A Retrospective Review: Famotidine Use Is Not Associated With Improved Outcomes in Hospitalized Patients With COVID-19
et al., American Journal of Gastroenterology, doi:10.14309/01.ajg.0000778736.01714.cd, Oct 2021
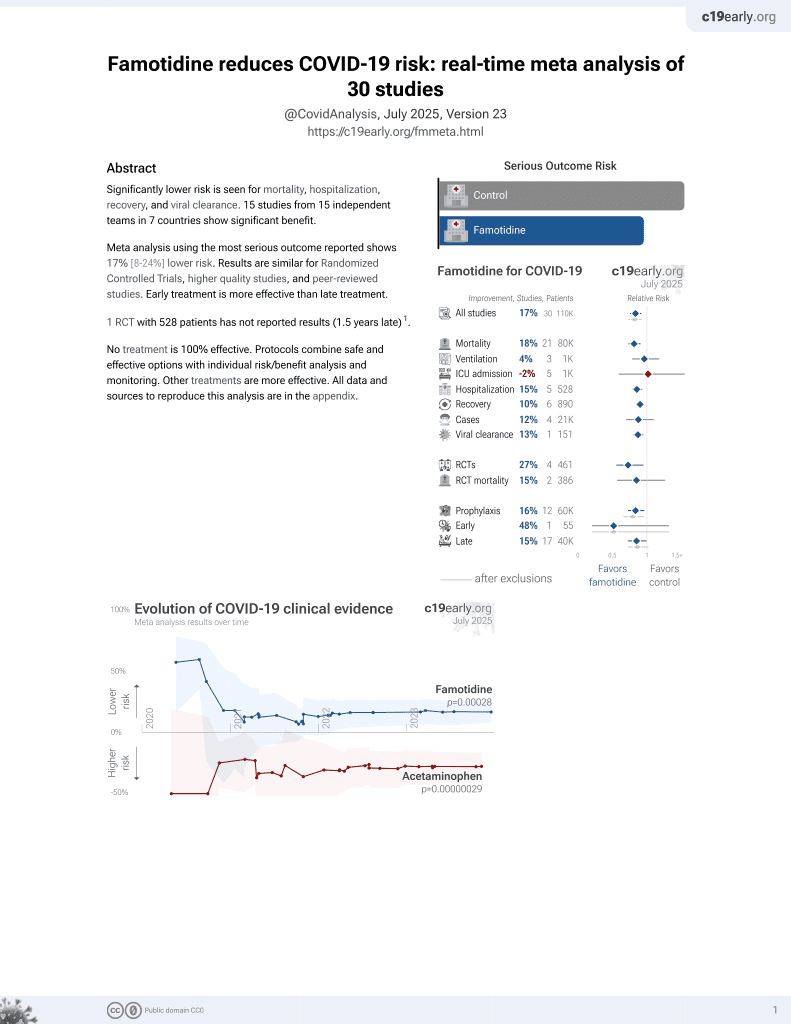
Famotidine for COVID-19
29th treatment shown to reduce risk in
October 2021, now with p = 0.00028 from 30 studies, recognized in 2 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 489 COVID+ hospitalized patients in the USA, showing higher mortality with famotidine treatment.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
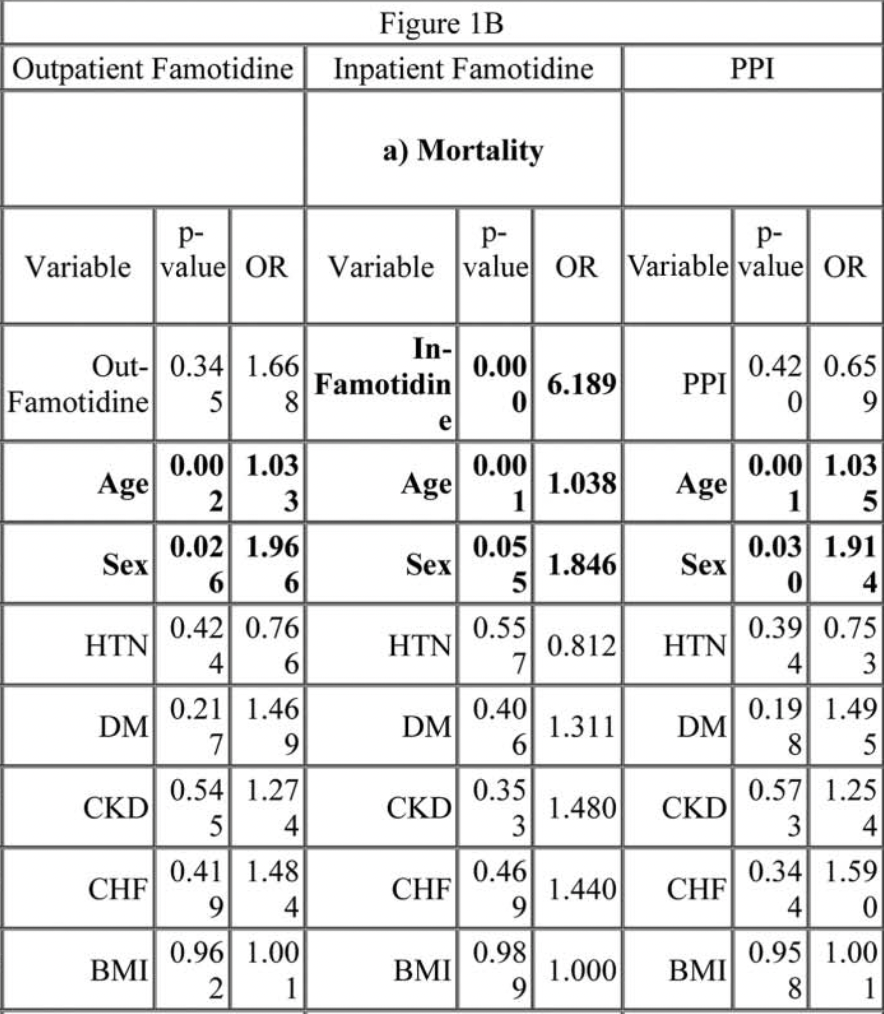
risk of death, 518.9% higher, OR 6.19, p < 0.001, treatment 137, control 352, RR approximated with OR.
|
|
risk of ICU admission, 2389.6% higher, OR 24.90, p < 0.001, treatment 137, control 352, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Stolow et al., 31 Oct 2021, retrospective, USA, peer-reviewed, 9 authors.
Abstract: S598
Abstracts
[1299] Table 1. Survey Demographics & Barriers assessed.
[1300] Table 1. Reasons for Ordering FIT pre vs post intervention.
evaluation. Despite these indications for FIT, we realized there were numerous instances at the
VAMC in which FIT was obtained inappropriately inpatient, such as in overt GI bleeding. This
quality improvement (QI) project aimed to identify and reduce the situations of inpatient FIT
usage, to educate on the proper indications for FIT, and to evaluate the impact on patient
outcomes.
Methods: A retrospective chart review was performed of 1 year of inpatient FIT usage. Subsequently, weekly pre-intervention questionaire surveys were distributed over 3 months to various
VA healthcare providers to gauge baseline understanding of FIT. Then, teaching and educational
handouts were provided (Figure 1). Data post intervention was collected over a 3 month period
and analyzed.
Results: A total of 400 FITs (on average 33/month) were ordered pre-intervention with 20% done on
patients with active GI bleeds: abdominal pain and diarrhea were other reasons. Pre-intervention surveys
were obtained from 74 individuals; 13% of respondents thought FIT was for GI bleeding while 7% were
unsure of FIT indication. Post educational intervention, 89 FITs (on average 30/month) were collected,
with the majority of ordering providers of medicine specialty. Anemia was the most common indication
for FIT at 64% (Table 1). Of the 1FITs, GI was only consulted on 76% of these cases post intervention in
which colonoscopy was performed in 38% of these cases. 31% of inpatients with 1FITs were critically ill
with multiple comorbidities, had no overt GI bleeding, and thus colonoscopy was deferred. Among the
FIT1 patients whom did not undergo endoscopic evaluation, about 40% had died from non GI related
causes by completion of the study.
Conclusion: FIT is overutilized in the hospital setting and it’s inpatient role is limited. Despite the
lack of difference in the number of FITs ordered pre and post educational intervention, our data
suggests 1FITs did not affect patient outcome or clinical management. We propose decreased usage
of FIT in the acute inpatient setting with a plan for continued educational intervention and setting
forth limitations to ordering providers.
S1300
The Wrong FITting: A Quality Improvement Project to Reduce Inpatient Fecal Immunochemical
Test (FIT) Usage at the Veterans Affairs Medical Center (VAMC)
Christine Chen, DO, Robert Taylor, MD, Tony Brar, MD, Patrick Stoner, DO, Adam Younis, MD,
Jake Wilson, MD, Nicole Ruiz, MD, George Marek, MD, PhD, Nakechand Pooran, MD.
University of Florida, Gainesville, FL.
Introduction: Fecal immunochemical test (FIT) utilizes antibodies to detect the globin (protein)
part of hemoglobin. Indications for FIT include screening for colorectal cancer (CRC) and in cases
of anemia without any overt gastrointestinal (GI) bleeding. An abnormal FIT could suggest the
presence of CRC, polyps, hemorrhoids, or ulcers and should be pursued with a colonoscopy for
[1300] Figure 1. Educational handouts on FIT usage were provided to healthcare providers.
The American Journal of GASTROENTEROLOGY
S1301 Presidential Poster Award
A Retrospective Review: Famotidine Use Is Not Associated With Improved Outcomes in
Hospitalized Patients With..
DOI record:
{
"DOI": "10.14309/01.ajg.0000778736.01714.cd",
"ISSN": [
"0002-9270",
"1572-0241"
],
"URL": "http://dx.doi.org/10.14309/01.ajg.0000778736.01714.cd",
"author": [
{
"affiliation": [],
"family": "Stolow",
"given": "Eugene",
"sequence": "first"
},
{
"affiliation": [],
"family": "El-Kurdi",
"given": "Bara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Harrington",
"given": "Allison",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Keiser",
"given": "Sylvia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kuwelker",
"given": "Saatchi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tejani",
"given": "Aziz",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Acosta",
"given": "Phillip",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Imam",
"given": "Zaid",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Echavarria",
"given": "Juan",
"sequence": "additional"
}
],
"container-title": [
"American Journal of Gastroenterology"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
10,
24
]
],
"date-time": "2021-10-24T15:54:00Z",
"timestamp": 1635090840000
},
"deposited": {
"date-parts": [
[
2021,
10,
24
]
],
"date-time": "2021-10-24T15:54:23Z",
"timestamp": 1635090863000
},
"indexed": {
"date-parts": [
[
2022,
1,
5
]
],
"date-time": "2022-01-05T17:00:36Z",
"timestamp": 1641402036413
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "print",
"value": "0002-9270"
},
{
"type": "electronic",
"value": "1572-0241"
}
],
"issue": "1",
"issued": {
"date-parts": [
[
2021,
10
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2021
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://journals.lww.com/10.14309/01.ajg.0000778736.01714.cd",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "276",
"original-title": [],
"page": "S598-S598",
"prefix": "10.14309",
"published": {
"date-parts": [
[
2021,
10
]
]
},
"published-print": {
"date-parts": [
[
2021,
10
]
]
},
"publisher": "Ovid Technologies (Wolters Kluwer Health)",
"reference-count": 0,
"references-count": 0,
"relation": {},
"score": 1,
"short-container-title": [
"Am J Gastroenterol"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Gastroenterology",
"Hepatology"
],
"subtitle": [],
"title": [
"S1301 A Retrospective Review: Famotidine Use Is Not Associated With Improved Outcomes in Hospitalized Patients With COVID-19"
],
"type": "journal-article",
"volume": "116"
}