Folic acid and methotrexate use and their association with COVID-19 diagnosis and mortality: a case–control analysis from the UK Biobank
et al., BMJ Open, doi:10.1136/bmjopen-2022-062945, Aug 2022
UK Biobank retrospective showing higher cases and mortality with folic acid supplementation.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
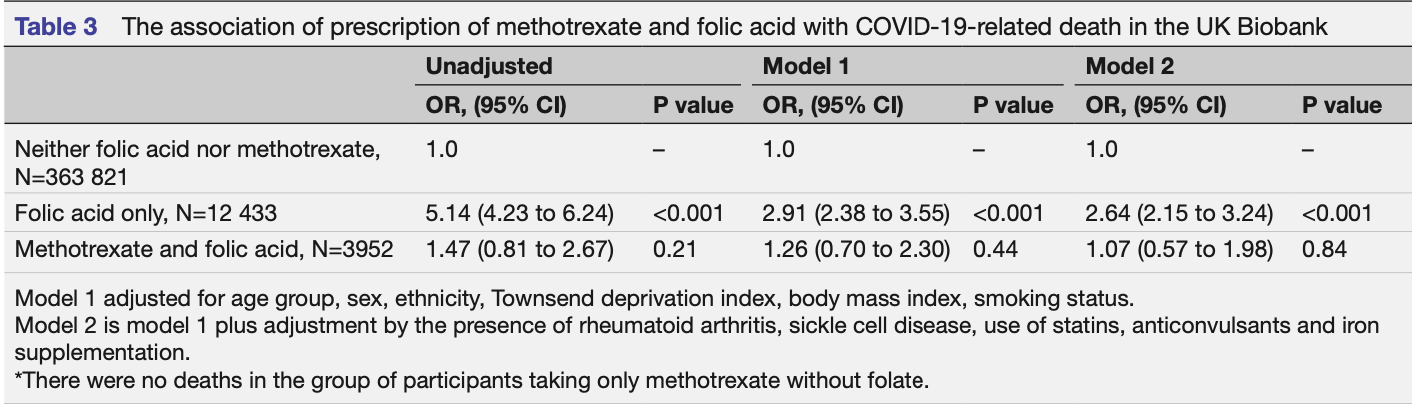
risk of death, 164.0% higher, OR 2.64, p < 0.001, adjusted per study, multivariable, model 2, RR approximated with OR.
|
|
risk of case, 51.0% higher, OR 1.51, p < 0.001, adjusted per study, multivariable, model 2, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Topless et al., 24 Aug 2022, retrospective, United Kingdom, peer-reviewed, 6 authors.
Contact: gaffo@uabmc.e.
Folic acid and methotrexate use and their association with COVID-19 diagnosis and mortality: a case–control analysis from the UK Biobank
BMJ Open, doi:10.1136/bmjopen-2022-062945
Objective To determine if methotrexate or folic acid prescription was associated with differential risk for COVID-19 diagnosis or mortality. Design Case-control analysis. Setting The population-based UK Biobank (UKBB) cohort. Participants Data from 380 380 UKBB participants with general practice prescription data for 2019-2021. Updated medical information was retrieved on 13 December 2021. Primary and secondary outcome measures The outcomes of COVID-19 diagnosis and COVID-19-related mortality were analysed by multivariable logistic regression. Exposures evaluated were prescription of folic acid and/or methotrexate. Criteria for COVID-19 diagnosis were (1) a positive SARS-CoV-2 test or (2) ICD-10 code for confirmed COVID-19 (U07.1) or probable COVID-19 (U07.2) in hospital records, or death records. By these criteria, 26 003 individuals were identified with COVID-19 of whom 820 were known to have died from COVID-19. Logistic regression statistical models were adjusted for age sex, ethnicity, Townsend deprivation index, body mass index, smoking status, presence of rheumatoid arthritis, sickle cell disease, use of anticonvulsants, statins and iron supplements. Results Compared with people prescribed neither folic acid nor methotrexate, people prescribed folic acid supplementation had increased risk of diagnosis of COVID -19 (OR 1.51 (1.42-1.61)). The prescription of methotrexate with or without folic acid was not associated with COVID-19 diagnosis (p≥0.18). People prescribed folic acid supplementation had positive association with death after a diagnosis of COVID-19 (OR 2.64 (2.15-3.24)) in a fully adjusted model. The prescription of methotrexate in combination with folic acid was not associated with an increased risk for COVID-19-related death (1.07 (0.57-1.98)). Conclusions We report an association of increased risk for COVID-19 diagnosis and COVID-19-related death in people prescribed folic acid supplementation. Our results also suggest that methotrexate might attenuate these associations.
Competing interests PR reports personal fees from Abbvie, Atom Biosciences, Eli Lilly, Gilead, Janssen, Novartis, UCB, Roche, Pfizer; meeting attendance support from BMS, Pfizer and UCB Pharma and grant funding from Janssen, Novartis, Pfizer and UCB Pharma, all outside the submitted work. ALG reports personal fees from SOBI, Selecta and honoraria from UptoDate, outside the submitted work. Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication Not applicable. Ethics approval This study involves human participants. The UK Biobank Resource (approval number 12611) was undertaken with ethical approval from the North West Multi-Centre Research Ethics Committee of the UK. This study was done under this ethical approval; researchers using the UK Biobank do not require separate ethical approval. The study complies with the Declaration of Helsinki and written informed consent was obtained from all participants. Participants gave informed consent to participate in the study before taking part. Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement Data are available in a public, open access repository. Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations..
References
Choi, Nguyen, Niu, Selection bias in rheumatic disease research, Nat Rev Rheumatol, doi:10.1038/nrrheum.2014.36
Davies, Jarvis, Increased mortality in community-tested cases of SARS-CoV-2 lineage B.1.1.7, Nature, doi:10.1038/s41586-021-03426-1
Dixit, Nettem, Madan, Folate supplementation in people with sickle cell disease, Cochrane Database Syst Rev, doi:10.2139/ssrn.3297902
Girelli, Marchi, Busti, Iron metabolism in infections: focus on COVID-19, Semin Hematol, doi:10.1053/j.seminhematol.2021.07.001
Gonciarz, Renslo, Melgar-Talavera, Ángel, Emerging role of ferrous iron in bacterial growth and host-pathogen interaction: New tools for chemical (micro)biology and antibacterial therapy, Curr Opin Chem Biol, doi:10.1016/j.atherosclerosis.2021.06.911
Green, Miller, Folate deficiency beyond megaloblastic anemia: hyperhomocysteinemia and other manifestations of dysfunctional folate status, Semin Hematol
Itelman, Wasserstrum, Segev, Clinical characterization of 162 COVID-19 patients in Israel: preliminary report from a large tertiary center, Isr Med Assoc J
Linnebank, Moskau, Semmler, American College of rheumatology guideline for the treatment of rheumatoid arthritis, Arthritis Rheumatol, doi:10.1002/art.41752
Maruvada, Stover, Mason, Knowledge gaps in understanding the metabolic and clinical effects of excess folates/ folic acid: a summary, and perspectives, from an NIH workshop, Am J Clin Nutr, doi:10.1093/ajcn/nqaa259
Morgan, Baggott, Vaughn, Factors associated with COVID-19-related death in people with rheumatic diseases: results from the COVID-19 global rheumatology alliance physician-reported registry, Arthritis Rheum, doi:10.1136/annrheumdis-2020-219498
Morgan, Baggott, Vaughn, Supplementation with folic acid during methotrexate therapy for rheumatoid arthritis. A double-blind, placebo-controlled trial, Ann Intern Med, doi:10.7326/0003-4819-121-11-199412010-00002
Schäfer, Strangfeld, Hyrich, Response to: 'Correspondence on 'Factors associated with COVID-19-related death in people with rheumatic diseases: results from the COVID-19 Global Rheumatology Alliance physician reported registry'' by Mulhearn et, Ann Rheum Dis, doi:10.1136/annrheumdis-2021-220134
Serseg, Benarous, Yousfi, Hispidin and Lepidine E: Two Natural Compounds and Folic Acid as Potential Inhibitors of 2019-novel Coronavirus Main Protease (2019-nCoVM pro ), Molecular Docking and SAR Study, Curr Comput Aided Drug Des, doi:10.2174/1573409916666200422075440
Stegmann, Dickmanns, Gerber, The folate antagonist methotrexate diminishes replication of the coronavirus SARS-CoV-2 and enhances the antiviral efficacy of remdesivir in cell culture models, Virus Res, doi:10.1016/j.virusres.2021.198469
Sudlow, Gallacher, Allen, Uk Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age, Epilepsy Behav, doi:10.1016/j.yebeh.2005.05.020
Thaker, Ch'ng, Hr, Viral hijacking of cellular metabolism, BMC Biol, doi:10.1186/s12915-019-0678-9
Wald, Morris, Blakemore, Public health failure in the prevention of neural tube defects: time to abandon the tolerable upper intake level of folate, Public Health Rev, doi:10.1186/s40985-018-0079-6
Wee, COVID-19's toll on the elderly and those with diabetes mellitus -Is vitamin B12 deficiency an accomplice?, Med Hypotheses, doi:10.1016/j.mehy.2020.110374
Zhang, Guo, Kim, SARS-CoV-2 hijacks folate and onecarbon metabolism for viral replication, doi:10.1038/s41467-021-21903-z
DOI record:
{
"DOI": "10.1136/bmjopen-2022-062945",
"ISSN": [
"2044-6055",
"2044-6055"
],
"URL": "http://dx.doi.org/10.1136/bmjopen-2022-062945",
"abstract": "<jats:sec><jats:title>Objective</jats:title><jats:p>To determine if methotrexate or folic acid prescription was associated with differential risk for COVID-19 diagnosis or mortality.</jats:p></jats:sec><jats:sec><jats:title>Design</jats:title><jats:p>Case–control analysis.</jats:p></jats:sec><jats:sec><jats:title>Setting</jats:title><jats:p>The population-based UK Biobank (UKBB) cohort.</jats:p></jats:sec><jats:sec><jats:title>Participants</jats:title><jats:p>Data from 380 380 UKBB participants with general practice prescription data for 2019–2021. Updated medical information was retrieved on 13 December 2021.</jats:p></jats:sec><jats:sec><jats:title>Primary and secondary outcome measures</jats:title><jats:p>The outcomes of COVID-19 diagnosis and COVID-19-related mortality were analysed by multivariable logistic regression. Exposures evaluated were prescription of folic acid and/or methotrexate. Criteria for COVID-19 diagnosis were (1) a positive SARS-CoV-2 test or (2) ICD-10 code for confirmed COVID-19 (U07.1) or probable COVID-19 (U07.2) in hospital records, or death records. By these criteria, 26 003 individuals were identified with COVID-19 of whom 820 were known to have died from COVID-19. Logistic regression statistical models were adjusted for age sex, ethnicity, Townsend deprivation index, body mass index, smoking status, presence of rheumatoid arthritis, sickle cell disease, use of anticonvulsants, statins and iron supplements.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Compared with people prescribed neither folic acid nor methotrexate, people prescribed folic acid supplementation had increased risk of diagnosis of COVID-19 (OR 1.51 (1.42–1.61)). The prescription of methotrexate with or without folic acid was not associated with COVID-19 diagnosis (p≥0.18). People prescribed folic acid supplementation had positive association with death after a diagnosis of COVID-19 (OR 2.64 (2.15–3.24)) in a fully adjusted model. The prescription of methotrexate in combination with folic acid was not associated with an increased risk for COVID-19-related death (1.07 (0.57–1.98)).</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>We report an association of increased risk for COVID-19 diagnosis and COVID-19-related death in people prescribed folic acid supplementation. Our results also suggest that methotrexate might attenuate these associations.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/bmjopen-2022-062945"
],
"author": [
{
"affiliation": [],
"family": "Topless",
"given": "Ruth",
"sequence": "first"
},
{
"affiliation": [],
"family": "Green",
"given": "Ralph",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Morgan",
"given": "Sarah L",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3156-3418",
"affiliation": [],
"authenticated-orcid": false,
"family": "Robinson",
"given": "Philip",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Merriman",
"given": "Tony",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7365-7212",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gaffo",
"given": "Angelo L",
"sequence": "additional"
}
],
"container-title": "BMJ Open",
"container-title-short": "BMJ Open",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2022,
8,
24
]
],
"date-time": "2022-08-24T15:21:52Z",
"timestamp": 1661354512000
},
"deposited": {
"date-parts": [
[
2022,
8,
24
]
],
"date-time": "2022-08-24T15:22:08Z",
"timestamp": 1661354528000
},
"indexed": {
"date-parts": [
[
2023,
3,
21
]
],
"date-time": "2023-03-21T09:53:41Z",
"timestamp": 1679392421686
},
"is-referenced-by-count": 2,
"issue": "8",
"issued": {
"date-parts": [
[
2022,
8
]
]
},
"journal-issue": {
"issue": "8",
"published-online": {
"date-parts": [
[
2022,
8,
24
]
]
},
"published-print": {
"date-parts": [
[
2022,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 23,
"start": {
"date-parts": [
[
2022,
8,
24
]
],
"date-time": "2022-08-24T00:00:00Z",
"timestamp": 1661299200000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjopen-2022-062945",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "e062945",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2022,
8
]
]
},
"published-online": {
"date-parts": [
[
2022,
8,
24
]
]
},
"published-print": {
"date-parts": [
[
2022,
8
]
]
},
"publisher": "BMJ",
"reference": [
{
"key": "2022082408201098000_12.8.e062945.1",
"unstructured": "Department of health and social care UG. Available: https://www.gov.uk/government/news/folic-acid-added-to-flour-to-prevent-spinal-conditions-in-babies [Accessed 01 Nov 2022]."
},
{
"article-title": "Folate supplementation in people with sickle cell disease",
"author": "Dixit",
"first-page": "CD011130",
"journal-title": "Cochrane Database Syst Rev",
"key": "2022082408201098000_12.8.e062945.2",
"volume": "3",
"year": "2018"
},
{
"DOI": "10.1002/ana.22229",
"doi-asserted-by": "publisher",
"key": "2022082408201098000_12.8.e062945.3"
},
{
"DOI": "10.1002/art.41752",
"article-title": "2021 American College of rheumatology guideline for the treatment of rheumatoid arthritis",
"author": "Fraenkel",
"doi-asserted-by": "crossref",
"first-page": "1108",
"journal-title": "Arthritis Rheumatol",
"key": "2022082408201098000_12.8.e062945.4",
"volume": "73",
"year": "2021"
},
{
"DOI": "10.7326/0003-4819-121-11-199412010-00002",
"doi-asserted-by": "publisher",
"key": "2022082408201098000_12.8.e062945.5"
},
{
"DOI": "10.1002/art.1780330102",
"doi-asserted-by": "publisher",
"key": "2022082408201098000_12.8.e062945.6"
},
{
"DOI": "10.1136/annrheumdis-2020-219498",
"doi-asserted-by": "publisher",
"key": "2022082408201098000_12.8.e062945.7"
},
{
"article-title": "SARS-CoV-2 hijacks folate and one-carbon metabolism for viral replication",
"author": "Zhang",
"journal-title": "Nat Commun",
"key": "2022082408201098000_12.8.e062945.8",
"volume": "12",
"year": "2021"
},
{
"key": "2022082408201098000_12.8.e062945.9",
"unstructured": "Apply for access. Available: https://www.ukbiobank.ac.uk/enable-your-research/apply-for-access [Accessed 22 June 2022]."
},
{
"DOI": "10.1371/journal.pmed.1001779",
"doi-asserted-by": "publisher",
"key": "2022082408201098000_12.8.e062945.10"
},
{
"DOI": "10.1016/j.yebeh.2005.05.020",
"doi-asserted-by": "publisher",
"key": "2022082408201098000_12.8.e062945.11"
},
{
"DOI": "10.1053/j.seminhematol.2021.07.001",
"article-title": "Iron metabolism in infections: focus on COVID-19",
"author": "Girelli",
"doi-asserted-by": "crossref",
"first-page": "182",
"journal-title": "Semin Hematol",
"key": "2022082408201098000_12.8.e062945.12",
"volume": "58",
"year": "2021"
},
{
"DOI": "10.1016/j.cbpa.2021.01.015",
"article-title": "Emerging role of ferrous iron in bacterial growth and host-pathogen interaction: New tools for chemical (micro)biology and antibacterial therapy",
"author": "Gonciarz",
"doi-asserted-by": "crossref",
"first-page": "170",
"journal-title": "Curr Opin Chem Biol",
"key": "2022082408201098000_12.8.e062945.13",
"volume": "61",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2021.08.004",
"article-title": "Statins reduce mortality in patients with COVID-19: an updated meta-analysis of 147 824 patients",
"author": "Diaz-Arocutipa",
"doi-asserted-by": "crossref",
"first-page": "374",
"journal-title": "Int J Infect Dis",
"key": "2022082408201098000_12.8.e062945.14",
"volume": "110",
"year": "2021"
},
{
"DOI": "10.1016/j.atherosclerosis.2021.06.911",
"article-title": "Statin use and mortality in COVID-19 patients: updated systematic review and meta-analysis",
"author": "Kollias",
"doi-asserted-by": "crossref",
"first-page": "114",
"journal-title": "Atherosclerosis",
"key": "2022082408201098000_12.8.e062945.15",
"volume": "330",
"year": "2021"
},
{
"DOI": "10.1038/s41586-021-03426-1",
"article-title": "Increased mortality in community-tested cases of SARS-CoV-2 lineage B.1.1.7",
"author": "Davies",
"doi-asserted-by": "crossref",
"first-page": "270",
"journal-title": "Nature",
"key": "2022082408201098000_12.8.e062945.16",
"volume": "593",
"year": "2021"
},
{
"DOI": "10.1186/s12915-019-0678-9",
"doi-asserted-by": "publisher",
"key": "2022082408201098000_12.8.e062945.17"
},
{
"DOI": "10.1016/j.virusres.2021.198469",
"article-title": "The folate antagonist methotrexate diminishes replication of the coronavirus SARS-CoV-2 and enhances the antiviral efficacy of remdesivir in cell culture models",
"author": "Stegmann",
"doi-asserted-by": "crossref",
"journal-title": "Virus Res",
"key": "2022082408201098000_12.8.e062945.18",
"volume": "302",
"year": "2021"
},
{
"article-title": "Folate deficiency beyond megaloblastic anemia: hyperhomocysteinemia and other manifestations of dysfunctional folate status",
"author": "Green",
"first-page": "47",
"journal-title": "Semin Hematol",
"key": "2022082408201098000_12.8.e062945.19",
"volume": "36",
"year": "1999"
},
{
"article-title": "Clinical characterization of 162 COVID-19 patients in Israel: preliminary report from a large tertiary center",
"author": "Itelman",
"first-page": "271",
"journal-title": "Isr Med Assoc J",
"key": "2022082408201098000_12.8.e062945.20",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1038/nrrheum.2014.36",
"doi-asserted-by": "publisher",
"key": "2022082408201098000_12.8.e062945.21"
},
{
"DOI": "10.1016/j.mehy.2020.110374",
"doi-asserted-by": "publisher",
"key": "2022082408201098000_12.8.e062945.22"
},
{
"DOI": "10.2174/1573409916666200422075440",
"article-title": "Hispidin and Lepidine E: Two Natural Compounds and Folic Acid as Potential Inhibitors of 2019-novel Coronavirus Main Protease (2019- nCoVM\n pro\n ), Molecular Docking and SAR Study",
"author": "Serseg",
"doi-asserted-by": "crossref",
"first-page": "469",
"journal-title": "Curr Comput Aided Drug Des",
"key": "2022082408201098000_12.8.e062945.23",
"volume": "17",
"year": "2021"
},
{
"DOI": "10.1136/annrheumdis-2021-220134",
"article-title": "Response to: 'Correspondence on 'Factors associated with COVID-19-related death in people with rheumatic diseases: results from the COVID-19 Global Rheumatology Alliance physician reported registry'' by Mulhearn et al",
"author": "Schäfer",
"doi-asserted-by": "crossref",
"journal-title": "Ann Rheum Dis",
"key": "2022082408201098000_12.8.e062945.24",
"year": "2021"
},
{
"DOI": "10.1186/s40985-018-0079-6",
"doi-asserted-by": "publisher",
"key": "2022082408201098000_12.8.e062945.25"
},
{
"DOI": "10.1093/ajcn/nqaa259",
"doi-asserted-by": "publisher",
"key": "2022082408201098000_12.8.e062945.26"
}
],
"reference-count": 26,
"references-count": 26,
"relation": {},
"resource": {
"primary": {
"URL": "https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2022-062945"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Folic acid and methotrexate use and their association with COVID-19 diagnosis and mortality: a case–control analysis from the UK Biobank",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "12"
}