens",
"key": "ref19",
"volume": "21",
"year": "2019"
},
{
"DOI": "10.1097/MD.0000000000018793",
"author": "Tang",
"doi-asserted-by": "publisher",
"first-page": "e18793",
"journal-title": "Medicine",
"key": "ref20",
"volume": "99",
"year": "2020"
},
{
"DOI": "10.1007/s40519-019-00815-4",
"author": "Bosello",
"doi-asserted-by": "publisher",
"first-page": "27",
"journal-title": "Eat Weight Disord",
"key": "ref21",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1016/j.glohj.2020.11.002",
"author": "Lange",
"doi-asserted-by": "publisher",
"first-page": "146",
"journal-title": "Glob Health J",
"key": "ref22",
"volume": "4",
"year": "2020"
},
{
"DOI": "10.3390/nu12051466",
"author": "Zabetakis",
"doi-asserted-by": "publisher",
"first-page": "1466",
"journal-title": "Nutrients",
"key": "ref23",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.3390/nu13103596",
"author": "Borsche",
"doi-asserted-by": "publisher",
"first-page": "3596",
"journal-title": "Nutrients",
"key": "ref24",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3390/nu12082358",
"author": "Alexander",
"doi-asserted-by": "publisher",
"first-page": "2358",
"journal-title": "Nutrients",
"key": "ref25",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(22)01530-6",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "729",
"journal-title": "Lancet",
"key": "ref26",
"volume": "400",
"year": "2022"
},
{
"DOI": "10.3389/fpubh.2022.843449",
"author": "Kacimi",
"doi-asserted-by": "publisher",
"first-page": "843449",
"journal-title": "Front Public Health",
"key": "ref27",
"volume": "10",
"year": "2022"
}
],
"reference-count": 27,
"references-count": 27,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.dovepress.com/improving-nutritional-status-was-associated-with-decreasing-disease-se-peer-reviewed-fulltext-article-IDR"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Pharmacology (medical)",
"Infectious Diseases",
"Pharmacology"
],
"subtitle": [],
"title": "Improving Nutritional Status Was Associated with Decreasing Disease Severity and Shortening of Negative Conversion Time of PCR Test in Non-ICU Patients with COVID-19",
"type": "journal-article",
"volume": "Volume 16"
}