Identification of Clinical Response Predictors of Tocilizumab Treatment in Patients with Severe COVID-19 Based on Single-Center Experience
et al., Journal of Clinical Medicine, doi:10.3390/jcm12062429, Mar 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Prospective study of 120 severe COVID-19 patients in Poland treated with tocilizumab, showing significantly higher mortality with low vitamin D levels.
This is the 166th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of death, 85.5% lower, OR 0.14, p = 0.003, cutoff 27ng/mL, inverted to make OR<1 favor high D levels (≥27ng/mL), RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Schmidt et al., 22 Mar 2023, prospective, Poland, peer-reviewed, 4 authors, study period 4 February, 2021 - 31 December, 2021.
Contact: wiktorpawelschmidt@gmail.com (corresponding author).
Identification of Clinical Response Predictors of Tocilizumab Treatment in Patients with Severe COVID-19 Based on Single-Center Experience
Journal of Clinical Medicine, doi:10.3390/jcm12062429
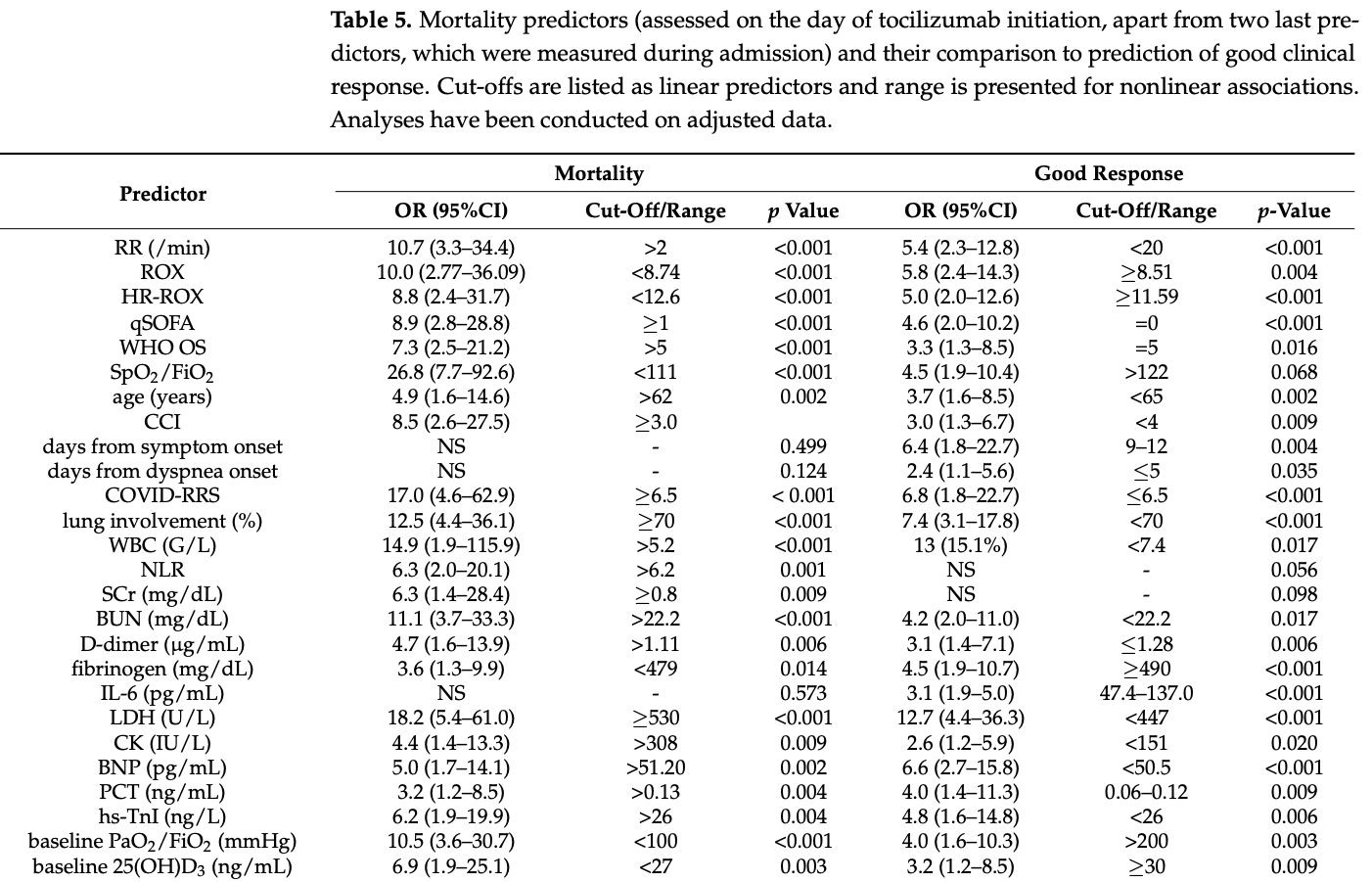
Hyperinflammation in COVID-19 plays a crucial role in pathogenesis and severity; thus, many immunomodulatory agents are applied in its treatment. We aimed to identify good clinical response predictors of tocilizumab (TCZ) treatment in severe COVID-19, among clinical, laboratory, and radiological variables. We conducted a prospective, observational study with 120 patients with severe COVID-19 not improving despite dexamethasone (DEX) treatment. We used parametric and non-parametric statistics, univariate logistic regression, receiver operating characteristic (ROC) curves, and nonlinear factors tertile analysis. In total, 86 (71.7%) patients achieved the primary outcome of a good clinical response to TCZ. We identified forty-nine predictive factors with potential utility in patient selection and treatment monitoring. The strongest included time from symptom onset between 9 and 12 days, less than 70% of estimated radiological lung involvement, and lower activity of lactate dehydrogenase. Additional predictors were associated with respiratory function, vitamin D concentration, comorbidities, and inflammatory/organ damage biomarkers. Adverse events analysis proved the safety of such a regimen. Our study confirmed that using TCZ early in the hyperinflammatory phase, before severe respiratory failure development, is most beneficial. Considering the described predictive factors, employing simple and widely available laboratory, radiological, and clinical tools can optimize patient selection for immunomodulatory treatment with TCZ.
Supplementary Materials: The following supporting information can be downloaded at: https://www. mdpi.com/article/10.3390/jcm12062429/s1, Table S1 . Definitions of additional outcomes of the study. Table S2 . Full demographic and initial clinical characteristics of study group, presented as n (%), mean (±SD) or median (Q1-Q3). Table S3 . Extended clinical characteristics of study groups, presented as median (Q1-Q3). p values were derived with Mann-Whitney U test. Table S4 . Extended laboratory characteristics of studied groups and outcomes, presented as median (Q1-Q3). p values were derived with Mann-Whitney U test. Table S5 . Outcomes and their prevalence upon administration and occurrence after treatment with tocilizumab in studied groups. Author Contributions: P.L. and K.P.-B. supervised the whole project. All authors participated in the conception and design of the study. P.L. conceived the analysis and W.S. designed it. Collection of data was performed by B.J. and W.S. Data were analyzed by W.S. and interpreted by W.S. and P.L. W.S. and B.J. were responsible for drafting the article, whereas K.P.-B. and P.L. gave critical revisions. All authors collectively gave final approval of the version of the article to be published. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest: The authors declare no conflict of interest.
References
Aithal, Watkins, Andrade, Larrey, Molokhia et al., Case Definition and Phenotype Standardization in Drug-Induced Liver Injury, Clin. Pharmacol. Ther, doi:10.1038/clpt.2011.58
Alqahtani, Albilal, Mahmoud, Aldibasi, Alharbi et al., Outcomes associated with tocilizumab with or without corticosteroid versus dexamethasone for treatment of patients with severe to critical COVID-19 pneumonia, J. Infect. Public Health, doi:10.1016/j.jiph.2021.11.017
Belen-Apak, Sarıalio Glu, Pulmonary intravascular coagulation in COVID-19: Possible pathogenesis and recommendations on anticoagulant/thrombolytic therapy, J. Thromb. Thrombolysis, doi:10.1007/s11239-020-02129-0
Berlin, Gulick, Martinez, Severe COVID-19, N. Engl. J. Med, doi:10.1056/NEJMcp2009575
Borczuk, Salvatore, Seshan, Patel, Bussel et al., COVID-19 pulmonary pathology: A multi-institutional autopsy cohort from Italy and New York City, Mod. Pathol, doi:10.1038/s41379-020-00661-1
Broman, Feuth, Vuorinen, Valtonen, Hohenthal et al., Early administration of tocilizumab in hospitalized COVID-19 patients with elevated inflammatory markers
Bryce, Grimes, Pujadas, Ahuja, Beasley et al., Pathophysiology of SARS-CoV-2: The Mount Sinai COVID-19 autopsy experience, Mod. Pathol, doi:10.1038/s41379-021-00793-y
Campins, Boixeda, Perez-Cordon, Aranega, Lopera et al., Early tocilizumab treatment could improve survival among COVID-19 patients, Clin. Exp. Rheumatol
Caricchio, Gallucci, Dass, Zhang, Gallucci et al., Preliminary predictive criteria for COVID-19 cytokine storm, Ann. Rheum. Dis, doi:10.1136/annrheumdis-2020-218323
Catoire, Tellier, De La Rivière, Beauvieux, Valdenaire et al., Assessment of the SpO 2 /FiO 2 ratio as a tool for hypoxemia screening in the emergency department, Am. J. Emerg. Med, doi:10.1016/j.ajem.2021.01.092
Charlson, Pompei, Ales, Mackenzie, A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation, J. Chronic Dis, doi:10.1016/0021-9681(87)90171-8
Cordeanu, Duthil, Severac, Lambach, Tousch et al., Prognostic Value of Troponin Elevation in COVID-19 Hospitalized Patients, J. Clin. Med, doi:10.3390/jcm9124078
D'ecclesiis, Gavioli, Martinoli, Raimondi, Chiocca et al., Vitamin D and SARS-CoV2 infection, severity and mortality: A systematic review and meta-analysis, PLoS ONE, doi:10.1371/journal.pone.0268396
De Benedetto, Lupia, Shbaklo, Bianchi, Concialdi et al., Prognostic evaluation of Acinetobacter baumannii ventilator associated pneumonia in COVID-19, Infez. Med, doi:10.53854/liim-3004-12
Di Micco, Russo, Carannante, Imparato, Cardillo et al., Prognostic Value of Fibrinogen among COVID-19 Patients Admitted to an Emergency Department: An Italian Cohort Study, J. Clin. Med, doi:10.3390/jcm9124134
El, Jamal, Pujadas, Ramos, Bryce et al., Tissue-based SARS-CoV-2 detection in fatal COVID-19 infections: Sustained direct viral-induced damage is not necessary to drive disease progression, Hum. Pathol, doi:10.1016/j.humpath.2021.04.012
Elm, Altman, Egger, Pocock, Gøtzsche et al., The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies, Ann. Intern. Med, doi:10.7326/0003-4819-147-8-200710160-00010
Fajgenbaum, June, Cytokine Storm, N. Engl. J. Med, doi:10.1056/NEJMra2026131
Fathi, Vakili, Sayehmiri, Mohamadkhani, Hajiesmaeili et al., The prognostic value of comorbidity for the severity of COVID-19: A systematic review and meta-analysis study, PLoS ONE, doi:10.1371/journal.pone.0246190
Fialek, Pruc, Smereka, Jas, Rahnama-Hezavah et al., Diagnostic value of lactate dehydrogenase in COVID-19: A systematic review and meta-analysis, Cardiol. J, doi:10.5603/CJ.a2022.0056
Fisher, Raymundo, Monteforte, Taub, Go, Tocilizumab in the treatment of critical COVID-19 pneumonia: A retrospective cohort study of mechanically ventilated patients, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.12.021
Flisiak, Horban, Jaroszewicz, Kozielewicz, Mastalerz-Migas et al., Management of SARS-CoV-2 infection: Recommendations of the Polish Association of Epidemiologists and Infectiologists as of 23 February 2022, Pol. Arch. Intern. Med, doi:10.20452/pamw.16230
Flisiak, Horban, Jaroszewicz, Kozielewicz, Pawłowska et al., Recommendations of management in SARS-CoV-2 infection of the Polish Association of Epidemiologists and Infectiologists, Pol. Arch. Intern. Med, doi:10.20452/pamw.15270
Flisiak, Jaroszewicz, Rogalska, Łapi Ński, Berkan-Kawi Ńska et al., Tocilizumab Improves the Prognosis of COVID-19 in Patients with High IL-6, J. Clin. Med, doi:10.3390/jcm10081583
Freund, Lemachatti, Krastinova, Van Laer, Claessens et al., Prognostic Accuracy of Sepsis-3 Criteria for In-Hospital Mortality Among Patients with Suspected Infection Presenting to the Emergency Department, JAMA, doi:10.1001/jama.2016.20329
Goh, Chai, Ong, Sewa, Phua et al., Early prediction of high flow nasal cannula therapy outcomes using a modified ROX index incorporating heart rate, J. Intensiv. Care, doi:10.1186/s40560-020-00458-z
Gungor, Atici, Baycan, Alici, Ozturk et al., Elevated D-dimer levels on admission are associated with severity and increased risk of mortality in COVID-19: A systematic review and meta-analysis, Am. J. Emerg. Med, doi:10.1016/j.ajem.2020.09.018
Hansell, Bankier, Macmahon, Mcloud, Müller et al., Society: Glossary of Terms for Thoracic Imaging, Radiology, doi:10.1148/radiol.2462070712
Henderson, Canna, Schulert, Volpi, Lee et al., On the Alert for Cytokine Storm: Immunopathology in COVID-19, Arthritis Rheumatol
Henry, Aggarwal, Wong, Benoit, Vikse et al., Lactate dehydrogenase levels predict coronavirus disease 2019 (COVID-19) severity and mortality: A pooled analysis, Am. J. Emerg. Med, doi:10.1016/j.ajem.2020.05.073
Hermine, Mariette, Tharaux, Resche-Rigon, Porcher et al., Effect of Tocilizumab vs Usual Care in Adults Hospitalized With COVID-19 and Moderate or Severe Pneumonia: A Randomized Clinical Trial, JAMA Intern. Med, doi:10.1001/jamainternmed.2020.6820
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet, doi:10.1016/S0140-6736(20)30183-5
Iba, Warkentin, Thachil, Levi, Levy, Proposal of the Definition for COVID-19-Associated Coagulopathy, J. Clin. Med, doi:10.3390/jcm10020191
Kaneko, Kameda, Ikeda, Ishii, Murakami et al., Tocilizumab in patients with adult-onset still's disease refractory to glucocorticoid treatment: A randomised, double-blind, placebo-controlled phase III trial, Ann. Rheum. Dis, doi:10.1136/annrheumdis-2018-213920
Kessel, Vollenberg, Masjosthusmann, Hinze, Wittkowski et al., Discrimination of COVID-19 From Inflammation-Induced Cytokine Storm Syndromes Using Disease-Related Blood Biomarkers, Arthritis Rheumatol, doi:10.1002/art.41763
Khwaja, KDIGO Clinical Practice Guidelines for Acute Kidney Injury, Nephron Clin. Pr, doi:10.1159/000339789
Knight, Caricchio, Casanova, Combes, Diamond et al., The intersection of COVID-19 and autoimmunity, J. Clin. Investig, doi:10.1172/JCI154886
Konstantinides, Meyer, Becattini, Bueno, Geersing et al., ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS), Eur. Heart J, doi:10.1093/eurheartj/ehz405
Kosior, Undas, Kopeć, Hryniewiecki, Torbicki et al., Guidance for anticoagulation management in venous thromboembolism during the coronavirus disease 2019 pandemic in Poland: An expert opinion of the Section on Pulmonary Circulation of the Polish Cardiac Society, Kardiologia Polska, doi:10.33963/KP.15425
Kumar, Karn, Trivedi, Kumar, Chauhan et al., Procalcitonin as a predictive marker in COVID-19: A systematic review and meta-analysis, PLoS ONE
Kwo, Cohen, Lim, Acg, Clinical Guideline: Evaluation of Abnormal Liver Chemistries, Off. J. Am. Coll. Gastroenterol, doi:10.1038/ajg.2016.517
Le, Li, Yuan, Shord, Nie et al., FDA Approval Summary: Tocilizumab for Treatment of Chimeric Antigen Receptor T Cell-Induced Severe or Life-Threatening Cytokine Release Syndrome, Oncologist, doi:10.1634/theoncologist.2018-0028
Leisman, Ronner, Pinotti, Taylor, Sinha et al., Cytokine elevation in severe and critical COVID-19: A rapid systematic review, meta-analysis, and comparison with other inflammatory syndromes, Lancet Respir. Med, doi:10.1016/S2213-2600(20)30404-5
Leszczy Ński, COVID-19: A short message to rheumatologists, Rheumatology, doi:10.5114/reum.2020.96685
Liu, Xie, Chen, Zhang, Cheng et al., Kidney Function Indicators Predict Adverse Outcomes of COVID-19, Med, doi:10.1016/j.medj.2020.09.001
Long, Yang, Li, Li, Chen et al., Abnormal Fibrinogen Level as a Prognostic Indicator in Coronavirus Disease Patients: A Retrospective Cohort Study, Front. Med, doi:10.3389/fmed.2021.687220
Manson, Crooks, Naja, Ledlie, Goulden et al., COVID-19-associated hyperinflammation and escalation of patient care: A retrospective longitudinal cohort study, Lancet Rheumatol, doi:10.1016/S2665-9913(20)30275-7
Marshall, Murthy, Diaz, Adhikari, Angus et al., WHO Working Group on the Clinical Characterisation and Management of COVID-19 infection A Minimal Common Outcome Measure Set for COVID-19 Clinical Research, Lancet Infect. Dis, doi:10.1016/S1473-3099(20)30483-7
Mazzolai, Aboyans, Ageno, Agnelli, Alatri et al., Diagnosis and management of acute deep vein thrombosis: A joint consensus document from the European Society of Cardiology working groups of aorta and peripheral vascular diseases and pulmonary circulation and right ventricular function, Eur. Heart J, doi:10.1093/eurheartj/ehx003
Mcgonagle, Kearney, O'regan, O'donnell, Quartuccio et al., Therapeutic implications of ongoing alveolar viral replication in COVID-19, Lancet Rheumatol, doi:10.1016/S2665-9913(21)00322-2
Mcnarry, Goldhill, Simple bedside assessment of level of consciousness: Comparison of two simple assessment scales with the Glasgow Coma scale, Anaesthesia, doi:10.1111/j.1365-2044.2004.03526.x
Medina-Hernández, Pérez-Navarro, Hernández-Ruiz, Villalobos-Osnaya, Hernández-Medel et al., Changes in lactate dehydrogenase on admission throughout the COVID-19 pandemic and possible impacts on prognostic capability, Biomarkers Med, doi:10.2217/bmm-2022-0364
Mehta, Fajgenbaum, Is severe COVID-19 a cytokine storm syndrome: A hyperinflammatory debate, Curr. Opin. Rheumatol, doi:10.1097/BOR.0000000000000822
Mehta, Haskard, Laffan, Chambers, Hunt, Thromboses and COVID-19: Reducing inflammation in addition to thromboprophylaxis, Lancet Rheumatol, doi:10.1016/S2665-9913(21)00003-5
Michael, Walton, Westenberg, García-Azorín, Singh et al., Consensus Clinical Guidance for Diagnosis and Management of Adult COVID-19 Encephalopathy Patients, J. Neuropsychiatry, doi:10.1176/appi.neuropsych.22010002
Millán, Mesa-Plaza, Guerrero-Santillán, Morales-Ortega, Bernal-Bello et al., Prognostic factors and combined use of tocilizumab and corticosteroids in a Spanish cohort of elderly COVID-19 patients, J. Med. Virol, doi:10.1002/jmv.27488
Minihan, Mcauliffe, Powell, Wong, Wilkie et al., Association between tocilizumab treatment of hyperinflammatory patients with COVID-19 in a critical care setting and elevated incidence of hospital-acquired bacterial and invasive fungal infections, J. Hosp. Infect, doi:10.1016/j.jhin.2022.04.007
Mutua, Henry, Von Csefalvay, Cheruiyot, Vikse et al., Tocilizumab in Addition to Standard of Care in the Management of COVID-19: A Meta-Analysis of RCTs, Acta Biomed, doi:10.23750/abm.v93i1.12208
Naik, Puri, Kajal, Mahajan, Bhalla et al., High-Dose Dexamethasone Versus Tocilizumab in Moderate to Severe COVID-19 Pneumonia: A Randomized Controlled Trial, Cureus, doi:10.7759/cureus.20353
Nauffal, Achanta, Goldhaber, Piazza, Association of ABO blood group type with cardiovascular events in COVID-19, J. Thromb. Thrombolysis, doi:10.1007/s11239-020-02364-5
Nienhold, Ciani, Koelzer, Tzankov, Haslbauer et al., Two distinct immunopathological profiles in autopsy lungs of COVID-19, Nat. Commun, doi:10.1038/s41467-020-18854-2
Olewicz-Gawlik, Ginter-Matuszewska, Kami Ński, Adamek, Bura et al., Changes in Inflammatory Markers after Administration of Tocilizumab in COVID-19: A Single-Center Retrospective Study, J. Clin. Med, doi:10.3390/jcm11010107
Patel, Saxena, Mehta, Recent updates in the clinical trials of therapeutic monoclonal antibodies targeting cytokine storm for the management of COVID-19, Heliyon, doi:10.1016/j.heliyon.2021.e06158
Peker, Şener, Aydo Gmuş, Antinuclear antibodies (ANAs) detected by indirect immunofluorescence (IIF) method in acute COVID-19 infection; future roadmap for laboratory diagnosis, J. Immunol. Methods, doi:10.1016/j.jim.2021.113174
Peng, Fu, Mei, Zheng, Liang et al., Efficacy and secondary infection risk of tocilizumab, sarilumab and anakinra in COVID-19 patients: A systematic review and meta-analysis, Rev. Med. Virol, doi:10.1002/rmv.2295
Petrelli, Cherri, Ghidini, Perego, Ghidini et al., Tocilizumab as treatment for COVID-19: A systematic review and meta-analysis, World J. Methodol, doi:10.5662/wjm.v11.i3.95
Piscoya, Del Riego, Cerna-Viacava, Rocco, Roman et al., Efficacy and harms of tocilizumab for the treatment of COVID-19 patients: A systematic review and meta-analysis, PLoS ONE, doi:10.1371/journal.pone.0269368
Ramos-Casals, Brito-Zerón, López-Guillermo, Khamashta, Bosch, Adult haemophagocytic syndrome, Lancet, doi:10.1016/S0140-6736(13)61048-X
Ranieri, Rubenfeld, Thompson, Ferguson, Caldwell et al., Acute Respiratory Distress Syndrome: The Berlin Definition, JAMA, doi:10.1001/jama.2012.5669
Rastogi, Bhansali, Khare, Suri, Yaddanapudi et al., Short term, high-dose vitamin D supplementation for COVID-19 disease: A randomised, placebo-controlled, study (SHADE study), Postgrad. Med. J, doi:10.1136/postgradmedj-2020-139065
Roca, Messika, Caralt, García-De-Acilu, Sztrymf et al., Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: The utility of the ROX index, J. Crit. Care
Roedl, Jarczak, Drolz, Wichmann, Boenisch et al., Severe liver dysfunction complicating course of COVID-19 in the critically ill: Multifactorial cause or direct viral effect?, Ann. Intensiv. Care, doi:10.1186/s13613-021-00835-3
Rosas, Diaz, Gottlieb, Lobo, Robinson et al., Tocilizumab and remdesivir in hospitalized patients with severe COVID-19 pneumonia: A randomized clinical trial, Intensiv. Care Med, doi:10.1007/s00134-021-06507-x
Ruan, Yang, Wang, Jiang, Song, Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China, Intensive Care Med, doi:10.1007/s00134-020-05991-x
Rutgers, Westerweel, Van Der Holt, Postma, Van Vonderen et al., Timely administration of tocilizumab improves outcome of hospitalized COVID-19 patients, PLoS ONE, doi:10.1371/journal.pone.0271807
Saleki, Shirzad, Javanian, Mohammadkhani, Alijani et al., Serum soluble Fas ligand is a severity and mortality prognostic marker for COVID-19 patients, Front. Immunol, doi:10.3389/fimmu.2022.947401
Salvarani, Dolci, Massari, Merlo, Cavuto et al., Effect of Tocilizumab vs Standard Care on Clinical Worsening in Patients Hospitalized with COVID-19 Pneumonia: A Randomized Clinical Trial, JAMA Intern. Med, doi:10.1001/jamainternmed.2020.6615
Schmidt, Jóźwiak, Czabajska, Pawlak-Buś, Leszczynski, On-admission laboratory predictors for developing critical COVID-19 during hospitalization-A multivariable logistic regression model, Ann. Agric. Environ. Med
Schmidt, Pawlak-Buś, Jóźwiak, Katulska, Leszczy Ński, Development and Validation of COVID-19 Radiological Risk Score (COVID-RRS): A Multivariable Radiological Score to Estimate the in-Hospital Mortality Risk in COVID-19 Patients, Eur. Rev. Med. Pharmacol. Sci, doi:10.26355/eurrev_202301_30892
Schulman, Kearon, The Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients, J. Thromb. Haemost, doi:10.1111/j.1538-7836.2005.01204.x
Selçuk, Keskin, Çınar, Günay, Do Gan et al., Prognostic significance of N-Terminal Pro-BNP in patients with COVID-19 pneumonia without previous history of heart failure, J. Cardiovasc. Thorac. Res, doi:10.34172/jcvtr.2021.26
Seymour, Liu, Kahn, Shankar-Hari, Singer et al., Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3), JAMA, doi:10.1001/jama.2016.0288
Shankar-Hari, Vale, Godolphin, Fisher, Higgins et al., Association Between Administration of IL-6 Antagonists and Mortality Among Patients Hospitalized for COVID-19: A Meta-analysis, JAMA, doi:10.1001/jama.2021.11330
Siddiqi, Mehra, COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal, J. Heart Lung Transplant, doi:10.1016/j.healun.2020.03.012
Singer, Deutschman, Seymour, Shankar-Hari, Annane et al., The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3), JAMA, doi:10.1001/jama.2016.0287
Stone, Frigault, Serling-Boyd, Fernandes, Harvey et al., Efficacy of Tocilizumab in Patients Hospitalized with COVID-19, N. Engl. J. Med
Subbe, Kruger, Rutherford, Gemmel, Validation of a modified Early Warning Score in medical admissions, QJM, doi:10.1093/qjmed/94.10.521
Taylor, Toh, Hoots, Wada, Levi, Scientific Subcommittee on Disseminated Intravascular Coagulation (DIC) of the International Society on Thrombosis and Haemostasis (ISTH) Towards Definition, Clinical and Laboratory Criteria, and a Scoring System for Disseminated Intravascular Coagulation, Thromb. Haemost
Thygesen, Alpert, Jaffe, Chaitman, Bax et al., Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction Fourth Universal Definition of Myocardial Infarction, J. Am. Coll. Cardiol, doi:10.1016/j.jacc.2018.08.1038
Toh, Hoots, SSC on Disseminated Intravascular Coagulation of the ISTH. The scoring system of the Scientific and Standardisation Committee on Disseminated Intravascular Coagulation of the International Society on Thrombosis and Haemostasis: A 5-year overview, J. Thromb. Haemost, doi:10.1111/j.1538-7836.2007.02313.x
Uhlig, Menon, Schmid, Recommendations for Reporting of Clinical Research Studies, Am. J. Kidney Dis
Van Kraaij, Mostard, Ramiro, Checa, Van Dongen et al., Tocilizumab in Severe COVID-19 Pneumonia and Concomitant Cytokine Release Syndrome, Eur. J. Case Rep. Intern. Med
Varga, Flammer, Steiger, Haberecker, Andermatt et al., Endothelial cell infection and endotheliitis in COVID-19, Lancet, doi:10.1016/S0140-6736(20)30937-5
Vela, Vela-Gaxha, Rexhepi, Olloni, Hyseni et al., Efficacy and safety of tocilizumab versus standard care/placebo in patients with COVID-19; A systematic review and meta-analysis of randomized clinical trials, Br. J. Clin. Pharmacol, doi:10.1111/bcp.15124
Viswanatha, Male, Shylaja, Efficacy and safety of tocilizumab in the management of COVID-19: A systematic review and meta-analysis of observational studies, Ann. Rheum. Dis, doi:10.55563/clinexprheumatol/4dg0or
Webb, Peltan, Jensen, Hoda, Hunter et al., Clinical criteria for COVID-19-associated hyperinflammatory syndrome: A cohort study, Lancet Rheumatol, doi:10.1016/S2665-9913(20)30343-X
Wettstein, Shelledy, Peters, Delivered oxygen concentrations using low-flow and high-flow nasal cannulas, Respir. Care
Wild, Porter, Molyneaux, George, Stewart et al., Understanding the burden of interstitial lung disease post-COVID-19: The UK Interstitial Lung Disease-Long COVID Study (UKILD-Long COVID), BMJ Open Respir. Res, doi:10.1136/bmjresp-2021-001049
Williamson, Walker, Bhaskaran, Bacon, Bates et al., Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Wolfe, Tomashek, Patterson, Gomez, Marconi et al., Baricitinib versus dexamethasone for adults hospitalised with COVID-19 (ACTT-4): A randomised, doubleblind, double placebo-controlled trial, Lancet Respir. Med, doi:10.1016/S2213-2600(22)00088-1
Wu, Mcgoogan, Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases from the Chinese Center for Disease Control and Prevention, JAMA, doi:10.1001/jama.2020.2648
Xu, Han, Li, Sun, Wang et al., Effective Treatment of Severe COVID-19 Patients with Tocilizumab, doi:10.1073/pnas.2005615117
Yokota, Tanaka, Kishimoto, Efficacy, safety and tolerability of tocilizumab in patients with systemic juvenile idiopathic arthritis, Ther. Adv. Musculoskelet. Dis, doi:10.1177/1759720X12455960
Zarębska-Michaluk, Jaroszewicz, Rogalska, Martonik, Pabjan et al., Effectiveness of Tocilizumab with and without Dexamethasone in Patients with Severe COVID-19: A Retrospective Study, J. Inflamm. Res, doi:10.2147/JIR.S322645
Zeng, Xie, Yang, Chao, Xu, Clinical efficacy of tocilizumab treatment in severe and critical COVID-19 patients, World J. Clin. Cases, doi:10.12998/wjcc.v8.i17.3763
Zhang, Chen, Yang, Yang, Effectiveness of tocilizumab in the treatment of hospitalized adults COVID-19: A Systematic Review and Meta-Analysis, Medicine, doi:10.1097/MD.0000000000028967
Zinellu, Sotgia, Carru, Mangoni, B-Type Natriuretic Peptide Concentrations, COVID-19 Severity, and Mortality: A Systematic Review and Meta-Analysis with Meta-Regression, Front. Cardiovasc. Med, doi:10.3389/fcvm.2021.690790
Çelik, Öztürk, From asymptomatic to critical illness: Decoding various clinical stages of Covid-19, Turk. J. Med. Sci, doi:10.3906/sag-2107-13
DOI record:
{
"DOI": "10.3390/jcm12062429",
"ISSN": [
"2077-0383"
],
"URL": "http://dx.doi.org/10.3390/jcm12062429",
"abstract": "<jats:p>Hyperinflammation in COVID-19 plays a crucial role in pathogenesis and severity; thus, many immunomodulatory agents are applied in its treatment. We aimed to identify good clinical response predictors of tocilizumab (TCZ) treatment in severe COVID-19, among clinical, laboratory, and radiological variables. We conducted a prospective, observational study with 120 patients with severe COVID-19 not improving despite dexamethasone (DEX) treatment. We used parametric and non-parametric statistics, univariate logistic regression, receiver operating characteristic (ROC) curves, and nonlinear factors tertile analysis. In total, 86 (71.7%) patients achieved the primary outcome of a good clinical response to TCZ. We identified forty-nine predictive factors with potential utility in patient selection and treatment monitoring. The strongest included time from symptom onset between 9 and 12 days, less than 70% of estimated radiological lung involvement, and lower activity of lactate dehydrogenase. Additional predictors were associated with respiratory function, vitamin D concentration, comorbidities, and inflammatory/organ damage biomarkers. Adverse events analysis proved the safety of such a regimen. Our study confirmed that using TCZ early in the hyperinflammatory phase, before severe respiratory failure development, is most beneficial. Considering the described predictive factors, employing simple and widely available laboratory, radiological, and clinical tools can optimize patient selection for immunomodulatory treatment with TCZ.</jats:p>",
"alternative-id": [
"jcm12062429"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-9409-9827",
"affiliation": [
{
"name": "Department of Rheumatology, Systemic Connective Tissue Diseases and Immunotherapy of Rheumatic Diseases, J. Strus Municipal Hospital, 61-285 Poznan, Poland"
},
{
"name": "Department of Internal Medicine, Poznan University of Medical Sciences, 61-701 Poznan, Poland"
},
{
"name": "Doctoral School, Poznan University of Medical Sciences, 60-812 Poznan, Poland"
}
],
"authenticated-orcid": false,
"family": "Schmidt",
"given": "Wiktor",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-1982-5980",
"affiliation": [
{
"name": "Department of Rheumatology, Systemic Connective Tissue Diseases and Immunotherapy of Rheumatic Diseases, J. Strus Municipal Hospital, 61-285 Poznan, Poland"
},
{
"name": "Department of Internal Medicine, Poznan University of Medical Sciences, 61-701 Poznan, Poland"
}
],
"authenticated-orcid": false,
"family": "Pawlak-Buś",
"given": "Katarzyna",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7668-4221",
"affiliation": [
{
"name": "Department of Rheumatology, Systemic Connective Tissue Diseases and Immunotherapy of Rheumatic Diseases, J. Strus Municipal Hospital, 61-285 Poznan, Poland"
}
],
"authenticated-orcid": false,
"family": "Jóźwiak",
"given": "Barbara",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Rheumatology, Systemic Connective Tissue Diseases and Immunotherapy of Rheumatic Diseases, J. Strus Municipal Hospital, 61-285 Poznan, Poland"
},
{
"name": "Department of Internal Medicine, Poznan University of Medical Sciences, 61-701 Poznan, Poland"
}
],
"family": "Leszczyński",
"given": "Piotr",
"sequence": "additional"
}
],
"container-title": "Journal of Clinical Medicine",
"container-title-short": "JCM",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
3,
22
]
],
"date-time": "2023-03-22T10:00:01Z",
"timestamp": 1679479201000
},
"deposited": {
"date-parts": [
[
2023,
3,
22
]
],
"date-time": "2023-03-22T11:59:58Z",
"timestamp": 1679486398000
},
"indexed": {
"date-parts": [
[
2023,
3,
23
]
],
"date-time": "2023-03-23T04:56:29Z",
"timestamp": 1679547389554
},
"is-referenced-by-count": 0,
"issue": "6",
"issued": {
"date-parts": [
[
2023,
3,
22
]
]
},
"journal-issue": {
"issue": "6",
"published-online": {
"date-parts": [
[
2023,
3
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
3,
22
]
],
"date-time": "2023-03-22T00:00:00Z",
"timestamp": 1679443200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2077-0383/12/6/2429/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "2429",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
3,
22
]
]
},
"published-online": {
"date-parts": [
[
2023,
3,
22
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1172/JCI154886",
"article-title": "The intersection of COVID-19 and autoimmunity",
"author": "Knight",
"doi-asserted-by": "crossref",
"first-page": "e154886",
"journal-title": "J. Clin. Investig.",
"key": "ref_1",
"volume": "131",
"year": "2021"
},
{
"DOI": "10.1056/NEJMra2026131",
"article-title": "Cytokine Storm",
"author": "Fajgenbaum",
"doi-asserted-by": "crossref",
"first-page": "2255",
"journal-title": "N. Engl. J. Med.",
"key": "ref_2",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1002/art.41285",
"article-title": "On the Alert for Cytokine Storm: Immunopathology in COVID-19",
"author": "Henderson",
"doi-asserted-by": "crossref",
"first-page": "1059",
"journal-title": "Arthritis Rheumatol.",
"key": "ref_3",
"volume": "72",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(13)61048-X",
"article-title": "Adult haemophagocytic syndrome",
"author": "Khamashta",
"doi-asserted-by": "crossref",
"first-page": "1503",
"journal-title": "Lancet",
"key": "ref_4",
"volume": "383",
"year": "2014"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "Lancet",
"key": "ref_5",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1007/s00134-020-05991-x",
"article-title": "Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China",
"author": "Ruan",
"doi-asserted-by": "crossref",
"first-page": "846",
"journal-title": "Intensive Care Med.",
"key": "ref_6",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.26444/aaem/145376",
"article-title": "On-admission laboratory predictors for developing critical COVID-19 during hospitalization—A multivariable logistic regression model",
"author": "Schmidt",
"doi-asserted-by": "crossref",
"first-page": "274",
"journal-title": "Ann. Agric. Environ. Med.",
"key": "ref_7",
"volume": "29",
"year": "2022"
},
{
"DOI": "10.1038/s41379-020-00661-1",
"article-title": "COVID-19 pulmonary pathology: A multi-institutional autopsy cohort from Italy and New York City",
"author": "Borczuk",
"doi-asserted-by": "crossref",
"first-page": "2156",
"journal-title": "Mod. Pathol.",
"key": "ref_8",
"volume": "33",
"year": "2020"
},
{
"DOI": "10.1038/s41467-020-18854-2",
"article-title": "Two distinct immunopathological profiles in autopsy lungs of COVID-19",
"author": "Nienhold",
"doi-asserted-by": "crossref",
"first-page": "5086",
"journal-title": "Nat. Commun.",
"key": "ref_9",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30937-5",
"article-title": "Endothelial cell infection and endotheliitis in COVID-19",
"author": "Varga",
"doi-asserted-by": "crossref",
"first-page": "1417",
"journal-title": "Lancet",
"key": "ref_10",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/j.humpath.2021.04.012",
"article-title": "Tissue-based SARS-CoV-2 detection in fatal COVID-19 infections: Sustained direct viral-induced damage is not necessary to drive disease progression",
"author": "Pujadas",
"doi-asserted-by": "crossref",
"first-page": "110",
"journal-title": "Hum. Pathol.",
"key": "ref_11",
"volume": "114",
"year": "2021"
},
{
"DOI": "10.1038/s41379-021-00793-y",
"article-title": "Pathophysiology of SARS-CoV-2: The Mount Sinai COVID-19 autopsy experience",
"author": "Bryce",
"doi-asserted-by": "crossref",
"first-page": "1456",
"journal-title": "Mod. Pathol.",
"key": "ref_12",
"volume": "34",
"year": "2021"
},
{
"DOI": "10.1097/BOR.0000000000000822",
"article-title": "Is severe COVID-19 a cytokine storm syndrome: A hyperinflammatory debate",
"author": "Mehta",
"doi-asserted-by": "crossref",
"first-page": "419",
"journal-title": "Curr. Opin. Rheumatol.",
"key": "ref_13",
"volume": "33",
"year": "2021"
},
{
"DOI": "10.1016/S2213-2600(20)30404-5",
"article-title": "Cytokine elevation in severe and critical COVID-19: A rapid systematic review, meta-analysis, and comparison with other inflammatory syndromes",
"author": "Leisman",
"doi-asserted-by": "crossref",
"first-page": "1233",
"journal-title": "Lancet Respir. Med.",
"key": "ref_14",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1007/s11239-020-02129-0",
"article-title": "Pulmonary intravascular coagulation in COVID-19: Possible pathogenesis and recommendations on anticoagulant/thrombolytic therapy",
"doi-asserted-by": "crossref",
"first-page": "278",
"journal-title": "J. Thromb. Thrombolysis",
"key": "ref_15",
"volume": "50",
"year": "2020"
},
{
"DOI": "10.1016/S2665-9913(20)30343-X",
"article-title": "Clinical criteria for COVID-19-associated hyperinflammatory syndrome: A cohort study",
"author": "Webb",
"doi-asserted-by": "crossref",
"first-page": "e754",
"journal-title": "Lancet Rheumatol.",
"key": "ref_16",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.1016/S2665-9913(21)00322-2",
"article-title": "Therapeutic implications of ongoing alveolar viral replication in COVID-19",
"author": "McGonagle",
"doi-asserted-by": "crossref",
"first-page": "e135",
"journal-title": "Lancet Rheumatol.",
"key": "ref_17",
"volume": "4",
"year": "2022"
},
{
"DOI": "10.1016/j.heliyon.2021.e06158",
"article-title": "Recent updates in the clinical trials of therapeutic monoclonal antibodies targeting cytokine storm for the management of COVID-19",
"author": "Patel",
"doi-asserted-by": "crossref",
"first-page": "e06158",
"journal-title": "Heliyon",
"key": "ref_18",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1073/pnas.2005615117",
"article-title": "Effective Treatment of Severe COVID-19 Patients with Tocilizumab",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "10970",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "ref_19",
"volume": "117",
"year": "2020"
},
{
"article-title": "Tocilizumab in Severe COVID-19 Pneumonia and Concomitant Cytokine Release Syndrome",
"author": "Mostard",
"first-page": "001675",
"journal-title": "Eur. J. Case Rep. Intern. Med.",
"key": "ref_20",
"volume": "7",
"year": "2020"
},
{
"article-title": "Early tocilizumab treatment could improve survival among COVID-19 patients",
"author": "Campins",
"first-page": "578",
"journal-title": "Clin. Exp. Rheumatol.",
"key": "ref_21",
"volume": "38",
"year": "2020"
},
{
"article-title": "Efficacy and safety of tocilizumab in the management of COVID-19: A systematic review and meta-analysis of observational studies",
"author": "Viswanatha",
"first-page": "634",
"journal-title": "Ann. Rheum. Dis.",
"key": "ref_22",
"volume": "40",
"year": "2022"
},
{
"DOI": "10.1111/bcp.15124",
"article-title": "Efficacy and safety of tocilizumab versus standard care/placebo in patients with COVID-19; A systematic review and meta-analysis of randomized clinical trials",
"author": "Vela",
"doi-asserted-by": "crossref",
"first-page": "1955",
"journal-title": "Br. J. Clin. Pharmacol.",
"key": "ref_23",
"volume": "88",
"year": "2022"
},
{
"DOI": "10.1097/MD.0000000000028967",
"article-title": "Effectiveness of tocilizumab in the treatment of hospitalized adults COVID-19: A Systematic Review and Meta-Analysis",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "e28967",
"journal-title": "Medicine",
"key": "ref_24",
"volume": "101",
"year": "2022"
},
{
"key": "ref_25",
"unstructured": "The WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, Shankar-Hari, M., Vale, C.L., Godolphin, P.J., Fisher, D., Higgins, J.P.T., Spiga, F., Savović, J., Tierney, J., and Baron, G. (2021). Association Between Administration of IL-6 Antagonists and Mortality Among Patients Hospitalized for COVID-19: A Meta-analysis. JAMA, 326, 499–518."
},
{
"DOI": "10.5662/wjm.v11.i3.95",
"article-title": "Tocilizumab as treatment for COVID-19: A systematic review and meta-analysis",
"author": "Petrelli",
"doi-asserted-by": "crossref",
"first-page": "95",
"journal-title": "World J. Methodol.",
"key": "ref_26",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/j.cmi.2022.02.027",
"article-title": "Early administration of tocilizumab in hospitalized COVID-19 patients with elevated inflammatory markers; COVIDSTORM—A prospective, randomized, single-centre, open-label study",
"author": "Broman",
"doi-asserted-by": "crossref",
"first-page": "844",
"journal-title": "Clin. Microbiol. Infect.",
"key": "ref_27",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1371/journal.pone.0271807",
"doi-asserted-by": "crossref",
"key": "ref_28",
"unstructured": "Rutgers, A., Westerweel, P.E., van der Holt, B., Postma, S., van Vonderen, M.G.A., Piersma, D.P., Postma, D., van den Berge, M., Jong, E., and de Vries, M. (2022). Timely administration of tocilizumab improves outcome of hospitalized COVID-19 patients. PLoS ONE, 17."
},
{
"DOI": "10.1001/jamainternmed.2020.6820",
"article-title": "Effect of Tocilizumab vs Usual Care in Adults Hospitalized With COVID-19 and Moderate or Severe Pneumonia: A Randomized Clinical Trial",
"author": "Hermine",
"doi-asserted-by": "crossref",
"first-page": "32",
"journal-title": "JAMA Intern. Med.",
"key": "ref_29",
"volume": "181",
"year": "2021"
},
{
"DOI": "10.1001/jamainternmed.2020.6615",
"article-title": "Effect of Tocilizumab vs Standard Care on Clinical Worsening in Patients Hospitalized with COVID-19 Pneumonia: A Randomized Clinical Trial",
"author": "Salvarani",
"doi-asserted-by": "crossref",
"first-page": "24",
"journal-title": "JAMA Intern. Med.",
"key": "ref_30",
"volume": "181",
"year": "2021"
},
{
"DOI": "10.1007/s00134-021-06507-x",
"article-title": "Tocilizumab and remdesivir in hospitalized patients with severe COVID-19 pneumonia: A randomized clinical trial",
"author": "Rosas",
"doi-asserted-by": "crossref",
"first-page": "1258",
"journal-title": "Intensiv. Care Med.",
"key": "ref_31",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2028836",
"article-title": "Efficacy of Tocilizumab in Patients Hospitalized with COVID-19",
"author": "Stone",
"doi-asserted-by": "crossref",
"first-page": "2333",
"journal-title": "N. Engl. J. Med.",
"key": "ref_32",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1634/theoncologist.2018-0028",
"article-title": "FDA Approval Summary: Tocilizumab for Treatment of Chimeric Antigen Receptor T Cell-Induced Severe or Life-Threatening Cytokine Release Syndrome",
"author": "Le",
"doi-asserted-by": "crossref",
"first-page": "943",
"journal-title": "Oncologist",
"key": "ref_33",
"volume": "23",
"year": "2018"
},
{
"DOI": "10.1136/annrheumdis-2018-213920",
"article-title": "Tocilizumab in patients with adult-onset still’s disease refractory to glucocorticoid treatment: A randomised, double-blind, placebo-controlled phase III trial",
"author": "Kaneko",
"doi-asserted-by": "crossref",
"first-page": "1720",
"journal-title": "Ann. Rheum. Dis.",
"key": "ref_34",
"volume": "77",
"year": "2018"
},
{
"DOI": "10.1177/1759720X12455960",
"article-title": "Efficacy, safety and tolerability of tocilizumab in patients with systemic juvenile idiopathic arthritis",
"author": "Yokota",
"doi-asserted-by": "crossref",
"first-page": "387",
"journal-title": "Ther. Adv. Musculoskelet. Dis.",
"key": "ref_35",
"volume": "4",
"year": "2012"
},
{
"article-title": "Recommendations of management in SARS-CoV-2 infection of the Polish Association of Epidemiologists and Infectiologists",
"author": "Flisiak",
"first-page": "352",
"journal-title": "Pol. Arch. Intern. Med.",
"key": "ref_36",
"volume": "130",
"year": "2020"
},
{
"article-title": "Management of SARS-CoV-2 infection: Recommendations of the Polish Association of Epidemiologists and Infectiologists as of 23 February 2022",
"author": "Flisiak",
"first-page": "16230",
"journal-title": "Pol. Arch. Intern. Med.",
"key": "ref_37",
"volume": "132",
"year": "2022"
},
{
"DOI": "10.5114/reum.2020.96685",
"article-title": "COVID-19: A short message to rheumatologists",
"doi-asserted-by": "crossref",
"first-page": "130",
"journal-title": "Rheumatology",
"key": "ref_38",
"volume": "58",
"year": "2020"
},
{
"DOI": "10.1056/NEJMcp2009575",
"article-title": "Severe COVID-19",
"author": "Berlin",
"doi-asserted-by": "crossref",
"first-page": "2451",
"journal-title": "N. Engl. J. Med.",
"key": "ref_39",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.2648",
"article-title": "Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases from the Chinese Center for Disease Control and Prevention",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "1239",
"journal-title": "JAMA",
"key": "ref_40",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.33963/KP.15425",
"article-title": "Guidance for anticoagulation management in venous thromboembolism during the coronavirus disease 2019 pandemic in Poland: An expert opinion of the Section on Pulmonary Circulation of the Polish Cardiac Society",
"author": "Kosior",
"doi-asserted-by": "crossref",
"first-page": "642",
"journal-title": "Kardiologia Polska",
"key": "ref_41",
"volume": "78",
"year": "2020"
},
{
"DOI": "10.7326/0003-4819-147-8-200710160-00010",
"article-title": "The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies",
"author": "Altman",
"doi-asserted-by": "crossref",
"first-page": "573",
"journal-title": "Ann. Intern. Med.",
"key": "ref_42",
"volume": "147",
"year": "2007"
},
{
"DOI": "10.1053/j.ajkd.2006.10.012",
"article-title": "Recommendations for Reporting of Clinical Research Studies",
"author": "Uhlig",
"doi-asserted-by": "crossref",
"first-page": "3",
"journal-title": "Am. J. Kidney Dis.",
"key": "ref_43",
"volume": "49",
"year": "2007"
},
{
"DOI": "10.1016/0021-9681(87)90171-8",
"article-title": "A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation",
"author": "Charlson",
"doi-asserted-by": "crossref",
"first-page": "373",
"journal-title": "J. Chronic Dis.",
"key": "ref_44",
"volume": "40",
"year": "1987"
},
{
"article-title": "Delivered oxygen concentrations using low-flow and high-flow nasal cannulas",
"author": "Wettstein",
"first-page": "604",
"journal-title": "Respir. Care",
"key": "ref_45",
"volume": "50",
"year": "2005"
},
{
"DOI": "10.1111/j.1365-2044.2004.03526.x",
"article-title": "Simple bedside assessment of level of consciousness: Comparison of two simple assessment scales with the Glasgow Coma scale",
"author": "McNarry",
"doi-asserted-by": "crossref",
"first-page": "34",
"journal-title": "Anaesthesia",
"key": "ref_46",
"volume": "59",
"year": "2004"
},
{
"DOI": "10.1093/qjmed/94.10.521",
"article-title": "Validation of a modified Early Warning Score in medical admissions",
"author": "Subbe",
"doi-asserted-by": "crossref",
"first-page": "521",
"journal-title": "QJM",
"key": "ref_47",
"volume": "94",
"year": "2001"
},
{
"DOI": "10.1001/jama.2016.0288",
"article-title": "Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)",
"author": "Seymour",
"doi-asserted-by": "crossref",
"first-page": "762",
"journal-title": "JAMA",
"key": "ref_48",
"volume": "315",
"year": "2016"
},
{
"DOI": "10.1001/jama.2016.20329",
"article-title": "Prognostic Accuracy of Sepsis-3 Criteria for In-Hospital Mortality Among Patients with Suspected Infection Presenting to the Emergency Department",
"author": "Freund",
"doi-asserted-by": "crossref",
"first-page": "301",
"journal-title": "JAMA",
"key": "ref_49",
"volume": "317",
"year": "2017"
},
{
"DOI": "10.1016/S1473-3099(20)30483-7",
"article-title": "WHO Working Group on the Clinical Characterisation and Management of COVID-19 infection A Minimal Common Outcome Measure Set for COVID-19 Clinical Research",
"author": "Marshall",
"doi-asserted-by": "crossref",
"first-page": "e192",
"journal-title": "Lancet Infect. Dis.",
"key": "ref_50",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1016/j.jcrc.2016.05.022",
"article-title": "Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: The utility of the ROX index",
"author": "Roca",
"doi-asserted-by": "crossref",
"first-page": "200",
"journal-title": "J. Crit. Care",
"key": "ref_51",
"volume": "35",
"year": "2016"
},
{
"DOI": "10.1186/s40560-020-00458-z",
"article-title": "Early prediction of high flow nasal cannula therapy outcomes using a modified ROX index incorporating heart rate",
"author": "Goh",
"doi-asserted-by": "crossref",
"first-page": "41",
"journal-title": "J. Intensiv. Care",
"key": "ref_52",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.ajem.2021.01.092",
"article-title": "Assessment of the SpO2/FiO2 ratio as a tool for hypoxemia screening in the emergency department",
"author": "Catoire",
"doi-asserted-by": "crossref",
"first-page": "116",
"journal-title": "Am. J. Emerg. Med.",
"key": "ref_53",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.1148/radiol.2462070712",
"article-title": "Fleischner Society: Glossary of Terms for Thoracic Imaging",
"author": "Hansell",
"doi-asserted-by": "crossref",
"first-page": "697",
"journal-title": "Radiology",
"key": "ref_54",
"volume": "246",
"year": "2008"
},
{
"article-title": "Development and Validation of COVID-19 Radiological Risk Score (COVID-RRS): A Multivariable Radiological Score to Estimate the in-Hospital Mortality Risk in COVID-19 Patients",
"author": "Schmidt",
"first-page": "384",
"journal-title": "Eur. Rev. Med. Pharmacol. Sci.",
"key": "ref_55",
"volume": "27",
"year": "2023"
},
{
"key": "ref_56",
"unstructured": "ARDS Definition of Task Force, Ranieri, V.M., Rubenfeld, G.D., Thompson, B.T., Ferguson, N.D., Caldwell, E., Fan, E., Camporota, L., and Slutsky, A.S. (2012). Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA, 307, 2526–2533."
},
{
"DOI": "10.1093/eurheartj/ehz405",
"article-title": "2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS)",
"author": "Konstantinides",
"doi-asserted-by": "crossref",
"first-page": "543",
"journal-title": "Eur. Heart J.",
"key": "ref_57",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1093/eurheartj/ehx003",
"article-title": "Diagnosis and management of acute deep vein thrombosis: A joint consensus document from the European Society of Cardiology working groups of aorta and peripheral vascular diseases and pulmonary circulation and right ventricular function",
"author": "Mazzolai",
"doi-asserted-by": "crossref",
"first-page": "4208",
"journal-title": "Eur. Heart J.",
"key": "ref_58",
"volume": "39",
"year": "2017"
},
{
"DOI": "10.3390/jcm10020191",
"doi-asserted-by": "crossref",
"key": "ref_59",
"unstructured": "Iba, T.E., Warkentin, T., Thachil, J., Levi, M., and Levy, J.H. (2021). Proposal of the Definition for COVID-19-Associated Coagulopathy. J. Clin. Med., 10."
},
{
"DOI": "10.1055/s-0037-1616068",
"article-title": "Scientific Subcommittee on Disseminated Intravascular Coagulation (DIC) of the International Society on Thrombosis and Haemostasis (ISTH) Towards Definition, Clinical and Laboratory Criteria, and a Scoring System for Disseminated Intravascular Coagulation",
"author": "Taylor",
"doi-asserted-by": "crossref",
"first-page": "1327",
"journal-title": "Thromb. Haemost.",
"key": "ref_60",
"volume": "86",
"year": "2001"
},
{
"DOI": "10.1111/j.1538-7836.2007.02313.x",
"article-title": "The scoring system of the Scientific and Standardisation Committee on Disseminated Intravascular Coagulation of the International Society on Thrombosis and Haemostasis: A 5-year overview",
"author": "Toh",
"doi-asserted-by": "crossref",
"first-page": "604",
"journal-title": "J. Thromb. Haemost.",
"key": "ref_61",
"volume": "5",
"year": "2007"
},
{
"DOI": "10.1111/j.1538-7836.2005.01204.x",
"article-title": "Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients",
"author": "Schulman",
"doi-asserted-by": "crossref",
"first-page": "692",
"journal-title": "J. Thromb. Haemost.",
"key": "ref_62",
"volume": "3",
"year": "2005"
},
{
"DOI": "10.1007/s11239-020-02364-5",
"article-title": "Association of ABO blood group type with cardiovascular events in COVID-19",
"author": "Nauffal",
"doi-asserted-by": "crossref",
"first-page": "584",
"journal-title": "J. Thromb. Thrombolysis",
"key": "ref_63",
"volume": "51",
"year": "2021"
},
{
"DOI": "10.1016/j.jacc.2018.08.1038",
"article-title": "Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction Fourth Universal Definition of Myocardial Infarction",
"author": "Thygesen",
"doi-asserted-by": "crossref",
"first-page": "2231",
"journal-title": "J. Am. Coll. Cardiol.",
"key": "ref_64",
"volume": "72",
"year": "2018"
},
{
"DOI": "10.1038/ajg.2016.517",
"article-title": "ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries",
"author": "Kwo",
"doi-asserted-by": "crossref",
"first-page": "18",
"journal-title": "Off. J. Am. Coll. Gastroenterol.",
"key": "ref_65",
"volume": "112",
"year": "2017"
},
{
"DOI": "10.1038/clpt.2011.58",
"article-title": "Case Definition and Phenotype Standardization in Drug-Induced Liver Injury",
"author": "Aithal",
"doi-asserted-by": "crossref",
"first-page": "806",
"journal-title": "Clin. Pharmacol. Ther.",
"key": "ref_66",
"volume": "89",
"year": "2011"
},
{
"DOI": "10.1186/s13613-021-00835-3",
"article-title": "Severe liver dysfunction complicating course of COVID-19 in the critically ill: Multifactorial cause or direct viral effect?",
"author": "Roedl",
"doi-asserted-by": "crossref",
"first-page": "44",
"journal-title": "Ann. Intensiv. Care",
"key": "ref_67",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1001/jama.2016.0287",
"article-title": "The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)",
"author": "Singer",
"doi-asserted-by": "crossref",
"first-page": "801",
"journal-title": "JAMA",
"key": "ref_68",
"volume": "315",
"year": "2016"
},
{
"DOI": "10.1159/000339789",
"article-title": "KDIGO Clinical Practice Guidelines for Acute Kidney Injury",
"author": "Khwaja",
"doi-asserted-by": "crossref",
"first-page": "c179",
"journal-title": "Nephron Clin. Pr.",
"key": "ref_69",
"volume": "120",
"year": "2012"
},
{
"DOI": "10.1176/appi.neuropsych.22010002",
"article-title": "Consensus Clinical Guidance for Diagnosis and Management of Adult COVID-19 Encephalopathy Patients",
"author": "Michael",
"doi-asserted-by": "crossref",
"first-page": "12",
"journal-title": "J. Neuropsychiatry",
"key": "ref_70",
"volume": "35",
"year": "2022"
},
{
"DOI": "10.1016/S2665-9913(20)30275-7",
"article-title": "COVID-19-associated hyperinflammation and escalation of patient care: A retrospective longitudinal cohort study",
"author": "Manson",
"doi-asserted-by": "crossref",
"first-page": "e594",
"journal-title": "Lancet Rheumatol.",
"key": "ref_71",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.1136/annrheumdis-2020-218323",
"article-title": "Preliminary predictive criteria for COVID-19 cytokine storm",
"author": "Caricchio",
"doi-asserted-by": "crossref",
"first-page": "88",
"journal-title": "Ann. Rheum. Dis.",
"key": "ref_72",
"volume": "80",
"year": "2020"
},
{
"DOI": "10.12998/wjcc.v8.i17.3763",
"article-title": "Clinical efficacy of tocilizumab treatment in severe and critical COVID-19 patients",
"author": "Zeng",
"doi-asserted-by": "crossref",
"first-page": "3763",
"journal-title": "World J. Clin. Cases",
"key": "ref_73",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.3906/sag-2107-13",
"article-title": "From asymptomatic to critical illness: Decoding various clinical stages of Covid-19",
"doi-asserted-by": "crossref",
"first-page": "3284",
"journal-title": "Turk. J. Med. Sci.",
"key": "ref_74",
"volume": "51",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2020.12.021",
"article-title": "Tocilizumab in the treatment of critical COVID-19 pneumonia: A retrospective cohort study of mechanically ventilated patients",
"author": "Fisher",
"doi-asserted-by": "crossref",
"first-page": "536",
"journal-title": "Int. J. Infect. Dis.",
"key": "ref_75",
"volume": "103",
"year": "2020"
},
{
"DOI": "10.1016/j.jhin.2022.04.007",
"article-title": "Association between tocilizumab treatment of hyperinflammatory patients with COVID-19 in a critical care setting and elevated incidence of hospital-acquired bacterial and invasive fungal infections",
"author": "Minihan",
"doi-asserted-by": "crossref",
"first-page": "29",
"journal-title": "J. Hosp. Infect.",
"key": "ref_76",
"volume": "126",
"year": "2022"
},
{
"DOI": "10.1016/S2665-9913(21)00003-5",
"article-title": "Thromboses and COVID-19: Reducing inflammation in addition to thromboprophylaxis",
"author": "Mehta",
"doi-asserted-by": "crossref",
"first-page": "e171",
"journal-title": "Lancet Rheumatol.",
"key": "ref_77",
"volume": "3",
"year": "2021"
},
{
"DOI": "10.1016/j.healun.2020.03.012",
"article-title": "COVID-19 illness in native and immunosuppressed states: A clinical–therapeutic staging proposal",
"author": "Siddiqi",
"doi-asserted-by": "crossref",
"first-page": "405",
"journal-title": "J. Heart Lung Transplant.",
"key": "ref_78",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0246190",
"doi-asserted-by": "crossref",
"key": "ref_79",
"unstructured": "Fathi, M., Vakili, K., Sayehmiri, F., Mohamadkhani, A., Hajiesmaeili, M., Rezaei-Tavirani, M., and Eilami, O. (2021). The prognostic value of comorbidity for the severity of COVID-19: A systematic review and meta-analysis study. PLoS ONE, 16."
},
{
"article-title": "Prognostic factors and combined use of tocilizumab and corticosteroids in a Spanish cohort of elderly COVID-19 patients",
"author": "Sedano",
"first-page": "1540",
"journal-title": "J. Med. Virol.",
"key": "ref_80",
"volume": "94",
"year": "2021"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"article-title": "Factors associated with COVID-19-related death using OpenSAFELY",
"author": "Williamson",
"doi-asserted-by": "crossref",
"first-page": "430",
"journal-title": "Nature",
"key": "ref_81",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.5603/CJ.a2022.0056",
"article-title": "Diagnostic value of lactate dehydrogenase in COVID-19: A systematic review and meta-analysis",
"author": "Fialek",
"doi-asserted-by": "crossref",
"first-page": "751",
"journal-title": "Cardiol. J.",
"key": "ref_82",
"volume": "29",
"year": "2022"
},
{
"DOI": "10.2217/bmm-2022-0364",
"article-title": "Changes in lactate dehydrogenase on admission throughout the COVID-19 pandemic and possible impacts on prognostic capability",
"doi-asserted-by": "crossref",
"first-page": "1019",
"journal-title": "Biomarkers Med.",
"key": "ref_83",
"volume": "16",
"year": "2022"
},
{
"DOI": "10.1016/j.ajem.2020.05.073",
"article-title": "Lactate dehydrogenase levels predict coronavirus disease 2019 (COVID-19) severity and mortality: A pooled analysis",
"author": "Henry",
"doi-asserted-by": "crossref",
"first-page": "1722",
"journal-title": "Am. J. Emerg. Med.",
"key": "ref_84",
"volume": "38",
"year": "2020"
},
{
"DOI": "10.3390/jcm11010107",
"doi-asserted-by": "crossref",
"key": "ref_85",
"unstructured": "Olewicz-Gawlik, A., Ginter-Matuszewska, B., Kamiński, M., Adamek, A., Bura, M., Mozer-Lisewska, I., and Kowala-Piaskowska, A. (2022). Changes in Inflammatory Markers after Administration of Tocilizumab in COVID-19: A Single-Center Retrospective Study. J. Clin. Med., 11."
},
{
"DOI": "10.34172/jcvtr.2021.26",
"article-title": "Prognostic significance of N-Terminal Pro-BNP in patients with COVID-19 pneumonia without previous history of heart failure",
"author": "Keskin",
"doi-asserted-by": "crossref",
"first-page": "141",
"journal-title": "J. Cardiovasc. Thorac. Res.",
"key": "ref_86",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3389/fcvm.2021.690790",
"article-title": "B-Type Natriuretic Peptide Concentrations, COVID-19 Severity, and Mortality: A Systematic Review and Meta-Analysis with Meta-Regression",
"author": "Zinellu",
"doi-asserted-by": "crossref",
"first-page": "690790",
"journal-title": "Front. Cardiovasc. Med.",
"key": "ref_87",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.3390/jcm9124078",
"doi-asserted-by": "crossref",
"key": "ref_88",
"unstructured": "Cordeanu, E.-M., Duthil, N., Severac, F., Lambach, H., Tousch, J., Jambert, L., Mirea, C., Delatte, A., Younes, W., and Frantz, A.-S. (2020). Prognostic Value of Troponin Elevation in COVID-19 Hospitalized Patients. J. Clin. Med., 9."
},
{
"DOI": "10.1371/journal.pone.0272840",
"doi-asserted-by": "crossref",
"key": "ref_89",
"unstructured": "Kumar, A., Karn, E., Trivedi, K., Kumar, P., Chauhan, G., Kumari, A., Pant, P., Munisamy, M., Prakash, J., and Sarkar, P.G. (2022). Procalcitonin as a predictive marker in COVID-19: A systematic review and meta-analysis. PLoS ONE, 17."
},
{
"DOI": "10.1016/j.medj.2020.09.001",
"article-title": "Kidney Function Indicators Predict Adverse Outcomes of COVID-19",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "38",
"journal-title": "Med",
"key": "ref_90",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1016/j.ajem.2020.09.018",
"article-title": "Elevated D-dimer levels on admission are associated with severity and increased risk of mortality in COVID-19: A systematic review and meta-analysis",
"author": "Gungor",
"doi-asserted-by": "crossref",
"first-page": "173",
"journal-title": "Am. J. Emerg. Med.",
"key": "ref_91",
"volume": "39",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0268396",
"doi-asserted-by": "crossref",
"key": "ref_92",
"unstructured": "D’Ecclesiis, O., Gavioli, C., Martinoli, C., Raimondi, S., Chiocca, S., Miccolo, C., Bossi, P., Cortinovis, D., Chiaradonna, F., and Palorini, R. (2022). Vitamin D and SARS-CoV2 infection, severity and mortality: A systematic review and meta-analysis. PLoS ONE, 17."
},
{
"DOI": "10.1136/postgradmedj-2020-139065",
"article-title": "Short term, high-dose vitamin D supplementation for COVID-19 disease: A randomised, placebo-controlled, study (SHADE study)",
"author": "Rastogi",
"doi-asserted-by": "crossref",
"first-page": "87",
"journal-title": "Postgrad. Med. J.",
"key": "ref_93",
"volume": "98",
"year": "2022"
},
{
"DOI": "10.3389/fmed.2021.687220",
"article-title": "Abnormal Fibrinogen Level as a Prognostic Indicator in Coronavirus Disease Patients: A Retrospective Cohort Study",
"author": "Long",
"doi-asserted-by": "crossref",
"first-page": "687220",
"journal-title": "Front. Med.",
"key": "ref_94",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.3390/jcm9124134",
"doi-asserted-by": "crossref",
"key": "ref_95",
"unstructured": "Di Micco, P., Russo, V., Carannante, N., Imparato, M., Cardillo, G., and Lodigiani, C. (2020). Prognostic Value of Fibrinogen among COVID-19 Patients Admitted to an Emergency Department: An Italian Cohort Study. J. Clin. Med., 9."
},
{
"DOI": "10.2139/ssrn.3770003",
"doi-asserted-by": "crossref",
"key": "ref_96",
"unstructured": "Flisiak, R., Jaroszewicz, J., Rogalska, M., Łapiński, T., Berkan-Kawińska, A., Bolewska, B., Tudrujek-Zdunek, M., Kozielewicz, D., Rorat, M., and Leszczyński, P. (2021). Tocilizumab Improves the Prognosis of COVID-19 in Patients with High IL-6. J. Clin. Med., 10."
},
{
"DOI": "10.1371/journal.pone.0269368",
"doi-asserted-by": "crossref",
"key": "ref_97",
"unstructured": "Piscoya, A., del Riego, A.P., Cerna-Viacava, R., Rocco, J., Roman, Y.M., Escobedo, A.A., Pasupuleti, V., White, C.M., and Hernandez, A.V. (2022). Efficacy and harms of tocilizumab for the treatment of COVID-19 patients: A systematic review and meta-analysis. PLoS ONE, 17."
},
{
"DOI": "10.1002/rmv.2295",
"article-title": "Efficacy and secondary infection risk of tocilizumab, sarilumab and anakinra in COVID-19 patients: A systematic review and meta-analysis",
"author": "Peng",
"doi-asserted-by": "crossref",
"first-page": "e2295",
"journal-title": "Rev. Med. Virol.",
"key": "ref_98",
"volume": "32",
"year": "2022"
},
{
"article-title": "Tocilizumab in Addition to Standard of Care in the Management of COVID-19: A Meta-Analysis of RCTs",
"author": "Mutua",
"first-page": "e2022014",
"journal-title": "Acta Biomed.",
"key": "ref_99",
"volume": "93",
"year": "2022"
},
{
"article-title": "High-Dose Dexamethasone Versus Tocilizumab in Moderate to Severe COVID-19 Pneumonia: A Randomized Controlled Trial",
"author": "Naik",
"first-page": "e20353",
"journal-title": "Cureus",
"key": "ref_100",
"volume": "13",
"year": "2021"
},
{
"article-title": "Prognostic evaluation of Acinetobacter baumannii ventilator associated pneumonia in COVID-19",
"author": "Lupia",
"first-page": "570",
"journal-title": "Infez. Med.",
"key": "ref_101",
"volume": "30",
"year": "2022"
},
{
"article-title": "Effectiveness of Tocilizumab with and without Dexamethasone in Patients with Severe COVID-19: A Retrospective Study",
"author": "Jaroszewicz",
"first-page": "3359",
"journal-title": "J. Inflamm. Res.",
"key": "ref_102",
"volume": "ume 14",
"year": "2021"
},
{
"DOI": "10.1016/j.jiph.2021.11.017",
"article-title": "Outcomes associated with tocilizumab with or without corticosteroid versus dexamethasone for treatment of patients with severe to critical COVID-19 pneumonia",
"author": "AlQahtani",
"doi-asserted-by": "crossref",
"first-page": "36",
"journal-title": "J. Infect. Public Health",
"key": "ref_103",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1016/S2213-2600(22)00088-1",
"article-title": "Baricitinib versus dexamethasone for adults hospitalised with COVID-19 (ACTT-4): A randomised, double-blind, double placebo-controlled trial",
"author": "Wolfe",
"doi-asserted-by": "crossref",
"first-page": "888",
"journal-title": "Lancet Respir. Med.",
"key": "ref_104",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1136/bmjresp-2021-001049",
"article-title": "Understanding the burden of interstitial lung disease post-COVID-19: The UK Interstitial Lung Disease-Long COVID Study (UKILD-Long COVID)",
"author": "Wild",
"doi-asserted-by": "crossref",
"first-page": "e001049",
"journal-title": "BMJ Open Respir. Res.",
"key": "ref_105",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2022.947401",
"article-title": "Serum soluble Fas ligand is a severity and mortality prognostic marker for COVID-19 patients",
"author": "Saleki",
"doi-asserted-by": "crossref",
"first-page": "947401",
"journal-title": "Front. Immunol.",
"key": "ref_106",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1002/art.41763",
"article-title": "Discrimination of COVID-19 From Inflammation-Induced Cytokine Storm Syndromes Using Disease-Related Blood Biomarkers",
"author": "Kessel",
"doi-asserted-by": "crossref",
"first-page": "1791",
"journal-title": "Arthritis Rheumatol.",
"key": "ref_107",
"volume": "73",
"year": "2021"
},
{
"DOI": "10.1016/j.jim.2021.113174",
"article-title": "Antinuclear antibodies (ANAs) detected by indirect immunofluorescence (IIF) method in acute COVID-19 infection; future roadmap for laboratory diagnosis",
"author": "Peker",
"doi-asserted-by": "crossref",
"first-page": "113174",
"journal-title": "J. Immunol. Methods",
"key": "ref_108",
"volume": "499",
"year": "2021"
}
],
"reference-count": 108,
"references-count": 108,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2077-0383/12/6/2429"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Identification of Clinical Response Predictors of Tocilizumab Treatment in Patients with Severe COVID-19 Based on Single-Center Experience",
"type": "journal-article",
"volume": "12"
}
