NSAID prescribing and adverse outcomes in common infections: a population-based cohort study
et al., BMJ Open, doi:10.1136/bmjopen-2023-077365, Jan 2024
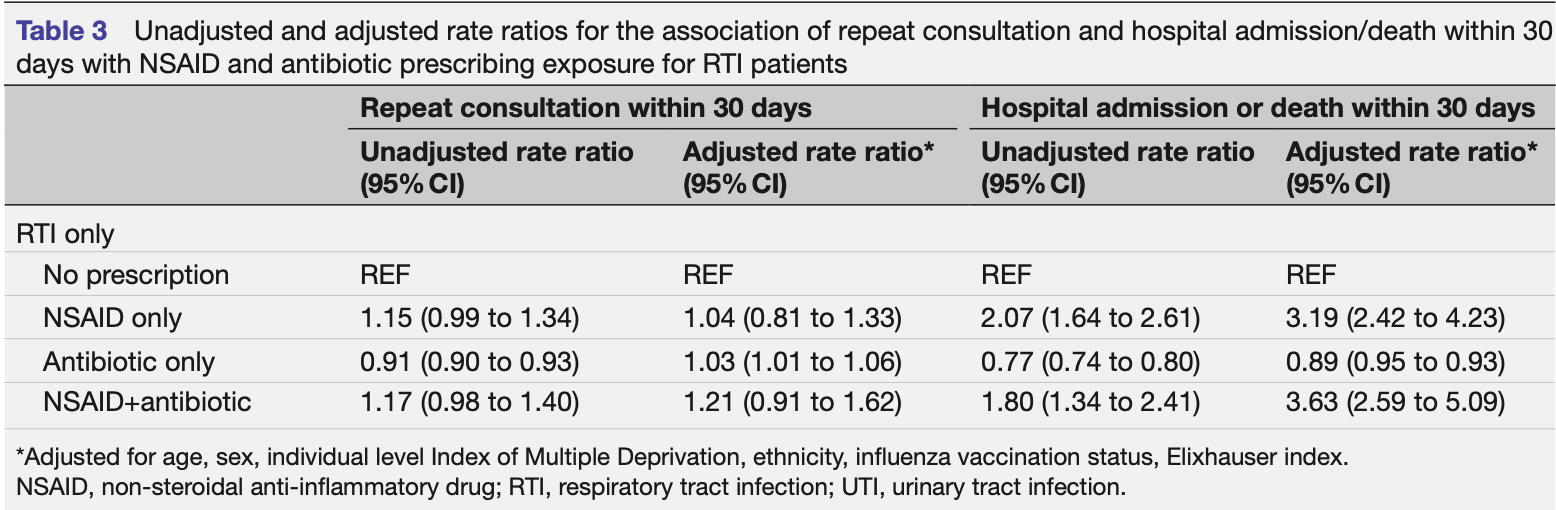
Retrospective 142,925 outpatients in the UK showing significantly higher risk of hospitalization or death with prescription of NSAIDs for respiratory tract infections (RTI) or urinary tract infections (UTI).
Practice-level analysis also found a 0.32 percentage point increase in hospitalizations/deaths for every 1 percentage point increase in NSAID prescribing.
NSAIDs may be harmful due to suppression of inflammatory and immune responses needed to clear infections. They inhibit cyclooxygenase enzymes and production of prostaglandins involved in inflammation. This anti-inflammatory effect could hamper the body's ability to fight the infection. NSAIDs may mask symptoms of worsening infection. By reducing pain, fever, and inflammation, they could provide symptomatic relief while the infection progresses unchecked, delaying further medical care. NSAIDs may increase risks of certain complications. There is some evidence linking NSAIDs to higher risk of cardiovascular events. The increased risk could also be partly explained by confounding factors not fully accounted for in the analyses, although practive-level analysis points to an association rather than confounding by indication.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
Study covers ibuprofen and indomethacin.
|
risk of death/hospitalization, 219.0% higher, OR 3.19, p < 0.001, adjusted per study, NSAID only vs. no prescription, multivariable, day 30, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Stuart et al., 3 Jan 2024, retrospective, United Kingdom, peer-reviewed, 7 authors.
NSAID prescribing and adverse outcomes in common infections: a population-based cohort study
doi:10.1136/bmjopen-2023-077365
Objectives Infections in primary care are often treated with non-steroidal anti-inflammatory drugs (NSAIDs). This study evaluates whether NSAID prescribing is associated with adverse outcomes for respiratory (RTIs) or urinary track (UTI) infections. Objectives To determine whether there is an association between NSAID prescribing and the rate of adverse outcomes for infections for individual consulting in primary care. Design Cohort study of electronic health records. Setting 87 general practices in the UK Clinical Practice Research Datalink GOLD. Participants 142 925 patients consulting with RTI or UTI. Primary and secondary outcome measures Repeat consultations, hospitalisation or death within 30 days of the initial consultation for RTI or UTI. Poisson models estimated the associations between NSAID exposure and outcome. Rate ratios were adjusted for gender, age, ethnicity, deprivation, antibiotic use, seasonal influenza vaccination status, comorbidities and general practice. Since prescribing variations by practice are not explained by case mix-hence, less impacted by confounding by indication-both individual-level and practice-level analyses are included. Results There was an increase in hospital admission/ death for acute NSAID prescriptions (RR 2.73, 95% CI 2.10 to 3.56) and repeated NSAID prescriptions (6.47, 4.46-9.39) in RTI patients, and for acute NSAID prescriptions for UTI (RR 3.03; 1.92 to 4.76). Practice-level analysis, controlling for practice population characteristics, found that for each percentage point increase in NSAID prescription, the percentages of hospital admission/ death within 30 days increased by 0.32 percentage points (95% CI 0.16 to 0.47). Conclusions In this non-randomised study, prescription of NSAIDs at consultations for RTI or UTIs in primary care is infrequent but may be associated with increased risk of hospital admission. This supports other observational and limited trial data that NSAID prescribing might be associated with worse outcomes following acute infection and should be prescribed with caution.
BACKGROUND Consultations for respiratory tract infections (RTIs) are common in primary care. A recent study using Clinical Practice Research Datalink (CPRD) practices found a consulting rate of 217 consultations per 1000 person years. 1 Urinary tract infection (UTI) are also common, with 11% of women experiencing at least one episode each year. 2 Most patients are be advised to self-manage infections at home and many use analgesics such as paracetamol and non-steroidal antiinflammatory drugs (NSAIDs) for symptom relief. 3 4 However, observational studies suggest that the use of NSAIDs during RTIs may be associated with increased risk of acute cardiovascular events, 5 and cyclooxygenase-2 inhibitors or non-selective NSAIDs may be associated with a further increase in risk. 6 7 There is also some evidence that exposure to NSAIDs during an episode of an acute infection may result in an increased risk of adverse..
References
Basille, Trouve, Plouvier, Non-steroidal anti-inflammatory drugs may worsen the course of community-acquired pneumonia: a cohort study, Lung, doi:10.1007/s00408-016-9973-1
Bhala, Emberson, Merhi, Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials, Lancet, doi:10.1016/S0140-6736(13)60900-9
Bourgeois, Ferroni, Leruez-Ville, Nonsteroidal anti-inflammatory drug without antibiotics for acute viral infection increases the empyema risk in children: a matched case-control study, J Pediatr, doi:10.1016/j.jpeds.2016.05.025
Butler, Hawking, Quigley, Incidence, severity, help seeking, and management of uncomplicated urinary tract infection: a population-based survey, Br J Gen Pract, doi:10.3399/bjgp15X686965
Butler, Hawking, Quigley, Incidence, severity, help seeking, and management of uncomplicated urinary tract infection: a population-based survey, Br J Gen Pract, doi:10.3399/bjgp15X686965
Butler, Hood, Verheij, Variation in antibiotic prescribing and its impact on recovery in patients with acute cough in primary care: prospective study in 13 countries, BMJ, doi:10.1136/bmj.b2242
Cars, Eriksson, Granath, Antibiotic use and bacterial complications following upper respiratory tract infections: a population-based study, BMJ Open, doi:10.1136/bmjopen-2017-016221
Chen, Wang, Liu, IP-10 and MCP-1 as biomarkers associated with disease severity of COVID-19, Mol Med, doi:10.1186/s10020-020-00230-x
Demeslay, Bonnecaze, Vairel, Possible role of antiinflammatory drugs in complications of pharyngitis. a retrospective analysis of 163 cases, Eur Ann Otorhinolaryngol Head Neck Dis, doi:10.1016/j.anorl.2013.08.005
Drake, Fairfield, Pius, Non-steroidal anti-inflammatory drug use and outcomes of COVID-19 in the ISARIC clinical characterisation protocol UK cohort: a matched, prospective cohort study, Lancet Rheumatol, doi:10.1016/S2665-9913(21)00104-1
Elixhauser, Steiner, Harris, Comorbidity measures for use with administrative data, Med Care, doi:10.1097/00005650-199801000-00004
Gulliford, Dregan, Moore, Continued high rates of antibiotic prescribing to adults with respiratory tract infection: survey of 568 UK general practices, BMJ Open, doi:10.1136/bmjopen-2014-006245
Gulliford, Moore, Little, Safety of reduced antibiotic prescribing for self limiting respiratory tract infections in primary care: cohort study using electronic health records, BMJ, doi:10.1136/bmj.i3410
Gulliford, Winter, Probability of sepsis after infection consultations in primary care in the United Kingdom in 2002-2017: population-based cohort study and decision analytic model, PLoS Med, doi:10.1371/journal.pmed.1003202
Herold, Jurinovic, Arnreich, Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19, J Allergy Clin Immunol, doi:10.1016/j.jaci.2020.05.008
Kotsiou, Zarogiannis, Gourgoulianis, Prehospital NSAIDs use prolong hospitalization in patients with pleuro-pulmonary infection, Respir Med, doi:10.1016/j.rmed.2016.12.005
Little, Moore, Kelly, Delayed antibiotic prescribing strategies for respiratory tract infections in primary care: pragmatic, factorial, randomised controlled trial, BMJ, doi:10.1136/bmj.g1606
Little, Moore, Kelly, Ibuprofen, paracetamol, and steam for patients with respiratory tract infections in primary care: pragmatic randomised factorial trial, BMJ, doi:10.1136/bmj.f6041
Little, Stuart, Andreou, Primary care randomised controlled trial of a tailored interactive website for the selfmanagement of respiratory infections (internet doctor), BMJ Open, doi:10.1136/bmjopen-2015-009769
Lund, Kristensen, Reilev, Adverse outcomes and mortality in users of non-steroidal anti-inflammatory drugs who tested positive for SARS-Cov-2: a danish nationwide cohort study, PLoS Med, doi:10.1371/journal.pmed.1003308
Mahadevan, Harley, Fordyce, Completeness and representativeness of small area socioeconomic data linked with the UK clinical practice research datalink (CPRD), J Epidemiol Community Health, doi:10.1136/jech-2022-219200
Mcnulty, Nichols, French, Expectations for consultations and antibiotics for respiratory tract infection in primary care: the RTI clinical iceberg, Br J Gen Pract, doi:10.3399/bjgp13X669149
Meier, Schmitz, Jick, Association between acetaminophen or nonsteroidal antiinflammatory drugs and risk of developing ovarian, breast, or colon cancer, Pharmacotherapy, doi:10.1592/phco.22.5.303.33189
Metcalfe, Masters, Delmestri, Coding algorithms for defining charlson and elixhauser co-morbidities in read-coded databases, BMC Med Res Methodol, doi:10.1186/s12874-019-0753-5
Mhra, Release notes: CPRD GOLD April 2021, CPRD GOLD
Nhs, Respiratory tract infections (RTIs)
Nhs, Urinary tract infections (UTIs)
Palin, Mölter, Belmonte, Antibiotic prescribing for common infections in UK general practice: variability and drivers, J Antimicrob Chemother, doi:10.1093/jac/dkz163
Piroulas, Devillers, Souty, Non-steroids anti-inflammatory drugs and risk of peritonsillar abscess in pharyngitis: a French longitudinal study in primary care †, Fam Pract, doi:10.1093/fampra/cmy111
Schneider, Lévesque, Zhang, Association of selective and conventional nonsteroidal antiinflammatory drugs with acute renal failure: a population-based, nested case-control analysis, Am J Epidemiol, doi:10.1093/aje/kwj331
Shiekh, Harley, Ghosh, Completeness, agreement, and representativeness of ethnicity recording in the United Kingdom's clinical practice research datalink (CPRD) and linked hospital episode statistics (HES), Popul Health Metr, doi:10.1186/s12963-023-00302-0
Smeeth, Thomas, Hall, Risk of myocardial infarction and stroke after acute infection or vaccination, N Engl J Med, doi:10.1056/NEJMoa041747
Stuart, Brotherwood, Van't Hoff, Exploring the appropriateness of antibiotic prescribing for common respiratory tract infections in UK primary care, J Antimicrob Chemother, doi:10.1093/jac/dkz410
Van Walraven, Austin, Jennings, A modification of the elixhauser comorbidity measures into a point system for hospital death using administrative data, Med Care, doi:10.1097/MLR.0b013e31819432e5
Vandenbroucke, Elm, Altman, Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration, PLoS Med, doi:10.1371/journal.pmed.0040297
Vik, Bollestad, Grude, Ibuprofen versus pivmecillinam for uncomplicated urinary tract infection in women-a double-blind, randomized non-inferiority trial, PLoS Med, doi:10.1371/journal.pmed.1002569
Voiriot, Philippot, Elabbadi, Risks related to the use of non-steroidal anti-inflammatory drugs in community-acquired pneumonia in adult and pediatric patients, J Clin Med, doi:10.3390/jcm8060786
Wen, Hsiao, Chan, Acute respiratory infection and use of nonsteroidal anti-inflammatory drugs on risk of acute myocardial infarction: a nationwide case-crossover study, J Infect Dis, doi:10.1093/infdis/jiw603
Wen, Hsiao, Lin, Risk of stroke associated with use of nonsteroidal anti-inflammatory drugs during acute respiratory infection episode, Pharmacoepidemiol Drug Saf, doi:10.1002/pds.4428
Wong, Mackenna, Morton, Use of non-steroidal anti-inflammatory drugs and risk of death from COVID-19: an opensafely cohort analysis based on two cohorts, Ann Rheum Dis, doi:10.1136/annrheumdis-2020-219517