Variation in Demographic Characteristics, Socioeconomic Status, Clinical Presentation and Selected Treatments in Mortality Among Patients with a Diagnosis of COVID-19 in the United States
et al., Value in Health, doi:10.1016/j.jval.2023.03.2056, Jun 2023
19th treatment shown to reduce risk in
March 2021, now with p = 0.000095 from 34 studies, recognized in 52 countries.
Efficacy is variant dependent.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
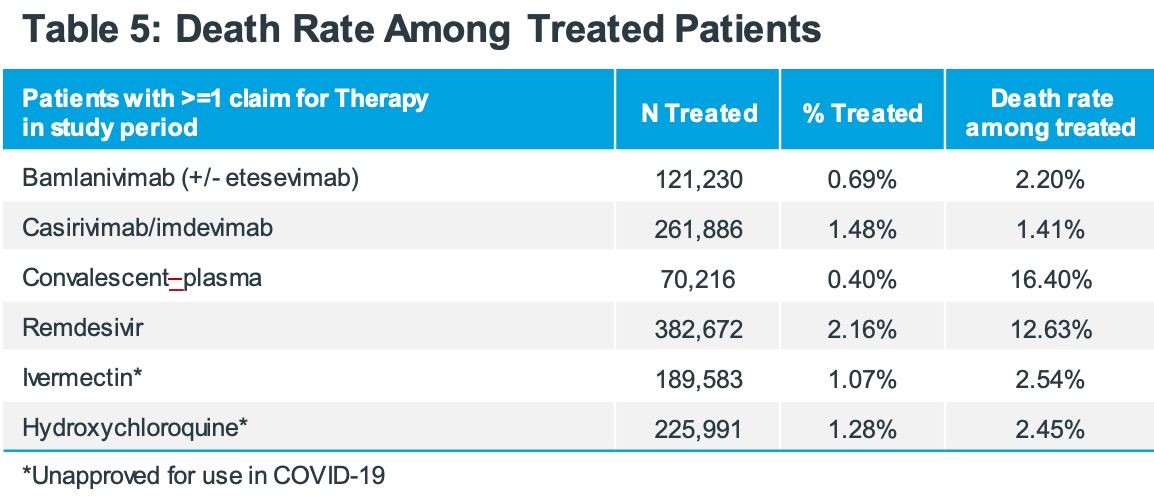
Retrospective analysis of mortality for COVID-19 patients in the USA. Authors do not provide adjusted results, preventing any strong evidence. However it is notable that, despite comparable treatment frequencies, the mortality for patients that received remdesivir or convalescent plasma during COVID-19 is 5-10 times higher than patients receiving monoclonal antibodies, HCQ, or ivermectin. In addition to confounding by indication, politicized treatments were more highly used earlier when politicization was lower and overall mortality was higher.
Adjusted analyses from this data may be valuable and it's unclear why they are not provided. Author has routinely published adjusted analyses, although approval to publish positive results for politicized treatments may not be possible.
Efficacy is variant dependent. In Vitro research suggests a lack of efficacy for many omicron variants1-7.
Study covers HCQ, ivermectin, convalescent plasma, remdesivir, bamlanivimab/etesevimab, and casirivimab/imdevimab.
1.
Liu et al., Striking Antibody Evasion Manifested by the Omicron Variant of SARS-CoV-2, bioRxiv, doi:10.1101/2021.12.14.472719.
2.
Sheward et al., Variable loss of antibody potency against SARS-CoV-2 B.1.1.529 (Omicron), bioRxiv, doi:10.1101/2021.12.19.473354.
3.
VanBlargan et al., An infectious SARS-CoV-2 B.1.1.529 Omicron virus escapes neutralization by several therapeutic monoclonal antibodies, bioRxiv, doi:10.1101/2021.12.15.472828.
4.
Tatham et al., Lack of Ronapreve (REGN-CoV; casirivimab and imdevimab) virological efficacy against the SARS-CoV 2 Omicron variant (B.1.1.529) in K18-hACE2 mice, bioRxiv, doi:10.1101/2022.01.23.477397.
5.
Pochtovyi et al., In Vitro Efficacy of Antivirals and Monoclonal Antibodies against SARS-CoV-2 Omicron Lineages XBB.1.9.1, XBB.1.9.3, XBB.1.5, XBB.1.16, XBB.2.4, BQ.1.1.45, CH.1.1, and CL.1, Vaccines, doi:10.3390/vaccines11101533.
Wade et al., 10 Jun 2023, retrospective, USA, peer-reviewed, 3 authors, study period 1 April, 2020 - 30 April, 2022.
Abstract: RWD26
Variation in Demographic Characteristics, Socioeconomic Status, Clinical Presentation and Selected Treatments in
Mortality Among Patients with a Diagnosis of COVID-19 in the United States
Rolin L Wade, RPh, MS; Riddhi Doshi, PhD; Dajun Tian, MS
IQVIA, Falls Church, Virginia, USA
Background
Results
• As of November 2022, 1,070,947 Coronavirus disease 2019 (COVID19)-related deaths were reported in the United States (US)1
• Older age, male sex, smoking, chronic obstructive pulmonary disease
(COPD), cardiovascular disease, diabetes, obesity, hypertension and
kidney disease are associated with a higher risk of mortality among
patients with COVID-19 infection2
• The US case-mortality rate for COVID-19 was reported to be 1.1%
as of March 20233
• Research on the impact of neighborhood socioeconomic
disadvantage on mortality in COVID-19 patients is lacking
Objective
• This study described the variation in patient demographic and clinical
characteristics and utilization of COVID-specific treatments by
neighborhood socioeconomic disadvantage among patients
confirmed dead after a medical claim with COVID-19 diagnosis
Table 2: Age Distribution of
Confirmed Deaths
Table 3: ADI Distribution of
Confirmed Deaths
Age Group: (n, %)
N
%
Total Mortality Population
563,744
100.00%
2,023
0.36%
0 - 17 y
18-34 y
8,606
1.53%
35-44 y
11,517
2.04%
ADI Level
N
%
0-20 Most Affluent
58,144
10.3%
21-40
91,629
41-60
45-54 y
25,572
4.54%
55-64 y
63,136
11.20%
65 -75 y
133,157
23.62%
> 75 y
319,730
56.72%
3 were unknown age
CCI 0
19.88%
Cardiovascular
CCI 3+
48.45%
CCI 1
15.72%
33.5%
57,887
CCI 2
15.96%
10.3%
CNS,
Cerebrovascular
3 were unknown ADI
Renal
Figure 1: Mortality Rate Total COVID-19 Study Population Q2-2020 to Q1-2022
Metabolic
8.00%
Study Design
7.30%
Mortality Rate
7.00%
• This retrospective cohort study utilized linked data from IQVIA’s
Professional fee claims (Dx), Longitudinal prescription claims (LRx)
and mortality data from Veritas Data Research to identify and
characterize patients with a COVID-19 diagnosis between April 1,
2020 and April 30, 2022
6.00%
3.00%
• A modified version of the Area Deprivation Index (ADI) was used to
assess neighborhood socioeconomic disadvantage from HIPAA
compliant databases
0.00%
• Presence of chain-of-event conditions (COE) (+/- 7 days of the last
COVID diagnosis date) and significant contributing conditions
(SCC) (over the study period) were assessed5
Mean Study Mortality
rate 3.19%
3.49%
4.00%
2.00%
2.39%
2.56%
J Hopkins reported
Mortality Rate 1.1%
Q2 2020
Q3 2020
Q4 2020
Q1 2021
Q2 2021
Q3 2021
Q4 2021
Q1 2022
Time Period
Figure 3: Mortality Rate by Age Group
18%
277,286,899
17,682,111
6.4%
Patients with a mortality flag in the Veritas Data Research database
563,744
0.2%
34.02%
10.95%
Atrial fibrillation and flutter
31.77%
15.50%
Congestive heart failure
37.82%
15.79%
Hypertensive heart disease without CHF
5.00%
7.43%
Hyperlipidemia, unspecified
39.88%
5.66%
Alzheimer disease, unspecified
11.20%
23.40%
Unspecified dementia
23.70%
21.62%
Stroke, not specified as hemorrhage or
infarction (I64)
11.56%
13.37%
Other specified disorders of kidney and ureter
13.62%
8.74%
Chronic kidney disease, unspecified
23.64%
15.30%
Unspecified diabetes mellitus without complications
0.69%
7.14%
Type 2 diabetes mellitus without complications
44.61%
7.46%
Obesity, unspecified
16.97%
2.75%
Pulmonary
Chronic..
DOI record:
{
"DOI": "10.1016/j.jval.2023.03.2056",
"ISSN": [
"1098-3015"
],
"URL": "http://dx.doi.org/10.1016/j.jval.2023.03.2056",
"alternative-id": [
"S1098301523021563"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "RWD26 Variation in Demographic Characteristics, Socioeconomic Status, Clinical Presentation and Selected Treatments in Mortality Among Patients with a Diagnosis of COVID-19 in the United States"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Value in Health"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.jval.2023.03.2056"
},
{
"label": "Content Type",
"name": "content_type",
"value": "simple-article"
},
{
"label": "Copyright",
"name": "copyright"
}
],
"author": [
{
"affiliation": [],
"family": "Wade",
"given": "R.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Doshi",
"given": "R.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tian",
"given": "D.",
"sequence": "additional"
}
],
"container-title": "Value in Health",
"container-title-short": "Value in Health",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.es",
"clinicalkey.com.au",
"valueinhealthjournal.com",
"clinicalkey.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2023,
6,
10
]
],
"date-time": "2023-06-10T16:28:47Z",
"timestamp": 1686414527000
},
"deposited": {
"date-parts": [
[
2023,
6,
10
]
],
"date-time": "2023-06-10T16:28:49Z",
"timestamp": 1686414529000
},
"indexed": {
"date-parts": [
[
2023,
6,
11
]
],
"date-time": "2023-06-11T04:15:44Z",
"timestamp": 1686456944667
},
"is-referenced-by-count": 0,
"issue": "6",
"issued": {
"date-parts": [
[
2023,
6
]
]
},
"journal-issue": {
"issue": "6",
"published-print": {
"date-parts": [
[
2023,
6
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
6,
1
]
],
"date-time": "2023-06-01T00:00:00Z",
"timestamp": 1685577600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S1098301523021563?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S1098301523021563?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "S365",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2023,
6
]
]
},
"published-print": {
"date-parts": [
[
2023,
6
]
]
},
"publisher": "Elsevier BV",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S1098301523021563"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Public Health, Environmental and Occupational Health",
"Health Policy"
],
"subtitle": [],
"title": "RWD26 Variation in Demographic Characteristics, Socioeconomic Status, Clinical Presentation and Selected Treatments in Mortality Among Patients with a Diagnosis of COVID-19 in the United States",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "26"
}
wade
