Multidimensional Sleep Health Prior to SARS-CoV-2 Infection and Risk of Post–COVID-19 Condition
et al., JAMA Network Open, doi:10.1001/jamanetworkopen.2023.15885, May 2023
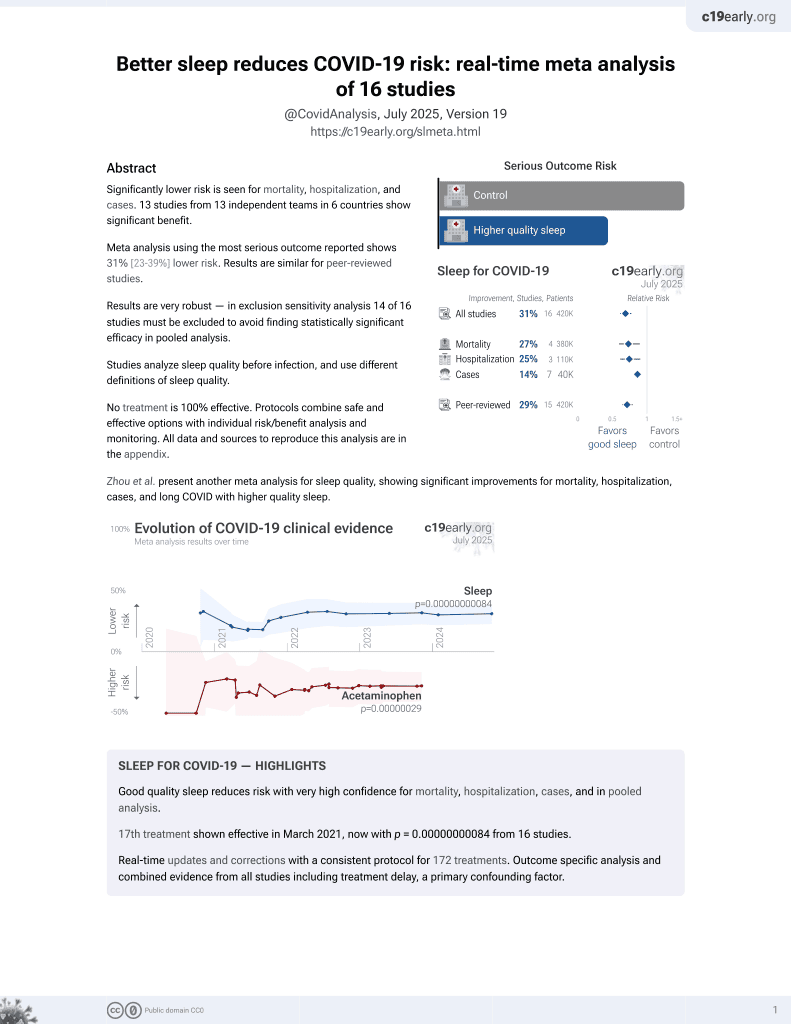
Sleep for COVID-19
18th treatment shown to reduce risk in
March 2021, now with p = 0.00000000084 from 16 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 1,979 nurses in the USA, showing lower risk of long COVID with better sleep quality.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
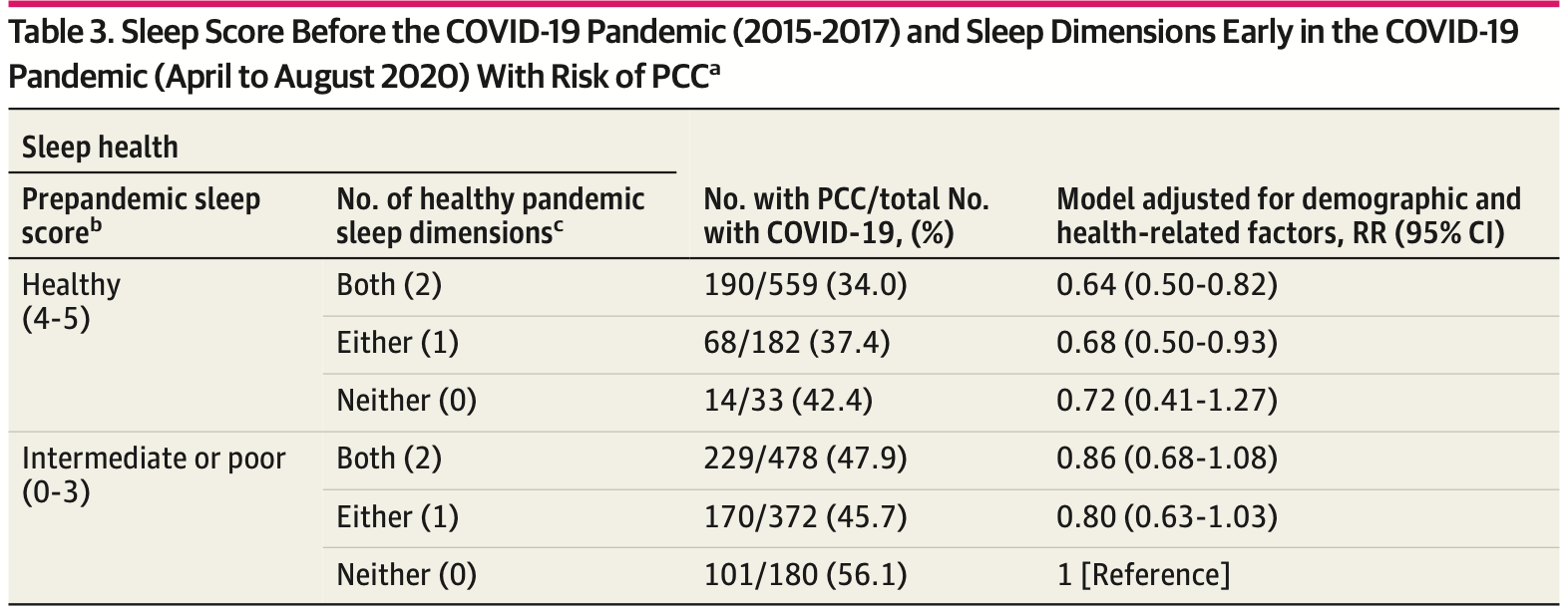
risk of long COVID, 36.0% lower, RR 0.64, p < 0.001, improved sleep 559, worse sleep 180, adjusted per study, healthy sleep before and during the pandemic, multivariable.
|
|
risk of long COVID, 18.0% lower, RR 0.82, p = 0.03, adjusted per study, healthy sleep during the pandemic, multivariable.
|
|
risk of long COVID, 30.0% lower, RR 0.70, p = 0.02, improved sleep 238, worse sleep 166, adjusted per study, healthy sleep before the pandemic, sleep score 5 vs. score 0 or 1, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Wang et al., 30 May 2023, retrospective, USA, peer-reviewed, 6 authors.
Multidimensional Sleep Health Prior to SARS-CoV-2 Infection and Risk of Post-COVID-19 Condition
doi:10.1001/jamanetworkopen.2023.15885
IMPORTANCE The association of multiple healthy sleep dimensions with post-COVID-19 condition (PCC), also known as long COVID, has not been investigated. OBJECTIVE To examine whether multidimensional sleep health before and during the COVID-19 pandemic, prior to SARS-CoV-2 infection, was associated with the risk of PCC. DESIGN, SETTING, AND PARTICIPANTS This prospective cohort study (2015-2021) included Nurses' Health Study II participants who reported testing positive (n = 2303) for SARS-CoV-2 infection in a substudy series of COVID-19-related surveys (n = 32 249) between April 2020 and November 2021. After exclusion for incomplete information about sleep health and nonresponse to a question about PCC, 1979 women were included in the analysis. EXPOSURES Sleep health was measured both before (June 1, 2015, to May 31, 2017) and early (April 1 to August 31, 2020) in the COVID-19 pandemic. Prepandemic sleep score was defined according to 5 dimensions: morning chronotype (assessed in 2015), 7 to 8 hours of sleep per day, low insomnia symptoms, no snoring, and no frequent daytime dysfunction (all assessed in 2017). On the first COVID-19 substudy survey (returned between April and August 2020), average daily sleep duration and sleep quality for the past 7 days were queried. MAIN OUTCOMES AND MEASURES SARS-CoV-2 infection and PCC (Ն4 weeks of symptoms) were self-reported during 1 year of follow-up. Comparisons were examined between June 8, 2022, and January 9, 2023, using Poisson regression models. RESULTS Of the 1979 participants reporting SARS-CoV-2 infection (mean [SD] age, 64.7 [4.6] years; 1979 [100%] female; and 1924 [97.2%] White vs 55 [2.8%] other races and ethnicities), 845 (42.7%) were frontline health care workers, and 870 (44.0%) developed PCC. Compared with women who had a prepandemic sleep score of 0 or 1 (least healthy), those who scored 5 (most healthy) had a 30% lower risk of developing PCC (multivariable-adjusted relative risk, 0.70; 95% CI, 0.52-0.94; P for trend <.001). Associations did not differ by health care worker status. No or little daytime dysfunction prepandemic and good sleep quality during the pandemic were independently associated with a lower risk of PCC (relative risk, 0.83 [95% CI, 0.71-0.98] and 0.82 [95% CI, 0.69-0.99], respectively). Results were similar when PCC was defined as having 8 or more weeks of symptoms or as having ongoing symptoms at the time of PCC assessment.
CONCLUSIONS AND RELEVANCE The findings indicate that healthy sleep measured prior to SARS-CoV-2 infection, both before and during the COVID-19 pandemic, may be protective against PCC. Future research should investigate whether interventions on sleep health may prevent PCC or improve PCC symptoms.
References
Amariglio, Townsend, Grodstein, Sperling, Rentz, Specific subjective memory complaints in older persons may indicate poor cognitive function, J Am Geriatr Soc, doi:10.1111/j.1532-5415.2011.03543.x
Antonelli, Pujol, Spector, Ourselin, Steves, Risk of long COVID associated with Delta versus Omicron variants of SARS-CoV-2, Lancet, doi:10.1016/S0140-6736(22)00941-2
Arendt, Melatonin and human rhythms, Chronobiol Int, doi:10.1080/07420520500464361
Azzolini, Levi, Sarti, Association between BNT162b2 vaccination and long COVID after infections not requiring hospitalization in health care workers, JAMA, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2022.11691&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2023.15885
Bao, Bertoia, Lenart, Origin, methods, and evolution of the Three Nurses' Health Studies, Am J Public Health, doi:10.2105/AJPH.2016.303338
Behan, Behan, Gow, Cavanagh, Gillespie, Enteroviruses and postviral fatigue syndrome, Ciba Found Symp, doi:10.1002/9780470514382.ch9
Besedovsky, Lange, Haack, The sleep-immune crosstalk in health and disease, Physiol Rev, doi:10.1152/physrev.00010.2018
Bliwise, Nekich, Dement, Relative validity of self-reported snoring as a symptom of sleep apnea in a sleep clinic population, Chest, doi:10.1378/chest.99.3.600
Choutka, Jansari, Hornig, Iwasaki, Unexplained post-acute infection syndromes, Nat Med, doi:10.1038/s41591-022-01810-6
Crook, Raza, Nowell, Young, Long COVID-mechanisms, risk factors, and management, BMJ, doi:10.1136/bmj.n1648
De Punder, Heim, Entringer, Association between chronotype and body mass index: the role of C-reactive protein and the cortisol response to stress, Psychoneuroendocrinology, doi:10.1016/j.psyneuen.2019.104388
Doi, Minowa, Uchiyama, Okawa, Subjective sleep quality and sleep problems in the general Japanese adult population, Psychiatry Clin Neurosci, doi:10.1046/j.1440-1819.2001.00830.x
Fan, Sun, Zhou, Sleep patterns, genetic susceptibility, and incident cardiovascular disease: a prospective study of 385 292 UK Biobank participants, Eur Heart J, doi:10.1093/eurheartj/ehz849
Geng, Li, Ma, Heianza, Qi, Adherence to a healthy sleep pattern and risk of chronic kidney disease: the UK Biobank study, Mayo Clin Proc, doi:10.1016/j.mayocp.2021.08.028
Go, Duke, Harrell, Development and validation of a Structured Telephone Interview for Dementia Assessment (STIDA): the NIMH Genetics Initiative, J Geriatr Psychiatry Neurol, doi:10.1177/089198879701000407
Groff, Sun, Ssentongo, Short-term and long-term rates of postacute sequelae of SARS-CoV-2 infection: a systematic review, JAMA Netw Open, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jamanetworkopen.2021.28568&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2023.15885
Hanson, Abbafati, Aerts, Global Burden of Disease Long COVID Collaborators. Estimated global proportions of individuals with persistent fatigue, cognitive, and respiratory symptom clusters following symptomatic COVID-19 in 2020 and 2021, JAMA, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2022.18931&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2023.15885
Hariyanto, Kurniawan, Obstructive sleep apnea (OSA) and outcomes from coronavirus disease 2019 (COVID-19) pneumonia: a systematic review and meta-analysis, Sleep Med, doi:10.1016/j.sleep.2021.03.029
Harvey, Stinson, Whitaker, Moskovitz, Virk, The subjective meaning of sleep quality: a comparison of individuals with and without insomnia, Sleep, doi:10.1093/sleep/31.3.383
Irwin, Olmstead, Carroll, Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation, Biol Psychiatry, doi:10.1016/j.biopsych.2015.05.014
Jahrami, Bahammam, Bragazzi, Saif, Faris et al., Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis, J Clin Sleep Med, doi:10.5664/jcsm.8930
Johnson, Jackson, Williams, Alcántara, Are sleep patterns influenced by race/ethnicity-a marker of relative advantage or disadvantage? evidence to date, Nat Sci Sleep, doi:10.2147/NSS.S169312
Jones, Maisha, Strausz, FinnGen. The public health impact of poor sleep on severe COVID-19, influenza and upper respiratory infections. medRxiv. Preprint posted online February 17, doi:10.1101/2022.02.16.22271055
Kantermann, Sung, Burgess, Comparing the Morningness-Eveningness Questionnaire and Munich ChronoType Questionnaire to the dim light melatonin onset, J Biol Rhythms, doi:10.1177/0748730415597520
Khullar, Zhang, Zang, Racial/ethnic disparities in post-acute sequelae of SARS-CoV-2 infection in New York: an EHR-based cohort study from the RECOVER program, J Gen Intern Med, doi:10.1007/s11606-022-07997-1
Leatherby, What previous COVID-19 waves tell us about the virus now, New York Times
Levine, Dailey, Rockhill, Tipping, Naughton et al., Validation of the Women's Health Initiative Insomnia Rating Scale in a multicenter controlled clinical trial, Psychosom Med, doi:10.1097/01.psy.0000151743.58067.f0
Li, Xue, Wang, Adherence to a healthy sleep pattern and incident heart failure: a prospective study of 408 802 UK Biobank participants, Circulation, doi:10.1161/CIRCULATIONAHA.120.050792
Li, Zheng, Ulsa, Poor sleep behavior burden and risk of COVID-19 mortality and hospitalization, Sleep, doi:10.1093/sleep/zsab138
Liu, Luo, Su, Associations of sleep and circadian phenotypes with COVID-19 susceptibility and hospitalization: an observational cohort study based on the UK Biobank and a two-sample Mendelian randomization study, Sleep, doi:10.1093/sleep/zsac003
Löwe, Wahl, Rose, A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population, J Affect Disord, doi:10.1016/j.jad.2009.06.019
Matenchuk, Mandhane, Kozyrskyj, Sleep, circadian rhythm, and gut microbiota, Sleep Med Rev, doi:10.1016/j.smrv.2020.101340
Morin, Vézina-Im, Ivers, Prevalent, incident, and persistent insomnia in a population-based cohort tested before (2018) and during the first-wave of COVID-19 pandemic, Sleep, doi:10.1093/sleep/zsab258
Nasserie, Hittle, Goodman, Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: a systematic review, JAMA Netw Open, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jamanetworkopen.2021.11417&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2023.15885
Ni, Zhou, Cen, Evidence for causal effects of sleep disturbances on risk for osteoarthritis: a univariable and multivariable Mendelian randomization study, Osteoarthritis Cartilage, doi:10.1016/j.joca.2021.11.021
Patel, Ayas, Malhotra, A prospective study of sleep duration and mortality risk in women, Sleep, doi:10.1093/sleep/27.3.440
Peng, Jing, Ma, He, Gao et al., Insomnia and sleep duration on COVID-19 susceptibility and hospitalization: a Mendelian randomization study, doi:10.3389/fpubh.2022.995664
Peppard, Young, Barnet, Palta, Hagen et al., Increased prevalence of sleep-disordered breathing in adults, Am J Epidemiol, doi:10.1093/aje/kws342
Pinotti, Bertolucci, Frigato, Chronic sleep deprivation markedly reduces coagulation factor VII expression, Haematologica, doi:10.3324/haematol.2010.022475
Prasannan, Heightman, Hillman, Impaired exercise capacity in post-COVID-19 syndrome: the role of VWF-ADAMTS13 axis, Blood Adv, doi:10.1182/bloodadvances.2021006944
Punjabi, Beamer, C-reactive protein is associated with sleep disordered breathing independent of adiposity, Sleep, doi:10.1093/sleep/30.1.29
Qiu, Yu, Li, Li, Sy, Prevalence of sleep disturbances in Chinese healthcare professionals: a systematic review and meta-analysis, Sleep Med, doi:10.1016/j.sleep.2019.01.047
Sambou, Zhao, Hong, Associations between sleep quality and health span: a prospective cohort study based on 328,850 UK Biobank participants, Front Genet, doi:10.3389/fgene.2021.663449
Sands-Lincoln, Loucks, Lu, Sleep duration, insomnia, and coronary heart disease among postmenopausal women in the Women's Health Initiative, J Womens Health (Larchmt), doi:10.1089/jwh.2012.3918
Simpson, Dinges, Sleep and inflammation, Nutr Rev, doi:10.1301/nr.2007.dec.S244-S252
Son, Jamil, Chowdhury, Circulating anti-nuclear autoantibodies in COVID-19 survivors predict long COVID symptoms, Eur Respir J, doi:10.1183/13993003.00970-2022
Subramanian, Nirantharakumar, Hughes, Symptoms and risk factors for long COVID in non-hospitalized adults, Nat Med, doi:10.1038/s41591-022-01909-w
Sudre, Murray, Varsavsky, Attributes and predictors of long COVID, Nat Med, doi:10.1038/s41591-021-01292-y
Toth, Sleep, sleep deprivation and infectious disease: studies in animals, Adv Neuroimmunol, doi:10.1016/0960-5428(94)00045-P
Troy, Hunter, Manson, Colditz, Stampfer et al., The validity of recalled weight among younger women, Int J Obes Relat Metab Disord
Van Buuren, Multiple imputation of discrete and continuous data by fully conditional specification, Stat Methods Med Res, doi:10.1177/0962280206074463
Wang, Quan, Chavarro, Associations of depression, anxiety, worry, perceived stress, and loneliness prior to infection with risk of post-COVID-19 conditions, JAMA Psychiatry, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jamapsychiatry.2022.2640&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2023.15885
Wolf, Hunter, Colditz, Reproducibility and validity of a self-administered physical activity questionnaire, Int J Epidemiol, doi:10.1093/ije/23.5.991
Young, Palta, Dempsey, Peppard, Nieto et al., Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study, WMJ
Yuan, Spiegelman, Rimm, Relative validity of nutrient intakes assessed by questionnaire, 24-hour recalls, and diet records as compared with urinary recovery and plasma concentration biomarkers: findings for women, Am J Epidemiol, doi:10.1093/aje/kwx328
Yuan, Spiegelman, Rimm, Validity of a dietary questionnaire assessed by comparison with multiple weighed dietary records or 24-hour recalls, Am J Epidemiol, doi:10.1093/aje/kww104
Zhang, Xu, Xie, Poor-sleep is associated with slow recovery from lymphopenia and an increased need for ICU care in hospitalized patients with COVID-19: a retrospective cohort study, Brain Behav Immun, doi:10.1016/j.bbi.2020.05.075
Zhou, Eckert, Tierney, Multiple imputation in public health research, Stat Med, doi:10.1002/sim.689
DOI record:
{
"DOI": "10.1001/jamanetworkopen.2023.15885",
"ISSN": [
"2574-3805"
],
"URL": "http://dx.doi.org/10.1001/jamanetworkopen.2023.15885",
"abstract": "<jats:sec id=\"ab-zoi230479-4\"><jats:title>Importance</jats:title><jats:p>The association of multiple healthy sleep dimensions with post–COVID-19 condition (PCC), also known as long COVID, has not been investigated.</jats:p></jats:sec><jats:sec id=\"ab-zoi230479-5\"><jats:title>Objective</jats:title><jats:p>To examine whether multidimensional sleep health before and during the COVID-19 pandemic, prior to SARS-CoV-2 infection, was associated with the risk of PCC.</jats:p></jats:sec><jats:sec id=\"ab-zoi230479-6\"><jats:title>Design, Setting, and Participants</jats:title><jats:p>This prospective cohort study (2015-2021) included Nurses’ Health Study II participants who reported testing positive (n = 2303) for SARS-CoV-2 infection in a substudy series of COVID-19–related surveys (n = 32 249) between April 2020 and November 2021. After exclusion for incomplete information about sleep health and nonresponse to a question about PCC, 1979 women were included in the analysis.</jats:p></jats:sec><jats:sec id=\"ab-zoi230479-7\"><jats:title>Exposures</jats:title><jats:p>Sleep health was measured both before (June 1, 2015, to May 31, 2017) and early (April 1 to August 31, 2020) in the COVID-19 pandemic. Prepandemic sleep score was defined according to 5 dimensions: morning chronotype (assessed in 2015), 7 to 8 hours of sleep per day, low insomnia symptoms, no snoring, and no frequent daytime dysfunction (all assessed in 2017). On the first COVID-19 substudy survey (returned between April and August 2020), average daily sleep duration and sleep quality for the past 7 days were queried.</jats:p></jats:sec><jats:sec id=\"ab-zoi230479-8\"><jats:title>Main Outcomes and Measures</jats:title><jats:p>SARS-CoV-2 infection and PCC (≥4 weeks of symptoms) were self-reported during 1 year of follow-up. Comparisons were examined between June 8, 2022, and January 9, 2023, using Poisson regression models.</jats:p></jats:sec><jats:sec id=\"ab-zoi230479-9\"><jats:title>Results</jats:title><jats:p>Of the 1979 participants reporting SARS-CoV-2 infection (mean [SD] age, 64.7 [4.6] years; 1979 [100%] female; and 1924 [97.2%] White vs 55 [2.8%] other races and ethnicities), 845 (42.7%) were frontline health care workers, and 870 (44.0%) developed PCC. Compared with women who had a prepandemic sleep score of 0 or 1 (least healthy), those who scored 5 (most healthy) had a 30% lower risk of developing PCC (multivariable-adjusted relative risk, 0.70; 95% CI, 0.52-0.94; <jats:italic>P</jats:italic> for trend &amp;lt;.001). Associations did not differ by health care worker status. No or little daytime dysfunction prepandemic and good sleep quality during the pandemic were independently associated with a lower risk of PCC (relative risk, 0.83 [95% CI, 0.71-0.98] and 0.82 [95% CI, 0.69-0.99], respectively). Results were similar when PCC was defined as having 8 or more weeks of symptoms or as having ongoing symptoms at the time of PCC assessment.</jats:p></jats:sec><jats:sec id=\"ab-zoi230479-10\"><jats:title>Conclusions and Relevance</jats:title><jats:p>The findings indicate that healthy sleep measured prior to SARS-CoV-2 infection, both before and during the COVID-19 pandemic, may be protective against PCC. Future research should investigate whether interventions on sleep health may prevent PCC or improve PCC symptoms.</jats:p></jats:sec>",
"author": [
{
"affiliation": [
{
"name": "Department of Nutrition, Harvard T. H. Chan School of Public Health, Boston, Massachusetts"
}
],
"family": "Wang",
"given": "Siwen",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Channing Division of Network Medicine, Department of Medicine, Brigham and Women’s Hospital and Harvard Medical School, Boston, Massachusetts"
}
],
"family": "Huang",
"given": "Tianyi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Environmental Health, Harvard T. H. Chan School of Public Health, Boston, Massachusetts"
}
],
"family": "Weisskopf",
"given": "Marc G.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Channing Division of Network Medicine, Department of Medicine, Brigham and Women’s Hospital and Harvard Medical School, Boston, Massachusetts"
}
],
"family": "Kang",
"given": "Jae H.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Nutrition, Harvard T. H. Chan School of Public Health, Boston, Massachusetts"
},
{
"name": "Channing Division of Network Medicine, Department of Medicine, Brigham and Women’s Hospital and Harvard Medical School, Boston, Massachusetts"
},
{
"name": "Department of Epidemiology, Harvard T. H. Chan School of Public Health, Boston, Massachusetts"
}
],
"family": "Chavarro",
"given": "Jorge E.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Environmental Health, Harvard T. H. Chan School of Public Health, Boston, Massachusetts"
}
],
"family": "Roberts",
"given": "Andrea L.",
"sequence": "additional"
}
],
"container-title": "JAMA Network Open",
"container-title-short": "JAMA Netw Open",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
5,
30
]
],
"date-time": "2023-05-30T15:32:32Z",
"timestamp": 1685460752000
},
"deposited": {
"date-parts": [
[
2023,
5,
30
]
],
"date-time": "2023-05-30T15:32:41Z",
"timestamp": 1685460761000
},
"indexed": {
"date-parts": [
[
2024,
2,
12
]
],
"date-time": "2024-02-12T07:32:39Z",
"timestamp": 1707723159153
},
"is-referenced-by-count": 4,
"issue": "5",
"issued": {
"date-parts": [
[
2023,
5,
30
]
]
},
"journal-issue": {
"issue": "5",
"published-print": {
"date-parts": [
[
2023,
5,
1
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://jamanetwork.com/journals/jamanetworkopen/articlepdf/2805380/wang_2023_oi_230479_1684423433.15861.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "10",
"original-title": [],
"page": "e2315885",
"prefix": "10.1001",
"published": {
"date-parts": [
[
2023,
5,
30
]
]
},
"published-online": {
"date-parts": [
[
2023,
5,
30
]
]
},
"publisher": "American Medical Association (AMA)",
"reference": [
{
"DOI": "10.1001/jama.2022.11691",
"article-title": "Association between BNT162b2 vaccination and long COVID after infections not requiring hospitalization in health care workers.",
"author": "Azzolini",
"doi-asserted-by": "publisher",
"first-page": "676",
"issue": "7",
"journal-title": "JAMA",
"key": "zoi230479r5",
"volume": "328",
"year": "2022"
},
{
"DOI": "10.1016/S0140-6736(22)00941-2",
"article-title": "Risk of long COVID associated with Delta versus Omicron variants of SARS-CoV-2.",
"author": "Antonelli",
"doi-asserted-by": "publisher",
"first-page": "2263",
"issue": "10343",
"journal-title": "Lancet",
"key": "zoi230479r6",
"volume": "399",
"year": "2022"
},
{
"DOI": "10.1001/jamanetworkopen.2021.11417",
"article-title": "Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: a systematic review.",
"author": "Nasserie",
"doi-asserted-by": "publisher",
"issue": "5",
"journal-title": "JAMA Netw Open",
"key": "zoi230479r7",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.28568",
"article-title": "Short-term and long-term rates of postacute sequelae of SARS-CoV-2 infection: a systematic review.",
"author": "Groff",
"doi-asserted-by": "publisher",
"issue": "10",
"journal-title": "JAMA Netw Open",
"key": "zoi230479r8",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1038/s41591-021-01292-y",
"article-title": "Attributes and predictors of long COVID.",
"author": "Sudre",
"doi-asserted-by": "publisher",
"first-page": "626",
"issue": "4",
"journal-title": "Nat Med",
"key": "zoi230479r9",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1001/jama.2022.18931",
"article-title": "Estimated global proportions of individuals with persistent fatigue, cognitive, and respiratory symptom clusters following symptomatic COVID-19 in 2020 and 2021.",
"author": "Wulf Hanson",
"doi-asserted-by": "publisher",
"first-page": "1604",
"issue": "16",
"journal-title": "JAMA",
"key": "zoi230479r10",
"volume": "328",
"year": "2022"
},
{
"DOI": "10.1046/j.1440-1819.2001.00830.x",
"article-title": "Subjective sleep quality and sleep problems in the general Japanese adult population.",
"author": "Doi",
"doi-asserted-by": "publisher",
"first-page": "213",
"issue": "3",
"journal-title": "Psychiatry Clin Neurosci",
"key": "zoi230479r11",
"volume": "55",
"year": "2001"
},
{
"DOI": "10.1093/sleep/zsab258",
"article-title": "Prevalent, incident, and persistent insomnia in a population-based cohort tested before (2018) and during the first-wave of COVID-19 pandemic (2020).",
"author": "Morin",
"doi-asserted-by": "publisher",
"issue": "1",
"journal-title": "Sleep",
"key": "zoi230479r13",
"volume": "45",
"year": "2022"
},
{
"DOI": "10.5664/jcsm.8930",
"article-title": "Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis.",
"author": "Jahrami",
"doi-asserted-by": "publisher",
"first-page": "299",
"issue": "2",
"journal-title": "J Clin Sleep Med",
"key": "zoi230479r14",
"volume": "17",
"year": "2021"
},
{
"DOI": "10.1093/sleep/zsab138",
"article-title": "Poor sleep behavior burden and risk of COVID-19 mortality and hospitalization.",
"author": "Li",
"doi-asserted-by": "publisher",
"issue": "8",
"journal-title": "Sleep",
"key": "zoi230479r15",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.1093/sleep/zsac003",
"article-title": "Associations of sleep and circadian phenotypes with COVID-19 susceptibility and hospitalization: an observational cohort study based on the UK Biobank and a two-sample Mendelian randomization study.",
"author": "Liu",
"doi-asserted-by": "publisher",
"issue": "6",
"journal-title": "Sleep",
"key": "zoi230479r16",
"volume": "45",
"year": "2022"
},
{
"DOI": "10.3389/fpubh.2022.995664",
"article-title": "Insomnia and sleep duration on COVID-19 susceptibility and hospitalization: a Mendelian randomization study.",
"author": "Peng",
"doi-asserted-by": "publisher",
"journal-title": "Front Public Health",
"key": "zoi230479r17",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1016/j.sleep.2021.03.029",
"article-title": "Obstructive sleep apnea (OSA) and outcomes from coronavirus disease 2019 (COVID-19) pneumonia: a systematic review and meta-analysis.",
"author": "Hariyanto",
"doi-asserted-by": "publisher",
"first-page": "47",
"journal-title": "Sleep Med",
"key": "zoi230479r18",
"volume": "82",
"year": "2021"
},
{
"DOI": "10.1016/0960-5428(94)00045-P",
"article-title": "Sleep, sleep deprivation and infectious disease: studies in animals.",
"author": "Toth",
"doi-asserted-by": "publisher",
"first-page": "79",
"issue": "1",
"journal-title": "Adv Neuroimmunol",
"key": "zoi230479r20",
"volume": "5",
"year": "1995"
},
{
"DOI": "10.1093/eurheartj/ehz849",
"article-title": "Sleep patterns, genetic susceptibility, and incident cardiovascular disease: a prospective study of 385?292 UK Biobank participants.",
"author": "Fan",
"doi-asserted-by": "publisher",
"first-page": "1182",
"issue": "11",
"journal-title": "Eur Heart J",
"key": "zoi230479r21",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1136/bmj.n1648",
"article-title": "Long COVID-mechanisms, risk factors, and management.",
"author": "Crook",
"doi-asserted-by": "publisher",
"first-page": "n1648",
"issue": "1648",
"journal-title": "BMJ",
"key": "zoi230479r22",
"volume": "374",
"year": "2021"
},
{
"DOI": "10.1002/9780470514382.ch9",
"article-title": "Enteroviruses and postviral fatigue syndrome.",
"author": "Behan",
"doi-asserted-by": "publisher",
"first-page": "146",
"journal-title": "Ciba Found Symp",
"key": "zoi230479r23",
"volume": "173",
"year": "1993"
},
{
"DOI": "10.1038/s41591-022-01810-6",
"article-title": "Unexplained post-acute infection syndromes.",
"author": "Choutka",
"doi-asserted-by": "publisher",
"first-page": "911",
"issue": "5",
"journal-title": "Nat Med",
"key": "zoi230479r24",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1152/physrev.00010.2018",
"article-title": "The sleep-immune crosstalk in health and disease.",
"author": "Besedovsky",
"doi-asserted-by": "publisher",
"first-page": "1325",
"issue": "3",
"journal-title": "Physiol Rev",
"key": "zoi230479r25",
"volume": "99",
"year": "2019"
},
{
"DOI": "10.2105/AJPH.2016.303338",
"article-title": "Origin, methods, and evolution of the Three Nurses’ Health Studies.",
"author": "Bao",
"doi-asserted-by": "publisher",
"first-page": "1573",
"issue": "9",
"journal-title": "Am J Public Health",
"key": "zoi230479r26",
"volume": "106",
"year": "2016"
},
{
"DOI": "10.1177/0748730415597520",
"article-title": "Comparing the Morningness-Eveningness Questionnaire and Munich ChronoType Questionnaire to the dim light melatonin onset.",
"author": "Kantermann",
"doi-asserted-by": "publisher",
"first-page": "449",
"issue": "5",
"journal-title": "J Biol Rhythms",
"key": "zoi230479r27",
"volume": "30",
"year": "2015"
},
{
"DOI": "10.1080/07420520500464361",
"article-title": "Melatonin and human rhythms.",
"author": "Arendt",
"doi-asserted-by": "publisher",
"first-page": "21",
"issue": "1-2",
"journal-title": "Chronobiol Int",
"key": "zoi230479r28",
"volume": "23",
"year": "2006"
},
{
"DOI": "10.1093/sleep/27.3.440",
"article-title": "A prospective study of sleep duration and mortality risk in women.",
"author": "Patel",
"doi-asserted-by": "publisher",
"first-page": "440",
"issue": "3",
"journal-title": "Sleep",
"key": "zoi230479r29",
"volume": "27",
"year": "2004"
},
{
"DOI": "10.1097/01.psy.0000151743.58067.f0",
"article-title": "Validation of the Women’s Health Initiative Insomnia Rating Scale in a multicenter controlled clinical trial.",
"author": "Levine",
"doi-asserted-by": "publisher",
"first-page": "98",
"issue": "1",
"journal-title": "Psychosom Med",
"key": "zoi230479r30",
"volume": "67",
"year": "2005"
},
{
"DOI": "10.1089/jwh.2012.3918",
"article-title": "Sleep duration, insomnia, and coronary heart disease among postmenopausal women in the Women’s Health Initiative.",
"author": "Sands-Lincoln",
"doi-asserted-by": "publisher",
"first-page": "477",
"issue": "6",
"journal-title": "J Womens Health (Larchmt)",
"key": "zoi230479r31",
"volume": "22",
"year": "2013"
},
{
"DOI": "10.1378/chest.99.3.600",
"article-title": "Relative validity of self-reported snoring as a symptom of sleep apnea in a sleep clinic population.",
"author": "Bliwise",
"doi-asserted-by": "publisher",
"first-page": "600",
"issue": "3",
"journal-title": "Chest",
"key": "zoi230479r32",
"volume": "99",
"year": "1991"
},
{
"DOI": "10.1093/sleep/31.3.383",
"article-title": "The subjective meaning of sleep quality: a comparison of individuals with and without insomnia.",
"author": "Harvey",
"doi-asserted-by": "publisher",
"first-page": "383",
"issue": "3",
"journal-title": "Sleep",
"key": "zoi230479r33",
"volume": "31",
"year": "2008"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.050792",
"article-title": "Adherence to a healthy sleep pattern and incident heart failure: a prospective study of 408 802 UK Biobank participants.",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "97",
"issue": "1",
"journal-title": "Circulation",
"key": "zoi230479r34",
"volume": "143",
"year": "2021"
},
{
"DOI": "10.1016/j.mayocp.2021.08.028",
"article-title": "Adherence to a healthy sleep pattern and risk of chronic kidney disease: the UK Biobank study.",
"author": "Geng",
"doi-asserted-by": "publisher",
"first-page": "68",
"issue": "1",
"journal-title": "Mayo Clin Proc",
"key": "zoi230479r35",
"volume": "97",
"year": "2022"
},
{
"DOI": "10.3389/fgene.2021.663449",
"article-title": "Associations between sleep quality and health span: a prospective cohort study based on 328,850 UK Biobank participants.",
"author": "Sambou",
"doi-asserted-by": "publisher",
"journal-title": "Front Genet",
"key": "zoi230479r36",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1001/jamapsychiatry.2022.2640",
"article-title": "Associations of depression, anxiety, worry, perceived stress, and loneliness prior to infection with risk of post-COVID-19 conditions.",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "1081",
"issue": "11",
"journal-title": "JAMA Psychiatry",
"key": "zoi230479r38",
"volume": "79",
"year": "2022"
},
{
"DOI": "10.1007/s11606-022-07997-1",
"article-title": "Racial/ethnic disparities in post-acute sequelae of SARS-CoV-2 infection in New York: an EHR-based cohort study from the RECOVER program.",
"author": "Khullar",
"doi-asserted-by": "publisher",
"first-page": "1127",
"issue": "5",
"journal-title": "J Gen Intern Med",
"key": "zoi230479r39",
"volume": "38",
"year": "2023"
},
{
"DOI": "10.2147/NSS",
"article-title": "Are sleep patterns influenced by race/ethnicity—a marker of relative advantage or disadvantage? evidence to date.",
"author": "Johnson",
"doi-asserted-by": "publisher",
"first-page": "79",
"journal-title": "Nat Sci Sleep",
"key": "zoi230479r40",
"volume": "11",
"year": "2019"
},
{
"DOI": "10.1093/aje/kww104",
"article-title": "Validity of a dietary questionnaire assessed by comparison with multiple weighed dietary records or 24-hour recalls.",
"author": "Yuan",
"doi-asserted-by": "publisher",
"first-page": "570",
"issue": "7",
"journal-title": "Am J Epidemiol",
"key": "zoi230479r41",
"volume": "185",
"year": "2017"
},
{
"DOI": "10.1093/aje/kwx328",
"article-title": "Relative validity of nutrient intakes assessed by questionnaire, 24-hour recalls, and diet records as compared with urinary recovery and plasma concentration biomarkers: findings for women.",
"author": "Yuan",
"doi-asserted-by": "publisher",
"first-page": "1051",
"issue": "5",
"journal-title": "Am J Epidemiol",
"key": "zoi230479r42",
"volume": "187",
"year": "2018"
},
{
"DOI": "10.1177/089198879701000407",
"article-title": "Development and validation of a Structured Telephone Interview for Dementia Assessment (STIDA): the NIMH Genetics Initiative.",
"author": "Go",
"doi-asserted-by": "publisher",
"first-page": "161",
"issue": "4",
"journal-title": "J Geriatr Psychiatry Neurol",
"key": "zoi230479r43",
"volume": "10",
"year": "1997"
},
{
"DOI": "10.1111/j.1532-5415.2011.03543.x",
"article-title": "Specific subjective memory complaints in older persons may indicate poor cognitive function.",
"author": "Amariglio",
"doi-asserted-by": "publisher",
"first-page": "1612",
"issue": "9",
"journal-title": "J Am Geriatr Soc",
"key": "zoi230479r44",
"volume": "59",
"year": "2011"
},
{
"DOI": "10.1016/j.jad.2009.06.019",
"article-title": "A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population.",
"author": "Löwe",
"doi-asserted-by": "publisher",
"first-page": "86",
"issue": "1-2",
"journal-title": "J Affect Disord",
"key": "zoi230479r45",
"volume": "122",
"year": "2010"
},
{
"DOI": "10.1002/(ISSN)1097-0258",
"article-title": "Multiple imputation in public health research.",
"author": "Zhou",
"doi-asserted-by": "publisher",
"first-page": "1541",
"issue": "9-10",
"journal-title": "Stat Med",
"key": "zoi230479r46",
"volume": "20",
"year": "2001"
},
{
"DOI": "10.1016/j.sleep.2019.01.047",
"article-title": "Prevalence of sleep disturbances in Chinese healthcare professionals: a systematic review and meta-analysis.",
"author": "Qiu",
"doi-asserted-by": "publisher",
"first-page": "258",
"journal-title": "Sleep Med",
"key": "zoi230479r48",
"volume": "67",
"year": "2020"
},
{
"DOI": "10.1177/0962280206074463",
"article-title": "Multiple imputation of discrete and continuous data by fully conditional specification.",
"author": "van Buuren",
"doi-asserted-by": "publisher",
"first-page": "219",
"issue": "3",
"journal-title": "Stat Methods Med Res",
"key": "zoi230479r49",
"volume": "16",
"year": "2007"
},
{
"DOI": "10.1038/s41591-022-01909-w",
"article-title": "Symptoms and risk factors for long COVID in non-hospitalized adults.",
"author": "Subramanian",
"doi-asserted-by": "publisher",
"first-page": "1706",
"issue": "8",
"journal-title": "Nat Med",
"key": "zoi230479r50",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1093/aje/kws342",
"article-title": "Increased prevalence of sleep-disordered breathing in adults.",
"author": "Peppard",
"doi-asserted-by": "publisher",
"first-page": "1006",
"issue": "9",
"journal-title": "Am J Epidemiol",
"key": "zoi230479r51",
"volume": "177",
"year": "2013"
},
{
"article-title": "Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study.",
"author": "Young",
"first-page": "246",
"issue": "5",
"journal-title": "WMJ",
"key": "zoi230479r52",
"volume": "108",
"year": "2009"
},
{
"DOI": "10.1016/j.bbi.2020.05.075",
"article-title": "Poor-sleep is associated with slow recovery from lymphopenia and an increased need for ICU care in hospitalized patients with COVID-19: a retrospective cohort study.",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "50",
"journal-title": "Brain Behav Immun",
"key": "zoi230479r53",
"volume": "88",
"year": "2020"
},
{
"DOI": "10.1016/j.psyneuen.2019.104388",
"article-title": "Association between chronotype and body mass index: the role of C-reactive protein and the cortisol response to stress.",
"author": "de Punder",
"doi-asserted-by": "publisher",
"journal-title": "Psychoneuroendocrinology",
"key": "zoi230479r54",
"volume": "109",
"year": "2019"
},
{
"DOI": "10.1016/j.biopsych.2015.05.014",
"article-title": "Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation.",
"author": "Irwin",
"doi-asserted-by": "publisher",
"first-page": "40",
"issue": "1",
"journal-title": "Biol Psychiatry",
"key": "zoi230479r55",
"volume": "80",
"year": "2016"
},
{
"DOI": "10.1093/sleep/30.1.29",
"article-title": "C-reactive protein is associated with sleep disordered breathing independent of adiposity.",
"author": "Punjabi",
"doi-asserted-by": "publisher",
"first-page": "29",
"issue": "1",
"journal-title": "Sleep",
"key": "zoi230479r56",
"volume": "30",
"year": "2007"
},
{
"DOI": "10.1301/nr.2007.dec.S244-S252",
"article-title": "Sleep and inflammation.",
"author": "Simpson",
"doi-asserted-by": "publisher",
"first-page": "S244",
"issue": "12, pt 2",
"journal-title": "Nutr Rev",
"key": "zoi230479r57",
"volume": "65",
"year": "2007"
},
{
"DOI": "10.1016/j.joca.2021.11.021",
"article-title": "Evidence for causal effects of sleep disturbances on risk for osteoarthritis: a univariable and multivariable Mendelian randomization study.",
"author": "Ni",
"doi-asserted-by": "publisher",
"first-page": "443",
"issue": "3",
"journal-title": "Osteoarthritis Cartilage",
"key": "zoi230479r58",
"volume": "30",
"year": "2022"
},
{
"DOI": "10.1183/13993003.00970-2022",
"article-title": "Circulating anti-nuclear autoantibodies in COVID-19 survivors predict long COVID symptoms.",
"author": "Son",
"doi-asserted-by": "publisher",
"issue": "1",
"journal-title": "Eur Respir J",
"key": "zoi230479r59",
"volume": "61",
"year": "2023"
},
{
"DOI": "10.1016/j.smrv.2020.101340",
"article-title": "Sleep, circadian rhythm, and gut microbiota.",
"author": "Matenchuk",
"doi-asserted-by": "publisher",
"journal-title": "Sleep Med Rev",
"key": "zoi230479r60",
"volume": "53",
"year": "2020"
},
{
"DOI": "10.3324/haematol.2010.022475",
"article-title": "Chronic sleep deprivation markedly reduces coagulation factor VII expression.",
"author": "Pinotti",
"doi-asserted-by": "publisher",
"first-page": "1429",
"issue": "8",
"journal-title": "Haematologica",
"key": "zoi230479r61",
"volume": "95",
"year": "2010"
},
{
"DOI": "10.1182/bloodadvances.2021006944",
"article-title": "Impaired exercise capacity in post-COVID-19 syndrome: the role of VWF-ADAMTS13 axis.",
"author": "Prasannan",
"doi-asserted-by": "publisher",
"first-page": "4041",
"issue": "13",
"journal-title": "Blood Adv",
"key": "zoi230479r62",
"volume": "6",
"year": "2022"
},
{
"DOI": "10.1093/ije/23.5.991",
"article-title": "Reproducibility and validity of a self-administered physical activity questionnaire.",
"author": "Wolf",
"doi-asserted-by": "publisher",
"first-page": "991",
"issue": "5",
"journal-title": "Int J Epidemiol",
"key": "zoi230479r63",
"volume": "23",
"year": "1994"
},
{
"article-title": "The validity of recalled weight among younger women.",
"author": "Troy",
"first-page": "570",
"issue": "8",
"journal-title": "Int J Obes Relat Metab Disord",
"key": "zoi230479r64",
"volume": "19",
"year": "1995"
},
{
"author": "Colten",
"key": "zoi230479r12",
"volume-title": "Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem",
"year": "2006"
},
{
"key": "zoi230479r1",
"unstructured": "Long COVID or post-COVID conditions. Centers for Disease Control and Prevention. Accessed August 24, 2022. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html"
},
{
"key": "zoi230479r2",
"unstructured": "Nearly one in five American adults who have had COVID-19 still have “long COVID.” Centers for Disease Control and Prevention. Accessed August 24, 2022. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/20220622.htm"
},
{
"key": "zoi230479r3",
"unstructured": "COVID-19 for health professionals: post COVID-19 condition (long COVID). Government of Canada. Accessed September 22, 2022. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/post-covid-19-condition.html"
},
{
"key": "zoi230479r4",
"unstructured": "FAIR Health, Inc. A Detailed Study of Patients With Long-Haul COVID: An Analysis of Private Healthcare Claims. FAIR Health, Inc; 2021. Accessed June 7, 2022. https://digirepo.nlm.nih.gov/master/borndig/9918334383006676/9918334383006676.pdf"
},
{
"DOI": "10.1101/2022.02.16.22271055",
"doi-asserted-by": "crossref",
"key": "zoi230479r19",
"unstructured": "Jones? SE, Maisha? FI, Strausz? SJ, ; FinnGen. The public health impact of poor sleep on severe COVID-19, influenza and upper respiratory infections.? medRxiv. Preprint posted online February 17, 2022. doi:10.1101/2022.02.16.2227105535194621"
},
{
"key": "zoi230479r37",
"unstructured": "Leatherby? L. What previous COVID-19 waves tell us about the virus now. New York Times. October 23, 2021. Accessed April 11, 2023. https://www.nytimes.com/interactive/2021/10/23/us/covid-surges.html"
},
{
"key": "zoi230479r47",
"unstructured": "Centers for Disease Control and Prevention. How much sleep do I need? 2017. Accessed June 8, 2022. https://www.cdc.gov/sleep/about_sleep/how_much_sleep.html"
}
],
"reference-count": 64,
"references-count": 64,
"relation": {},
"resource": {
"primary": {
"URL": "https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2805380"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Multidimensional Sleep Health Prior to SARS-CoV-2 Infection and Risk of Post–COVID-19 Condition",
"type": "journal-article",
"volume": "6"
}