Neurological sequelae of long COVID: a comprehensive review of diagnostic imaging, underlying mechanisms, and potential therapeutics
et al., Frontiers in Neurology, doi:10.3389/fneur.2024.1465787, Feb 2025
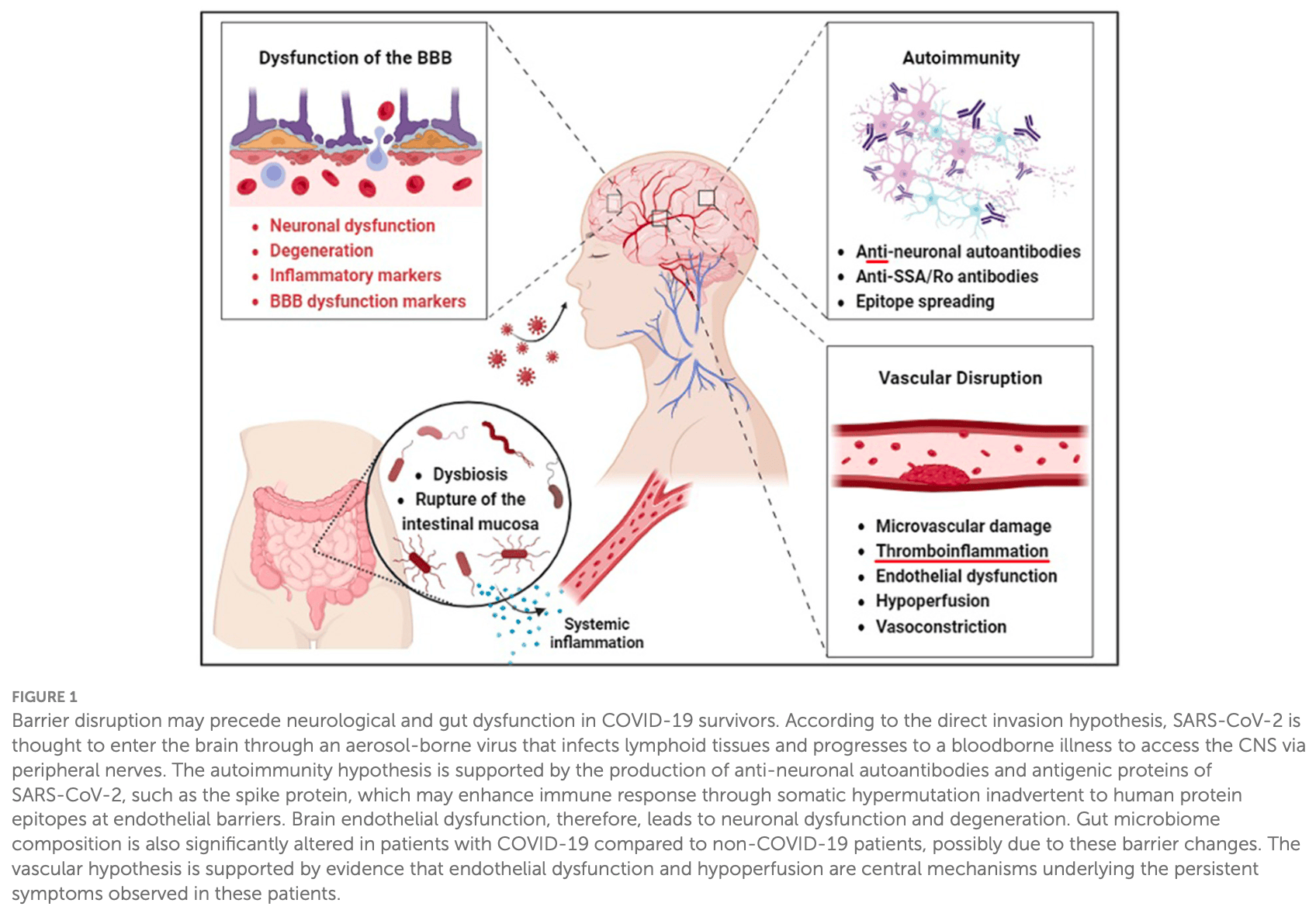
Review of neurological sequelae of long COVID (LC), focusing on cognitive dysfunction, diagnostic tools, underlying mechanisms, and potential therapeutic approaches. The authors examine how long COVID can cause chronic insomnia, fatigue, mood disorders, and cognitive impairments. Several mechanistic hypotheses are explored, including CNS invasion, neuroinflammation, blood-brain barrier disruption, gut-brain axis dysregulation, and vascular disruption.
Talkington et al., 7 Feb 2025, peer-reviewed, 19 authors.
Contact: gbix@tulane.edu.
Neurological sequelae of long COVID: a comprehensive review of diagnostic imaging, underlying mechanisms, and potential therapeutics
One lingering e ect of the COVID-pandemic created by SARS-CoV-is the emergence of Long COVID (LC), characterized by enduring neurological sequelae a ecting a significant portion of survivors. This review provides a thorough analysis of these neurological disruptions with respect to cognitive dysfunction, which broadly manifest as chronic insomnia, fatigue, mood dysregulation, and cognitive impairments with respect to cognitive dysfunction. Furthermore, we characterize how diagnostic tools such as PET, MRI, EEG, and ultrasonography provide critical insight into subtle neurological anomalies that may mechanistically explain the Long COVID disease phenotype. In this review, we explore the mechanistic hypotheses of these neurological changes, which describe CNS invasion, neuroinflammation, blood-brain barrier disruption, and gut-brain axis dysregulation, along with the novel vascular disruption hypothesis that highlights endothelial dysfunction and hypoperfusion as a core underlying mechanism. We lastly evaluate the clinical treatment landscape, scrutinizing the e cacy of various therapeutic strategies ranging from antivirals to antiinflammatory agents in mitigating the multifaceted symptoms of LC.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Afrin, Weinstock, Molderings, Covid-19 hyperinflammation and post-Covid-19 illness may be rooted in mast cell activation syndrome, Int J Infect Dis, doi:10.1016/j.ijid.2020.09.016
Ajčević, Iscra, Furlanis, Michelutti, Miladinović et al., Cerebral hypoperfusion in post-COVID-19 cognitively impaired subjects revealed by arterial spin labeling MRI, Sci Rep, doi:10.1038/s41598-023-32275-3
Alqedari, Altabtbaei, Espinoza, Bin-Hasan, Alghounaim et al., Host-Microbiome Associations in Saliva Predict COVID-19 Severity. bioRxiv
Antony, Haneef, Systematic review of EEG findings in 617 patients diagnosed with COVID-19, Seizure, doi:10.1016/j.seizure.2020.10.014
Arbour, Day, Newcombe, Talbot, Neuroinvasion by human respiratory coronaviruses, J Virol, doi:10.1128/JVI.74.19.8913-8921.2000
Arun, Storan, Myers, Mast cell activation syndrome and the link with long COVID, Br J Hosp Med, doi:10.12968/hmed.2022.0123
Asadi-Pooya, Akbari, Emami, Lotfi, Rostamihosseinkhani et al., Long COVID syndrome-associated brain fog, J Med Virol, doi:10.1002/jmv.27404
Azcue, Gomez-Esteban, Acera, Tijero, Fernandez et al., Brain fog of post-COVID-19 condition and Chronic Fatigue Syndrome, same medical disorder?, J Transl Med, doi:10.1186/s12967-022-03764-2
Batiha, Al-Kuraishy, Gareeb, Welson, Pathophysiology of post-COVID syndromes: a new perspective, Virology J, doi:10.1186/s12985-022-01891-2
Becker, Lin, Doernberg, Stone, Navis et al., Assessment of cognitive function in patients after COVID-19 infection, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.30645
Bird, Low serotonin linked to long COVID, Nat Rev Immunol, doi:10.1038/s41577-023-00966-7
Blackett, Sun, Purpura, Margolis, Elkind et al., Decreased gut microbiome tryptophan metabolism and serotonergic signaling in patients with persistent mental health and gastrointestinal symptoms after COVID-19, Clin Transl Gastroenterol, doi:10.1155/2021/2911578
Bohmwald, Gálvez, Ríos, Kalergis, Neurologic alterations due to respiratory virus infections, Front Cell Neurosci, doi:10.3389/fncel.2018.00386
Bonometti, Sacchi, Stobbione, Lauritano, Tamiazzo et al., The first case of systemic lupus erythematosus (SLE) triggered by COVID-19 infection, Eur Rev Med Pharmacol Sci, doi:10.1111/ijd.15257
Boufidou, Medić, Lampropoulou, Siafakas, Tsakris et al., SARS-CoV-2 reinfections and long COVID in the post-omicron phase of the pandemic, Int J Mol Sci, doi:10.3390/ijms241612962
Butler, Pollak, Rooney, Michael, Nicholson, Neuropsychiatric complications of covid-19, BMJ, doi:10.1136/bmj.m3871
Caroppo, Mazza, Sannella, Marano, Avallone et al., Will nothing be the same again?: Changes in lifestyle during COVID-19 pandemic and consequences on mental health, Int J Environ Res Public Health, doi:10.3390/ijerph18168433
Cecchetti, Agosta, Canu, Basaia, Barbieri et al., Cognitive, EEG, and MRI features of COVID-19 survivors: a 10-month study, J Neurol, doi:10.1007/s00415-022-11047-5
Chen, Burgt, Smit, Audhoe, Boer et al., Investigating the potential added value of [18 F]FDG-PET/CT in long COVID patients with persistent symptoms: a proof of concept study, Nucl Med Commun, doi:10.1093/rheumatology/keab247.053
Chen, Yang, Chen, Cui, COVID-19 and cognitive impairment: neuroinvasive and blood-brain barrier dysfunction, J Neuroinflamm, doi:10.1186/s12974-022-02579-8
Chenchula, Ray, Sadasivam, Famotidine repurposing for novel corona virus disease of 2019: a systematic review, Drug Res, doi:10.1055/a-1397-6763
Cheng, Anderson, Didehbani, Fine, Fleming et al., Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of mental health symptoms in patients with post-acute sequelae of SARS-CoV-2 infection (PASC), PM R, doi:10.1002/pmrj.13085
Clemente, Rocca, Quaranta, Iannuzzi, Vecchio et al., Prefrontal dysfunction in post-COVID-19 hyposmia: an EEG/fNIRS study, Front Hum Neurosci, doi:10.3389/fnhum.2023.1240831
Combes, Courau, Kuhn, Hu, Ray et al., Global absence and targeting of protective immune states in severe COVID-19, Nature, doi:10.1038/s41586-021-03234-7
Davis, Assaf, Mccorkell, Wei, Low et al., Characterizing long COVID in an international cohort: 7 months of symptoms and their impact, EClinicalMedicine, doi:10.1016/j.eclinm.2021.101019
Davis, Mccorkell, Vogel, Topol, Long COVID: major findings, mechanisms and recommendations, Nat Rev Microbiol, doi:10.1038/s41579-022-00846-2
Destras, Bal, Escuret, Morfin, Lina et al., Systematic SARS-CoV-2 screening in cerebrospinal fluid during the COVID-19 pandemic, Lancet Microbe, doi:10.1016/S2666-5247(20)30066-5
Disner, Beevers, Haigh, Neural mechanisms of the cognitive model of depression, Nat Rev Neurosci, doi:10.1038/nrn3027
Dixit, Churchill, Nsair, Hsu, Post-acute COVID-19 syndrome and the cardiovascular system: what is known?, Am Heart J Plus, doi:10.1016/j.ahjo.2021.100025
Dos, Miggiolaro, Covid-19 cytokine storm in pulmonary tissue: Anatomopathological and immunohistochemical findings, Respir Med Case Rep, doi:10.1016/j.rmcr.2020.101292
Durstenfeld, Peluso, Lin, Peyser, Isasi et al., Effect of 12 mg vs 6 mg of dexamethasone on the number of days alive without life support in adults with COVID-19 and severe hypoxemia: The COVID STEROID 2 randomized trial, Clin Microbiol Infect, doi:10.1001/jama.2021.18295
Escher, Breakey, Lämmle, Aird, Phenotypic heterogeneity of the endothelium: II. Representative vascular beds, Thromb Res, doi:10.1161/01.RES.0000255690.03436.ae
Fajgenbaum, June, Cytokine storm, N Engl J Med, doi:10.1056/NEJMra2026131
Fancourt, Steptoe, Bu, Psychological consequences of long COVID: comparing trajectories of depressive and anxiety symptoms before and after contracting SARS-CoV-2 between matched long-and short-COVID groups, Br J Psychiatry, doi:10.1192/bjp.2022.155
Fernandez-De-Las-Penas, Gomez-Mayordomo, De-La-Llave-Rincon, Palacios-Cena, Rodriguez-Jimenez et al., Anxiety, depression and poor sleep quality as long-term post-COVID sequelae in previously hospitalized patients: a multicenter study, J Infect, doi:10.1016/j.jinf.2021.06.022
Ford, Slaughter, Edwards, Long COVID and significant activity limitation among adults, by age -United States, June 1-13, 2022 to, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm7232a3
Frontera, Yang, Lewis, Patel, Medicherla et al., prospective study of long-term outcomes among hospitalized COVID-19 patients with and without neurological complications, J Neurol Sci, doi:10.1016/j.jns.2021.117486
Fry, Logemann, Waldron, Holker, Porter et al., Emotional functioning in long COVID: comparison to post-concussion syndrome using the Personality Assessment Inventory, Clin Neuropsychol, doi:10.1080/13854046.2023.2264546
Furlanis, Stella, Biaduzzini, Bellavita, Frezza et al., Cognitive deficit in post-acute COVID-19: an opportunity for EEG evaluation?, Neurol Sci, doi:10.1007/s10072-023-06615-0
Fusco, Lorenzo, Cintoni, Porcari, Rinninella et al., Shortchain fatty-acid-producing bacteria: key components of the human gut microbiota, Nutrients, doi:10.3390/nu15092211
Giron, Peluso, Ding, Kenny, Zilberstein et al., Markers of fungal translocation are elevated during post-acute sequelae of SARS-CoV-2 and induce NF-κB signaling, JCI Insight, doi:10.1172/jci.insight.160989
Giustino, Pinney, Reddy, Johnston-Cox, Mechanick, Coronavirus and cardiovascular disease, myocardial injury, and arrhythmia: JACC focus seminar, J Am Coll Cardiol, doi:10.1016/j.jacc.2020.08.059
Glynne, Tahmasebi, Gant, Gupta, Long COVID following mild SARS-CoV-2 infection: characteristic T cell alterations and response to antihistamines, J Investig Med, doi:10.1136/jim-2021-002051
Gorna, Macdermott, Rayner, Hara, Evans et al., Long COVID guidelines need to reflect lived experience, Lancet, doi:10.1016/S0140-6736(20)32705-7
Greene, Connolly, Brennan, Laffan, 'keeffe et al., Blood-brain barrier disruption in Long COVID-associated cognitive impairment, doi:10.21203/rs.3.rs-2069710/v2
Grobbelaar, Venter, Vlok, Ngoepe, Laubscher et al., SARS-CoV-2 spike protein S1 induces fibrin(ogen) resistant to fibrinolysis: implications for microclot formation in COVID-19, Biosci Rep, doi:10.1042/BSR20210611
Guedj, Campion, Dudouet, Kaphan, Bregeon et al., Neuropathophysiology of coronavirus disease 2019: neuroinflammation and blood brain barrier disruption are critical pathophysiological processes that contribute to the clinical symptoms of SARS-CoV-2 infection, Eur J Nucl Med Mol Imaging, doi:10.1007/s10787-021-00806-x
Guo, Briese, Ranjan, Allicock, Yates, Deficient butyrate-producing capacity in the gut microbiome is associated with bacterial network disturbances and fatigue symptoms in ME/CFS, Cell Host Microbe, doi:10.3390/cells11071239
Góralczyk-Bińkowska, Szmajda-Krygier, Kozłowska, The microbiota-gut-brain axis in psychiatric disorders, Int J Mol Sci, doi:10.3390/ijms231911245
Haidar, Jourdi, Hassan, Ashekyan, Fardoun et al., Neurological and neuropsychological changes associated with SARS-CoV-2 infection: new observations, new mechanisms, Neuroscientist, doi:10.1177/1073858420984106
Hellgren, Thornberg, Samuelsson, Levi, Divanoglou et al., Brain MRI and neuropsychological findings at long-term follow-up after COVID-19 hospitalisation: an observational cohort study, BMJ Open, doi:10.1136/bmjopen-2021-055164
Houben-Wilke, Goertz, Delbressine, Vaes, Meys et al., The impact of long COVID-19 on mental health: observational 6-month follow-up study, JMIR Ment Health, doi:10.2196/33704
Huang, Huang, Wang, Li, Ren et al., 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study, Lancet, doi:10.1016/S0140-6736(23)01175-3
Huang, Ling, Manyande, Wu, Xiang, Brain imaging changes in patients recovered from COVID-19: a narrative review, Front Neurosci, doi:10.3389/fnins.2022.855868
Hugon, Msika, Queneau, Farid, Paquet, Long COVID: cognitive complaints (brain fog) and dysfunction of the cingulate cortex, J Neurol, doi:10.1007/s00415-021-10655-x
Ikeda, Nishida, Yamano, Kimura, Andrade et al., Long-COVID and post-COVID health complications. An upto-date review on clinical conditions and their possible molecular mechanisms viruses, Pharmacol Ther, doi:10.3390/v13040700
Iosef, Knauer, Nicholson, Van Nynatten, Cepinskas et al., Plasma proteome of Long-COVID patients indicates HIF-mediated vasculoproliferative disease with impact on brain and heart function, J Transl Med, doi:10.1186/s12967-023-04149-9
Jana, Greenwood, Hansmann, Presence of a SARS-COV-2 protein enhances Amyloid Formation of Serum Amyloid A, J Phys Chem B, doi:10.1021/acs.jpcb.1c04871
Jung, Helbok, Matschke, Krasemann, Altmeppen et al., NeuroCOVID: insights into neuroinvasion and pathophysiology, Clini Transl Neurosci, doi:10.3390/ctn6020010
Kao, Frankland, Covid, fog demystified, Cell, doi:10.1016/j.cell.2022.06.020
Karaman, Leppänen, Alitalo, Talotta, Impaired VEGF-A-mediated neurovascular crosstalk induced by SARS-CoV-2 spike protein: a potential hypothesis explaining long COVID-19 symptoms and COVID-19 vaccine side effects? Microorganisms, Development, doi:10.3390/microorganisms10122452
Kazantseva, Enikeeva, Takhirova, Davydova, Mustafin et al., Host genetic variants linked to COVID-19 neurological complications and susceptibility in young adults-A preliminary analysis, J Pers Med, doi:10.3390/jpm13010123
Kempuraj, Aenlle, Cohen, Mathew, Isler et al., COVID-19 and long COVID: disruption of the neurovascular unit, blood-brain barrier, and tight junctions, Neuroscientist, doi:10.1177/10738584231194927
Khatoon, Prasad, Kumar, COVID-19 associated nervous system manifestations, Sleep Med, doi:10.1016/j.sleep.2021.07.005
Klein, Wood, Jaycox, Dhodapkar, Lu et al., Distinguishing features of long COVID identified through immune profiling, Nature, doi:10.1038/s41586-023-06651-y
Kreye, Reincke, Prüss, Do cross-reactive antibodies cause neuropathology in COVID-19?, Nat Rev Immunol, doi:10.1038/s41577-020-00458-y
Krishnan, Lin, Prewitt, Potter, Multidisciplinary approach to brain fog and related persisting symptoms post COVID-19, J Health Serv Psychol, doi:10.1007/s42843-022-00056-7
Lammi, Nakanishi, Jones, Andrews, Karjalainen et al., Genome-wide association study of long COVID, medRxiv, doi:10.1101/2023.06.29.23292056v1
Leng, Shah, Ahmad, Premraj, Wildi et al., Pathogenesis underlying neurological manifestations of long COVID syndrome and potential therapeutics, Cells, doi:10.3390/cells12050816
Li, Li, Wen, Zhang, Cao, Coronavirus infections in the central nervous system and respiratory tract show distinct features in hospitalized children, Intervirology, doi:10.1159/000453066
Li, Yang, Morrisey, Foxp4: A novel member of the Foxp subfamily of winged-helix genes co-expressed with Foxp1 and Foxp2 in pulmonary and gut tissues, Gene Expression Patt, doi:10.1016/S1567-133X(02)00058-3
Lipton, Ischemic cell death in brain neurons, Physiol Rev, doi:10.1152/physrev.1999.79.4.1431
Logarbo, Yang, Longo, Kingry, Courseault, Long COVID and the diagnosis of underlying hypermobile Ehlers-Danlos syndrome and hypermobility spectrum disorders, PM & R, doi:10.1002/pmrj.13120
Ma, Zhang, Zhou, Li, Ge et al., Metagenomic analysis reveals oropharyngeal microbiota alterations in patients with COVID-19, Signal Transduct Target Ther, doi:10.1038/s41392-021-00614-3
Magnus, Gunnes, Tveito, Bakken, Ghaderi et al., Chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) is associated with pandemic influenza infection, but not with an adjuvanted pandemic influenza vaccine, Vaccine, doi:10.1016/j.vaccine.2015.10.018
Maloney, Gao, Proinflammatory cytokines increase vascular endothelial growth factor expression in alveolar epithelial cells, Mediators Inflamm, doi:10.1155/2015/387842
Marcic, Marcic, Kojundzic, Guic, Marcic et al., Chronic endothelial dysfunction after COVID-19 infection shown by transcranial color-coded doppler: a cross-sectional study, Biomedicines, doi:10.3390/biomedicines10102550
Marizzoni, Cattaneo, Mirabelli, Festari, Lopizzo et al., Short-chain fatty acids and lipopolysaccharide as mediators between gut dysbiosis and amyloid pathology in Alzheimer's disease, J Alzheimers Dis
Mayer, Nance, Chen, The gut-brain axis, Annu Rev Med, doi:10.1146/annurev-med-042320-014032
Mcquaid, Brady, Deane, SARS-CoV-2: is there neuroinvasion? Fluids Barriers CNS, doi:10.1186/s12987-021-00267-y
Mekhael, Lim, Hajjar, Noujaim, Pottle et al., Studying the effect of long COVID-19 infection on sleep quality using wearable health devices: observational study, J Med Internet Res, doi:10.2196/38000
Mendez, Balanza-Martinez, Luperdi, Estrada, Latorre et al., Long-term neuropsychiatric outcomes in COVID-19 survivors: a 1-year longitudinal study, J Intern Med, doi:10.1111/joim.13389
Mohiuddin, Alexander, Holcomb, Alexander, Plotkin et al., Cerebral Vasomotor Reactivity Testing in the Middle Cerebral Artery Using Transcranial Doppler to Assess Brain Dysregulation in Long-haul COVID Patients
Mohseni, Raissi, Sharifan, Barikro, Amiri et al., Therapeutic status of famotidine in COVID-19 patients: a review, Infect Disord Drug Targets, doi:10.2174/1871526522666220107125511
Moldofsky, Patcai, Komaroff, Lipkin, Vm et al., Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study, Trends Mol Med, doi:10.1016/j.molmed.2021.06.002
Moller, Borg, Janson, Lerm, Normark et al., Cognitive dysfunction in post-COVID-19 condition: Mechanisms, management, and rehabilitation, J Intern Med, doi:10.1111/joim.13720
Monastero, Baschi, Persistent cognitive dysfunction in a non-hospitalized covid-19 long-hauler patient responding to cognitive rehabilitation and citicoline treatment, Brain Sci, doi:10.3390/brainsci13091275
Monje, Iwasaki, The neurobiology of long COVID, Neuron, doi:10.1016/j.neuron.2022.10.006
Moriguchi, Harii, Goto, Harada, Sugawara et al., A first case of meningitis/encephalitis associated with SARS-Coronavirus-2, Int J Infect Dis, doi:10.1016/j.ijid.2020.03.062
Moura, Oliveira, Torres, Tavares-Junior, Nobrega et al., Central hypersomnia and chronic insomnia: expanding the spectrum of sleep disorders in long COVID syndrome -a prospective cohort study, BMC Neurol, doi:10.1186/s12883-022-02940-7
Mourad, Thibault, Holland, Yang, Young et al., Modafinil: a review and its potential use in the treatment of long COVID fatigue and neurocognitive deficits, Am J Psychiatry Resid, doi:10.1176/appi.ajp-rj.2022.170402
Murphy, MRI Scans Show COVID's 'Significant' Impact on the Brain
Palacio-Toro, Hernández-Botero, Duque-Montoya, Osorio, Echeverry et al., Acute meningoencephalitis associated with SARS-CoV-2 infection in Colombia, J Neurovirol, doi:10.1007/s13365-021-01023-6
Patel, Knauer, Nicholson, Daley, Nynatten et al., critical analysis of SARS-CoV-2 (COVID-19) complexities, emerging variants, and therapeutic interventions and vaccination strategies, Cold Spring Harb Perspect Biol, doi:10.1155/2021/7880448
Patel, Reddy, Shumway, Araujo, Physiology, Sleep Stages
Peluso, Sans, Forman, Nylander, Ho et al., Plasma markers of neurologic injury and inflammation in people with selfreported neurologic postacute sequelae of SARS-CoV-2 infection, Neurology, doi:10.1212/NXI.0000000000200003
Perego, Callard, Stras, Melville-Jóhannesson, Pope et al., Why the patient-made term 'Long Covid' is needed, Wellcome Open Res, doi:10.12688/wellcomeopenres.16307.1
Perlman, Evans, Afifi, Effect of olfactory bulb ablation on spread of a neurotropic coronavirus into the mouse brain, J Exp Med, doi:10.1084/jem.172.4.1127
Philippe, Günther, Rancic, Cavagna, Renaud et al., VEGF-A plasma levels are associated with impaired DLCO and radiological sequelae in long COVID patients, Angiogenesis, doi:10.1007/s10456-023-09890-9
Premraj, Kannapadi, Briggs, Seal, Battaglini et al., Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: a meta-analysis, J Neurol Sci, doi:10.1016/j.jns.2022.120162
Pretorius, Vlok, Venter, Bezuidenhout, Laubscher et al., Persistent clotting protein pathology in Long COVID/post-acute sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin, Cardiovasc Diabetol, doi:10.1186/s12933-021-01359-7
Pszczołowska, Walczak, Misków, Antosz, Batko et al., Molecular cross-talk between long COVID-19 and Alzheimer's disease, GeroScience, doi:10.1007/s11357-024-01096-1
Reese, Blau, Casiraghi, Bergquist, Loomba et al., Generalisable long COVID subtypes: findings from the NIH N3C and RECOVER programmes, EBioMedicine, doi:10.1016/j.ebiom.2022.104413
Reinders, Sho, Izawa, Wang, Mukhopadhyay et al., Proinflammatory functions of vascular endothelial growth factor in alloimmunity, J Clin Invest, doi:10.1172/JCI17712
Reyes, Stovall, Punyamurthula, Longo, Maraganore et al., The impact of gut microbiome and diet on post-acute sequelae of SARS-CoV-2 infection, J Neurol Sci, doi:10.1016/j.jns.2024.123295
Richter, Schulze, James, Siems, Trampe et al., Hypoechogenicity of brainstem raphe in long-COVID syndrome-less common but independently associated with depressive symptoms: a cross-sectional study, J Neurol, doi:10.1007/s00415-022-11154-3
Rousso, Pearson, Gaber, Miquelajauregui, Li et al., Foxp-mediated suppression of N-cadherin regulates neuroepithelial character and progenitor maintenance in the CNS, Neuron, doi:10.1016/j.neuron.2012.02.024
Saltzman, Longo, Hansel, Long-COVID stress symptoms: Mental health, anxiety, depression, or posttraumatic stress, Psychol Trauma, doi:10.1037/tra0001567
Salvucci, Codella, Coppola, Zacchei, Grassi et al., Antihistamines improve cardiovascular manifestations and other symptoms of long-COVID attributed to mast cell activation, Front Cardiovasc Med, doi:10.3389/fcvm.2023.1202696
Savytskyi, Pruc, Malysz, Maslyukov, Szarpak, Post-COVID-19 postural orthostatic tachycardia syndrome, Cardiol J, doi:10.5603/CJ.a2022.0021
Scott, Webb, James, Rowse, Weich, Improving sleep quality leads to better mental health: a meta-analysis of randomised controlled trials, Sleep Med Rev, doi:10.1016/j.smrv.2021.101556
Shafiee, Athar, Amini, Hajishah, Siahvoshi et al., The role of the neutral amino acid transporter B0AT1 (SLC6A19) in Hartnup disorder and protein nutrition, Rev Med Virol, doi:10.1186/s12877-020-01644-2
Shiraliyeva, Chen, Azimi-Nekoo, Kishore, FRI463 A Case Of Post COVID-19 Subacute Thyroiditis: A Thyroid Equivalent Of Long COVID?, J Endocr Soc, doi:10.1210/jendso/bvad114.1810
Sollini, Morbelli, Ciccarelli, Cecconi, Aghemo et al., Long COVID hallmarks on [18F]FDG-PET/CT: a case-control study, Eur J Nucl Med Mol Imaging, doi:10.1007/s00259-021-05294-3
Sonka, Susta, Diagnosis and management of central hypersomnias, Ther Adv Neurol Disord, doi:10.1177/1756285612454692
Subotički, Ajtić, Živković, Diklić, Ðikić et al., vegf regulation of angiogenic factors via inflammatory signaling in myeloproliferative neoplasms, Int J Mol Sci, doi:10.3390/ijms22136671
Sumantri, Rengganis, Immunological dysfunction and mast cell activation syndrome in long COVID, Asia Pac Allergy, doi:10.5415/apallergy.0000000000000022
Sun, Yao, Kim, Tall, Ferreira et al., Effectiveness of Paxlovid in reducing severe Coronavirus disease 2019 and mortality in high-Risk Patients, Infect Genet Evol, doi:10.1093/cid/ciac443
Suran, Long COVID linked with unemployment in new analysis, JAMA, doi:10.1001/jama.2023.0157
Swanson, Mcgavern, Viral diseases of the central nervous system, Curr Opin Virol, doi:10.1016/j.coviro.2014.12.009
Sykes, Holdsworth, Jawad, Gunasekera, Morice et al., Post-COVID-19 symptom burden: what is long-COVID and how should we manage it?, Lung, doi:10.1007/s00408-021-00423-z
Takahashi, Liu, Hirokawa, Takahashi, Expression of Foxp4 in the developing and adult rat forebrain, J Neurosci Res, doi:10.1038/s41586-021-03767-x
Tam, Leung, Tong, Kwan, Foxp4 is essential in maintenance of Purkinje cell dendritic arborization in the mouse cerebellum, Neuroscience, doi:10.1016/j.neuroscience.2010.10.023
Taquet, Dercon, Luciano, Geddes, Hussain et al., Incidence, co-occurrence, and evolution of long-COVID features: a 6-month retrospective cohort study of 273,618 survivors of COVID-19, PLoS Med, doi:10.1371/journal.pmed.1003773
Tarasev, Ferranti, Allen, Gao, Topping et al., Lanetta Bronté-Hall, Patrick Hines; whole blood adhesion to VCAM-1 and P-selectin and RBC mechanical fragility can be compromised in long covid-19 patients with sickle cell disease, Blood, doi:10.1182/blood-2021-154308
Thaweethai, Jolley, Karlson, Levitan, Levy et al., Development of a definition of postacute sequelae of SARS-CoV-2 infection, JAMA, doi:10.1001/jama.2023.8823
Theoharides, Cholevas, Polyzoidis, Politis, Long-COVID syndromeassociated brain fog and chemofog: Luteolin to the rescue, Biofactors, doi:10.1002/biof.1726
Theoharides, Conti, COVID-19, and multisystem inflammatory syndrome, or is it mast cell activation syndrome?, J Biol Regul Homeost Agents, doi:10.23812/20-EDIT3
Thornton, Fraioli, Wan, Garthwaite, Ganeshan et al., Evolution of (18)F-FDG PET/CT findings in patients after COVID-19: an initial investigation, J Nucl Med, doi:10.2967/jnumed.121.262296
Vasilev, Blokhin, Khoruzhaya, Kodenko, Kolyshenkov et al., Routine brain MRI findings on the long-term effects of COVID-19: a scoping review, Diagnostics, doi:10.3390/diagnostics13152533
Viso, Zhou, Thiffault, Lawson, Cross et al., Recurrent FOXP4 nonsense variant in two unrelated patients: association with neurodevelopmental disease and congenital diaphragmatic hernia, Am J Med Genet A, doi:10.1002/ajmg.a.63006
Wang, Yu, Jing, Wu, Novakovic et al., Long COVID: the nature of thrombotic sequelae determines the necessity of early anticoagulation, Front Cell Infect Microbiol, doi:10.2174/1570161111311020005
Weinstock, Mast cell activation symptoms are prevalent in Long-COVID, Int J Infect Dis, doi:10.1016/j.ijid.2021.09.043
Wong, Devason, Umana, Cox, Dohnalová et al., Serotonin reduction in post-acute sequelae of viral infection, Cell, doi:10.1016/j.cell.2023.09.013
Wong, Weitzer, Long COVID and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)-a systemic review and comparison of clinical presentation and symptomatology, Medicina, doi:10.3390/medicina57050418
Woodburn, Bollinger, Wohleb, The semantics of microglia activation: neuroinflammation, homeostasis, and stress, J Neuroinflammation, doi:10.1186/s12974-021-02309-6
Woodruff, Ramonell, Nguyen, Cashman, Saini et al., Extrafollicular B cell responses correlate with neutralizing antibodies and morbidity in COVID-19, Nat Immunol, doi:10.1038/s41590-020-00814-z
Wu, SARS-CoV-2-triggered mast cell rapid degranulation induces alveolar epithelial inflammation and lung injury, Signal Transduct Target Ther, doi:10.1038/s41392-021-00849-0
Wölfel, Corman, Guggemos, Virological assessment of hospitalized patients with COVID-2019, Nature, doi:10.1038/s41586-020-2196-x
Xiang, Jing, Wang, Novakovic, Shi, Persistent Lung Injury and Prothrombotic State in Long COVID, Front Immunol, doi:10.3389/fimmu.2022.862522
Xiang, Wu, Jing, Novakovic, Shi, The intersection of obesity and (long) COVID-19: hypoxia, thrombotic inflammation, and vascular endothelial injury, Front Cardiovasc Med, doi:10.3389/fcvm.2023.1062491
Xu, Gao, Xia, Chen, Zeng et al., Rapid gut dysbiosis induced by stroke exacerbates brain infarction in turn, Gut, doi:10.1136/gutjnl-2020-323263
Xu, Ilyas, Weng, Endothelial dysfunction in COVID-19: an overview of evidence, biomarkers, mechanisms and potential therapies, Acta Pharmacol Sin, doi:10.1038/s41401-022-00998-0
Xu, Li, Zhu, Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding, Nat Med, doi:10.1038/s41591-020-0817-4
Xu, Xie, Al-Aly, Long-term neurologic outcomes of COVID-19, Nat Med, doi:10.1038/s41591-022-02001-z
Yeh, Collins, Cohen, Duffner, Faden, Detection of coronavirus in the central nervous system of a child with acute disseminated encephalomyelitis, Pediatrics, doi:10.1542/peds.113.1.e73
Yeoh, Zuo, Lui, Zhang, Liu et al., Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19, Gut, doi:10.1136/gutjnl-2020-323020
Yiannopoulou, Vakrakou, Anastasiou, Nikolopoulou, Sourdi et al., Cerebrospinal fluid anti-neuronal autoantibodies in COVID-19-associated limbic encephalitis with acute cerebellar ataxia and myoclonus syndrome: case report and literature review, Diagnostics, doi:10.3390/diagnostics13122055
Yin, Peluso, Luo, Thomas, Shin et al., Long COVID manifests with T cell dysregulation, inflammation, and an uncoordinated adaptive immune response to SARS-CoV-2. bioRxiv
Zachariah, Nair, Goel, Balasubramanian, Mackie et al., Targeting raised von Willebrand levels and macrophage activation in severe COVID-19: Consider low volume plasma exchange and low dose steroid, Thromb Res, doi:10.1016/j.thromres.2020.05.001
Zhao, Huang, Huang, Liu, Shao et al., Prevalence of NSAID use among people with COVID-19 and the association with COVID-19related outcomes: Systematic review and meta-analysis, Br J Clin Pharmacol, doi:10.1111/bcp.15512
Zhou, Han, Chen, Hou, Hua et al., Clinical and autoimmune characteristics of severe and critical cases of COVID-19, Clin Transl Sci, doi:10.1111/cts.12805
Zn, Mj, St, Lp, Rg, Navigating immunosuppression in a pandemic: A guide for the dermatologist from the COVID Task Force of the Medical Dermatology Society and Society of Dermatology Hospitalists, J Am Acad Dermatol, doi:10.1016/j.jaad.2020.06.051
Zuo, Estes, Ali, Gandhi, Yalavarthi et al., Prothrombotic autoantibodies in serum from patients hospitalized with COVID-19, Sci Transl Med, doi:10.1126/scitranslmed.abd3876
DOI record:
{
"DOI": "10.3389/fneur.2024.1465787",
"ISSN": [
"1664-2295"
],
"URL": "http://dx.doi.org/10.3389/fneur.2024.1465787",
"abstract": "<jats:p>One lingering effect of the COVID-19 pandemic created by SARS-CoV-2 is the emergence of Long COVID (LC), characterized by enduring neurological sequelae affecting a significant portion of survivors. This review provides a thorough analysis of these neurological disruptions with respect to cognitive dysfunction, which broadly manifest as chronic insomnia, fatigue, mood dysregulation, and cognitive impairments with respect to cognitive dysfunction. Furthermore, we characterize how diagnostic tools such as PET, MRI, EEG, and ultrasonography provide critical insight into subtle neurological anomalies that may mechanistically explain the Long COVID disease phenotype. In this review, we explore the mechanistic hypotheses of these neurological changes, which describe CNS invasion, neuroinflammation, blood-brain barrier disruption, and gut-brain axis dysregulation, along with the novel vascular disruption hypothesis that highlights endothelial dysfunction and hypoperfusion as a core underlying mechanism. We lastly evaluate the clinical treatment landscape, scrutinizing the efficacy of various therapeutic strategies ranging from antivirals to anti-inflammatory agents in mitigating the multifaceted symptoms of LC.</jats:p>",
"alternative-id": [
"10.3389/fneur.2024.1465787"
],
"author": [
{
"affiliation": [],
"family": "Talkington",
"given": "Grant McGee",
"sequence": "first"
},
{
"affiliation": [],
"family": "Kolluru",
"given": "Paresh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gressett",
"given": "Timothy E.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ismael",
"given": "Saifudeen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Meenakshi",
"given": "Umar",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Acquarone",
"given": "Mariana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Solch-Ottaiano",
"given": "Rebecca J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "White",
"given": "Amanda",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ouvrier",
"given": "Blake",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Paré",
"given": "Kristina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Parker",
"given": "Nicholas",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Watters",
"given": "Amanda",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Siddeeque",
"given": "Nabeela",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sullivan",
"given": "Brooke",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ganguli",
"given": "Nilesh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Calero-Hernandez",
"given": "Victor",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hall",
"given": "Gregory",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Longo",
"given": "Michele",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bix",
"given": "Gregory J.",
"sequence": "additional"
}
],
"container-title": "Frontiers in Neurology",
"container-title-short": "Front. Neurol.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2025,
2,
7
]
],
"date-time": "2025-02-07T05:10:46Z",
"timestamp": 1738905046000
},
"deposited": {
"date-parts": [
[
2025,
2,
19
]
],
"date-time": "2025-02-19T15:31:45Z",
"timestamp": 1739979105000
},
"indexed": {
"date-parts": [
[
2025,
2,
19
]
],
"date-time": "2025-02-19T16:10:02Z",
"timestamp": 1739981402303,
"version": "3.37.3"
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2025,
2,
7
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
2,
7
]
],
"date-time": "2025-02-07T00:00:00Z",
"timestamp": 1738886400000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fneur.2024.1465787/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2025,
2,
7
]
]
},
"published-online": {
"date-parts": [
[
2025,
2,
7
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1016/j.sleep.2021.07.005",
"article-title": "COVID-19 associated nervous system manifestations",
"author": "Khatoon",
"doi-asserted-by": "publisher",
"first-page": "231",
"journal-title": "Sleep Med.",
"key": "B1",
"volume": "91",
"year": "2022"
},
{
"DOI": "10.1038/s41579-022-00846-2",
"article-title": "Long COVID: major findings, mechanisms and recommendations",
"author": "Davis",
"doi-asserted-by": "publisher",
"first-page": "133",
"journal-title": "Nat Rev Microbiol.",
"key": "B2",
"volume": "21",
"year": "2023"
},
{
"DOI": "10.15585/mmwr.mm7232a3",
"article-title": "Long COVID and significant activity limitation among adults, by age — United States, June 1–13, 2022 to June 7–19",
"author": "Ford",
"doi-asserted-by": "publisher",
"first-page": "866",
"journal-title": "MMWR Morb Mortal Wkly Rep.",
"key": "B3",
"volume": "72",
"year": "2023"
},
{
"DOI": "10.3390/ijms241612962",
"article-title": "SARS-CoV-2 reinfections and long COVID in the post-omicron phase of the pandemic",
"author": "Boufidou",
"doi-asserted-by": "publisher",
"first-page": "12962",
"journal-title": "Int J Mol Sci.",
"key": "B4",
"volume": "24",
"year": "2023"
},
{
"DOI": "10.1016/j.ebiom.2022.104413",
"article-title": "Generalisable long COVID subtypes: findings from the NIH N3C and RECOVER programmes",
"author": "Reese",
"doi-asserted-by": "publisher",
"first-page": "104413",
"journal-title": "EBioMedicine.",
"key": "B5",
"volume": "87",
"year": "2023"
},
{
"DOI": "10.1016/j.jns.2021.117486",
"article-title": "prospective study of long-term outcomes among hospitalized COVID-19 patients with and without neurological complications",
"author": "Frontera",
"doi-asserted-by": "publisher",
"first-page": "117486",
"journal-title": "J Neurol Sci.",
"key": "B6",
"volume": "426",
"year": "2021"
},
{
"DOI": "10.12688/wellcomeopenres.16307.1",
"article-title": "Why the patient-made term ‘Long Covid’ is needed",
"author": "Perego",
"doi-asserted-by": "publisher",
"first-page": "224",
"journal-title": "Wellcome Open Res.",
"key": "B7",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1001/jama.2023.8823",
"article-title": "Development of a definition of postacute sequelae of SARS-CoV-2 infection",
"author": "Thaweethai",
"doi-asserted-by": "publisher",
"first-page": "1934",
"journal-title": "JAMA.",
"key": "B8",
"volume": "329",
"year": "2023"
},
{
"DOI": "10.1371/journal.pmed.1003773",
"article-title": "Incidence, co-occurrence, and evolution of long-COVID features: a 6-month retrospective cohort study of 273,618 survivors of COVID-19",
"author": "Taquet",
"doi-asserted-by": "publisher",
"first-page": "e1003773",
"journal-title": "PLoS Med.",
"key": "B9",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1136/bmj.m3871",
"article-title": "Neuropsychiatric complications of covid-19",
"author": "Butler",
"doi-asserted-by": "publisher",
"journal-title": "BMJ.",
"key": "B10",
"year": ""
},
{
"DOI": "10.1016/S0140-6736(20)32705-7",
"article-title": "Long COVID guidelines need to reflect lived experience",
"author": "Gorna",
"doi-asserted-by": "publisher",
"first-page": "455",
"journal-title": "Lancet.",
"key": "B11",
"volume": "397",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.30645",
"article-title": "Assessment of cognitive function in patients after COVID-19 infection",
"author": "Becker",
"doi-asserted-by": "publisher",
"first-page": "e2130645",
"journal-title": "JAMA Netw Open.",
"key": "B12",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1186/s12883-022-02940-7",
"article-title": "Central hypersomnia and chronic insomnia: expanding the spectrum of sleep disorders in long COVID syndrome - a prospective cohort study",
"author": "Moura",
"doi-asserted-by": "publisher",
"first-page": "417",
"journal-title": "BMC Neurol.",
"key": "B13",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1177/1756285612454692",
"article-title": "Diagnosis and management of central hypersomnias",
"author": "Sonka",
"doi-asserted-by": "publisher",
"first-page": "297",
"journal-title": "Ther Adv Neurol Disord.",
"key": "B14",
"volume": "5",
"year": "2012"
},
{
"DOI": "10.2196/38000",
"article-title": "Studying the effect of long COVID-19 infection on sleep quality using wearable health devices: observational study",
"author": "Mekhael",
"doi-asserted-by": "publisher",
"first-page": "e38000",
"journal-title": "J Med Internet Res.",
"key": "B15",
"volume": "24",
"year": "2022"
},
{
"article-title": "Physiology, Sleep Stages",
"author": "Patel",
"key": "B16",
"volume-title": "StatPearls",
"year": "2024"
},
{
"DOI": "10.1016/j.smrv.2021.101556",
"article-title": "Improving sleep quality leads to better mental health: a meta-analysis of randomised controlled trials",
"author": "Scott",
"doi-asserted-by": "publisher",
"first-page": "101556",
"journal-title": "Sleep Med Rev.",
"key": "B17",
"volume": "60",
"year": "2021"
},
{
"DOI": "10.1186/s12974-022-02579-8",
"article-title": "COVID-19 and cognitive impairment: neuroinvasive and blood–brain barrier dysfunction",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "222",
"journal-title": "J Neuroinflamm.",
"key": "B18",
"volume": "19",
"year": "2022"
},
{
"DOI": "10.1037/tra0001567",
"article-title": "Long-COVID stress symptoms: Mental health, anxiety, depression, or posttraumatic stress",
"author": "Saltzman",
"doi-asserted-by": "publisher",
"first-page": "1169",
"journal-title": "Psychol Trauma.",
"key": "B19",
"volume": "16",
"year": "2024"
},
{
"DOI": "10.1111/joim.13389",
"article-title": "Long-term neuropsychiatric outcomes in COVID-19 survivors: a 1-year longitudinal study",
"author": "Mendez",
"doi-asserted-by": "publisher",
"first-page": "247",
"journal-title": "J Intern Med.",
"key": "B20",
"volume": "291",
"year": "2022"
},
{
"DOI": "10.1192/bjp.2022.155",
"article-title": "Psychological consequences of long COVID: comparing trajectories of depressive and anxiety symptoms before and after contracting SARS-CoV-2 between matched long- and short-COVID groups",
"author": "Fancourt",
"doi-asserted-by": "publisher",
"first-page": "74",
"journal-title": "Br J Psychiatry.",
"key": "B21",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.2196/33704",
"article-title": "The impact of long COVID-19 on mental health: observational 6-month follow-up study",
"author": "Houben-Wilke",
"doi-asserted-by": "publisher",
"first-page": "e33704",
"journal-title": "JMIR Ment Health.",
"key": "B22",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1007/s00408-021-00423-z",
"article-title": "Post-COVID-19 symptom burden: what is long-COVID and how should we manage it?",
"author": "Sykes",
"doi-asserted-by": "publisher",
"first-page": "113",
"journal-title": "Lung.",
"key": "B23",
"volume": "199",
"year": "2021"
},
{
"DOI": "10.1016/j.jinf.2021.06.022",
"article-title": "Anxiety, depression and poor sleep quality as long-term post-COVID sequelae in previously hospitalized patients: a multicenter study",
"author": "Fernandez-de-Las-Penas",
"doi-asserted-by": "publisher",
"first-page": "496",
"journal-title": "J Infect",
"key": "B24",
"volume": "83",
"year": "2021"
},
{
"DOI": "10.1007/s42843-022-00056-7",
"article-title": "Multidisciplinary approach to brain fog and related persisting symptoms post COVID-19",
"author": "Krishnan",
"doi-asserted-by": "publisher",
"first-page": "31",
"journal-title": "J Health Serv Psychol.",
"key": "B25",
"volume": "48",
"year": "2022"
},
{
"DOI": "10.1186/s12967-022-03764-2",
"article-title": "Brain fog of post-COVID-19 condition and Chronic Fatigue Syndrome, same medical disorder?",
"author": "Azcue",
"doi-asserted-by": "publisher",
"first-page": "569",
"journal-title": "J Transl Med.",
"key": "B26",
"volume": "20",
"year": "2022"
},
{
"DOI": "10.1002/biof.1726",
"article-title": "Long-COVID syndrome-associated brain fog and chemofog: Luteolin to the rescue",
"author": "Theoharides",
"doi-asserted-by": "publisher",
"first-page": "232",
"journal-title": "Biofactors.",
"key": "B27",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.1016/j.cell.2022.06.020",
"article-title": "fog demystified",
"author": "Kao",
"doi-asserted-by": "publisher",
"first-page": "2391",
"journal-title": "Cell.",
"key": "B28",
"volume": "185",
"year": "2022"
},
{
"DOI": "10.1002/jmv.27404",
"article-title": "Long COVID syndrome-associated brain fog",
"author": "Asadi-Pooya",
"doi-asserted-by": "publisher",
"first-page": "979",
"journal-title": "J Med Virol.",
"key": "B29",
"volume": "94",
"year": "2022"
},
{
"DOI": "10.5603/CJ.a2022.0021",
"article-title": "Post-COVID-19 postural orthostatic tachycardia syndrome",
"author": "Savytskyi",
"doi-asserted-by": "publisher",
"first-page": "531",
"journal-title": "Cardiol J.",
"key": "B30",
"volume": "29",
"year": "2022"
},
{
"DOI": "10.1016/j.ahjo.2021.100025",
"article-title": "Post-acute COVID-19 syndrome and the cardiovascular system: what is known?",
"author": "Dixit",
"doi-asserted-by": "publisher",
"first-page": "100025",
"journal-title": "Am Heart J Plus.",
"key": "B31",
"volume": "5",
"year": "2021"
},
{
"DOI": "10.1186/s12985-022-01891-2",
"article-title": "Al-kuraishy HM, Al-Gareeb AI, Welson NN. Pathophysiology of post-COVID syndromes: a new perspective",
"author": "Batiha",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Virology J.",
"key": "B32",
"volume": "19",
"year": "2022"
},
{
"DOI": "10.1016/j.ijid.2021.09.043",
"article-title": "Mast cell activation symptoms are prevalent in Long- COVID",
"author": "Weinstock",
"doi-asserted-by": "publisher",
"first-page": "217",
"journal-title": "Int J Infect Dis.",
"key": "B33",
"volume": "112",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2020.09.016",
"article-title": "Covid-19 hyperinflammation and post-Covid-19 illness may be rooted in mast cell activation syndrome",
"author": "Afrin",
"doi-asserted-by": "publisher",
"first-page": "327",
"journal-title": "Int J Infect Dis.",
"key": "B34",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.5415/apallergy.0000000000000022",
"article-title": "Immunological dysfunction and mast cell activation syndrome in long COVID",
"author": "Sumantri",
"doi-asserted-by": "publisher",
"first-page": "50",
"journal-title": "Asia Pac Allergy.",
"key": "B35",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1002/pmrj.13120",
"article-title": "Long COVID and the diagnosis of underlying hypermobile Ehlers-Danlos syndrome and hypermobility spectrum disorders",
"author": "Logarbo",
"doi-asserted-by": "publisher",
"first-page": "935",
"journal-title": "PM & R.",
"key": "B36",
"volume": "16",
"year": "2024"
},
{
"DOI": "10.1080/13854046.2023.2264546",
"article-title": "Emotional functioning in long COVID: comparison to post-concussion syndrome using the Personality Assessment Inventory",
"author": "Fry",
"doi-asserted-by": "publisher",
"first-page": "963",
"journal-title": "Clin Neuropsychol.",
"key": "B37",
"volume": "38",
"year": "2024"
},
{
"DOI": "10.21203/rs.3.rs-2069710/v2",
"author": "Greene",
"doi-asserted-by": "publisher",
"journal-title": "Blood-brain barrier disruption in Long COVID-associated cognitive impairment.",
"key": "B38",
"year": "2022"
},
{
"DOI": "10.1001/jama.2023.0157",
"article-title": "Long COVID linked with unemployment in new analysis",
"author": "Suran",
"doi-asserted-by": "publisher",
"first-page": "701",
"journal-title": "JAMA.",
"key": "B39",
"volume": "329",
"year": "2023"
},
{
"DOI": "10.1016/j.eclinm.2021.101019",
"article-title": "Characterizing long COVID in an international cohort: 7 months of symptoms and their impact",
"author": "Davis",
"doi-asserted-by": "publisher",
"first-page": "101019",
"journal-title": "EClinicalMedicine.",
"key": "B40",
"volume": "38",
"year": "2021"
},
{
"DOI": "10.1111/joim.13720",
"article-title": "Cognitive dysfunction in post-COVID-19 condition: Mechanisms, management, and rehabilitation",
"author": "Moller",
"doi-asserted-by": "publisher",
"first-page": "563",
"journal-title": "J Intern Med.",
"key": "B41",
"volume": "294",
"year": "2023"
},
{
"DOI": "10.1007/s00415-021-10655-x",
"article-title": "Long COVID: cognitive complaints (brain fog) and dysfunction of the cingulate cortex",
"author": "Hugon",
"doi-asserted-by": "publisher",
"first-page": "44",
"journal-title": "J Neurol.",
"key": "B42",
"volume": "269",
"year": "2022"
},
{
"DOI": "10.3389/fnhum.2023.1240831",
"article-title": "Prefrontal dysfunction in post-COVID-19 hyposmia: an EEG/fNIRS study",
"author": "Clemente",
"doi-asserted-by": "publisher",
"first-page": "1240831",
"journal-title": "Front Hum Neurosci.",
"key": "B43",
"volume": "17",
"year": "2023"
},
{
"DOI": "10.3390/ijerph18168433",
"article-title": "Will nothing be the same again?",
"author": "Caroppo",
"doi-asserted-by": "publisher",
"first-page": "16",
"journal-title": "Int J Environ Res Public Health.",
"key": "B44",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.3390/brainsci13091275",
"article-title": "Persistent cognitive dysfunction in a non-hospitalized covid-19 long-hauler patient responding to cognitive rehabilitation and citicoline treatment",
"author": "Monastero",
"doi-asserted-by": "publisher",
"journal-title": "Brain Sci 13:.",
"key": "B45",
"year": "1275"
},
{
"DOI": "10.1007/s00259-021-05294-3",
"article-title": "Long COVID hallmarks on [18F]FDG-PET/CT: a case-control study",
"author": "Sollini",
"doi-asserted-by": "publisher",
"first-page": "3187",
"journal-title": "Eur J Nucl Med Mol Imaging.",
"key": "B46",
"volume": "48",
"year": "2021"
},
{
"DOI": "10.1136/bmjopen-2021-055164",
"article-title": "Brain MRI and neuropsychological findings at long-term follow-up after COVID-19 hospitalisation: an observational cohort study",
"author": "Hellgren",
"doi-asserted-by": "publisher",
"first-page": "10",
"journal-title": "BMJ Open.",
"key": "B47",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.3389/fnins.2022.855868",
"article-title": "Brain imaging changes in patients recovered from COVID-19: a narrative review",
"author": "Huang",
"doi-asserted-by": "publisher",
"first-page": "855868",
"journal-title": "Front Neurosci.",
"key": "B48",
"volume": "16",
"year": "2022"
},
{
"DOI": "10.2967/jnumed.121.262296",
"article-title": "Evolution of (18)F-FDG PET/CT findings in patients after COVID-19: an initial investigation",
"author": "Thornton",
"doi-asserted-by": "publisher",
"first-page": "270",
"journal-title": "J Nucl Med.",
"key": "B49",
"volume": "63",
"year": "2022"
},
{
"DOI": "10.1038/s41591-022-02001-z",
"article-title": "Long-term neurologic outcomes of COVID-19",
"author": "Xu",
"doi-asserted-by": "publisher",
"first-page": "2406",
"journal-title": "Nat Med",
"key": "B50",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.3390/diagnostics13152533",
"article-title": "Routine brain MRI findings on the long-term effects of COVID-19: a scoping review",
"author": "Vasilev",
"doi-asserted-by": "publisher",
"first-page": "2533",
"journal-title": "Diagnostics.",
"key": "B51",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1016/j.seizure.2020.10.014",
"article-title": "Systematic review of EEG findings in 617 patients diagnosed with COVID-19",
"author": "Antony",
"doi-asserted-by": "publisher",
"first-page": "234",
"journal-title": "Seizure.",
"key": "B52",
"volume": "83",
"year": "2020"
},
{
"DOI": "10.1007/s00415-022-11047-5",
"article-title": "Cognitive, EEG, and MRI features of COVID-19 survivors: a 10-month study",
"author": "Cecchetti",
"doi-asserted-by": "publisher",
"first-page": "3400",
"journal-title": "J Neurol.",
"key": "B53",
"volume": "269",
"year": "2022"
},
{
"DOI": "10.1007/s10072-023-06615-0",
"article-title": "Cognitive deficit in post-acute COVID-19: an opportunity for EEG evaluation?",
"author": "Furlanis",
"doi-asserted-by": "publisher",
"first-page": "1491",
"journal-title": "Neurol Sci.",
"key": "B54",
"volume": "44",
"year": "2023"
},
{
"author": "Mohiuddin",
"journal-title": "Cerebral Vasomotor Reactivity Testing in the Middle Cerebral Artery Using Transcranial Doppler to Assess Brain Dysregulation in Long-haul COVID Patients",
"key": "B55",
"year": "2023"
},
{
"DOI": "10.3390/biomedicines10102550",
"article-title": "Chronic endothelial dysfunction after COVID-19 infection shown by transcranial color-coded doppler: a cross-sectional study",
"author": "Marcic",
"doi-asserted-by": "publisher",
"first-page": "2550",
"journal-title": "Biomedicines.",
"key": "B56",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1007/s00415-022-11154-3",
"article-title": "Hypoechogenicity of brainstem raphe in long-COVID syndrome-less common but independently associated with depressive symptoms: a cross-sectional study",
"author": "Richter",
"doi-asserted-by": "publisher",
"first-page": "4604",
"journal-title": "J Neurol.",
"key": "B57",
"volume": "269",
"year": "2022"
},
{
"DOI": "10.1016/S0140-6736(23)01175-3",
"article-title": "6-month consequences of COVID-19 in patients discharged from hospital: a cohort study",
"author": "Huang",
"doi-asserted-by": "publisher",
"first-page": "e21",
"journal-title": "Lancet.",
"key": "B58",
"volume": "401",
"year": "2023"
},
{
"DOI": "10.1038/s41577-023-00966-7",
"article-title": "Low serotonin linked to long COVID",
"author": "Bird",
"doi-asserted-by": "publisher",
"first-page": "784",
"journal-title": "Nat Rev Immunol.",
"key": "B59",
"volume": "23",
"year": "2023"
},
{
"DOI": "10.1038/s41586-023-06651-y",
"article-title": "Distinguishing features of long COVID identified through immune profiling",
"author": "Klein",
"doi-asserted-by": "publisher",
"first-page": "139",
"journal-title": "Nature.",
"key": "B60",
"volume": "623",
"year": "2023"
},
{
"DOI": "10.3390/medicina57050418",
"article-title": "Long COVID and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)-a systemic review and comparison of clinical presentation and symptomatology",
"author": "Wong",
"doi-asserted-by": "publisher",
"first-page": "418",
"journal-title": "Medicina.",
"key": "B61",
"volume": "57",
"year": "2021"
},
{
"DOI": "10.1016/j.coviro.2014.12.009",
"article-title": "Viral diseases of the central nervous system",
"author": "Swanson",
"doi-asserted-by": "publisher",
"first-page": "44",
"journal-title": "Curr Opin Virol",
"key": "B62",
"volume": "1",
"year": "2014"
},
{
"DOI": "10.1084/jem.172.4.1127",
"article-title": "Effect of olfactory bulb ablation on spread of a neurotropic coronavirus into the mouse brain",
"author": "Perlman",
"doi-asserted-by": "publisher",
"first-page": "1127",
"journal-title": "J Exp Med",
"key": "B63",
"volume": "172",
"year": "2020"
},
{
"DOI": "10.3389/fncel.2018.00386",
"article-title": "Neurologic alterations due to respiratory virus infections",
"author": "Bohmwald",
"doi-asserted-by": "publisher",
"first-page": "30416428",
"journal-title": "Front Cell Neurosci.",
"key": "B64",
"volume": "12",
"year": "2018"
},
{
"DOI": "10.1186/s12987-021-00267-y",
"article-title": "SARS-CoV-2: is there neuroinvasion?",
"author": "McQuaid",
"doi-asserted-by": "publisher",
"first-page": "34261487",
"journal-title": "Fluids Barriers CNS.",
"key": "B65",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1128/JVI.74.19.8913-8921.2000",
"article-title": "Neuroinvasion by human respiratory coronaviruses",
"author": "Arbour",
"doi-asserted-by": "publisher",
"first-page": "8913",
"journal-title": "J Virol.",
"key": "B66",
"volume": "74",
"year": "2000"
},
{
"DOI": "10.1159/000453066",
"article-title": "Coronavirus infections in the central nervous system and respiratory tract show distinct features in hospitalized children",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "163",
"journal-title": "Intervirology.",
"key": "B67",
"volume": "59",
"year": "2016"
},
{
"DOI": "10.1542/peds.113.1.e73",
"article-title": "Detection of coronavirus in the central nervous system of a child with acute disseminated encephalomyelitis",
"author": "Yeh",
"doi-asserted-by": "publisher",
"first-page": "2500",
"journal-title": "Pediatrics.",
"key": "B68",
"volume": "113",
"year": "2004"
},
{
"DOI": "10.1016/S2666-5247(20)30066-5",
"article-title": "Systematic SARS-CoV-2 screening in cerebrospinal fluid during the COVID-19 pandemic",
"author": "Destras",
"doi-asserted-by": "publisher",
"first-page": "e149",
"journal-title": "Lancet Microbe.",
"key": "B69",
"volume": "1",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.03.062",
"article-title": "A first case of meningitis/encephalitis associated with SARS-Coronavirus-2",
"author": "Moriguchi",
"doi-asserted-by": "publisher",
"first-page": "55",
"journal-title": "Int J Infect Dis.",
"key": "B70",
"volume": "94",
"year": "2020"
},
{
"DOI": "10.1007/s13365-021-01023-6",
"article-title": "Acute meningoencephalitis associated with SARS-CoV-2 infection in Colombia",
"author": "Palacio-Toro",
"doi-asserted-by": "publisher",
"first-page": "960",
"journal-title": "J Neurovirol.",
"key": "B71",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1177/1073858420984106",
"article-title": "Neurological and neuropsychological changes associated with SARS-CoV-2 infection: new observations, new mechanisms",
"author": "Haidar",
"doi-asserted-by": "publisher",
"first-page": "552",
"journal-title": "Neuroscientist.",
"key": "B72",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1111/cts.12805",
"article-title": "Clinical and autoimmune characteristics of severe and critical cases of COVID-19",
"author": "Zhou",
"doi-asserted-by": "publisher",
"first-page": "1077",
"journal-title": "Clin Transl Sci.",
"key": "B73",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1126/scitranslmed.abd3876",
"article-title": "Prothrombotic autoantibodies in serum from patients hospitalized with COVID-19",
"author": "Zuo",
"doi-asserted-by": "publisher",
"first-page": "570",
"journal-title": "Sci Transl Med.",
"key": "B74",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1038/s41577-020-00458-y",
"article-title": "Do cross-reactive antibodies cause neuropathology in COVID-19?",
"author": "Kreye",
"doi-asserted-by": "publisher",
"first-page": "645",
"journal-title": "Nat Rev Immunol.",
"key": "B75",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1038/s41586-021-03234-7",
"article-title": "Global absence and targeting of protective immune states in severe COVID-19",
"author": "Combes",
"doi-asserted-by": "publisher",
"first-page": "124",
"journal-title": "Nature.",
"key": "B76",
"volume": "591",
"year": "2021"
},
{
"key": "B77",
"unstructured": "Long COVID manifests with T cell dysregulation, inflammation, and an uncoordinated adaptive immune response to SARS-CoV-2\n \n \n \n Yin\n K\n \n \n Peluso\n MJ\n \n \n Luo\n X\n \n \n Thomas\n R\n \n \n Shin\n MG\n \n \n Neidleman\n J\n \n \n bioRxiv\n \n 2023"
},
{
"DOI": "10.3390/diagnostics13122055",
"article-title": "Cerebrospinal fluid anti-neuronal autoantibodies in COVID-19-associated limbic encephalitis with acute cerebellar ataxia and myoclonus syndrome: case report and literature review",
"author": "Yiannopoulou",
"doi-asserted-by": "publisher",
"first-page": "37370950",
"journal-title": "Diagnostics.",
"key": "B78",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1038/s41590-020-00814-z",
"article-title": "Extrafollicular B cell responses correlate with neutralizing antibodies and morbidity in COVID-19",
"author": "Woodruff",
"doi-asserted-by": "publisher",
"first-page": "1506",
"journal-title": "Nat Immunol.",
"key": "B79",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1016/j.rmcr.2020.101292",
"article-title": "Covid-19 cytokine storm in pulmonary tissue: Anatomopathological and immunohistochemical findings",
"author": "Ribeiro Dos Santos Miggiolaro",
"doi-asserted-by": "publisher",
"first-page": "101292",
"journal-title": "Respir Med Case Rep.",
"key": "B80",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1038/s41392-021-00849-0",
"article-title": "SARS-CoV-2-triggered mast cell rapid degranulation induces alveolar epithelial inflammation and lung injury",
"author": "Wu",
"doi-asserted-by": "publisher",
"first-page": "428",
"journal-title": "Signal Transduct Target Ther.",
"key": "B81",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.23812/20-EDIT3",
"article-title": "COVID-19, and multisystem inflammatory syndrome, or is it mast cell activation syndrome?",
"author": "Theoharides",
"doi-asserted-by": "publisher",
"first-page": "1633",
"journal-title": "J Biol Regul Homeost Agents.",
"key": "B82",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.12968/hmed.2022.0123",
"article-title": "Mast cell activation syndrome and the link with long COVID",
"author": "Arun",
"doi-asserted-by": "publisher",
"first-page": "35938771",
"journal-title": "Br J Hosp Med.",
"key": "B83",
"volume": "83",
"year": "2022"
},
{
"DOI": "10.1016/j.jns.2022.120162",
"article-title": "Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: a meta-analysis",
"author": "Premraj",
"doi-asserted-by": "publisher",
"first-page": "120162",
"journal-title": "J Neurol Sci.",
"key": "B84",
"volume": "434",
"year": "2022"
},
{
"DOI": "10.1056/NEJMra2026131",
"article-title": "Cytokine storm",
"author": "Fajgenbaum",
"doi-asserted-by": "publisher",
"first-page": "2255",
"journal-title": "N Engl J Med.",
"key": "B85",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.3390/ctn6020010",
"article-title": "NeuroCOVID: insights into neuroinvasion and pathophysiology",
"author": "Jung",
"doi-asserted-by": "publisher",
"first-page": "10",
"journal-title": "Clini Transl Neurosci.",
"key": "B86",
"volume": "6",
"year": "2022"
},
{
"DOI": "10.1152/physrev.1999.79.4.1431",
"article-title": "Ischemic cell death in brain neurons",
"author": "Lipton",
"doi-asserted-by": "publisher",
"first-page": "1431",
"journal-title": "Physiol Rev",
"key": "B87",
"volume": "79",
"year": "1999"
},
{
"DOI": "10.1007/s11357-024-01096-1",
"article-title": "Molecular cross-talk between long COVID-19 and Alzheimer's disease",
"author": "Pszczołowska",
"doi-asserted-by": "publisher",
"first-page": "2885",
"journal-title": "GeroScience.",
"key": "B88",
"volume": "46",
"year": "2024"
},
{
"DOI": "10.1177/10738584231194927",
"article-title": "COVID-19 and long COVID: disruption of the neurovascular unit, blood-brain barrier, and tight junctions",
"author": "Kempuraj",
"doi-asserted-by": "publisher",
"first-page": "10738584231194928",
"journal-title": "Neuroscientist.",
"key": "B89",
"volume": "2023",
"year": "2023"
},
{
"DOI": "10.1186/s12974-021-02309-6",
"article-title": "The semantics of microglia activation: neuroinflammation, homeostasis, and stress",
"author": "Woodburn",
"doi-asserted-by": "publisher",
"first-page": "258",
"journal-title": "J Neuroinflammation.",
"key": "B90",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1016/j.neuron.2022.10.006",
"article-title": "The neurobiology of long COVID",
"author": "Monje",
"doi-asserted-by": "publisher",
"first-page": "3484",
"journal-title": "Neuron.",
"key": "B91",
"volume": "110",
"year": "2022"
},
{
"DOI": "10.1172/jci.insight.160989",
"article-title": "Markers of fungal translocation are elevated during post-acute sequelae of SARS-CoV-2 and induce NF-κB signaling",
"author": "Giron",
"doi-asserted-by": "publisher",
"first-page": "15",
"journal-title": "JCI Insight.",
"key": "B92",
"volume": "7",
"year": "2022"
},
{
"DOI": "10.1212/NXI.0000000000200003",
"article-title": "Plasma markers of neurologic injury and inflammation in people with self-reported neurologic postacute sequelae of SARS-CoV-2 infection",
"author": "Peluso",
"doi-asserted-by": "publisher",
"first-page": "35701186",
"journal-title": "Neurology.",
"key": "B93",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1186/s12967-023-04149-9",
"article-title": "Plasma proteome of Long-COVID patients indicates HIF-mediated vasculo-proliferative disease with impact on brain and heart function",
"author": "Iosef",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Transl Med.",
"key": "B94",
"volume": "21",
"year": "2023"
},
{
"DOI": "10.1007/s10456-023-09890-9",
"article-title": "VEGF-A plasma levels are associated with impaired DLCO and radiological sequelae in long COVID patients",
"author": "Philippe",
"doi-asserted-by": "publisher",
"first-page": "51",
"journal-title": "Angiogenesis.",
"key": "B95",
"volume": "27",
"year": "2024"
},
{
"DOI": "10.1155/2015/387842",
"article-title": "Proinflammatory cytokines increase vascular endothelial growth factor expression in alveolar epithelial cells",
"author": "Maloney",
"doi-asserted-by": "publisher",
"first-page": "387842",
"journal-title": "Mediators Inflamm.",
"key": "B96",
"volume": "2015",
"year": "2015"
},
{
"DOI": "10.1172/JCI17712",
"article-title": "Proinflammatory functions of vascular endothelial growth factor in alloimmunity",
"author": "Reinders",
"doi-asserted-by": "publisher",
"first-page": "1655",
"journal-title": "J Clin Invest.",
"key": "B97",
"volume": "112",
"year": "2003"
},
{
"DOI": "10.3390/ijms22136671",
"article-title": "vegf regulation of angiogenic factors via inflammatory signaling in myeloproliferative neoplasms",
"author": "Subotički",
"doi-asserted-by": "publisher",
"first-page": "6671",
"journal-title": "Int J Mol Sci.",
"key": "B98",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1242/dev.151019",
"article-title": "Vascular endothelial growth factor signaling in development and disease",
"author": "Karaman",
"doi-asserted-by": "publisher",
"first-page": "dev151019",
"journal-title": "Development",
"key": "B99",
"volume": "145",
"year": "2018"
},
{
"DOI": "10.3390/microorganisms10122452",
"article-title": "Impaired VEGF-A-mediated neurovascular crosstalk induced by SARS-CoV-2 spike protein: a potential hypothesis explaining long COVID-19 symptoms and COVID-19 vaccine side effects?",
"author": "Talotta",
"doi-asserted-by": "publisher",
"first-page": "2452",
"journal-title": "Microorganisms.",
"key": "B100",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1186/s10020-022-00548-8",
"article-title": "Elevated vascular transformation blood biomarkers in Long-COVID indicate angiogenesis as a key pathophysiological mechanism",
"author": "Patel",
"doi-asserted-by": "publisher",
"first-page": "122",
"journal-title": "Mol Med.",
"key": "B101",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1101/cshperspect.a020412",
"article-title": "The blood-brain barrier",
"author": "Daneman",
"doi-asserted-by": "publisher",
"first-page": "a020412",
"journal-title": "Cold Spring Harb Perspect Biol",
"key": "B102",
"volume": "7",
"year": "2015"
},
{
"DOI": "10.1016/j.biopha.2021.112550",
"article-title": "critical analysis of SARS-CoV-2 (COVID-19) complexities, emerging variants, and therapeutic interventions and vaccination strategies",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "112550",
"journal-title": "Biomed Pharmacother.",
"key": "B103",
"volume": "146",
"year": "2021"
},
{
"DOI": "10.3389/fncel.2023.1125109",
"article-title": "Alteration of the blood-brain barrier by COVID-19 and its implication in the permeation of drugs into the brain",
"author": "Hernández-Parra",
"doi-asserted-by": "publisher",
"first-page": "1125109",
"journal-title": "Front Cell Neurosci.",
"key": "B104",
"volume": "17",
"year": "2023"
},
{
"DOI": "10.1155/2021/7880448",
"article-title": "Neuropsychiatric ramifications of COVID-19: short-chain fatty acid deficiency and disturbance of microbiota-gut-brain axis signaling",
"author": "Sajdel-Sulkowska",
"doi-asserted-by": "publisher",
"first-page": "7880448",
"journal-title": "Biomed Res Int.",
"key": "B105",
"volume": "2021",
"year": "2021"
},
{
"key": "B106",
"unstructured": "Host-Microbiome Associations in Saliva Predict COVID-19 Severity\n \n \n \n Alqedari\n H\n \n \n Altabtbaei\n K\n \n \n Espinoza\n JL\n \n \n Bin-Hasan\n S\n \n \n Alghounaim\n M\n \n \n Alawady\n A\n \n \n bioRxiv\n \n 2023"
},
{
"DOI": "10.14309/ctg.0000000000000524",
"article-title": "Decreased gut microbiome tryptophan metabolism and serotonergic signaling in patients with persistent mental health and gastrointestinal symptoms after COVID-19",
"author": "Blackett",
"doi-asserted-by": "publisher",
"first-page": "e00524",
"journal-title": "Clin Transl Gastroenterol.",
"key": "B107",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.3389/fnut.2022.868845",
"article-title": "Tryptophan metabolism and COVID-19-induced skeletal muscle damage: Is ACE2 a key regulator?",
"author": "Takeshita",
"doi-asserted-by": "publisher",
"first-page": "868845",
"journal-title": "Front Nutr.",
"key": "B108",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1155/2021/2911578",
"article-title": "Tryptophan-kynurenine pathway in COVID-19-dependent musculoskeletal pathology: a minireview",
"author": "Vyavahare",
"doi-asserted-by": "publisher",
"first-page": "34621138",
"journal-title": "Mediators Inflamm",
"key": "B109",
"volume": "2021",
"year": "2021"
},
{
"DOI": "10.1016/j.cell.2023.09.013",
"article-title": "Serotonin reduction in post-acute sequelae of viral infection",
"author": "Wong",
"doi-asserted-by": "publisher",
"first-page": "4851",
"journal-title": "Cell",
"key": "B110",
"volume": "186",
"year": "2023"
},
{
"DOI": "10.1038/s41392-021-00614-3",
"article-title": "Metagenomic analysis reveals oropharyngeal microbiota alterations in patients with COVID-19",
"author": "Ma",
"doi-asserted-by": "publisher",
"first-page": "191",
"journal-title": "Signal Transduct Target Ther.",
"key": "B111",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1136/gutjnl-2020-323020",
"article-title": "Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19",
"author": "Yeoh",
"doi-asserted-by": "publisher",
"first-page": "698",
"journal-title": "Gut.",
"key": "B112",
"volume": "70",
"year": "2020"
},
{
"DOI": "10.3390/ijms231911245",
"article-title": "The microbiota-gut-brain axis in psychiatric disorders",
"author": "Góralczyk-Bińkowska",
"doi-asserted-by": "publisher",
"first-page": "11245",
"journal-title": "Int J Mol Sci.",
"key": "B113",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1146/annurev-med-042320-014032",
"article-title": "The gut-brain axis",
"author": "Mayer",
"doi-asserted-by": "publisher",
"first-page": "439",
"journal-title": "Annu Rev Med.",
"key": "B114",
"volume": "73",
"year": "2022"
},
{
"DOI": "10.3390/nu15092211",
"article-title": "Short-chain fatty-acid-producing bacteria: key components of the human gut microbiota",
"author": "Fusco",
"doi-asserted-by": "publisher",
"first-page": "2211",
"journal-title": "Nutrients.",
"key": "B115",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1016/j.pharmthera.2022.108273",
"article-title": "Short-chain fatty acid receptors and gut microbiota as therapeutic targets in metabolic, immune, and neurological diseases",
"author": "Ikeda",
"doi-asserted-by": "publisher",
"first-page": "108273",
"journal-title": "Pharmacol Ther.",
"key": "B116",
"volume": "239",
"year": "2022"
},
{
"DOI": "10.3390/v13040700",
"article-title": "Long-COVID and post-COVID health complications. An up-to-date review on clinical conditions and their possible molecular mechanisms viruses",
"author": "Silva Andrade",
"doi-asserted-by": "publisher",
"first-page": "700",
"journal-title": "Viruses.",
"key": "B117",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3389/fcimb.2022.861703",
"article-title": "Long COVID: the nature of thrombotic sequelae determines the necessity of early anticoagulation",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "861703",
"journal-title": "Front Cell Infect Microbiol.",
"key": "B118",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.2174/1570161111311020005",
"article-title": "Endothelial dysfunction in sepsis",
"author": "Boisramé-Helms",
"doi-asserted-by": "publisher",
"first-page": "150",
"journal-title": "Curr Vasc Pharmacol",
"key": "B119",
"volume": "11",
"year": "2013"
},
{
"DOI": "10.1016/j.thromres.2020.04.014",
"article-title": "Severe COVID-19 infection associated with endothelial activation",
"author": "Escher",
"doi-asserted-by": "publisher",
"first-page": "62",
"journal-title": "Thromb Res.",
"key": "B120",
"volume": "190",
"year": "2020"
},
{
"DOI": "10.1161/01.RES.0000255690.03436.ae",
"article-title": "Phenotypic heterogeneity of the endothelium: II. Representative vascular beds",
"author": "Aird",
"doi-asserted-by": "publisher",
"first-page": "174",
"journal-title": "Circ Res.",
"key": "B121",
"volume": "100",
"year": "2007"
},
{
"DOI": "10.1016/j.thromres.2020.05.001",
"article-title": "Targeting raised von Willebrand factor levels and macrophage activation in severe COVID-19: Consider low volume plasma exchange and low dose steroid",
"author": "Zachariah",
"doi-asserted-by": "publisher",
"first-page": "2",
"journal-title": "Thromb Res.",
"key": "B122",
"volume": "192",
"year": "2020"
},
{
"key": "B123",
"unstructured": "Murphy\n H\n \n \n MRI Scans Show COVID's ‘Significant’ Impact on the Brain\n \n 2022"
},
{
"DOI": "10.1182/blood-2021-154308",
"article-title": "Lanetta Bronté-Hall, Patrick Hines; whole blood adhesion to VCAM-1 and P-selectin and RBC mechanical fragility can be compromised in long covid-19 patients with sickle cell disease",
"author": "Tarasev",
"doi-asserted-by": "publisher",
"first-page": "959",
"journal-title": "Blood.",
"key": "B124",
"volume": "138",
"year": "2021"
},
{
"DOI": "10.3389/fcvm.2023.1062491",
"article-title": "The intersection of obesity and (long) COVID-19: hypoxia, thrombotic inflammation, and vascular endothelial injury",
"author": "Xiang",
"doi-asserted-by": "publisher",
"first-page": "1062491",
"journal-title": "Front Cardiovasc Med.",
"key": "B125",
"volume": "10",
"year": "2023"
},
{
"DOI": "10.3389/fimmu.2022.862522",
"article-title": "Persistent Lung Injury and Prothrombotic State in Long COVID",
"author": "Xiang",
"doi-asserted-by": "publisher",
"first-page": "862522",
"journal-title": "Front Immunol.",
"key": "B126",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1038/s41598-023-32275-3",
"article-title": "Cerebral hypoperfusion in post-COVID-19 cognitively impaired subjects revealed by arterial spin labeling MRI",
"author": "Ajčević",
"doi-asserted-by": "publisher",
"first-page": "5808",
"journal-title": "Sci Rep.",
"key": "B127",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1016/j.jacc.2020.08.059",
"article-title": "Coronavirus and cardiovascular disease, myocardial injury, and arrhythmia: JACC focus seminar",
"author": "Giustino",
"doi-asserted-by": "publisher",
"first-page": "2011",
"journal-title": "J Am Coll Cardiol",
"key": "B128",
"volume": "76",
"year": "2020"
},
{
"DOI": "10.1097/MNM.0000000000001689",
"article-title": "Investigating the potential added value of [18 F]FDG-PET/CT in long COVID patients with persistent symptoms: a proof of concept study",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "495",
"journal-title": "Nucl Med Commun.",
"key": "B129",
"volume": "44",
"year": "2023"
},
{
"DOI": "10.1093/rheumatology/keab247.053",
"article-title": "P056 Recurrent ACE-inhibitor induced angioedema in a patient with long COVID-19 syndrome",
"author": "Crawshaw",
"doi-asserted-by": "publisher",
"first-page": "53",
"journal-title": "Rheumatology.",
"key": "B130",
"volume": "60",
"year": "2021"
},
{
"DOI": "10.1210/jendso/bvad114.1810",
"article-title": "FRI463 A Case Of Post COVID-19 Subacute Thyroiditis: A Thyroid Equivalent Of Long COVID?",
"author": "Shiraliyeva",
"doi-asserted-by": "publisher",
"journal-title": "J Endocr Soc 7:.",
"key": "B131",
"year": "1810"
},
{
"key": "B132",
"unstructured": "Genome-wide association study of long COVID\n \n \n \n Lammi\n V\n \n \n Nakanishi\n T\n \n \n Jones\n SE\n \n \n Andrews\n SJ\n \n \n Karjalainen\n J\n \n \n Cortés\n B\n \n \n medRxiv\n \n 2023"
},
{
"DOI": "10.1016/S1567-133X(02)00058-3",
"article-title": "Foxp4: A novel member of the Foxp subfamily of winged-helix genes co-expressed with Foxp1 and Foxp2 in pulmonary and gut tissues",
"author": "Lu MM Li",
"doi-asserted-by": "publisher",
"first-page": "223",
"journal-title": "Gene Expression Patt.",
"key": "B133",
"volume": "2",
"year": "2002"
},
{
"DOI": "10.1002/jnr.21770",
"article-title": "Expression of Foxp4 in the developing and adult rat forebrain",
"author": "Takahashi",
"doi-asserted-by": "publisher",
"first-page": "3106",
"journal-title": "J Neurosci Res.",
"key": "B134",
"volume": "86",
"year": "2008"
},
{
"DOI": "10.1038/s41586-021-03767-x",
"article-title": "Mapping the human genetic architecture of COVID-19",
"doi-asserted-by": "publisher",
"first-page": "472",
"journal-title": "Nature",
"key": "B135",
"volume": "600",
"year": "2021"
},
{
"DOI": "10.1016/j.neuron.2012.02.024",
"article-title": "Foxp-mediated suppression of N-cadherin regulates neuroepithelial character and progenitor maintenance in the CNS",
"author": "Rousso",
"doi-asserted-by": "publisher",
"first-page": "314",
"journal-title": "Neuron.",
"key": "B136",
"volume": "74",
"year": "2012"
},
{
"DOI": "10.1016/j.neuroscience.2010.10.023",
"article-title": "Foxp4 is essential in maintenance of Purkinje cell dendritic arborization in the mouse cerebellum",
"author": "Tam",
"doi-asserted-by": "publisher",
"first-page": "562",
"journal-title": "Neuroscience.",
"key": "B137",
"volume": "172",
"year": "2011"
},
{
"DOI": "10.1002/ajmg.a.63006",
"article-title": "Recurrent FOXP4 nonsense variant in two unrelated patients: association with neurodevelopmental disease and congenital diaphragmatic hernia",
"author": "Del Viso",
"doi-asserted-by": "publisher",
"first-page": "259",
"journal-title": "Am J Med Genet A.",
"key": "B138",
"volume": "191",
"year": "2023"
},
{
"DOI": "10.3390/jpm13010123",
"article-title": "Host genetic variants linked to COVID-19 neurological complications and susceptibility in young adults-A preliminary analysis",
"author": "Kazantseva",
"doi-asserted-by": "publisher",
"first-page": "123",
"journal-title": "J Pers Med.",
"key": "B139",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1074/jbc.M300760200",
"article-title": "Expression of liver X receptor target genes decreases cellular amyloid beta peptide secretion",
"author": "Sun",
"doi-asserted-by": "publisher",
"first-page": "27688",
"journal-title": "J Biol Chem.",
"key": "B140",
"volume": "278",
"year": "2003"
},
{
"DOI": "10.1016/j.meegid.2022.105379",
"article-title": "Genome-wide association studies of COVID-19: connecting the dots",
"author": "Ferreira",
"doi-asserted-by": "publisher",
"first-page": "105379",
"journal-title": "Infect Genet Evol.",
"key": "B141",
"volume": "106",
"year": "2022"
},
{
"DOI": "10.1093/cid/ciac443",
"article-title": "Effectiveness of Paxlovid in reducing severe Coronavirus disease 2019 and mortality in high-Risk Patients",
"author": "Najjar-Debbiny",
"doi-asserted-by": "publisher",
"first-page": "e342",
"journal-title": "Clin Infect Dis.",
"key": "B142",
"volume": "76",
"year": "2023"
},
{
"DOI": "10.1002/jmv.29333",
"article-title": "Association of nirmatrelvir for acute SARS-CoV-2 infection with subsequent Long COVID symptoms in an observational cohort study",
"author": "Durstenfeld",
"doi-asserted-by": "publisher",
"first-page": "e29333",
"journal-title": "J Med Virol.",
"key": "B143",
"volume": "96",
"year": "2024"
},
{
"DOI": "10.1016/j.cmi.2022.04.018",
"article-title": "Remdesivir for the treatment of COVID-19: a systematic review and meta-analysis",
"author": "Lee",
"doi-asserted-by": "publisher",
"first-page": "1203",
"journal-title": "Clin Microbiol Infect.",
"key": "B144",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1001/jama.2021.18295",
"article-title": "Effect of 12 mg vs 6 mg of dexamethasone on the number of days alive without life support in adults with COVID-19 and severe hypoxemia: The COVID STEROID 2 randomized trial",
"author": "COVID STEROID 2 Trial",
"doi-asserted-by": "publisher",
"first-page": "1807",
"journal-title": "JAMA.",
"key": "B145",
"volume": "326",
"year": "2021"
},
{
"DOI": "10.3389/fcvm.2023.1202696",
"article-title": "Antihistamines improve cardiovascular manifestations and other symptoms of long-COVID attributed to mast cell activation",
"author": "Salvucci",
"doi-asserted-by": "publisher",
"first-page": "1202696",
"journal-title": "Front Cardiovasc Med.",
"key": "B146",
"volume": "10",
"year": "2023"
},
{
"DOI": "10.1001/jamanetworkopen.2023.8516",
"article-title": "Dexamethasone for inpatients with COVID-19 in a national cohort",
"author": "Mourad",
"doi-asserted-by": "publisher",
"first-page": "e238516",
"journal-title": "JAMA Netw Open.",
"key": "B147",
"volume": "6",
"year": "2023"
},
{
"DOI": "10.1016/j.heliyon.2022.e10906",
"article-title": "The role of melatonin as an adjuvant in the treatment of COVID-19: a systematic review",
"author": "Faridzadeh",
"doi-asserted-by": "publisher",
"first-page": "e10906",
"journal-title": "Heliyon.",
"key": "B148",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.1001/jamanetworkopen.2022.3890",
"article-title": "Association of early aspirin use with in-hospital mortality in patients with moderate COVID-19",
"author": "Chow",
"doi-asserted-by": "publisher",
"first-page": "e223890",
"journal-title": "JAMA Netw Open.",
"key": "B149",
"volume": "5",
"year": "2022"
},
{
"DOI": "10.1176/appi.ajp-rj.2022.170402",
"article-title": "Modafinil: a review and its potential use in the treatment of long COVID fatigue and neurocognitive deficits",
"author": "Pliszka",
"doi-asserted-by": "publisher",
"first-page": "5",
"journal-title": "Am J Psychiatry Resid.",
"key": "B150",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1136/jim-2021-002051",
"article-title": "Long COVID following mild SARS-CoV-2 infection: characteristic T cell alterations and response to antihistamines",
"author": "Glynne",
"doi-asserted-by": "publisher",
"first-page": "61",
"journal-title": "J Investig Med.",
"key": "B151",
"volume": "70",
"year": "2022"
},
{
"DOI": "10.2174/1871526522666220107125511",
"article-title": "Therapeutic status of famotidine in COVID-19 patients: a review",
"author": "Mohseni",
"doi-asserted-by": "publisher",
"first-page": "125511",
"journal-title": "Infect Disord Drug Targets.",
"key": "B152",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1055/a-1397-6763",
"article-title": "Famotidine repurposing for novel corona virus disease of 2019: a systematic review",
"author": "Chenchula",
"doi-asserted-by": "publisher",
"first-page": "295",
"journal-title": "Drug Res.",
"key": "B153",
"volume": "71",
"year": "2021"
},
{
"DOI": "10.1111/bcp.15512",
"article-title": "Prevalence of NSAID use among people with COVID-19 and the association with COVID-19-related outcomes: Systematic review and meta-analysis",
"author": "Zhao",
"doi-asserted-by": "publisher",
"first-page": "5113",
"journal-title": "Br J Clin Pharmacol.",
"key": "B154",
"volume": "88",
"year": "2022"
},
{
"DOI": "10.1007/s00259-021-05215-4",
"article-title": "18F-FDG brain PET hypometabolism in patients with long COVID",
"author": "Guedj",
"doi-asserted-by": "publisher",
"first-page": "2823",
"journal-title": "Eur J Nucl Med Mol Imaging.",
"key": "B155",
"volume": "48",
"year": "2021"
},
{
"DOI": "10.1007/s10787-021-00806-x",
"article-title": "Neuropathophysiology of coronavirus disease 2019: neuroinflammation and blood brain barrier disruption are critical pathophysiological processes that contribute to the clinical symptoms of SARS-CoV-2 infection",
"author": "Welcome",
"doi-asserted-by": "publisher",
"first-page": "939",
"journal-title": "Inflammopharmacology.",
"key": "B156",
"volume": "29",
"year": "2021"
},
{
"DOI": "10.1038/s41586-020-2196-x",
"article-title": "Virological assessment of hospitalized patients with COVID-2019",
"author": "Wölfel",
"doi-asserted-by": "publisher",
"first-page": "465",
"journal-title": "Nature.",
"key": "B157",
"volume": "581",
"year": "2020"
},
{
"DOI": "10.1038/s41591-020-0817-4",
"article-title": "Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding",
"author": "Xu",
"doi-asserted-by": "publisher",
"first-page": "502",
"journal-title": "Nat Med.",
"key": "B158",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.26355/eurrev_202009_23060",
"article-title": "The first case of systemic lupus erythematosus (SLE) triggered by COVID-19 infection",
"author": "Bonometti",
"doi-asserted-by": "publisher",
"first-page": "9695",
"journal-title": "Eur Rev Med Pharmacol Sci.",
"key": "B159",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1111/ijd.15257",
"article-title": "COVID-19: An overview for dermatologists",
"author": "Sanghvi",
"doi-asserted-by": "publisher",
"first-page": "1437",
"journal-title": "Int J Dermatol.",
"key": "B160",
"volume": "59",
"year": "2020"
},
{
"DOI": "10.1016/j.jaad.2020.06.051",
"article-title": "Navigating immunosuppression in a pandemic: A guide for the dermatologist from the COVID Task Force of the Medical Dermatology Society and Society of Dermatology Hospitalists",
"author": "O",
"doi-asserted-by": "publisher",
"first-page": "1150",
"journal-title": "J Am Acad Dermatol",
"key": "B161",
"volume": "83",
"year": "2020"
},
{
"DOI": "10.1002/rmv.2437",
"article-title": "Reactivation of herpesviruses during COVID-19: a systematic review and meta-analysis",
"author": "Shafiee",
"doi-asserted-by": "publisher",
"first-page": "2437",
"journal-title": "Rev Med Virol.",
"key": "B162",
"volume": "33",
"year": "2023"
},
{
"DOI": "10.1002/iub.210",
"article-title": "The role of the neutral amino acid transporter B0AT1 (SLC6A19) in Hartnup disorder and protein nutrition",
"author": "Bröer",
"doi-asserted-by": "publisher",
"first-page": "591",
"journal-title": "IUBMB Life.",
"key": "B163",
"volume": "61",
"year": "2009"
},
{
"DOI": "10.1042/CS20200477",
"article-title": "ACE2 and gut amino acid transport",
"author": "Camargo",
"doi-asserted-by": "publisher",
"first-page": "2823",
"journal-title": "Clin Sci.",
"key": "B164",
"volume": "134",
"year": "2020"
},
{
"DOI": "10.1186/s12877-020-01644-2",
"article-title": "Dysbiosis, gut barrier dysfunction and inflammation in dementia: a pilot study",
"author": "Stadlbauer",
"doi-asserted-by": "publisher",
"journal-title": "BMC Geriatr",
"key": "B165",
"year": ""
},
{
"article-title": "Short-chain fatty acids and lipopolysaccharide as mediators between gut dysbiosis and amyloid pathology in Alzheimer's disease",
"author": "Marizzoni",
"first-page": "2011",
"journal-title": "J Alzheimers Dis",
"key": "B166",
"volume": "78",
"year": "2022"
},
{
"DOI": "10.1038/s41401-022-00998-0",
"article-title": "Endothelial dysfunction in COVID-19: an overview of evidence, biomarkers, mechanisms and potential therapies",
"author": "Xu",
"doi-asserted-by": "publisher",
"first-page": "695",
"journal-title": "Acta Pharmacol Sin.",
"key": "B167",
"volume": "44",
"year": "2023"
},
{
"DOI": "10.1016/j.vaccine.2015.10.018",
"article-title": "Chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) is associated with pandemic influenza infection, but not with an adjuvanted pandemic influenza vaccine",
"author": "Magnus",
"doi-asserted-by": "publisher",
"first-page": "6173",
"journal-title": "Vaccine.",
"key": "B168",
"volume": "33",
"year": "2015"
},
{
"DOI": "10.1186/1471-2377-11-37",
"article-title": "Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study",
"author": "Moldofsky",
"doi-asserted-by": "publisher",
"first-page": "37",
"journal-title": "BMC Neurol",
"key": "B169",
"volume": "11",
"year": "2011"
},
{
"DOI": "10.1016/j.molmed.2021.06.002",
"article-title": "Insights from myalgic encephalomyelitis/chronic fatigue syndrome may help unravel the pathogenesis of postacute COVID-19 syndrome",
"author": "Komaroff",
"doi-asserted-by": "publisher",
"first-page": "895",
"journal-title": "Trends Mol Med",
"key": "B170",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1080/19490976.2023.2249146",
"article-title": "Gut microbiota from patients with COVID-19 cause alterations in mice that resemble post-COVID symptoms",
"author": "Almeida",
"doi-asserted-by": "crossref",
"first-page": "2249146",
"journal-title": "Gut Microbes.",
"key": "B171",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1016/j.chom.2023.01.004",
"article-title": "Deficient butyrate-producing capacity in the gut microbiome is associated with bacterial network disturbances and fatigue symptoms in ME/CFS",
"author": "Guo",
"doi-asserted-by": "publisher",
"first-page": "288",
"journal-title": "Cell Host Microbe",
"key": "B172",
"volume": "31",
"year": "2023"
},
{
"DOI": "10.3390/cells11071239",
"article-title": "The influence of gut dysbiosis in the pathogenesis and management of ischemic stroke",
"author": "Chidambaram",
"doi-asserted-by": "publisher",
"journal-title": "Cells 11:.",
"key": "B173",
"year": "1239"
},
{
"DOI": "10.1136/gutjnl-2020-323263",
"article-title": "Rapid gut dysbiosis induced by stroke exacerbates brain infarction in turn",
"author": "Xu",
"doi-asserted-by": "publisher",
"first-page": "1486",
"journal-title": "Gut.",
"key": "B174",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.1186/s12933-021-01359-7",
"article-title": "Persistent clotting protein pathology in Long COVID/post-acute sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin",
"author": "Pretorius",
"doi-asserted-by": "publisher",
"first-page": "172",
"journal-title": "Cardiovasc Diabetol.",
"key": "B175",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1042/BSR20210611",
"article-title": "SARS-CoV-2 spike protein S1 induces fibrin(ogen) resistant to fibrinolysis: implications for microclot formation in COVID-19",
"author": "Grobbelaar",
"doi-asserted-by": "publisher",
"first-page": "BSR20210611",
"journal-title": "Biosci Rep",
"key": "B176",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.3390/cells12050816",
"article-title": "Pathogenesis underlying neurological manifestations of long COVID syndrome and potential therapeutics",
"author": "Leng",
"doi-asserted-by": "publisher",
"first-page": "816",
"journal-title": "Cells.",
"key": "B177",
"volume": "12",
"year": "2023"
},
{
"DOI": "10.1021/acs.jpcb.1c04871",
"article-title": "Presence of a SARS-COV-2 protein enhances Amyloid Formation of Serum Amyloid A",
"author": "Jana",
"doi-asserted-by": "publisher",
"first-page": "9155",
"journal-title": "J Phys Chem B.",
"key": "B178",
"volume": "125",
"year": "2021"
},
{
"DOI": "10.1038/nrn3027",
"article-title": "Neural mechanisms of the cognitive model of depression",
"author": "Disner",
"doi-asserted-by": "publisher",
"first-page": "467",
"journal-title": "Nat Rev Neurosci.",
"key": "B179",
"volume": "12",
"year": "2011"
},
{
"DOI": "10.1016/j.jns.2024.123295",
"article-title": "The impact of gut microbiome and diet on post-acute sequelae of SARS-CoV-2 infection",
"author": "Reyes",
"doi-asserted-by": "publisher",
"journal-title": "J Neurol Sci.",
"key": "B180",
"year": "2024"
},
{
"DOI": "10.1002/pmrj.13085",
"article-title": "Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of mental health symptoms in patients with post-acute sequelae of SARS-CoV-2 infection (PASC)",
"author": "Cheng",
"doi-asserted-by": "publisher",
"first-page": "1588",
"journal-title": "PM R.",
"key": "B181",
"volume": "15",
"year": "2023"
}
],
"reference-count": 181,
"references-count": 181,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fneur.2024.1465787/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Neurological sequelae of long COVID: a comprehensive review of diagnostic imaging, underlying mechanisms, and potential therapeutics",
"type": "journal-article",
"update-policy": "https://doi.org/10.3389/crossmark-policy",
"volume": "15"
}