Non-steroidal anti-inflammatory drug use and outcomes of COVID-19 in the ISARIC Clinical Characterisation Protocol UK cohort: a matched, prospective cohort study
et al., The Lancet Rheumatology, doi:10.1016/S2665-9913(21)00104-1, Jul 2021
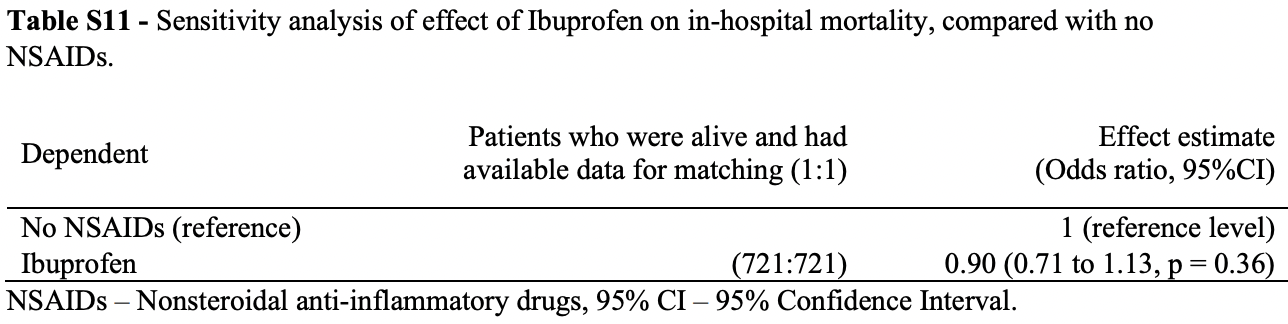
Prospective study of 78,674 COVID-19 patients, showing no significant difference in mortality with ibuprofen use.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 10.0% lower, OR 0.90, p = 0.36, adjusted per study, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Drake et al., 31 Jul 2021, prospective, United Kingdom, peer-reviewed, 13 authors, study period 17 January, 2020 - 10 August, 2020.
Contact: ewen.harrison@ed.ac.uk.
Non-steroidal anti-inflammatory drug use and outcomes of COVID-19 in the ISARIC Clinical Characterisation Protocol UK cohort: a matched, prospective cohort study
The Lancet Rheumatology, doi:10.1016/s2665-9913(21)00104-1
Background Early in the pandemic it was suggested that pre-existing use of non-steroidal anti-inflammatory drugs (NSAIDs) could lead to increased disease severity in patients with COVID-19. NSAIDs are an important analgesic, particularly in those with rheumatological disease, and are widely available to the general public without prescription. Evidence from community studies, administrative data, and small studies of hospitalised patients suggest NSAIDs are not associated with poorer COVID-19 outcomes. We aimed to characterise the safety of NSAIDs and identify whether pre-existing NSAID use was associated with increased severity of COVID-19 disease. Methods This prospective, multicentre cohort study included patients of any age admitted to hospital with a confirmed or highly suspected SARS-CoV-2 infection leading to COVID-19 between Jan 17 and Aug 10, 2020. The primary outcome was in-hospital mortality, and secondary outcomes were disease severity at presentation, admission to critical care, receipt of invasive ventilation, receipt of non-invasive ventilation, use of supplementary oxygen, and acute kidney injury. NSAID use was required to be within the 2 weeks before hospital admission. We used logistic regression to estimate the effects of NSAIDs and adjust for confounding variables. We used propensity score matching to further estimate effects of NSAIDS while accounting for covariate differences in populations.
Results
Between Jan 17 and Aug 10, 2020, we enrolled 78 674 patients across 255 health-care facilities in England, Scotland, and Wales. 72 179 patients had death outcomes available for matching; 40 406 (56•2%) of 71 915 were men, 31 509 (43•8%) were women. In this cohort, 4211 (5•8%) patients were recorded as taking systemic NSAIDs before admission to hospital. Following propensity score matching, balanced groups of NSAIDs users and NSAIDs non-users were obtained (4205 patients in each group). At hospital admission, we observed no significant differences in severity between exposure groups. After adjusting for explanatory variables, NSAID use was not associated with worse in-hospital mortality (matched OR 0•95, 95% CI 0•84-1•07; p=0•35), critical care admission (1•01, 0•87-1•17; p=0•89), requirement for invasive ventilation (0•96, 0•80-1•17; p=0•69), requirement for non-invasive ventilation (1•12, 0•96-1•32; p=0•14), requirement for oxygen (1•00, 0•89-1•12; p=0•97), or occurrence of acute kidney injury (1•08, 0•92-1•26; p=0•33). Interpretation NSAID use is not associated with higher mortality or increased severity of COVID-19. Policy makers should consider reviewing issued advice around NSAID prescribing and COVID-19 severity.
References
Basille, Trouve, Plouvier, Andrejak, Jounieaux, Non-steroidal anti-inflammatory drugs may worsen the course of community-acquired pneumonia: a cohort study, Eur Respir J
Canan, Gokhale, Carruthers, Characterization of lung inflammation and its impact on macrophage function in aging, J Leukoc Biol
Chandan, Zemedikun, Thayakaran, Non-steroidal anti-inflammatory drugs and susceptibility to COVID-19, Arthritis Rheumatol
Chen, Wang, Liu, IP-10 and MCP-1 as biomarkers associated with disease severity of COVID-19, Mol Med
Clinicaltrials, Gov, Inhaled ibuprofen to treat COVID-19
Corte, Caselli, Castellino, Bajocchi, Trotta, Prophylaxis and treatment of NSAID-induced gastroduodenal disorders, Drug Saf
Fang, Karakiulakis, Roth, Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?, Lancet Respir Med
Fishgar, Greifer, Leyrat, Stuart, MatchThem: matching and weighting after multiple imputation, Set
Harris, Taylor, Thielke, Payne, Gonzalez et al., Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support, J Biomed Inform
Herold, Jurinovic, Arnreich, Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19, J Allergy Clin Immunol
Ho, Tipoe, Zheng, In vitro study of regulation of IL-6 production in bronchiectasis, Respir Med
Horby, Pessoa-Amorim, Peto, Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): preliminary results of a randomised, controlled, open-label, platform trial, doi:10.1101/2021.02.11.21249258
Kdigo, KDIGO Clinical Practice Guideline for Acute Kidney Injury
Kotsiou, Zarogiannis, Gourgoulianis, Prehospital NSAIDs use prolong hospitalization in patients with pleuropulmonary infection, Respir Med
Ling, Montez-Rath, Mathur, Kapphahn, Desai, How to apply multiple imputation in propensity score matching with partially observed confounders: a simulation study and practical recommendations
Little, Moore, Kelly, Ibuprofen, paracetamol, and steam for patients with respiratory tract infections in primary care: pragmatic randomised factorial trial, BMJ
Lund, Reilev, Hallas, Association of nonsteroidal anti-inflammatory drug use and adverse outcomes among patients hospitalized with influenza, JAMA Netw Open
Matute-Bello, Frevert, Martin, Animal models of acute lung injury, Am J Physiol Lung Cell Mol Physiol
Möller, Pruijm, Adler, Scherer, Villiger et al., Chronic NSAID use and long-term decline of renal function in a prospective rheumatoid arthritis cohort study, Ann Rheum Dis
O'hare, Arthritis drug effective in treating sickest COVID-19 patients
The, Group, Dexamethasone in hospitalized patients with COVID-19, N Engl J Med
Trelle, Reichenbach, Wandel, Cardiovascular safety of non-steroidal anti-inflammatory drugs: network meta-analysis, BMJ
Voiriot, Philippot, Elabbadi, Elbim, Chalumeau et al., Risks related to the use of non-steroidal antiinflammatory drugs in community-acquired pneumonia in adult and pediatric Patients, J Clin Med
Von Elm, Altman, Egger, Pocock, Gøtzsche et al., The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies, PLoS Med
Wen, Hsiao, Chan, Lin, Shen et al., Acute respiratory infection and use of nonsteroidal antiinflammatory drugs on risk of acute myocardial infarction: a nationwide case-crossover study, J Infect Dis
DOI record:
{
"DOI": "10.1016/s2665-9913(21)00104-1",
"ISSN": [
"2665-9913"
],
"URL": "http://dx.doi.org/10.1016/S2665-9913(21)00104-1",
"alternative-id": [
"S2665991321001041"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Non-steroidal anti-inflammatory drug use and outcomes of COVID-19 in the ISARIC Clinical Characterisation Protocol UK cohort: a matched, prospective cohort study"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "The Lancet Rheumatology"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/S2665-9913(21)00104-1"
},
{
"label": "CrossRef DOI link to the associated document",
"name": "associatedlink",
"value": "https://doi.org/10.1016/S2665-9913(21)00144-2"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 The Author(s). Published by Elsevier Ltd."
}
],
"author": [
{
"affiliation": [],
"family": "Drake",
"given": "Thomas M",
"sequence": "first"
},
{
"affiliation": [],
"family": "Fairfield",
"given": "Cameron J",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pius",
"given": "Riinu",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Knight",
"given": "Stephen R",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Norman",
"given": "Lisa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Girvan",
"given": "Michelle",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hardwick",
"given": "Hayley E",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Docherty",
"given": "Annemarie B",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thwaites",
"given": "Ryan S",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Openshaw",
"given": "Peter J M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Baillie",
"given": "J Kenneth",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Harrison",
"given": "Ewen M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Semple",
"given": "Malcolm G",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Baillie",
"given": "J Kenneth",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Semple",
"given": "Malcolm G",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Openshaw",
"given": "Peter JM",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Carson",
"given": "Gail",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alex",
"given": "Beatrice",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bach",
"given": "Benjamin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Barclay",
"given": "Wendy S",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bogaert",
"given": "Debby",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chand",
"given": "Meera",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cooke",
"given": "Graham S",
"sequence": "additional"
},
{
"affiliation": [],
"family": "da Silva Filipe",
"given": "Ana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "de Silva",
"given": "Thushan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Docherty",
"given": "Annemarie B",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dunning",
"given": "Jake",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fletcher",
"given": "Tom",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Green",
"given": "Christopher A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Harrison",
"given": "Ewen M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hiscox",
"given": "Julian A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ho",
"given": "Antonia YW",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Horby",
"given": "Peter W",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ijaz",
"given": "Samreen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Khoo",
"given": "Say",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Klenerman",
"given": "Paul",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Law",
"given": "Andrew",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lim",
"given": "Wei Shen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mentzer",
"given": "Alexander J",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Merson",
"given": "Laura",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Meynert",
"given": "Alison M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Moore",
"given": "Shona C",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Noursadeghi",
"given": "Mahdad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Palmarini",
"given": "Massimo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Paxton",
"given": "William A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pollakis",
"given": "Georgios",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Price",
"given": "Nicholas",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rambaut",
"given": "Andrew",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Robertson",
"given": "David L",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Russell",
"given": "Clark D",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sancho-Shimizu",
"given": "Vanessa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Scott",
"given": "Janet T",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sigfrid",
"given": "Louise",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Solomon",
"given": "Tom",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sriskandan",
"given": "Shiranee",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Stuart",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Summers",
"given": "Charlotte",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tedder",
"given": "Richard S",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thompson",
"given": "AA Roger",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thomson",
"given": "Emma C",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thwaites",
"given": "Ryan S",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Turtle",
"given": "Lance CW",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zambon",
"given": "Maria",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Donohue",
"given": "Chloe",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Griffiths",
"given": "Fiona",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hardwick",
"given": "Hayley",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lyons",
"given": "Ruth",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Oosthuyzen",
"given": "Wilna",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Drake",
"given": "Thomas M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fairfield",
"given": "Cameron J",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Knight",
"given": "Stephen R",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mclean",
"given": "Kenneth A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Murphy",
"given": "Derek",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Norman",
"given": "Lisa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pius",
"given": "Riinu",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shaw",
"given": "Catherine A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Connor",
"given": "Marie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dalton",
"given": "Jo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gamble",
"given": "Carrol",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Girvan",
"given": "Michelle",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Halpin",
"given": "Sophie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Harrison",
"given": "Janet",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jackson",
"given": "Clare",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Marsh",
"given": "Laura",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Roberts",
"given": "Stephanie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Saviciute",
"given": "Egle",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Clohisey",
"given": "Sara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hendry",
"given": "Ross",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Law",
"given": "Andrew",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Leeming",
"given": "Gary",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Scott-Brown",
"given": "James",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wham",
"given": "Murray",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Greenhalf",
"given": "William",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McDonald",
"given": "Sara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shaw",
"given": "Victoria",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Keating",
"given": "Seán",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ahmed",
"given": "Katie A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Armstrong",
"given": "Jane A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ashworth",
"given": "Milton",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Asiimwe",
"given": "Innocent G",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bakshi",
"given": "Siddharth",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Barlow",
"given": "Samantha L",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Booth",
"given": "Laura",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Brennan",
"given": "Benjamin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bullock",
"given": "Katie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Carlucci",
"given": "Nicola",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cass",
"given": "Emily",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Catterall",
"given": "Benjamin WA",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Clark",
"given": "Jordan J",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Clarke",
"given": "Emily A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cole",
"given": "Sarah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cooper",
"given": "Louise",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cox",
"given": "Helen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Davis",
"given": "Christopher",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dincarslan",
"given": "Oslem",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Doce Carracedo",
"given": "Alejandra",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dunn",
"given": "Chris",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dyer",
"given": "Philip",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Elliott",
"given": "Angela",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Evans",
"given": "Anthony",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Finch",
"given": "Lorna",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fisher",
"given": "Lewis WS",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Flaherty",
"given": "Lisa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Foster",
"given": "Terry",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Garcia-Dorival",
"given": "Isabel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Greenhalf",
"given": "William",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gunning",
"given": "Philip",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hartley",
"given": "Catherine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Holmes",
"given": "Anthony",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jensen",
"given": "Rebecca L",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jones",
"given": "Christopher B",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jones",
"given": "Trevor R",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Khandaker",
"given": "Shadia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "King",
"given": "Katharine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kiy",
"given": "Robyn T.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Koukorava",
"given": "Chrysa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lake",
"given": "Annette",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lant",
"given": "Suzannah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Latawiec",
"given": "Diane",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lavelle-Langham",
"given": "Lara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lefteri",
"given": "Daniella",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lett",
"given": "Lauren",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Livoti",
"given": "Lucia A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mancini",
"given": "Maria",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Massey",
"given": "Hannah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Maziere",
"given": "Nicole",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McDonald",
"given": "Sarah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McEvoy",
"given": "Laurence",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McLauchlan",
"given": "John",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Metelmann",
"given": "Soeren",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Miah",
"given": "Nahida S",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Middleton",
"given": "Joanna",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mitchell",
"given": "Joyce",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Moore",
"given": "Shona C",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Murphy",
"given": "Ellen G",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Penrice-Randal",
"given": "Rebekah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pilgrim",
"given": "Jack",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Prince",
"given": "Tessa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Reynolds",
"given": "Will",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ridley",
"given": "P. Matthew",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sales",
"given": "Debby",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shaw",
"given": "Victoria E",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shears",
"given": "Rebecca K",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Small",
"given": "Benjamin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Subramaniam",
"given": "Krishanthi S",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Szemiel",
"given": "Agnieska",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Taggart",
"given": "Aislynn",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tanianis-Hughes",
"given": "Jolanta",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thomas",
"given": "Jordan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Trochu",
"given": "Erwan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "van Tonder",
"given": "Libby",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wilcock",
"given": "Eve",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "J. Eunice",
"sequence": "additional"
},
{
"affiliation": [],
"family": "MacLean",
"given": "Alan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McCafferty",
"given": "Sarah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Morrice",
"given": "Kirstie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Murphy",
"given": "Lee",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wrobel",
"given": "Nicola",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Adeniji",
"given": "Kayode",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Agranoff",
"given": "Daniel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Agwuh",
"given": "Ken",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ail",
"given": "Dhiraj",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Aldera",
"given": "Erin L.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alegria",
"given": "Ana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Angus",
"given": "Brian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ashish",
"given": "Abdul",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Atkinson",
"given": "Dougal",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bari",
"given": "Shahedal",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Barlow",
"given": "Gavin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Barnass",
"given": "Stella",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Barrett",
"given": "Nicholas",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bassford",
"given": "Christopher",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Basude",
"given": "Sneha",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Baxter",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Beadsworth",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bernatoniene",
"given": "Jolanta",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Berridge",
"given": "John",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Best",
"given": "Nicola",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bothma",
"given": "Pieter",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Brittain-Long",
"given": "Robin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bulteel",
"given": "Naomi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Burden",
"given": "Tom",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Burtenshaw",
"given": "Andrew",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Caruth",
"given": "Vikki",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chadwick",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chadwick",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chambler",
"given": "Duncan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chee",
"given": "Nigel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Child",
"given": "Jenny",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chukkambotla",
"given": "Srikanth",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Clark",
"given": "Tom",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Collini",
"given": "Paul",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cosgrove",
"given": "Catherine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cupitt",
"given": "Jason",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cutino-Moguel",
"given": "Maria-Teresa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dark",
"given": "Paul",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dawson",
"given": "Chris",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dervisevic",
"given": "Samir",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Donnison",
"given": "Phil",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Douthwaite",
"given": "Sam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "DuRand",
"given": "Ingrid",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dushianthan",
"given": "Ahilanadan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dyer",
"given": "Tristan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Evans",
"given": "Cariad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Eziefula",
"given": "Chi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fegan",
"given": "Chrisopher",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Finn",
"given": "Adam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fullerton",
"given": "Duncan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Garg",
"given": "Sanjeev",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Garg",
"given": "Sanjeev",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Garg",
"given": "Atul",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gkrania-Klotsas",
"given": "Effrossyni",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Godden",
"given": "Jo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Goldsmith",
"given": "Arthur",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Graham",
"given": "Clive",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hardy",
"given": "Elaine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hartshorn",
"given": "Stuart",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Harvey",
"given": "Daniel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Havalda",
"given": "Peter",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hawcutt",
"given": "Daniel B",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hobrok",
"given": "Maria",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hodgson",
"given": "Luke",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hormis",
"given": "Anil",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jacobs",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jain",
"given": "Susan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jennings",
"given": "Paul",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kaliappan",
"given": "Agilan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kasipandian",
"given": "Vidya",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kegg",
"given": "Stephen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kelsey",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kendall",
"given": "Jason",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kerrison",
"given": "Caroline",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kerslake",
"given": "Ian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Koch",
"given": "Oliver",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Koduri",
"given": "Gouri",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Koshy",
"given": "George",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Laha",
"given": "Shondipon",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Laird",
"given": "Steven",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Larkin",
"given": "Susan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Leiner",
"given": "Tamas",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lillie",
"given": "Patrick",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Limb",
"given": "James",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Linnett",
"given": "Vanessa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Little",
"given": "Jeff",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lyttle",
"given": "Mark",
"sequence": "additional"
},
{
"affiliation": [],
"family": "MacMahon",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [],
"family": "MacNaughton",
"given": "Emily",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mankregod",
"given": "Ravish",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Masson",
"given": "Huw",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Matovu",
"given": "Elijah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McCullough",
"given": "Katherine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McEwen",
"given": "Ruth",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Meda",
"given": "Manjula",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mills",
"given": "Gary",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Minton",
"given": "Jane",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mirfenderesky",
"given": "Mariyam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mohandas",
"given": "Kavya",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mok",
"given": "Quen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Moon",
"given": "James",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Moore",
"given": "Elinoor",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Morgan",
"given": "Patrick",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Morris",
"given": "Craig",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mortimore",
"given": "Katherine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Moses",
"given": "Samuel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mpenge",
"given": "Mbiye",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mulla",
"given": "Rohinton",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Murphy",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nagarajan",
"given": "Thapas",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nagel",
"given": "Megan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nelson",
"given": "Mark",
"sequence": "additional"
},
{
"affiliation": [],
"family": "O'Shea",
"given": "Matthew K.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ostermann",
"given": "Marlies",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Otahal",
"given": "Igor",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pais",
"given": "Mark",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Panchatsharam",
"given": "Selva",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Papakonstantinou",
"given": "Danai",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Papineni",
"given": "Padmasayee",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Paraiso",
"given": "Hassan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Patel",
"given": "Brij",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pattison",
"given": "Natalie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pepperell",
"given": "Justin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Peters",
"given": "Mark",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Phull",
"given": "Mandeep",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pintus",
"given": "Stefania",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Post",
"given": "Frank",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Price",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Prout",
"given": "Rachel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rae",
"given": "Nikolas",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Reschreiter",
"given": "Henrik",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Reynolds",
"given": "Tim",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Richardson",
"given": "Neil",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Roberts",
"given": "Mark",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Roberts",
"given": "Devender",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rose",
"given": "Alistair",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rousseau",
"given": "Guy",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ryan",
"given": "Brendan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Saluja",
"given": "Taranprit",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sarah",
"given": "Sarah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shah",
"given": "Aarti",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shankar-Hari",
"given": "Manu",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shanmuga",
"given": "Prad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sharma",
"given": "Anil",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shawcross",
"given": "Anna",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Singh Pooni",
"given": "Jagtur",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sizer",
"given": "Jeremy",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Smith",
"given": "Richard",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Snelson",
"given": "Catherine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Spittle",
"given": "Nick",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Staines",
"given": "Nikki",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Stambach",
"given": "Tom",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Stewart",
"given": "Richard",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Subudhi",
"given": "Pradeep",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Szakmany",
"given": "Tamas",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tatham",
"given": "Kate",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thomas",
"given": "Jo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thompson",
"given": "Chris",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thompson",
"given": "Robert",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tridente",
"given": "Ascanio",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tupper-Carey",
"given": "Darell",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Twagira",
"given": "Mary",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ustianowski",
"given": "Andrew",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vallotton",
"given": "Nick",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vincent-Smith",
"given": "Lisa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Visuvanathan",
"given": "Shico",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vuylsteke",
"given": "Alan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Waddy",
"given": "Sam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wake",
"given": "Rachel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Walden",
"given": "Andrew",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Welters",
"given": "Ingeborg",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Whitehouse",
"given": "Tony",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Whittaker",
"given": "Paul",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Whittington",
"given": "Ashley",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wijesinghe",
"given": "Meme",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Williams",
"given": "Martin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wilson",
"given": "Lawrence",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Winchester",
"given": "Stephen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wiselka",
"given": "Martin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wolverson",
"given": "Adam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wooton",
"given": "Daniel G",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Workman",
"given": "Andrew",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yates",
"given": "Bryan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Young",
"given": "Peter",
"sequence": "additional"
}
],
"container-title": "The Lancet Rheumatology",
"container-title-short": "The Lancet Rheumatology",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"thelancet.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
5,
7
]
],
"date-time": "2021-05-07T23:26:07Z",
"timestamp": 1620429967000
},
"deposited": {
"date-parts": [
[
2021,
11,
7
]
],
"date-time": "2021-11-07T02:01:06Z",
"timestamp": 1636250466000
},
"funder": [
{
"DOI": "10.13039/501100013342",
"doi-asserted-by": "publisher",
"name": "NIHR Imperial Biomedical Research Centre"
},
{
"DOI": "10.13039/100010269",
"doi-asserted-by": "publisher",
"name": "Wellcome Trust"
},
{
"DOI": "10.13039/501100001322",
"doi-asserted-by": "publisher",
"name": "South African Medical Research Council"
},
{
"DOI": "10.13039/501100000272",
"doi-asserted-by": "publisher",
"name": "National Institute for Health Research"
},
{
"DOI": "10.13039/100000865",
"doi-asserted-by": "publisher",
"name": "Bill & Melinda Gates Foundation"
}
],
"indexed": {
"date-parts": [
[
2022,
8,
12
]
],
"date-time": "2022-08-12T13:30:21Z",
"timestamp": 1660311021788
},
"is-referenced-by-count": 29,
"issue": "7",
"issued": {
"date-parts": [
[
2021,
7
]
]
},
"journal-issue": {
"issue": "7",
"published-print": {
"date-parts": [
[
2021,
7
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
7,
1
]
],
"date-time": "2021-07-01T00:00:00Z",
"timestamp": 1625097600000
}
},
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
3,
23
]
],
"date-time": "2021-03-23T00:00:00Z",
"timestamp": 1616457600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2665991321001041?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2665991321001041?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "e498-e506",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
7
]
]
},
"published-print": {
"date-parts": [
[
2021,
7
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"article-title": "WHO guidelines for the use of analgesics in cancer pain",
"author": "Ventafridda",
"first-page": "93",
"journal-title": "Int J Tissue React",
"key": "10.1016/S2665-9913(21)00104-1_bib1",
"volume": "7",
"year": "1985"
},
{
"article-title": "Covid-19: ibuprofen should not be used for managing symptoms, say doctors and scientists",
"author": "Day",
"journal-title": "BMJ",
"key": "10.1016/S2665-9913(21)00104-1_bib3",
"volume": "368",
"year": "2020"
},
{
"article-title": "Covid-19: ibuprofen can be used for symptoms, says UK agency, but reasons for change in advice are unclear",
"author": "Torjesen",
"journal-title": "BMJ",
"key": "10.1016/S2665-9913(21)00104-1_bib4",
"volume": "369",
"year": "2020"
},
{
"article-title": "Non-steroidal anti-inflammatory drugs and covid-19",
"author": "Little",
"journal-title": "BMJ",
"key": "10.1016/S2665-9913(21)00104-1_bib5",
"volume": "368",
"year": "2020"
},
{
"article-title": "Use of non-steroidal anti-inflammatory drugs and risk of death from COVID-19: an OpenSAFELY cohort analysis based on two cohorts",
"author": "Wong",
"journal-title": "Ann Rheum Dis",
"key": "10.1016/S2665-9913(21)00104-1_bib7",
"year": "2021"
},
{
"DOI": "10.1007/s40121-020-00363-w",
"article-title": "Ibuprofen and NSAID use in COVID-19 infected patients is not associated with worse outcomes: a prospective cohort study",
"author": "Abu Esba",
"doi-asserted-by": "crossref",
"first-page": "253",
"journal-title": "Infect Dis Ther",
"key": "10.1016/S2665-9913(21)00104-1_bib8",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1111/cts.12904",
"article-title": "Association between prescribed ibuprofen and severe COVID-19 infection: a nationwide register-based cohort study",
"author": "Kragholm",
"doi-asserted-by": "crossref",
"first-page": "1103",
"journal-title": "Clin Transl Sci",
"key": "10.1016/S2665-9913(21)00104-1_bib9",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.3390/jcm9082586",
"article-title": "Prior routine use of non-steroidal anti-inflammatory drugs (NSAIDs) and important outcomes in hospitalised patients with COVID-19",
"author": "Bruce",
"doi-asserted-by": "crossref",
"journal-title": "J Clin Med",
"key": "10.1016/S2665-9913(21)00104-1_bib10",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1371/journal.pmed.1003308",
"article-title": "Adverse outcomes and mortality in users of non-steroidal anti-inflammatory drugs who tested positive for SARS-CoV-2: a Danish nationwide cohort study",
"author": "Lund",
"doi-asserted-by": "crossref",
"journal-title": "PLoS Med",
"key": "10.1016/S2665-9913(21)00104-1_bib11",
"volume": "17",
"year": "2020"
},
{
"article-title": "Association between NSAIDs use and adverse clinical outcomes among adults hospitalized with COVID-19 in South Korea: a nationwide study",
"author": "Jeong",
"journal-title": "Clin Infect Dis",
"key": "10.1016/S2665-9913(21)00104-1_bib12",
"year": "2020"
},
{
"DOI": "10.1002/art.41593",
"article-title": "Non-steroidal anti-inflammatory drugs and susceptibility to COVID-19",
"author": "Chandan",
"doi-asserted-by": "crossref",
"first-page": "731",
"journal-title": "Arthritis Rheumatol",
"key": "10.1016/S2665-9913(21)00104-1_bib13",
"volume": "73",
"year": "2021"
},
{
"DOI": "10.1136/annrheumdis-2013-204078",
"article-title": "Chronic NSAID use and long-term decline of renal function in a prospective rheumatoid arthritis cohort study",
"author": "Möller",
"doi-asserted-by": "crossref",
"first-page": "718",
"journal-title": "Ann Rheum Dis",
"key": "10.1016/S2665-9913(21)00104-1_bib14",
"volume": "74",
"year": "2015"
},
{
"DOI": "10.2165/00002018-199920060-00006",
"article-title": "Prophylaxis and treatment of NSAID-induced gastroduodenal disorders",
"author": "La Corte",
"doi-asserted-by": "crossref",
"first-page": "527",
"journal-title": "Drug Saf",
"key": "10.1016/S2665-9913(21)00104-1_bib15",
"volume": "20",
"year": "1999"
},
{
"DOI": "10.1016/j.rmed.2016.12.005",
"article-title": "Prehospital NSAIDs use prolong hospitalization in patients with pleuro-pulmonary infection",
"author": "Kotsiou",
"doi-asserted-by": "crossref",
"first-page": "28",
"journal-title": "Respir Med",
"key": "10.1016/S2665-9913(21)00104-1_bib16",
"volume": "123",
"year": "2017"
},
{
"article-title": "Non-steroidal anti-inflammatory drugs may worsen the course of community-acquired pneumonia: a cohort study",
"author": "Basille",
"journal-title": "Eur Respir J",
"key": "10.1016/S2665-9913(21)00104-1_bib17",
"volume": "48",
"year": "2016"
},
{
"DOI": "10.1001/jamanetworkopen.2020.13880",
"article-title": "Association of nonsteroidal anti-inflammatory drug use and adverse outcomes among patients hospitalized with influenza",
"author": "Lund",
"doi-asserted-by": "crossref",
"journal-title": "JAMA Netw Open",
"key": "10.1016/S2665-9913(21)00104-1_bib18",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.3390/jcm8060786",
"article-title": "Risks related to the use of non-steroidal anti-inflammatory drugs in community-acquired pneumonia in adult and pediatric Patients",
"author": "Voiriot",
"doi-asserted-by": "crossref",
"first-page": "786",
"journal-title": "J Clin Med",
"key": "10.1016/S2665-9913(21)00104-1_bib19",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.1093/infdis/jiw603",
"article-title": "Acute respiratory infection and use of nonsteroidal anti-inflammatory drugs on risk of acute myocardial infarction: a nationwide case-crossover study",
"author": "Wen",
"doi-asserted-by": "crossref",
"first-page": "503",
"journal-title": "J Infect Dis",
"key": "10.1016/S2665-9913(21)00104-1_bib20",
"volume": "215",
"year": "2017"
},
{
"DOI": "10.1136/bmj.f6041",
"article-title": "Ibuprofen, paracetamol, and steam for patients with respiratory tract infections in primary care: pragmatic randomised factorial trial",
"author": "Little",
"doi-asserted-by": "crossref",
"journal-title": "BMJ",
"key": "10.1016/S2665-9913(21)00104-1_bib21",
"volume": "347",
"year": "2013"
},
{
"DOI": "10.1152/ajplung.00010.2008",
"article-title": "Animal models of acute lung injury",
"author": "Matute-Bello",
"doi-asserted-by": "crossref",
"first-page": "L379",
"journal-title": "Am J Physiol Lung Cell Mol Physiol",
"key": "10.1016/S2665-9913(21)00104-1_bib22",
"volume": "295",
"year": "2008"
},
{
"DOI": "10.1371/journal.pmed.0040296",
"article-title": "The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies",
"author": "von Elm",
"doi-asserted-by": "crossref",
"first-page": "e296",
"journal-title": "PLoS Med",
"key": "10.1016/S2665-9913(21)00104-1_bib25",
"volume": "4",
"year": "2007"
},
{
"DOI": "10.1016/j.jbi.2008.08.010",
"article-title": "Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support",
"author": "Harris",
"doi-asserted-by": "crossref",
"first-page": "377",
"journal-title": "J Biomed Inform",
"key": "10.1016/S2665-9913(21)00104-1_bib26",
"volume": "42",
"year": "2009"
},
{
"author": "Ling",
"key": "10.1016/S2665-9913(21)00104-1_bib28"
},
{
"author": "Fishgar",
"key": "10.1016/S2665-9913(21)00104-1_bib29"
},
{
"DOI": "10.1016/S2213-2600(20)30116-8",
"article-title": "Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?",
"author": "Fang",
"doi-asserted-by": "crossref",
"first-page": "e21",
"journal-title": "Lancet Respir Med",
"key": "10.1016/S2665-9913(21)00104-1_bib31",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1136/bmj.c7086",
"article-title": "Cardiovascular safety of non-steroidal anti-inflammatory drugs: network meta-analysis",
"author": "Trelle",
"doi-asserted-by": "crossref",
"journal-title": "BMJ",
"key": "10.1016/S2665-9913(21)00104-1_bib32",
"volume": "342",
"year": "2011"
},
{
"DOI": "10.1016/j.jaci.2020.05.008",
"article-title": "Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19",
"author": "Herold",
"doi-asserted-by": "crossref",
"first-page": "128",
"journal-title": "J Allergy Clin Immunol",
"key": "10.1016/S2665-9913(21)00104-1_bib34",
"volume": "146",
"year": "2020"
},
{
"DOI": "10.1186/s10020-020-00230-x",
"article-title": "IP-10 and MCP-1 as biomarkers associated with disease severity of COVID-19",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "97",
"journal-title": "Mol Med",
"key": "10.1016/S2665-9913(21)00104-1_bib35",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1016/j.rmed.2003.10.012",
"article-title": "In vitro study of regulation of IL-6 production in bronchiectasis",
"author": "Ho",
"doi-asserted-by": "crossref",
"first-page": "334",
"journal-title": "Respir Med",
"key": "10.1016/S2665-9913(21)00104-1_bib36",
"volume": "98",
"year": "2004"
},
{
"DOI": "10.1189/jlb.4A0214-093RR",
"article-title": "Characterization of lung inflammation and its impact on macrophage function in aging",
"author": "Canan",
"doi-asserted-by": "crossref",
"first-page": "473",
"journal-title": "J Leukoc Biol",
"key": "10.1016/S2665-9913(21)00104-1_bib37",
"volume": "96",
"year": "2014"
},
{
"DOI": "10.1056/NEJMoa2021436",
"article-title": "Dexamethasone in hospitalized patients with COVID-19",
"doi-asserted-by": "crossref",
"first-page": "693",
"journal-title": "N Engl J Med",
"key": "10.1016/S2665-9913(21)00104-1_bib38",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2100433",
"article-title": "Interleukin-6 Receptor Antagonists in Critically Ill Patients with Covid-19",
"doi-asserted-by": "crossref",
"first-page": "1491",
"journal-title": "N Engl J Med",
"key": "10.1016/S2665-9913(21)00104-1_bib39",
"volume": "384",
"year": "2021"
},
{
"article-title": "Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): preliminary results of a randomised, controlled, open-label, platform trial",
"author": "Horby",
"journal-title": "medRxiv",
"key": "10.1016/S2665-9913(21)00104-1_bib40",
"year": "2021"
},
{
"author": "O'Hare",
"key": "10.1016/S2665-9913(21)00104-1_bib41"
}
],
"reference-count": 34,
"references-count": 34,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2665991321001041"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Immunology",
"Immunology and Allergy",
"Rheumatology"
],
"subtitle": [],
"title": "Non-steroidal anti-inflammatory drug use and outcomes of COVID-19 in the ISARIC Clinical Characterisation Protocol UK cohort: a matched, prospective cohort study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "3"
}