International Multicenter Study Comparing Cancer to Non-Cancer Patients with COVID-19: Impact of Risk Factors and Treatment Modalities on Survivorship
et al., medRxiv, doi:10.1101/2022.08.25.22279181, Aug 2022
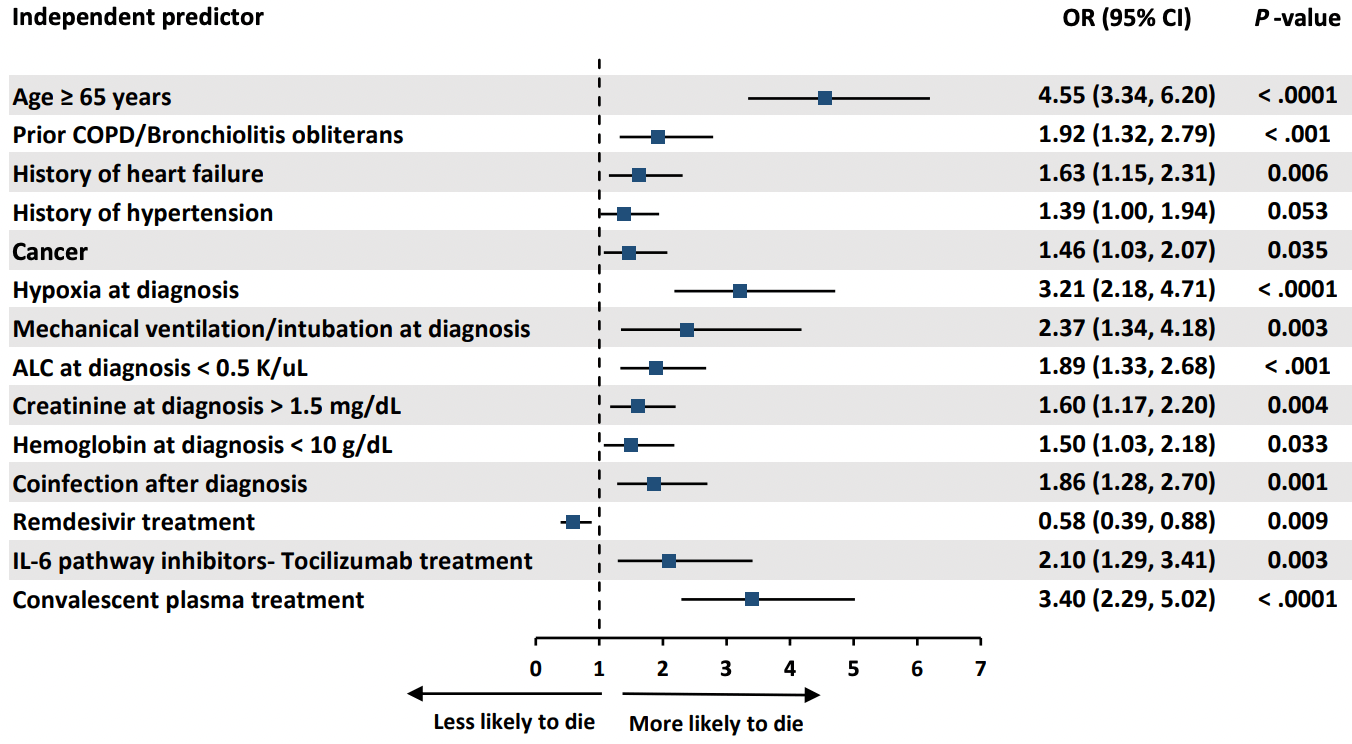
Retrospective 3,966 COVID-19 patients, 1,115 with cancer, showing lower mortality with remdesivir and higher mortality with convalescent plasma.
Study covers convalescent plasma and remdesivir.
|
risk of death, 240.0% higher, OR 3.40, p < 0.001, treatment 284, control 3,682, adjusted per study, multivariable, day 30, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Raad et al., 26 Aug 2022, retrospective, multiple countries, preprint, 52 authors, study period January 2020 - November 2020.
Contact: achaftari@mdanderson.org, rhachem@mdanderson.org.
International Multicenter Study Comparing Cancer to Non-Cancer Patients with COVID-19: Impact of Risk Factors and Treatment Modalities on Survivorship
doi:10.1101/2022.08.25.22279181
Background: In this international multicenter study we aimed to determine the independent risk factors associated with increased 30-day mortality and the impact of novel treatment modalities in a large group of cancer and non-cancer patients with COVID-19 from multiple countries.
Methods: We retrospectively collected de-identified data on a cohort of cancer and non-cancer patients diagnosed with COVID-19 between January and November 2020, from 16 international centers. Results: We analyzed 3966 COVID-19 confirmed patients, 1115 cancer and 2851 non-cancer patients. Cancer patients were more likely to be pancytopenic, and have a smoking history, pulmonary disorders, hypertension, diabetes mellitus, and corticosteroid use in the preceding two weeks (p≤0.01). In addition, they were more likely to present with higher inflammatory biomarkers (D-dimer, ferritin and procalcitonin), but were less likely to present with clinical symptoms (p≤0.01). By multivariable logistic regression analysis, cancer was an independent risk factor for 30-day mortality (OR 1.46; 95% CI 1.03 to 2.07; p=0.035). Older age (≥65 years) was the strongest predictor of 30-day mortality in all patients (OR 4.55; 95% CI 3.34 to6.20; p< 0.0001). Remdesivir was the only therapeutic agent independently associated with decreased 30day mortality (OR 0.58; CI 0.39-0.88; p=0.009). Among patients on low-flow oxygen at admission, patients who received remdesivir had a lower 30-day mortality rate than those who did not (5.9% vs 17.6%; p=0.03).
Conclusions: Cancer is an independent risk factor for increased 30-day all-cause mortality from COVID-19. Remdesivir, particularly in patients receiving low-flow oxygen, can reduce 30-day all-cause mortality. .
References
Albiges, Foulon, Bayle, Determinants of the outcomes of patients with cancer infected with SARS-CoV-2: results from the Gustave Roussy cohort, Nat Cancer
Beigel, Tomashek, Dodd, Remdesivir for the Treatment of Covid-19 -Final Report
Bernal, Da Silva, Musungaie, Molnupiravir for Oral Treatment of Covid-19 in Nonhospitalized Patients, N Engl J Med
Chavez-Macgregor, Lei, Zhao, Scheet, Giordano, Evaluation of COVID-19 Mortality and Adverse Outcomes in US Patients With or Without Cancer, JAMA Oncol
Gottlieb, Vaca, Paredes, Early Remdesivir to Prevent Progression to Severe Covid-19 in Outpatients, N Engl J Med
He, Chen, Chen, COVID-19 in persons with haematological cancers, Leukemia
Janiaud, Axfors, Schmitt, Association of Convalescent Plasma Treatment With Clinical Outcomes in Patients With COVID-19: A Systematic Review and Meta-analysis, JAMA
Klassen, Sj, Johnson, Carter, Wiggins et al., The Effect of convalescent plasma therapy on COVID-19 patient mortality: systematic review and meta-analysis, Mayo Clinic Proceedings
Kucirka, Lauer, Laeyendecker, Boon, Lessler, Variation in False-Negative Rate of Reverse Transcriptase Polymerase Chain Reaction-Based SARS-CoV-2 Tests by Time Since Exposure, Ann Intern Med
Kuderer, Choueiri, Shah, Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study, Lancet
Lai, Chen, Wang, Chen, Wang et al., Clinical efficacy and safety of remdesivir in patients with COVID-19: a systematic review and network meta-analysis of randomized controlled trials, J Antimicrob Chemother
Lee, Cazier, Angelis, COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study, Lancet
Libster, Marc, Wappner, Early High-Titer Plasma Therapy to Prevent Severe Covid-19 in Older Adults, N Engl J Med
Liu, Lin, Baine, Convalescent plasma treatment of severe COVID-19: a propensity score-matched control study, Nat Med
Lunski, Burton, Tawagi, Multivariate mortality analyses in COVID-19: Comparing patients with cancer and patients without cancer in Louisiana
Mahase, Covid-19: Pfizer's paxlovid is 89% effective in patients at risk of serious illness, company reports, BMJ
Mehta, Goel, Kabarriti, Case Fatality Rate of Cancer Patients with COVID-19 in a New York Hospital System, Cancer Discov
Mozaffari, Chandak, Zhang, Remdesivir treatment in hospitalized patients with COVID-19: a comparative analysis of in-hospital all-cause mortality in a large multi-center observational cohort, Clin Infect Dis
Reafc-Twg, Sterne, Murthy, Association Between Administration of Systemic Corticosteroids and Mortality Among Critically Ill Patients With COVID-19: A Meta-analysis, JAMA
Recovery, Horby, Lim, Dexamethasone in Hospitalized Patients with Covid-19, N Engl J Med
Rezagholizadeh, Khiali, Sarbakhsh, Entezari-Maleki, Remdesivir for treatment of COVID-19; an updated systematic review and meta-analysis, Eur J Pharmacol
Rivera, Peters, Panagiotou, Utilization of COVID-19 Treatments and Clinical Outcomes among Patients with Cancer: A COVID-19 and Cancer Consortium (CCC19) Cohort Study, Cancer Discov
Robilotti, Babady, Mead, Determinants of COVID-19 disease severity in patients with cancer, Nat Med
Ruthrich, Giessen-Jung, Borgmann, COVID-19 in cancer patients: clinical characteristics and outcome-an analysis of the LEOSS registry, Ann Hematol
Salazar, Christensen, Graviss, Significantly Decreased Mortality in a Large Cohort of Coronavirus Disease 2019 (COVID-19) Patients Transfused Early with Convalescent Plasma Containing High-Titer Anti-Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Spike Protein IgG, Am J Pathol
Shrestha, Budhathoki, Syed, Rawal, Raut et al., Remdesivir: A potential gamechanger or just a myth? A systematic review and meta-analysis, Life Sci
Siddiqi, Mehra, COVID-19 illness in native and immunosuppressed states: A clinicaltherapeutic staging proposal, J Heart Lung Transplant
Siemieniuk, Bartoszko, Ge, Drug treatments for covid-19: living systematic review and network meta-analysis, BMJ
Stc, Pan, Peto, Repurposed Antiviral Drugs for Covid-19 -Interim WHO Solidarity Trial Results, N Engl J Med
Tian, Yuan, Xiao, Clinical characteristics and risk factors associated with COVID-19 disease severity in patients with cancer in Wuhan, China: a multicentre, retrospective, cohort study, Lancet Oncol
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
DOI record:
{
"DOI": "10.1101/2022.08.25.22279181",
"URL": "http://dx.doi.org/10.1101/2022.08.25.22279181",
"abstract": "<jats:p>Background: In this international multicenter study we aimed to determine the independent risk factors associated with increased 30-day mortality and the impact of novel treatment modalities in a large group of cancer and non-cancer patients with COVID-19 from multiple countries.\n Methods: We retrospectively collected de-identified data on a cohort of cancer and non-cancer patients diagnosed with COVID-19 between January and November 2020, from 16 international centers.\nResults: We analyzed 3966 COVID-19 confirmed patients, 1115 cancer and 2851 non-cancer patients. Cancer patients were more likely to be pancytopenic, and have a smoking history, pulmonary disorders, hypertension, diabetes mellitus, and corticosteroid use in the preceding two weeks (p≤0.01). In addition, they were more likely to present with higher inflammatory biomarkers (D-dimer, ferritin and procalcitonin), but were less likely to present with clinical symptoms (p≤0.01). By multivariable logistic regression analysis, cancer was an independent risk factor for 30-day mortality (OR 1.46; 95% CI 1.03 to 2.07; p=0.035). Older age (≥65 years) was the strongest predictor of 30-day mortality in all patients (OR 4.55; 95% CI 3.34 to6.20; p< 0.0001). Remdesivir was the only therapeutic agent independently associated with decreased 30-day mortality (OR 0.58; CI 0.39-0.88; p=0.009). Among patients on low-flow oxygen at admission, patients who received remdesivir had a lower 30-day mortality rate than those who did not (5.9% vs 17.6%; p=0.03). \nConclusions: Cancer is an independent risk factor for increased 30-day all-cause mortality from COVID-19. Remdesivir, particularly in patients receiving low-flow oxygen, can reduce 30-day all-cause mortality.</jats:p>",
"accepted": {
"date-parts": [
[
2022,
8,
26
]
]
},
"author": [
{
"affiliation": [],
"family": "Raad",
"given": "Issam",
"sequence": "first"
},
{
"affiliation": [],
"family": "Hachem",
"given": "Ray",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nigo",
"given": "Masayuki",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Datoguia",
"given": "Tarcila",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dagher",
"given": "Hiba",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jiang",
"given": "Ying",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6064-6837",
"affiliation": [],
"authenticated-orcid": false,
"family": "Subbiah",
"given": "Vivek",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Siddiqui",
"given": "Bilal",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bayle",
"given": "Arnaud",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Somer",
"given": "Robert",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fernandez-Cruz",
"given": "Ana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gorak",
"given": "Edward",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bhinder",
"given": "Arvinder",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nobuyoshi",
"given": "Mori",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hamerschlak",
"given": "Nelson",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shelanski",
"given": "Samuel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dragovich",
"given": "Tomislav",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kiat",
"given": "Yee Elise Vong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fakhreddine",
"given": "Suha",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hanna",
"given": "Pierre Abi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chemaly",
"given": "Roy F",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mulanovich",
"given": "Victor",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Adachi",
"given": "Javier A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Borjan",
"given": "Jovan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Khawaja",
"given": "Fareed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Granwehr",
"given": "Bruno",
"sequence": "additional"
},
{
"affiliation": [],
"family": "John",
"given": "Teny",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Guevara",
"given": "Eduardo Yepez",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Torres",
"given": "Harrys",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ammakkanavar",
"given": "Natraj Reddy",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yibirin",
"given": "Marcel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Reyes",
"given": "Cielito",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pande",
"given": "Mala",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ali",
"given": "Noman",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rojo",
"given": "Raniv",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ali",
"given": "Shahnoor",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Deeba",
"given": "Rita",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chaftari",
"given": "Patrick",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Matsuo",
"given": "Takahiro",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ishikawa",
"given": "Kazuhiro",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hasegawa",
"given": "Ryo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Aguado-Noya",
"given": "Ramon",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Garcia",
"given": "Alvaro Garcia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Puchol",
"given": "Cristina Traseira",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lee",
"given": "Dong-Gun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Slavin",
"given": "Monica",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0213-5470",
"affiliation": [],
"authenticated-orcid": false,
"family": "Teh",
"given": "Benjamin W",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Arias",
"given": "Cesar A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kontoyiannis",
"given": "Dimitrios",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Malek",
"given": "Alexandre E.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8097-8452",
"affiliation": [],
"authenticated-orcid": false,
"family": "Chaftari",
"given": "Anne Marie",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Data-Driven Determinants for COVID-19 Oncology Discovery Effort (D3CODE) Team",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
8,
26
]
],
"date-time": "2022-08-26T20:15:19Z",
"timestamp": 1661544919000
},
"deposited": {
"date-parts": [
[
2022,
8,
26
]
],
"date-time": "2022-08-26T20:15:19Z",
"timestamp": 1661544919000
},
"group-title": "Infectious Diseases (except HIV/AIDS)",
"indexed": {
"date-parts": [
[
2022,
8,
26
]
],
"date-time": "2022-08-26T20:41:45Z",
"timestamp": 1661546505711
},
"institution": [
{
"name": "medRxiv"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
8,
26
]
]
},
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2022.08.25.22279181",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2022,
8,
26
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2022,
8,
26
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "http://medrxiv.org/lookup/doi/10.1101/2022.08.25.22279181"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "International Multicenter Study Comparing Cancer to Non-Cancer Patients with COVID-19: Impact of Risk Factors and Treatment Modalities on Survivorship",
"type": "posted-content"
}
raad2