Analysis of trace elements (Zn and Cu) levels in COVID-19 patients with ICU and Non-ICU hospitalization
et al., Research Square, doi:10.21203/rs.3.rs-2418159/v1, Jan 2023
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000028 from 47 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
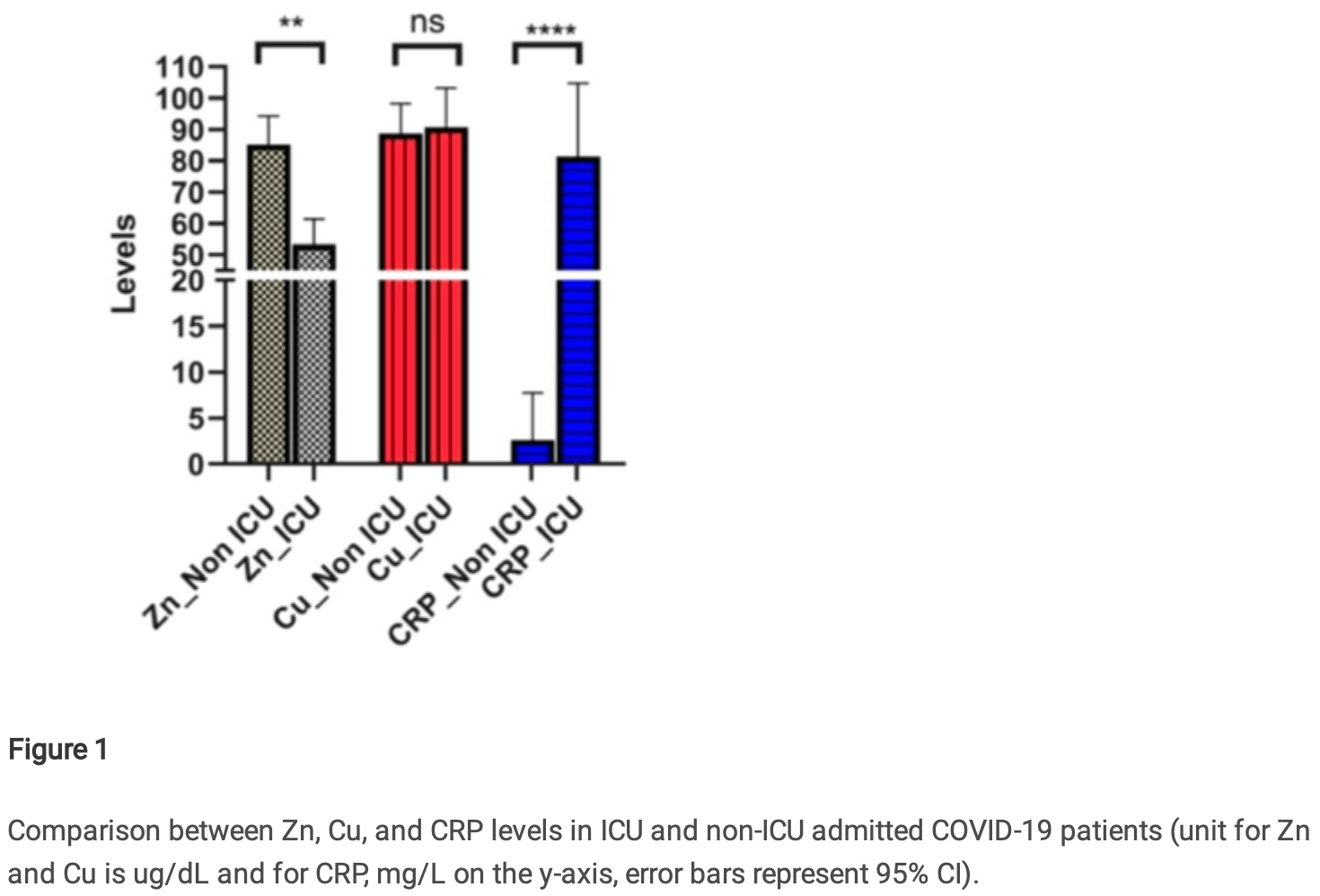
Prospective analysis of 122 hospitalized COVID-19 patients, showing significantly lower zinc levels in ICU patients compared with non-ICU patients. Zinc levels were lower in non-survivors compared with survivors, without statistical significance.
Ram et al., 3 Jan 2023, prospective, preprint, 10 authors, study period July 2020 - November 2020.
Analysis of trace elements (Zn and Cu) levels in COVID-19 patients with ICU and Non-ICU hospitalization
doi:10.21203/rs.3.rs-2418159/v1
Background: The persistence of the COVID-19 pandemic besides its current resurgence and continuously increasing fatalities indicates a vital need for severity assessment at its early stages. Recent studies have already ascribed mortality to chronic in ammation. But the part of trace elements, especially zinc and copper that have been known to possess antiviral roles for a long time is least studied in COVID-19. Methods: The study comprised 122 COVID-19-positive participants admitted to the tertiary care hospital. Among them, eighty-one (~66%) were admitted to ICU under high severity. Levels of Zn and Cu along with CRP were analyzed and compared among ICU and non-ICU admitted patients. Using ROC analysis, the potential and precise levels for de ning severity were determined. Results: We found a signi cant reduction in Zn levels (p=0.001) in ICU-admitted patients compared to the non-ICU group which was more pronounced in females and patients aged above 50 years. Reduction in the levels of Zn is accompanied by elevated CRP levels (p<0.001) in ICU patients with no effect on Cu levels. Upon ROC analysis, Zn and CRP were found to have signi cant AUC (p<0.0001). Further, CRP to Zn ratio displayed improved AUC with 90% sensitivity indicating their applicability to predict ICU requirements. Conclusions: The present study was primarily aimed to predict the status of zinc and copper in COVID-19 patients and their utility as a prognostic tool for deciding the severity. Our ndings indicate that CRP to Zn ratio might feasibly be used to predict the progression of COVID-19 toward severity.
References
Akinloye, Oyewale, Oguntibeju, Evaluation of trace elements in pregnant women with preeclampsia, African J Biotechnol
Anuk, Polat, Akdas, Erol, Tanacan et al., The Relation Between Trace Element Status (Zinc, Copper, Magnesium) and Clinical Outcomes in COVID-19 Infection During Pregnancy, Biol Trace Elem Res, doi:10.1007/s12011-020-02496-y
Armbruster, Pry, Limit of blank, limit of detection and limit of quantitation, Clin Biochem Rev
Bao, Knoell, Zinc modulates cytokine-induced lung epithelial cell barrier permeability, Am J Physiol -Lung Cell Mol Physiol, doi:10.1152/ajplung.00207.2006
Channappanavar, Fehr, Vijay, Dysregulated Type I Interferon and In ammatory Monocyte-Macrophage Responses Cause Lethal Pneumonia in SARS-CoV-Infected Mice
Chen, Zhou, Dong, Qu, Gong et al., Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study, Lancet, doi:10.1016/S0140-6736(20)30211-7
Dharmalingam, Birdi, Tomo, Sreenivasulu, Charan et al., Trace Elements as Immunoregulators in SARS-CoV-2 and Other Viral Infections, Indian J Clin Biochem, doi:10.1007/s12291-021-00961-6
Fujimori, Sato, Hayata, Nagao, Nakayam et al., Novel antiviral characteristics of nanosized copper(i) iodide particles showing inactivation activity against 2009 pandemic H1N1 in uenza virus, Appl Environ Microbiol, doi:10.1128/AEM.06284-11
Galloway, Mcmillan, Sattar, Effect of the in ammatory response on trace element and vitamin status, Ann Clin Biochem, doi:10.1258/0004563001899429
Gammoh, Rink, Zinc in infection and in ammation, Nutrients, doi:10.3390/nu9060624
Godfrey, Godfrey, Godfrey, Riley, A randomized clinical trial on the treatment of oral herpes with topical zinc oxide/glycine, Altern Ther Health Med
Hemilä, Zinc lozenges and the common cold: a meta-analysis comparing zinc acetate and zinc gluconate, and the role of zinc dosage, JRSM Open, doi:10.1177/2054270417694291
Heyninck, Beyaert, The cytokine-inducible zinc nger protein A20 inhibits IL-1-induced NF-κB activation at the level of TRAF6, FEBS Lett, doi:10.1016/S0014-5793(98)01645-7
Hoffman, Zinc-induced copper de ciency, Lancet, doi:10.1016/S0140-6736(87)92233-1
Huang, Failla, Copper De ciency Suppresses Effector Activities of Differentiated U937 cells
Ibs, Function, Rink, Zinc-Altered Immune Function, Sci York
Iovino, Mazziotta, Carulli, Guerrini, Morganti et al., High-dose zinc oral supplementation after stem cell transplantation causes an increase of TRECs and CD4+ naïve lymphocytes and prevents TTV reactivation, Leuk Res, doi:10.1016/j.leukres.2018.04.016
Jothimani, Kailasam, Danielraj, Nallathambi, COVID-19: Poor outcomes in patients with zinc deifciency, Int J Infect Dis, doi:10.1016/j.ijid.2020.09.014
Kirmit, Kader, Aksoy, Bal, Nural et al., Trace elements and oxidative stress status in patients with psoriasis, Postep Dermatologii i Alergol, doi:10.5114/ada.2020.94265
Laine, Tuomainen, Salonen, Virtanen, Serum copper-to-zinc-ratio and risk of incident infection in men: the Kuopio Ischaemic Heart Disease Risk Factor Study, Eur J Epidemiol, doi:10.1007/s10654-020-00644-1
Markowicz, Donat, Glaude, Pommier, Curlier et al., Level of CRP predicts need for respiratory support in hospitalized COVID-19 patients
Novello, Stirpe, The effects of copper and other ions on the ribonucleic acid polymerase activity of isolated rat liver nuclei, Biochem J, doi:10.1042/bj1110115
Pal, Ram, Zohmangaihi, Biswas, Suri et al., High Prevalence of Hypocalcemia in Nonsevere COVID-19 Patients : A Retrospective Case-Control Study, doi:10.3389/fmed.2020.590805
Pal, Squitti, Picozza, Pawar, Rongioletti et al., Zinc and COVID-19: Basis of Current Clinical Trials, Biol Trace Elem Res, doi:10.1007/s12011-020-02437-9
Pathak, Kapil, Kapoor, Dwivedi, Singh, Magnitude of zinc de ciency among nulliparous nonpregnant women in a rural community of Haryana State, India, Food Nutr Bull, doi:10.1177/156482650302400407
Perrin, Oxford, Inhibition of the particle-associated RNA-dependent RNA polymerase activity of in uenza viruses by chelating agents, J Gen Virol
Pisano, Hilas, Zinc and taste disturbances in older adults: A review of the literature, Consult Pharm, doi:10.4140/TCP.n.2016.267
Reeves, Dell, Effects of dietary zinc deprivation on the activity of angiotensin-converting enzyme in serum of rats and guinea pigs, J Nutr, doi:10.1093/jn/116.1.128
Sagripanti, Routson, Bonifacino, Lytle, Mechanism of copper-mediated inactivation of herpes simplex virus, Antimicrob Agents Chemother, doi:10.1128/aac.41.4.812
Sagripanti, Routson, Lytle, Virus inactivation by copper or iron ions alone and in the presence of peroxide, Appl Environ Microbiol, doi:10.1128/aem.59.12.4374-4376.1993
Saigal, Hanekom, Does zinc improve symptoms of viral upper respiratory tract infection? Evidence-Based, Pract, doi:10.1097/EBP.0000000000000489
Saini, Saini, Ram, Soni, Suri et al., COVID-19 associated variations in liver function parameters: A retrospective study, Postgrad Med J, doi:10.1136/postgradmedj-2020-138930
Samadi, Isikhan, Tinkov, Lay, Doşa et al., Zinc, copper, and oxysterol levels in patients with type 1 and type 2 diabetes mellitus, Clin Nutr, doi:10.1016/j.clnu.2019.07.026
Schroeder, Cousins, Interleukin 6 regulates metallothionein gene expression and zinc metabolism in hepatocyte monolayer cultures, Proc Natl Acad Sci U S A, doi:10.1073/pnas.87.8.3137
Sharifpour, Rangaraju, Liu, Alabyad, Nahab et al., C-Reactive protein as a prognostic indicator in hospitalized patients with COVID-19, PLoS One, doi:10.1371/journal.pone.0242400
Speth, Carrera, Jean-Baptiste, Joachim, Concentration-dependent effects of zinc on angiotensin-converting enzyme-2 activity (1067.4), Fed Am Soc Exp Biol, doi:10.1096/fasebj.28.1_supplement.1067.4
Tang, Liu, Zhang, Xu, Wen, Cytokine Storm in COVID-19: The Current Evidence and Treatment Strategies, Front Immunol, doi:10.3389/mmu.2020.01708
Thomas, Patel, Bittel, Wolski, Wang et al., Effect of High-Dose Zinc and Ascorbic Acid Supplementation vs Usual Care on Symptom Length and Reduction among Ambulatory Patients with SARS-CoV-2 Infection: The COVID A to Z Randomized Clinical Trial, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.0369
Turner, Cetnarowski, Effect of treatment with zinc gluconate or zinc acetate on experimental and natural colds, Clin Infect Dis, doi:10.1086/317437
Van, Morris, Mg, Gamble, Bn, Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1, N Engl J Med, doi:10.1056/NEJMc2004973
Velthuis, Van Den Worml, Sims, Baric, Snijder et al., Zn2+ inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture, PLoS Pathog, doi:10.1371/journal.ppat.1001176
Vogel-González, Talló-Parra, Herrera-Fernández, Pérez-Vilaró, Chillón et al., Low zinc levels at admission associates with poor clinical outcomes in sars-cov-2 infection, Nutrients, doi:10.3390/nu13020562
Wang, C-reactive protein levels in the early stage of COVID-19 2020, doi:10.1016/j.medmal.2020.03.007
