Persistent Neurological Deficits in Mouse PASC Reveal Antiviral Drug Limitations
et al., bioRxiv, doi:10.1101/2024.06.02.596989, Jun 2024
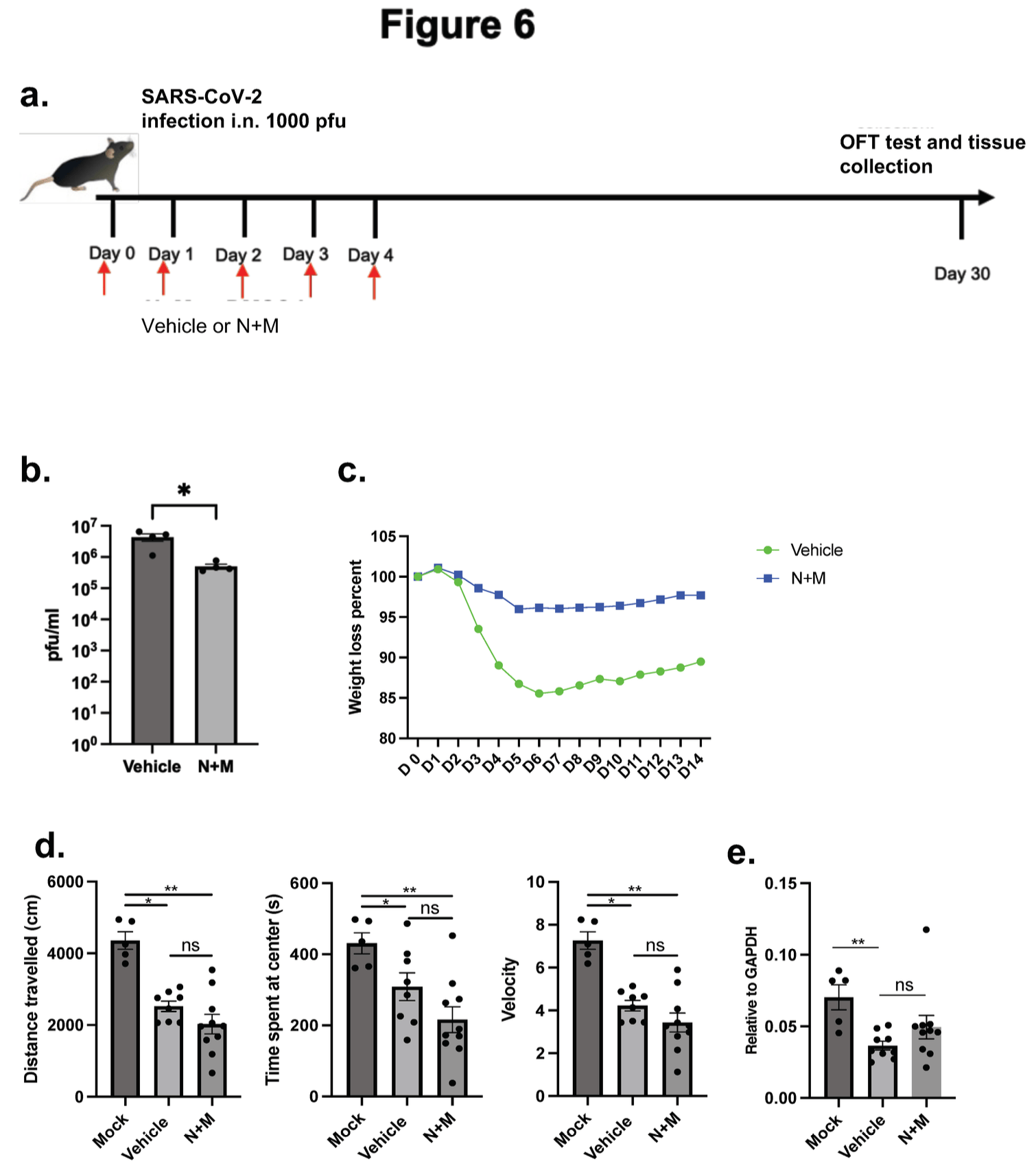
Mouse study showing persistent neurological deficits after SARS-CoV-2 infection, and failure of nirmatrelvir and molnupiravir to prevent neurological damage.
Authors found decreased tyrosine hydroxylase expression in the olfactory bulb and substantia nigra, along with elevated neuroinflammation and microglia activation, months after infection. Behavioral tests revealed impaired motor function. Similar decreases in tyrosine hydroxylase were seen in the substantia nigra of deceased COVID-19 patients.
Early treatment with systemic antivirals nirmatrelvir and molnupiravir did not prevent neurological damage. Administering treatments directly to the respiratory mucosa, where viral replication initially occurs, may be important to minimize the risk of neurological damage.
Study covers molnupiravir and paxlovid.
Verma et al., 3 Jun 2024, USA, preprint, 10 authors.
Contact: stanley-perlman@uiowa.edu.
Persistent Neurological Deficits in Mouse PASC Reveal Antiviral Drug Limitations
Post-Acute Sequelae of COVID-19 (PASC) encompasses persistent neurological symptoms, including olfactory and autonomic dysfunction. Here, we report chronic neurological dysfunction in mice infected with a virulent mouse-adapted SARS-CoV-2 that does not infect the brain. Long after recovery from nasal infection, we observed loss of tyrosine hydroxylase (TH) expression in olfactory bulb glomeruli and neurotransmitter levels in the substantia nigra (SN) persisted. Vulnerability of dopaminergic neurons in these brain areas was accompanied by increased levels of proinflammatory cytokines and neurobehavioral changes. RNAseq analysis unveiled persistent microglia activation, as found in human neurodegenerative diseases. Early treatment with antivirals (nirmatrelvir and molnupiravir) reduced virus titers and lung inflammation but failed to prevent neurological abnormalities, as observed in patients. Together these results show that chronic deficiencies in neuronal function in SARS-CoV-2-infected mice are not directly linked to ongoing olfactory epithelium dysfunction. Rather, they bear similarity with neurodegenerative disease, the vulnerability of which is exacerbated by chronic inflammation.
Author's contributions The study was designed by SP and AKV. Experiments were conducted by AKV, SL, ED, LCL. AKV, MH, QQ, CRY, MWA and SP acquired and analyzed data. JE helped with RNAseq data analysis. LCL, MH provided reagents. Manuscript was initially prepared by AKV and SP. All of the authors revised and approved the final manuscript.
Conflict of Interest The authors declare no conflict of interest directly related to this study. MWA is a cofounder and owns shares in Aromha, Inc. He has received in kind contributions from Eli Lilly and research
References
Albers, Tabert, Devanand, Olfactory dysfuncAon as a predictor of neurodegeneraAve disease, Curr Neurol Neurosci Rep, doi:10.1007/s11910-996-0018-7
Apple, Risk factors and abnormal cerebrospinal fluid associate with cogniAve symptoms amer mild COVID-19, Ann Clin Transl Neurol, doi:10.1002/acn3.51498
Arentz, CharacterisAcs and Outcomes of 21 CriAcally Ill PaAents With COVID-19 in Washington State, JAMA, doi:10.1001/jama.2020.4326
Awad, Al-Hussaniy, Alburghaif, Tawfeeq, The role of COVID-19 in myopathy: incidence, causes, treatment, and prevenAon, J Med Life, doi:10.25122/jml-2022-0167
Baker, Unilateral, neonatal olfactory deprivaAon alters tyrosine hydroxylase expression but not aromaAc amino acid decarboxylase or GABA immunoreacAvity, Neuroscience, doi:10.1016/0306-4522(90)90018-y
Beckman, SARS-CoV-2 infects neurons and induces neuroinflammaAon in a non-human primate model of COVID-19, Cell Rep, doi:10.1016/j.celrep.2022.111573
Bendella, Brain Volume Changes amer COVID-19 Compared to Healthy Controls by ArAficial Intelligence-Based MRI Volumetry, DiagnosNcs, doi:10.3390/diagnostics13101716
Brunjes, Unilateral naris closure and olfactory system development, Brain Res Brain Res Rev, doi:10.1016/0165-0173(94)90007-8
Bryche, Massive transient damage of the olfactory epithelium associated with infecAon of sustentacular cells by SARS-CoV-2 in golden Syrian hamsters, Brain Behav Immun, doi:10.1016/j.bbi.2020.06.032
Bueno-Carrasco, Structural mechanism for tyrosine hydroxylase inhibiAon by dopamine and reacAvaAon by Ser40 phosphorylaAon, Nat Commun, doi:10.1038/s41467-021-27657-y
Capelli, MRI evidence of olfactory system alteraAons in paAents with COVID-19 and neurological symptoms, J Neurol, doi:10.1007/s00415-023-11561-0
Cgg, AAA CTC C -3' -GGA CAG CTT CTC CGT TTC AGA C-3' PARK -ACG ATG TGG TGG TTC TTC CAG G-3
Chiu, COVID-19-induced anosmia associated with olfactory bulb atrophy, Neuroradiology, doi:10.1007/s00234-020-02554-1
Chou, Global Incidence of Neurological ManifestaAons Among PaAents Hospitalized With COVID-19-A Report for the GCS-NeuroCOVID ConsorAum and the ENERGY ConsorAum, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.12131
Congdon, Nirmatrelvir/ritonavir and risk of long COVID symptoms: a retrospecAve cohort study, Sci Rep, doi:10.1038/s41598-023-46912-4
Dani, Autonomic dysfuncAon in 'long COVID': raAonale, physiology and management strategies, Clin Med (Lond), doi:10.7861/clinmed.2020-0896
De Freitas, Syncope and COVID-19 disease -A systemaAc review, Auton Neurosci, doi:10.1016/j.autneu.2021.102872
Deleidi, Isacson, Viral and inflammatory triggers of neurodegeneraAve diseases, Sci Transl Med, doi:10.1126/scitranslmed.3003492
Doty, OlfacAon in Parkinson's disease and related disorders, Neurobiol Dis, doi:10.1016/j.nbd.2011.10.026
Doty, Olfactory dysfuncAon in neurodegeneraAve diseases: is there a common pathological substrate?, Lancet Neurol, doi:10.1016/S1474-4422(17)30123-0
Douaud, SARS-CoV-2 is associated with changes in brain structure in UK Biobank, Nature, doi:10.1038/s41586-022-04569-5
Duda, Olfactory system pathology as a model of Lewy neurodegeneraAve disease, J Neurol Sci, doi:10.1016/j.jns.2009.08.042
Durstenfeld, AssociaAon of nirmatrelvir for acute SARS-CoV-2 infecAon with subsequent Long COVID symptoms in an observaAonal cohort study, J Med Virol, doi:10.1002/jmv.29333
Eden, Viral AnAgen and Inflammatory Biomarkers in Cerebrospinal Fluid in PaAents With COVID-19 InfecAon and Neurologic Symptoms Compared With Control ParAcipants Without InfecAon or Neurologic Symptoms, JAMA Netw Open, doi:10.1001/jamanetworkopen.2022.13253
Ellul, Neurological associaAons of COVID-19, Lancet Neurol, doi:10.1016/S1474-4422(20)30221-0
Farhadian, Self-Reported Neuropsychiatric Post-COVID-19 CondiAon and CSF Markers of NeuroinflammaAon, JAMA Netw Open, doi:10.1001/jamanetworkopen.2023.42741
Fernandez-Castaneda, Mild respiratory COVID can cause mulA-lineage neural cell and myelin dysregulaAon, Cell, doi:10.1016/j.cell.2022.06.008
Frosolini, MagneAc Resonance Imaging Confirmed Olfactory Bulb ReducAon in Long COVID-19: Literature Review and Case Series, Brain Sci, doi:10.3390/brainsci12040430
Goeryler, SARS-CoV-2, COVID-19 and Parkinson's Disease-Many Issues Need to Be Clarified-A CriAcal Review, Brain Sci, doi:10.3390/brainsci12040456
Haavik, Toska, Tyrosine hydroxylase and Parkinson's disease, Mol Neurobiol, doi:10.1007/BF02741387
Huang, Zhang, Tan, Chen, Links between COVID-19 and Parkinson's disease/Alzheimer's disease: reciprocal impacts, medical care strategies and underlying mechanisms, Transl Neurodegener, doi:10.1186/s40035-023-00337-1
Javoy-Agid, Decreased tyrosine hydroxylase messenger RNA in the surviving dopamine neurons of the substanAa nigra in Parkinson's disease: an in situ hybridizaAon study, Neuroscience, doi:10.1016/0306-4522(90)90389-l
Kaufer, Microgliosis and neuronal proteinopathy in brain persist beyond viral clearance in SARS-CoV-2 hamster model, EBioMedicine, doi:10.1016/j.ebiom.2022.103999
Khan, Delirium Incidence, DuraAon, and Severity in CriAcally Ill PaAents With Coronavirus Disease, Crit Care Explor, doi:10.1097/CCE.0000000000000290
Khan, Visualizing in deceased COVID-19 paAents how SARS-CoV-2 aYacks the respiratory and olfactory mucosae but spares the olfactory bulb, Cell, doi:10.1016/j.cell.2021.10.027
Kim, The AssociaAon of Pre-exisAng Diagnoses of Alzheimer's Disease and Parkinson's Disease and Coronavirus Disease 2019 InfecAon, Severity and Mortality: Results From the Korean NaAonal Health Insurance Database, Front Aging Neurosci, doi:10.3389/fnagi.2022.821235
Kishimoto-Urata, Prolonged and extended impacts of SARS-CoV-2 on the olfactory neurocircuit, Sci Rep, doi:10.1038/s41598-022-09731-7
Ladopoulos, COVID-19: Neuroimaging Features of a Pandemic, J Neuroimaging, doi:10.1111/jon.12819
Lechien, ObjecAve olfactory evaluaAon of self-reported loss of smell in a case series of 86 COVID-19 paAents, Head Neck, doi:10.1002/hed.26279
Lechien, Prevalence and 6-month recovery of olfactory dysfuncAon: a mulAcentre study of 1363 COVID-19 paAents, J Intern Med, doi:10.1111/joim.13209
Lee, ParAculate maYer exposure and neurodegeneraAve diseases: A comprehensive update on toxicity and mechanisms, Ecotoxicol Environ Saf, doi:10.1016/j.ecoenv.2023.115565
Mao, Neurologic ManifestaAons of Hospitalized PaAents With Coronavirus Disease 2019 in Wuhan, China, JAMA Neurol, doi:10.1001/jamaneurol.2020.1127
Maranol, Psychomotor agitaAon and hyperacAve delirium in COVID-19 paAents treated with aripiprazole 9.75 mg/1.3 ml immediate release, Psychopharmacology (Berl), doi:10.1007/s00213-020-05644-3
Matschke, Neuropathology of paAents with COVID-19 in Germany: a post-mortem case series, Lancet Neurol, doi:10.1016/S1474-4422(20)30308-2
Matschke, Young COVID-19 PaAents Show a Higher Degree of Microglial AcAvaAon When Compared to Controls, Front Neurol, doi:10.3389/fneur.2022.908081
Maurizi, Influenza caused epidemic encephaliAs (encephaliAs lethargica): the circumstanAal evidence and a challenge to the nonbelievers, Med Hypotheses, doi:10.1016/j.mehy.2009.12.012
Oaklander, Peripheral Neuropathy EvaluaAons of PaAents With Prolonged Long COVID, Neurol Neuroimmunol Neuroinflamm, doi:10.1212/NXI.0000000000001146
Pan, Meyerholz, Perlman, Cells that survive acute murine SARS-CoV-2 infecAon are detected nearly exclusively in the respiratory tract, J Clin Invest, doi:10.1172/JCI172659
Perez-Lloret, Barrantes, Deficits in cholinergic neurotransmission and their clinical correlates in Parkinson's disease, NPJ Parkinsons Dis, doi:10.1038/npjparkd.2016.1
Philippens, Brain InflammaAon and Intracellular alpha-Synuclein Aggregates in Macaques amer SARS-CoV-2 InfecAon, Viruses, doi:10.3390/v14040776
Poewe, Parkinson disease, Nat Rev Dis Primers, doi:10.1038/nrdp.2017.13
Poloni, COVID-19-related neuropathology and microglial acAvaAon in elderly with and without demenAa, Brain Pathol, doi:10.1111/bpa.12997
Prut, Belzung, The open field as a paradigm to measure the effects of drugs on anxiety-like behaviors: a review, Eur J Pharmacol, doi:10.1016/s0014-2999(03)01272-x
Ranger, PreexisAng Neuropsychiatric CondiAons and Associated Risk of Severe COVID-19 InfecAon and Other Acute Respiratory InfecAons, JAMA Psychiatry, doi:10.1001/jamapsychiatry.2022.3614
Rao, Hidayathullah, Hegde, Adhikari, Parkinsonism: An emerging post COVID sequelae, IDCases, doi:10.1016/j.idcr.2022.e01388
Ravenholt, Foege, influenza, encephaliAs lethargica, parkinsonism, Lancet, doi:10.1016/s0140-6736(82)90820-0
Renaud, Clinical Outcomes for PaAents With Anosmia 1 Year Amer COVID-19 Diagnosis, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.15352
Rinne, Rummukainen, Paljarvi, Rinne, DemenAa in Parkinson's disease is related to neuronal loss in the medial substanAa nigra, Ann Neurol, doi:10.1002/ana.410260107
Rodriguez, Innate immune signaling in the olfactory epithelium reduces odorant receptor levels: modeling transient smell loss in COVID-19 paAents, medRxiv, doi:10.1101/2020.06.14.20131128
Saiegh, Status of SARS-CoV-2 in cerebrospinal fluid of paAents with COVID-19 and stroke, J Neurol Neurosurg Psychiatry, doi:10.1136/jnnp-2020-323522
Simunovic, Gene expression profiling of substanAa nigra dopamine neurons: further insights into Parkinson's disease pathology, Brain, doi:10.1093/brain/awn323
Soung, COVID-19 induces CNS cytokine expression and loss of hippocampal neurogenesis, Brain, doi:10.1093/brain/awac270
Sudre, ageusia, and other COVID-19-like symptoms in associaAon with a posiAve SARS-CoV-2 test, across six naAonal digital surveillance plagorms: an observaAonal study, Lancet Digit Health, doi:10.1016/S2589-7500(21)00115-1
Surmeier, Determinants of dopaminergic neuron loss in Parkinson's disease, FEBS J, doi:10.1111/febs.14607
Tata, Velluto, D'angelo, Reale, Cholinergic system dysfuncAon and neurodegeneraAve diseases: cause or effect?, CNS Neurol Disord Drug Targets, doi:10.2174/1871527313666140917121132
Taubenberger, Morens, Influenza: the mother of all pandemics, Emerg Infect Dis, doi:10.3201/eid1201.050979
Th, ACA CAG TAC ATC CGT CAT GC-3' 5'-GCA AAT GTGCGG TCAGCC AAC A-3' IL-6 5'-GAG GAT ACC ACT CCC AAC AGA CC-3' 5'-AAG TGC ATC ATC GTT GTT ACA-3' IFN-b 5'-TCA GAA TGA GTG GTG GTT GC-3' 5
Tolleson, Claassen, The funcAon of tyrosine hydroxylase in the normal and Parkinsonian brain, CNS Neurol Disord Drug Targets, doi:10.2174/187152712800792794
Verma, Zheng, Meyerholz, Perlman, SARS-CoV-2 infecAon of sustentacular cells disrupts olfactory signaling pathways, JCI Insight, doi:10.1172/jci.insight.160277
Wellford, Moseman, Olfactory immune response to SARS-CoV-2, Cell Mol Immunol, doi:10.1038/s41423-023-01119-5
Wilke, Delirium in hospitalized COVID-19 paAents: Predictors and implicaAons for paAent outcome, PLoS One, doi:10.1371/journal.pone.0278214
Wong, Eicosanoid signalling blockade protects middle-aged mice from severe COVID-19, Nature, doi:10.1038/s41586-022-04630-3
Wong, Serotonin reducAon in post-acute sequelae of viral infecAon, Cell, doi:10.1016/j.cell.2023.09.013
Wu, Mcgoogan, CharacterisAcs of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and PrevenAon, JAMA, doi:10.1001/jama.2020.2648
Xie, Bowe, Al-Aly, Burdens of post-acute sequelae of COVID-19 by severity of acute infecAon, demographics and health status, Nat Commun, doi:10.1038/s41467-021-26513-3
Xing, Sapuan, Dineen, Auer, Life span pigmentaAon changes of the substanAa nigra detected by neuromelanin-sensiAve MRI, Mov Disord, doi:10.1002/mds.27502
Xu, Xie, Al-Aly, Long-term neurologic outcomes of COVID-19, Nature medicine, doi:10.1038/s41591-022-02001-z
Xydakis, Post-viral effects of COVID-19 in the olfactory system and their implicaAons, Lancet Neurol, doi:10.1016/S1474-4422(21)00182-4
Yang, SARS-CoV-2 infecAon causes dopaminergic neuron senescence, Cell Stem Cell, doi:10.1016/j.stem.2023.12.012
Yu, Travaglio, Popovic, Leal, Marans, Alzheimer's and Parkinson's Diseases Predict Different COVID-19 Outcomes: A UK Biobank Study, Geriatrics, doi:10.3390/geriatrics6010010
Zheng, COVID-19 treatments and pathogenesis including anosmia in K18-hACE2 mice, Nature, doi:10.1038/s41586-020-2943-z
DOI record:
{
"DOI": "10.1101/2024.06.02.596989",
"URL": "http://dx.doi.org/10.1101/2024.06.02.596989",
"abstract": "<jats:title>Abstract</jats:title><jats:p>Post-Acute Sequelae of COVID-19 (PASC) encompasses persistent neurological symptoms, including olfactory and autonomic dysfunction. Here, we report chronic neurological dysfunction in mice infected with a virulent mouse-adapted SARS-CoV-2 that does not infect the brain. Long after recovery from nasal infection, we observed loss of tyrosine hydroxylase (TH) expression in olfactory bulb glomeruli and neurotransmitter levels in the substantia nigra (SN) persisted. Vulnerability of dopaminergic neurons in these brain areas was accompanied by increased levels of proinflammatory cytokines and neurobehavioral changes. RNAseq analysis unveiled persistent microglia activation, as found in human neurodegenerative diseases. Early treatment with antivirals (nirmatrelvir and molnupiravir) reduced virus titers and lung inflammation but failed to prevent neurological abnormalities, as observed in patients. Together these results show that chronic deficiencies in neuronal function in SARS-CoV-2-infected mice are not directly linked to ongoing olfactory epithelium dysfunction. Rather, they bear similarity with neurodegenerative disease, the vulnerability of which is exacerbated by chronic inflammation.</jats:p>",
"accepted": {
"date-parts": [
[
2024,
6,
3
]
]
},
"author": [
{
"affiliation": [],
"family": "Verma",
"given": "Abhishek Kumar",
"sequence": "first"
},
{
"affiliation": [],
"family": "Lowery",
"given": "Shea",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lin",
"given": "Li-Chin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Duraisami",
"given": "Eazhisaivallabi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abrahante Lloréns",
"given": "Juan E.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Qiu",
"given": "Qiang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hefti",
"given": "Marco",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yu",
"given": "C. Ron",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7855-3455",
"affiliation": [],
"authenticated-orcid": false,
"family": "Albers",
"given": "Mark W.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Perlman",
"given": "Stanley",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
6,
4
]
],
"date-time": "2024-06-04T05:30:20Z",
"timestamp": 1717479020000
},
"deposited": {
"date-parts": [
[
2024,
6,
7
]
],
"date-time": "2024-06-07T11:18:31Z",
"timestamp": 1717759111000
},
"group-title": "Microbiology",
"indexed": {
"date-parts": [
[
2024,
6,
8
]
],
"date-time": "2024-06-08T00:30:36Z",
"timestamp": 1717806636822
},
"institution": [
{
"name": "bioRxiv"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
6,
3
]
]
},
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2024.06.02.596989",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2024,
6,
3
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2024,
6,
3
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference": [
{
"DOI": "10.1001/jama.2020.2648",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.1"
},
{
"DOI": "10.1001/jama.2020.4326",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.2"
},
{
"DOI": "10.1016/S1474-4422(20)30221-0",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.3"
},
{
"DOI": "10.1097/CCE.0000000000000290",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.4"
},
{
"DOI": "10.1001/jamanetworkopen.2021.12131",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.5"
},
{
"DOI": "10.1016/S1474-4422(21)00182-4",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.6"
},
{
"DOI": "10.1002/hed.26279",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.7"
},
{
"DOI": "10.1016/S2589-7500(21)00115-1",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.8"
},
{
"DOI": "10.1001/jamaneurol.2020.1127",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.9"
},
{
"DOI": "10.1371/journal.pone.0278214",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.10"
},
{
"DOI": "10.1136/jnnp-2020-323522",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.11"
},
{
"DOI": "10.1111/jon.12819",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.12"
},
{
"DOI": "10.25122/jml-2022-0167",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.13"
},
{
"DOI": "10.1212/NXI.0000000000001146",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.14"
},
{
"DOI": "10.7861/clinmed.2020-0896",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.15"
},
{
"DOI": "10.1016/j.autneu.2021.102872",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.16"
},
{
"DOI": "10.1007/s00213-020-05644-3",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.17"
},
{
"DOI": "10.1038/s41591-022-02001-z",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.18"
},
{
"DOI": "10.1001/jamanetworkopen.2023.42741",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.19"
},
{
"DOI": "10.1111/joim.13209",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.20"
},
{
"DOI": "10.1001/jamanetworkopen.2021.15352",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.21"
},
{
"DOI": "10.1016/j.cell.2022.06.008",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.22"
},
{
"DOI": "10.1002/acn3.51498",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.23"
},
{
"DOI": "10.1001/jamanetworkopen.2022.13253",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.24"
},
{
"DOI": "10.1126/scitranslmed.3003492",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.25"
},
{
"DOI": "10.3390/geriatrics6010010",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.26"
},
{
"DOI": "10.1186/s40035-023-00337-1",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.27"
},
{
"DOI": "10.3389/fnagi.2022.821235",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.28"
},
{
"DOI": "10.1001/jamapsychiatry.2022.3614",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.29"
},
{
"DOI": "10.1172/jci.insight.160277",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.30"
},
{
"DOI": "10.1016/j.cell.2021.10.027",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.31"
},
{
"DOI": "10.1016/j.bbi.2020.06.032",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.32"
},
{
"DOI": "10.1101/2020.06.14.20131128",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.33"
},
{
"DOI": "10.1038/s41423-023-01119-5",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.34"
},
{
"DOI": "10.1038/s41586-022-04569-5",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.35"
},
{
"DOI": "10.3390/diagnostics13101716",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.36"
},
{
"DOI": "10.1093/brain/awac270",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.37"
},
{
"DOI": "10.3390/v14040776",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.38"
},
{
"DOI": "10.1016/0306-4522(90)90389-L",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.39"
},
{
"DOI": "10.1002/ana.410260107",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.40"
},
{
"DOI": "10.1016/S1474-4422(17)30123-0",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.41"
},
{
"DOI": "10.1016/j.jns.2009.08.042",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.42"
},
{
"DOI": "10.1016/j.nbd.2011.10.026",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.43"
},
{
"DOI": "10.1007/s11910-996-0018-7",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.44"
},
{
"DOI": "10.1016/j.ecoenv.2023.115565",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.45"
},
{
"DOI": "10.3201/eid1201.051442",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.46"
},
{
"DOI": "10.1016/j.mehy.2009.12.012",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.47"
},
{
"DOI": "10.1016/s0140-6736(82)90820-0",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.48"
},
{
"DOI": "10.1038/s41586-022-04630-3",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.49"
},
{
"DOI": "10.1016/0306-4522(90)90018-Y",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.50"
},
{
"DOI": "10.1016/0165-0173(94)90007-8",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.51"
},
{
"DOI": "10.1038/s41467-021-27657-y",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.52"
},
{
"DOI": "10.1007/bf02741387",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.53"
},
{
"DOI": "10.1038/nrdp.2017.13",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.54"
},
{
"DOI": "10.2174/187152712800792794",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.55"
},
{
"DOI": "10.1111/febs.14607",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.56"
},
{
"DOI": "10.2174/1871527313666140917121132",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.57"
},
{
"DOI": "10.1038/npjparkd.2016.1",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.58"
},
{
"DOI": "10.1093/brain/awn323",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.59"
},
{
"DOI": "10.1016/S1474-4422(20)30308-2",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.60"
},
{
"DOI": "10.1016/S0014-2999(03)01272-X",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.61"
},
{
"DOI": "10.1038/s41467-021-26513-3",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.62"
},
{
"DOI": "10.1038/s41586-020-2943-z",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.63"
},
{
"DOI": "10.1002/mds.27502",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.64"
},
{
"DOI": "10.3390/brainsci12040430",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.65"
},
{
"DOI": "10.1007/s00234-020-02554-1",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.66"
},
{
"DOI": "10.1007/s00415-023-11561-0",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.67"
},
{
"DOI": "10.1172/JCI172659",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.68"
},
{
"DOI": "10.1016/j.celrep.2022.111573",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.69"
},
{
"DOI": "10.3389/fneur.2022.908081",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.70"
},
{
"DOI": "10.1111/bpa.12997",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.71"
},
{
"DOI": "10.1016/j.ebiom.2022.103999",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.72"
},
{
"DOI": "10.1038/s41598-022-09731-7",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.73"
},
{
"DOI": "10.1016/j.stem.2023.12.012",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.74"
},
{
"DOI": "10.1016/j.cell.2023.09.013",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.75"
},
{
"DOI": "10.1016/j.idcr.2022.e01388",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.76"
},
{
"DOI": "10.3390/brainsci12040456",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.77"
},
{
"DOI": "10.1038/s41598-023-46912-4",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.78"
},
{
"DOI": "10.1002/jmv.29333",
"doi-asserted-by": "publisher",
"key": "2024060704150675000_2024.06.02.596989v1.79"
}
],
"reference-count": 79,
"references-count": 79,
"relation": {},
"resource": {
"primary": {
"URL": "http://biorxiv.org/lookup/doi/10.1101/2024.06.02.596989"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"subtype": "preprint",
"title": "Persistent Neurological Deficits in Mouse PASC Reveal Antiviral Drug Limitations",
"type": "posted-content"
}
verma2