Effect of Vitamin D3 supplementation vs. dietary-hygienic measures on SARS-COV-2 infection rates in hospital workers with 25-hydroxyvitamin D3 [25(OH)D3] levels >20 ng/mL
et al., medRxiv, doi:10.1101/2022.07.12.22277450, NCT04810949, Jul 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
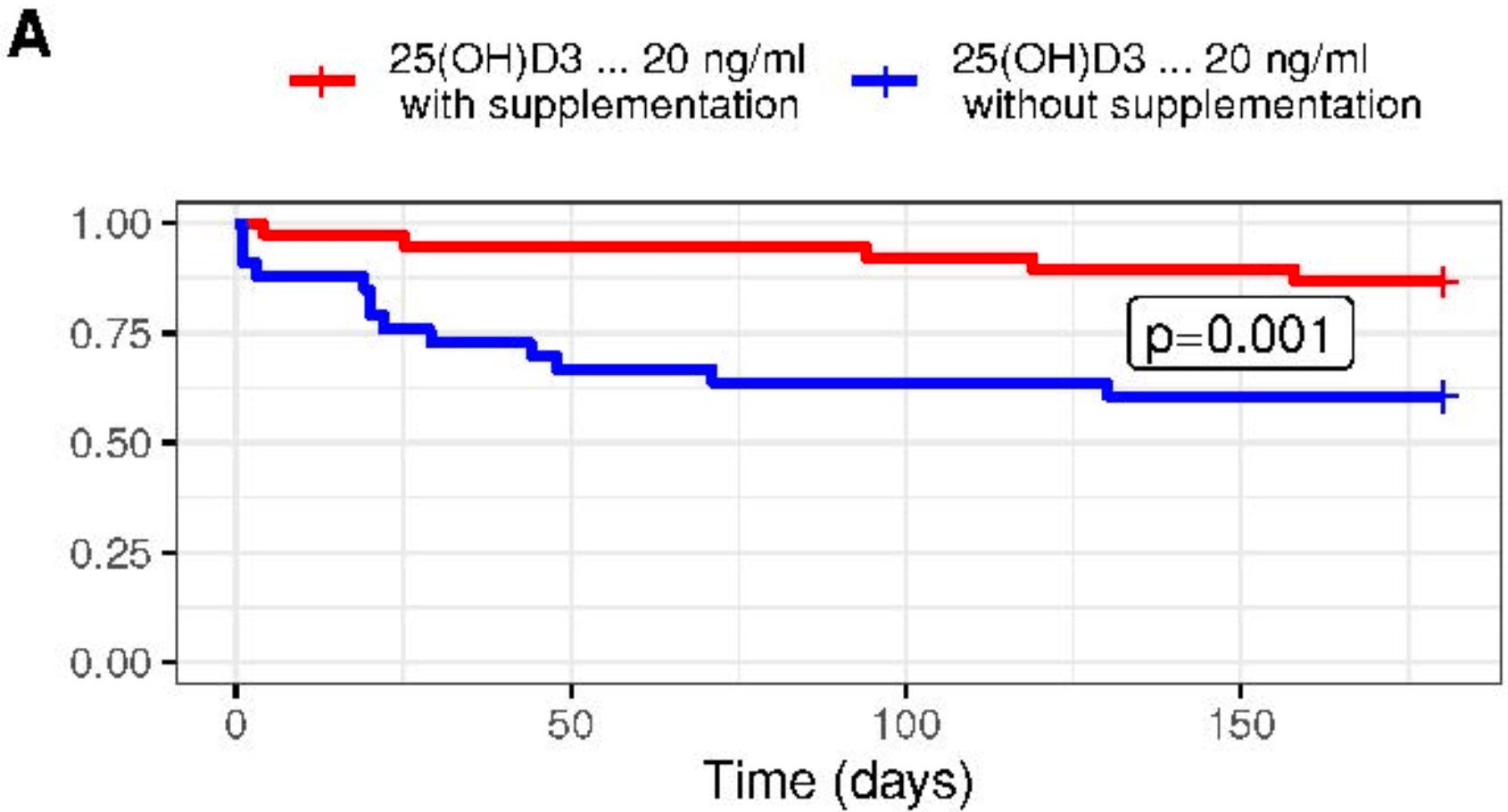
RCT healthcare workers with vitamin D levels between 20-100 ng/mL, 43 treated with vitamin D 52,000 IU monthly, and 42 with dietary-hygienic measures, which were also focused on increasing vitamin D, including sun exposure for at least 10 minutes per day between 10:00-18:00, and consuming foods rich in vitamin D. There was significantly lower risk of COVID-19 with supplementation vs. diet/sun. Authors also report on patients with levels <20 ng/mL where treatment was recommended for all patients, however many patients declined treatment. In these non-randomized patients, lower risk was seen at 4 months with vitamin D supplementation, however there was no significant difference at 6 months.
Interpretation of the results is difficult because all groups had intervention aimed at increasing vitamin D. Supplemented patients showed greater improvement in levels, however dietary/sun patients could have a therapeutic advantage due to regular versus monthly consumption, and due to other benefits of the dietary/sun intervention. Authors indicate they asked patients monthly about consumption of food with vitamin D, however no results are provided.
Bolus treatment is less effective.
Pharmacokinetics and the potential side effects of high bolus doses suggest
that ongoing treatment spread over time is more appropriate.
Research has confirmed that lower dose regular treatment with vitamin D is more
effective than intermittent high-dose bolus treatment for various conditions,
including rickets and acute respiratory infections1,2. The biological mechanisms supporting these
findings involve the induction of enzymes such as 24-hydroxylase and
fibroblast growth factor 23 (FGF23) by high-dose bolus treatments. These
enzymes play roles in inactivating vitamin D, which can paradoxically reduce
levels of activated vitamin D and suppress its activation for extended periods
post-dosage. Evidence indicates that 24-hydroxylase activity may remain
elevated for several weeks following a bolus dose, leading to reduced levels
of the activated form of vitamin D. Additionally, FGF23 levels can increase
for at least three months after a large bolus dose, which also contributes to
the suppression of vitamin D activation1.
|
risk of hospitalization, 73.7% higher, RR 1.74, p = 1.00, treatment 2 of 38 (5.3%), control 1 of 33 (3.0%), G1 vs. G2.
|
|
risk of case, 79.0% lower, HR 0.21, p = 0.008, treatment 5 of 38 (13.2%), control 13 of 33 (39.4%), NNT 3.8, 6 months, Cox proportional hazards, G1 vs. G2.
|
|
risk of case, 59.1% lower, RR 0.41, p = 0.04, treatment 6 of 43 (14.0%), control 14 of 41 (34.1%), NNT 5.0, 4 months, G1 vs. G2.
|
|
risk of case, 79.1% lower, RR 0.21, p = 0.003, treatment 3 of 43 (7.0%), control 14 of 42 (33.3%), NNT 3.8, 3 months, G1 vs. G2.
|
|
risk of ICU admission, 57.1% lower, RR 0.43, p = 1.00, treatment 0 of 24 (0.0%), control 1 of 72 (1.4%), NNT 72, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), G3 vs. G4.
|
|
risk of hospitalization, 350.0% higher, RR 4.50, p = 0.10, treatment 3 of 24 (12.5%), control 2 of 72 (2.8%), G3 vs. G4.
|
|
risk of case, 15.0% higher, HR 1.15, p = 0.72, treatment 9 of 24 (37.5%), control 29 of 72 (40.3%), 6 months, Cox proportional hazards, G3 vs. G4.
|
|
risk of case, 32.1% lower, RR 0.68, p = 0.35, treatment 7 of 27 (25.9%), control 29 of 76 (38.2%), NNT 8.2, 4 months, G3 vs. G4.
|
|
risk of case, 22.2% lower, RR 0.78, p = 0.64, treatment 7 of 28 (25.0%), control 27 of 84 (32.1%), NNT 14, 3 months, G3 vs. G4.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Romero-Ibarguengoitia et al., 15 Jul 2022, Randomized Controlled Trial, Mexico, preprint, mean age 44.4, 5 authors, study period May 2020 - August 2020, dosage 52,000IU single dose, monthly, this trial compares with another treatment - results may be better when compared to placebo, trial NCT04810949 (history).
Contact: drgzzcantu@gmail.com.
Effect of Vitamin D3 supplementation vs. dietary-hygienic measures on SARS-COV-2 infection rates in hospital workers with 25-hydroxyvitamin D3 [25(OH)D3] levels ≥20 ng/mL
doi:10.1101/2022.07.12.22277450
Background. There is scant information on the effect of supplementation with vitamin D 3 in SARS-COV-2 infection cases when patient D3] levels are between 20-100ng/mL. Our aim was to evaluate the effect of supplementation with vitamin D 3 vs. dietary-hygienic measures on the SARS-COV-2 infection rate in participants with serum 25(OH)D 3 levels >20ng/mL. Methods. We invited hospital workers with 25(OH)D 3 levels between 20-100 ng/mL and no previous SARS-COV-2 infection; they were randomized as follows: treatment options were a) vitamin D 3 supplementation (52,000 IU monthly, G1) or b) dietary-hygienic measures (G2). We conducted a 3-to 6-month follow-up of SARS-COV-2 infections. Participants with 25(OH)D 3 levels <20 ng/mL were also analyzed. We divided these latter participants depending on whether they were supplemented (G3) or not (G4). Results. We analyzed 198 participants, with an average age of 44.4 (SD 9) years, and 130 (65.7%) were women. G1 had less cases of SARS-COV-2 infection than G2 after a follow-up of 3-to 6months (p<0.05). There were no differences between G3 and G4 at the 3-and 6-month follow-up cutoff points (p>0.05). Using mixed effect Cox regression analysis in 164 participants that completed six months of follow-up, vitamin D 3 supplementation appeared to act as a protective factor against SARS-COV-2 infection (HR 0.21, p=0.008) in G1 and G2. None of the participants treated with the supplementation doses had serum 25(OH)D 3 levels > 100ng/mL.
Conclusion. Vitamin D 3 supplementation in participants with 25(OH)D 3 levels between 20-100 ng/mL have a lower rate of SARS-COV-2 infection in comparison with the use of dietaryhygienic measures at six months follow-up.
Competing interests: The author(s) have no conflicts of interest to declare.
Ethics Statement: This research project was approved by the local IRB of the Universidad de Monterrey (Ref.
30062020-a-CN-CI ). An informed consent form was obtained from each participant. .
Disclosure The authors have no potential conflicts of interest associated with this study. Author Approval: all authors read an approved the final version of the manuscript. Protocol access: This study protocol can be reviewed in Clinicaltrials.gov. supplementation; G2: 25(OH)D3 >20 ng/mL without supplementation; G3: 25(OH)D3 <20 ng/mL with supplementation; G4 25(OH)D3 <20 ng/mL without supplementation.
References
Bilezikian, ENDOCRINOLOGY: Vitamin D and COVID
Bouillon, Verlinden, Verstuyf, Is Vitamin D2 Really Bioequivalent to Vitamin D3?, Endocrinology
Chen, Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study, The Lancet
Cherrie, Ultraviolet A radiation and COVID 19 deaths in the USA with replication studies in England and Italy*, Br. J. Dermatol
Chiodini, Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes, Front. Public Health
Crowe, Plasma concentrations of 25-hydroxyvitamin D in meat eaters, fish eaters, vegetarians and vegans: results from the EPIC-Oxford study, Public Health Nutr
De Niet, A Randomized Study to Compare a Monthly to a Daily Administration of Vitamin D3 Supplementation, Nutrients
Demir, Demir, Aygun, Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease, J. Med. Virol
Dror, Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness, PLOS ONE
Džopalić, Božić-Nedeljković, Jurišić, The role of vitamin A and vitamin D in the modulation of the immune response with focus on innate lymphoid cells, Cent. Eur. J. Immunol
Ejaz, COVID-19 and comorbidities: Deleterious impact on infected patients, J. Infect. Public Health
Gorman, Weller, Investigating the Potential for Ultraviolet Light to Modulate Morbidity and Mortality From COVID-19: A Narrative Review and Update, Front. Cardiovasc. Med
Griffin, Perspective: Vitamin D supplementation prevents rickets and acute respiratory infections when given as daily maintenance but not as intermittent bolus: implications for COVID-19, Clin. Med
Holick, Treatment, and Prevention of Vitamin D Deficiency: an Endocrine Society Clinical Practice Guideline, J. Clin. Endocrinol. Metab
Holick, Vitamin, Deficiency, None, N. Engl. J. Med
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin. Exp. Res
Jiang, Review of the Clinical Characteristics of Coronavirus Disease 2019 (COVID-19), J. Gen. Intern. Med
Loucera, Real world evidence of calcifediol or vitamin D prescription and mortality rate of COVID-19 in a retrospective cohort of hospitalized Andalusian patients, Sci. Rep
Martinez Moreno, Vitamin D modulates tissue factor and protease activated receptor 2 expression in vascular smooth muscle cells, FASEB J
Mattoli, Filling the Gap Until Full Vaccine Deployment in the War on Coronavirus Disease-19, Infect. Dis. Ther
Oristrell, Vitamin D supplementation and COVID-19 risk: a population-based, cohort study, J. Endocrinol. Invest
Quesada-Gomez, Entrenas-Castillo, Bouillon, Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections: Revised Ms SBMB 2020_166, J. Steroid Biochem. Mol. Biol
Santi, Impact of the Pandemic on NonInfected Cardiometabolic Patients: A Survey in Countries of Latin America-Rationale and Design of the CorCOVID LATAM Study, CJC Open
Schulz, Altman, Moher, Group, None
Seal, Association of Vitamin D Status and COVID-19-Related Hospitalization and Mortality, J. Gen. Intern. Med
Spiteri, First cases of coronavirus disease 2019 (COVID-19) in the WHO European Region, Eurosurveillance
Szarpak, A systematic review and meta-analysis of effect of vitamin D levels on the incidence of COVID-19, Cardiol. J
Teshome, Adane, Girma, Mekonnen, The Impact of Vitamin D Level on COVID-19 Infection: Systematic Review and Meta-Analysis, Front. Public Health
Villasis-Keever, Efficacy and Safety of Vitamin D Supplementation to Prevent COVID-19 in Frontline Healthcare Workers. A Randomized Clinical Trial, Arch. Med. Res
