A Pilot Study on Oxidative Stress during the Recovery Phase in Critical COVID-19 Patients in a Rehabilitation Facility: Potential Utility of the PAOT® Technology for Assessing Total Anti-Oxidative Capacity
et al., Biomedicines, doi:10.3390/biomedicines11051308, Apr 2023
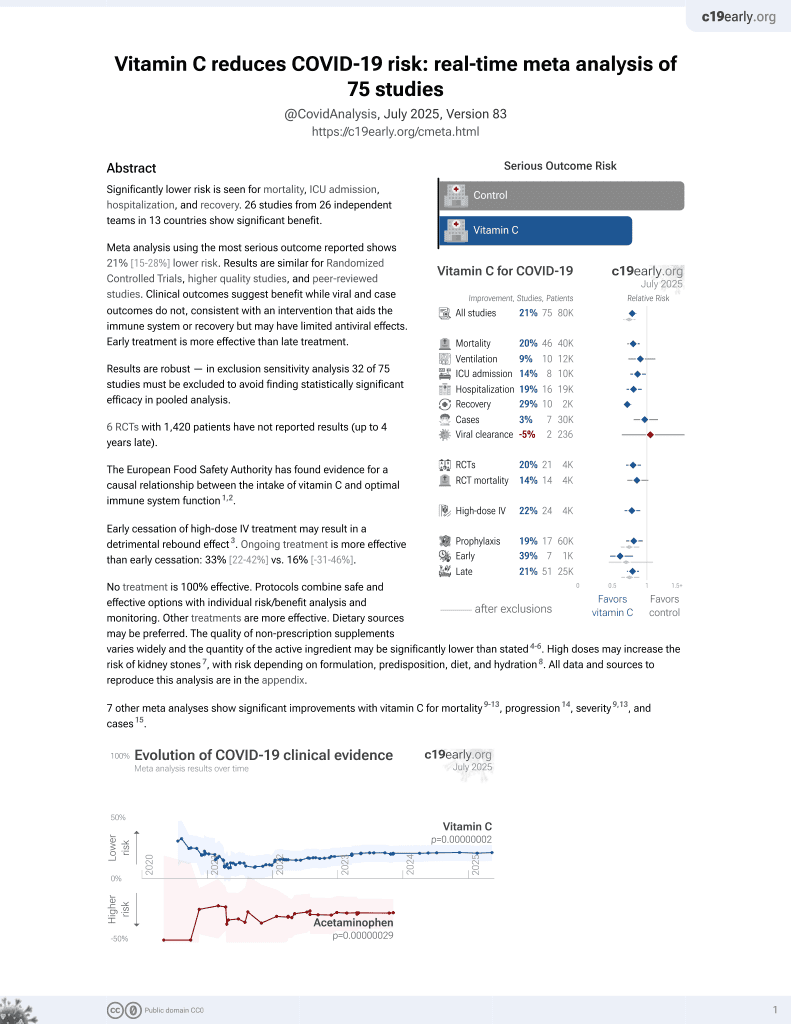
Vitamin C for COVID-19
6th treatment shown to reduce risk in
September 2020, now with p = 0.000000076 from 73 studies, recognized in 22 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
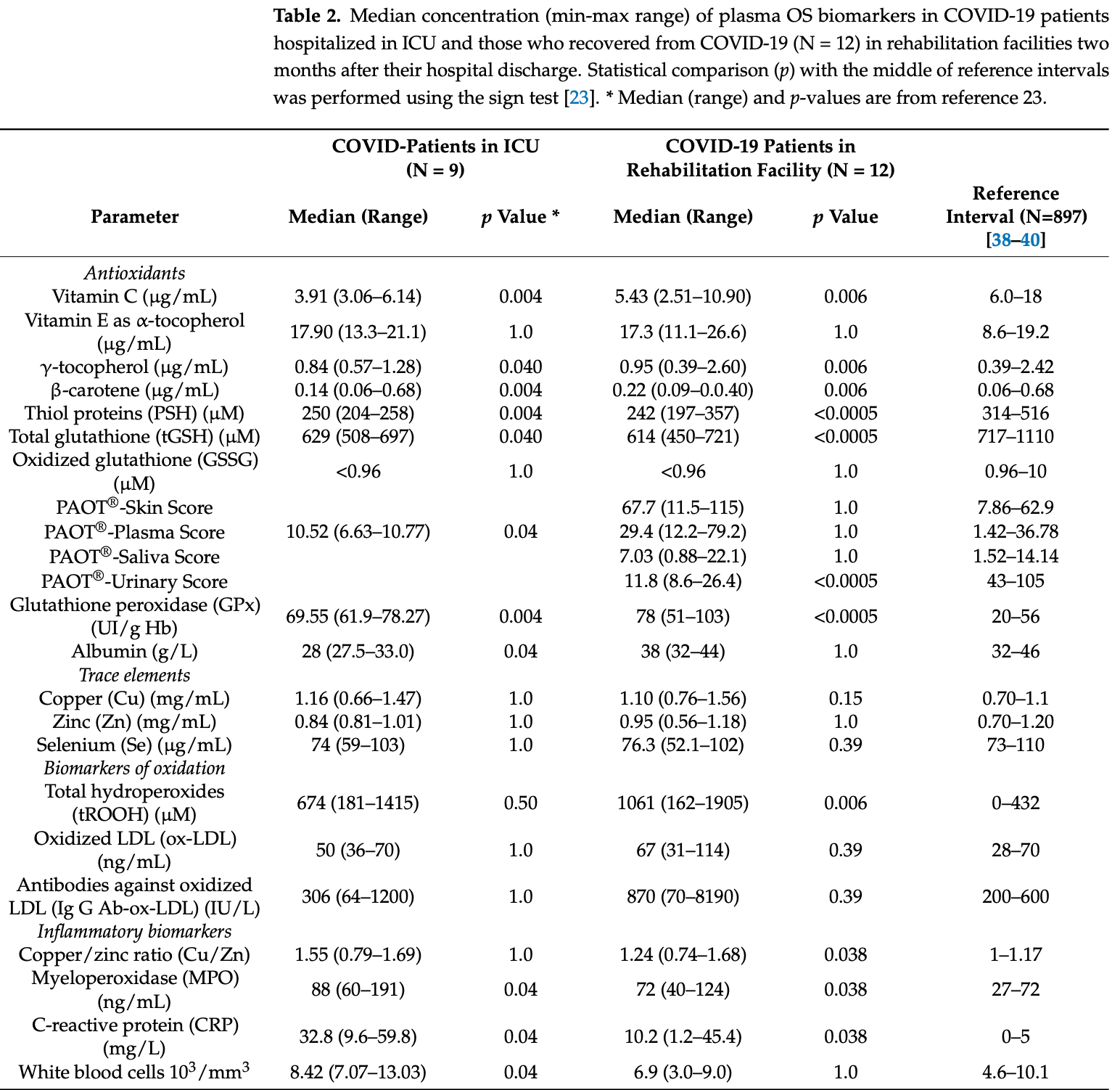
Analysis of 12 COVID-19 ICU patients showing vitamin C levels significantly below the reference range, and remaining low 2 months after discharge.
Pincemail et al., 28 Apr 2023, Belgium, peer-reviewed, 16 authors.
Contact: j.pincemail@chuliege.be (corresponding author).
A Pilot Study on Oxidative Stress during the Recovery Phase in Critical COVID-19 Patients in a Rehabilitation Facility: Potential Utility of the PAOT® Technology for Assessing Total Anti-Oxidative Capacity
Biomedicines, doi:10.3390/biomedicines11051308
Background: Oxidative stress (OS) could cause various COVID-19 complications. Recently, we have developed the Pouvoir AntiOxydant Total (PAOT®) technology for reflecting the total antioxidant capacity (TAC) of biological samples. We aimed to investigate systemic oxidative stress status (OSS) and to evaluate the utility of PAOT®for assessing TAC during the recovery phase in critical COVID-19 patients in a rehabilitation facility. Materials and Methods: In a total of 12 critical COVID-19 patients in rehabilitation, 19 plasma OSS biomarkers were measured: antioxidants, TAC, trace elements, oxidative damage to lipids, and inflammatory biomarkers. TAC level was measured in plasma, saliva, skin, and urine, using PAOT and expressed as PAOT-Plasma, -Saliva, -Skin, and -Urine scores, respectively. Plasma OSS biomarker levels were compared with levels from previous studies on hospitalized COVID-19 patients and with the reference population. Correlations between four PAOT scores and plasma OSS biomarker levels were analyzed. Results: During the recovery phase, plasma levels in antioxidants (γ-tocopherol, β-carotene, total glutathione, vitamin C and thiol proteins) were significantly lower than reference intervals, whereas total hydroperoxides and myeloperoxidase (a marker of inflammation) were significantly higher. Copper negatively correlated with total hydroperoxides (r = 0.95, p = 0.001). A similar, deeply modified OSS was already observed in COVID-19 patients hospitalized in an intensive care unit. TAC evaluated in saliva, urine, and skin correlated negatively with copper and with plasma total hydroperoxides. To conclude, the systemic OSS, determined using a large number of biomarkers, was always significantly increased in cured COVID-19 patients during their recovery phase. The less costly evaluation of TAC using an electrochemical method could potentially represent a good alternative to the individual analysis of biomarkers linked to pro-oxidants.
Supplementary Materials: The following supporting information can be downloaded at: https: //www.mdpi.com/article/10.3390/biomedicines11051308/s1. Figure S1 : Individual plasma concentrations of antioxidants observed in COVID-19 patients as compared to CHU Liège reference intervals. LRV: lower reference value; URV: upper reference value.
Conflicts of Interest: The authors from academic institutions declare no conflict of interest. IEA had no role in the design of the study, the interpretation of data, or the decision to publish the results in Biomedicines.
References
Bartolini, Stabile, Bastianelli, Giustarini, Pierucci et al., SARS-2-CoV2 infection impairs the metabolism and redox function of cellular glutathione, Redox Biol
Bartosz, Non-enzymatic capacity assays: Limitations of use in medicine, Free Radic. Res, doi:10.3109/10715761003758114
Berr, Balansard, Arnaud, Roussel, Alpérovitch, Cognitive decline is associated with systemic oxidative stress: The EVA Study, J. Am. Geriatr. Soc, doi:10.1111/j.1532-5415.2000.tb02603.x
Bomer, Beverborg, Hoes, Streng, Vermeer et al., Selenium and outcome in heart failure, Eur. J. Heart Fail, doi:10.1002/ejhf.1644
Brainina, Gerasimova, Varzakova, Kazakov, Galperin, Noninvasive method of determining skin antioxidant/oxidant activity: Clinical and cosmetics applications, Anal. Bioanal. Electrochem
Butterworth, Baum, Porter, A modification of the Ellman procedure for the estimation of protein sulfhydryl groups, Arch. Biochem. Biophys, doi:10.1016/0003-9861(67)90409-2
Carrion-Garcia, Guerra-Hernandez, Garcia-Villanova, Serafini, Sanchez et al., Plasma non-enzymatic antioxidant capacity (NEAC) in relation to dietary NEAC, nutrient antioxidants and inflammation, doi:10.3390/antiox9040301
Cavezzi, Troiani, Corrao, COVID-19: Hemoglobin, iron, and hypoxia beyond inflammation. A narrative review, Clin. Pract, doi:10.4081/cp.2020.1271
Cecchini, Cecchini, SARS-CoV-2 infection pathogenesis is related to oxidative stress as a response to aggression, Med. Hypotheses, doi:10.1016/j.mehy.2020.110102
Cekerevac, Turnic, Draginic, Andjic, Zivkovic et al., Predicting severity and intrahospital mortality in COVID-19; the place and role of oxidative stress, Oxidative Med. Cell. Longev, doi:10.1155/2021/6615787
Checa, Aran, Reactive oxygen species: Drivers of physiological and pathological processes, J. Inflamm. Res, doi:10.2147/JIR.S275595
D'oria, Schipani, Leonardi, Natalicchio, Perrini et al., The role of oxidative stress in cardiac disease: From physiological response to injury factor, Oxid. Med. Cell. Longev, doi:10.1155/2020/5732956
Da Silva Marques, Da Mata, Silveira, Marques, Amaral et al., Hydrogen peroxide release kinetics into saliva from different whitening products: A double-blind, randomized clinical trial, Clin. Oral. Investig
Daenen, Andries, Mekahli, Van Schepdael, Jouret et al., Oxidative stress in chronic kidney disease, Pediatr. Nephrol, doi:10.1007/s00467-018-4005-4
Davies, Hawkins, The role of myeloperoxidase in biomolecule modification, chronic inflammation, and disease, Antioxid. Redox Signal, doi:10.1089/ars.2020.8030
Davies, Protein oxidation and peroxidation, Biochem. J, doi:10.1042/BJ20151227
Deth, Clarke, Ni, Trivedi, Clinical evaluation of glutathione concentrations after consumption of milk containing different subtypes of β-casein: Results from a randomized, cross-over clinical trial, Nutr. J, doi:10.1186/s12937-016-0201-x
Duthie, Duthie, Russell, Kyle, Macdiarmid et al., Effect of increasing fruit and vegetable intake by dietary intervention on nutritional biomarkers and attitudes to dietary change: A randomised trial, Eur. J. Nutr, doi:10.1007/s00394-017-1469-0
Ehrenwald, Chislom, Fox, Intact ceruloplasmin oxidatively modifies low density lipoprotein, J. Clin. Investig, doi:10.1172/JCI117127
Evan, Omaye, Use of saliva biomarkers to monitor efficacy of vitamin C in exercise-induced oxidative stress, Antioxidants, doi:10.3390/antiox6010005
Fernandes, De Brito, Silva Dos Reis, Sato, Pereir, SARS-CoV-2 and other respiratory viruses: What does oxidative stress have to do with it?, Oxid. Med. Cell. Longev, doi:10.1155/2020/8844280
Gaetke, Chow, Copper toxicity, oxidative stress and antioxidant nutrients, Toxicology, doi:10.1016/S0300-483X(03)00159-8
Gall, Lemeshow, Saulnier, A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study, JAMA, doi:10.1001/jama.1993.03510240069035
Ganini, Canistro, Jang, Sadler, Mason et al., Ceruloplasmin (ferroxidase) oxidized hydroxylamine probes: Deceptive implications for free radical detection. Free Radic, Biol. Med, doi:10.1016/j.freeradbiomed.2012.07.013
Geng, Wei, Qian, Huay, Lodato et al., Pathophysiological characteristics and therapeutic approaches for pulmonary injury and cardiovascular complications of coronavirus disease, Cardiovasc. Pathol
Gey, Optimum plasma levels of antioxidant micronutrients-Ten years of antioxidant hypothesis on atherosclerosis, New Asp. Nutr. Status
Gianazza, Brioschi, Fernandez, Casalnuovo, Altomare et al., Lipid Peroxidation in Atherosclerotic Cardiovascular Diseases, Antioxid. Redox Signal, doi:10.1089/ars.2019.7955
Guerrero, Acosta, Inflammatory and oxidative stress in rotavirus infection, World J. Virol, doi:10.5501/wjv.v5.i2.38
Guo, Chen, Yeh, Der-Yun, Wang, Cu/Zn Ratios are associated with nutritional status, oxidative stress, inflammation and Immune abnormalities in patients on peritoneal dialysis, Clin. Biochem, doi:10.1016/j.clinbiochem.2010.12.017
Guo, Wang, Effects of zinc supplementation on plasma Copper/Zinc ratios, oxidative stress, and immunological status in hemodialysis patients, Int. J. Med. Sci, doi:10.7150/ijms.5291
Hajam, Rani, Ganie, Sheikh, Javaid et al., None, Oxidative Stress in Human Pathology and Aging: Molecular Mechanisms and Perspectives. Cells, doi:10.3390/cells11030552
Holford, Carr, Zawari, Vizcaychipi, Vitamin C intervention for critical COVID-A pragmatic review of the current level of evidence, Life, doi:10.3390/life11111166
Holmes, O'connor, Perry, Tracey, Wessely et al., Multidisciplinary research priorities for the COVID-19 pandemic: A call for mental health science, Lancet Psychiatry, doi:10.1016/S2215-0366(20)30168-1
Huang, Rose, Hoffmann, The role of selenium in inflammation and immunity: From molecular mechanisms to therapeutic opportunities, Antioxid. Redox Signal, doi:10.1089/ars.2011.4145
Ii'yasova, Scarbrough, Spasojevic, Urinary biomarkers of oxidative stress, Clin. Chim. Acta, doi:10.1016/j.cca.2012.06.012
Jarosz, Olbert, Wyszogrodzka, Młyniec, Librowski, Antioxidant and anti-inflammatory effects of zinc. Zincdependent NF-κB signaling, Inflammopharmacology, doi:10.1007/s10787-017-0309-4
Jiang, Natural forms of vitamin E: Metabolism, antioxidant and anti-inflammatory activities and the role in disease prevention 543 and therapy. Free Radic, Biol. Med, doi:10.1016/j.freeradbiomed.2014.03.035
Jones, Redefining oxidative stress, Antioxid. Redox Signal, doi:10.1089/ars.2006.8.1865
Joris, Minguet, Colson, Joris, Fadeur et al., Cardiopulmonary exercise testing in critically ill coronavirus disease 2019 survivors: Evidence of a sustained exercise intolerance and hypermetabolism, Crit. Care Explor, doi:10.1097/CCE.0000000000000491
Kaci, Belhaffef, Meziane, Dostert, Menu et al., Arab-Tehranv, E. Nanoemulsions and topical creams for the safe and effective delivery of lipophilic antioxidant coenzyme Q10, J. Food Process Technol, doi:10.1016/j.colsurfb.2018.04.010
Karkhanei, Ghane, Mehri, Evaluation of oxidative stress level: Total antioxidant capacity, total oxidant status and glutathione activity in patients with COVID-19. New Microbes New Infect, doi:10.1016/j.nmni.2021.100897
Kumar, Singh, Maniar, Chawdhary, Bhattacharyya et al., Plasma hydrogen peroxide: A myth or reality?, Int. J. Clin. Biochem, doi:10.1007/s12291-018-0746-x
Lafaurie, Zaror, Díaz-Báez, Castillo, De Ávila et al., Evaluation of substantivity of hypochlorous acid as an antiplaque agent: A randomized controlled trial, Int. J. Dent. Hyg, doi:10.1111/idh.12342
Levine, Eck, Vitamin, Working on the x-axis1,2. Am, J. Clin. Nutr, doi:10.3945/ajcn.2009.28687
Lindblad, Tveden-Nyborg, Lykkesfeldt, Regulation of vitamin C homeostasis during deficiency, Nutrients, doi:10.3390/nu5082860
Lindstrom, Murray, Schaum's Easy Outline of Statistics
Macieczyk, Zalewska, Ladny, Salivary antioxidant barrier, redox status, and oxidative damage to proteins and lipids in healthy children, adults, and the elderly, Oxid. Med. Cell. Longev, doi:10.1155/2019/4393460
Maciejczyk, Szulimowska, Taranta-Janusz, Werbel, Wasileewska et al., Salivary FRAP as a marker of chronic kidney disease progression in children, Antioxidants, doi:10.3390/antiox8090409
Martín-Fernandez, Aller, Heredia-Rodríguez, Gomez-Sanchez, Martínez-Paz et al., Lipid peroxidation as a hallmark of severity in COVID-19 patients, Redox Biol, doi:10.1016/j.redox.2021.102181
Mckay, Lyner, Linden, Kee, Moitry et al., Association of low plasma antioxidant levels with all-cause mortality and coronary events in healthy middle-aged men from France and Northern Ireland in the PRIME study, Eur. J. Nutr, doi:10.1007/s00394-020-02455-2
Mezzetti, Pierdomenico, Costantini, Romano, De Cesare et al., Copper/zinc ratio and systemic oxidant load: Effect of aging and aging-related degenerative diseases. Free Radic, Biol. Med, doi:10.1016/S0891-5849(98)00109-9
Milleriii, Appel, Risby, Effect of dietary patterns on measures of lipid peroxidation. Results from a randomized Clinical trial, Circulation, doi:10.1161/01.CIR.98.22.2390
Moghaddam, Heller, Sun, Seelig, Cherkezov et al., Selenium deficiency is associated with mortality risk from COVID-19, Nutrients, doi:10.3390/nu12072098
Moore, Roberts, Measurement of lipid peroxidation, Free Radic. Res, doi:10.3109/10715769809065821
Morris, Khurasany, Nguyen, Kim, Guilford et al., Glutathione and infection, doi:10.1016/j.bbagen.2012.10.012
Muhammad, Kani, Iliya, Muhammad, Binji et al., Deficiency of antioxidants and increased oxidative stress in COVID-19 patients: A cross-sectional comparative study in Jigawa, Northwestern Nigeria, SAGE Open Med, doi:10.1177/2050312121991246
Mukaka, A guide to appropriate use of correlation coefficient in medical research, Malawi Med. J
Munteanu, Apetre, Analytical methods U-used in D-determining antioxidant activity: A review, Int. J. Mol. Sci, doi:10.3390/ijms22073380
Nitti, Marengo, Furfaro, Pronzato, Marinari et al., Hormesis and oxidative distress: Pathophysiology of reactive oxygen species and the open question of antioxidant modulation and supplementation, Antioxidants, doi:10.3390/antiox11081613
Omaye, Tumbull, Sauerlich, Selected methods for the determination of ascorbic acid in animal cells, tissues and fluids, Methods Enzym
Otifi, Adiga, Endothelial dysfunction in COVID-19 infection, Am. J. Med. Sci, doi:10.1016/j.amjms.2021.12.010
Ozgünes, Gürer, Tuner, Correlation between plasma malondialdehyde and ceruloplasmin activity values in rheumatoid arthritis, Clin. Biochem, doi:10.1016/0009-9120(94)00081-6
Ozturk, Kurutos, Ataseven, Copper/zinc and copper/selenium ratios, and oxidative stress as biochemical markers in recurrent aphthous stomatitis, J. Trace Elem. Med. Biol, doi:10.1016/j.jtemb.2013.04.002
Park, Kim, Lee, Impact of oxidative stress on lung diseases, Respirology, doi:10.1111/j.1440-1843.2008.01447.x
Peluso, Raguzzini, Salivary and urinary total antioxidant capacity as biomarkers of oxidative stress in humans, Pathol. Res. Int, doi:10.1155/2016/5480267
Pincemail, Cavalier, Charlier, Cheramy-Bien, Brevers et al., Oxidative stress status in COVID-19 patients hospitalized in intensive care unit for severe pneumonia. A pilot study, Antioxidants, doi:10.3390/antiox10020257
Pincemail, Cillard, Nève, Defraigne, Mesure de la capacité antioxydante globale du plasma: Une revue critique, Ann. Biol. Clin
Pincemail, Defraigne, Cheramy-Bien, Dardenne, Donneau et al., On the potential increase of the oxidative stress status in patients with abdominal aortic aneurysm, Redox Rep, doi:10.1179/1351000212Y.0000000012
Pincemail, Kaci, Cheramy-Bien, Defraigne, Electrochemical methodology for evaluating skin oxidative stress status (OSS). Diseases, doi:10.3390/diseases7020040
Pincemail, Kaci, Kevers, Tabart, Elle et al., An easy electrochemical method for evaluating antioxidant capacity of wines, Diseases, doi:10.3390/diseases7010010
Pincemail, Le Goff, Charlier, Gillion, Cheramy-Bien et al., Evaluation biologique du stress oxydant. Application en routine clinique, Nutr. Et Endocrinol
Pincemail, Vanbelle, Gaspard, Collette, Haleng et al., Effect of different contraceptive methods on the oxidative stress status in women aged 40-48 years from the ELAN study in the province of Liège, Hum. Reprod, doi:10.1093/humrep/dem146
Polizzi, Torrisi, Santonocito, Di Stefano, Indelicato et al., Influence of myeloperoxidase levels on periodontal disease: An applied clinical study, App. Sci, doi:10.3390/app10031037
Poljšak, Dahmane, Free radicals and extrinsic skin aging, Dermatol. Res. Pract, doi:10.1155/2012/135206
Poljšak, Dahmane, Godic, Intrinsic skin aging: The role of oxidative stress, Acta Derm. Alp. Pannonica Adriat
Prasad, Tyagi, Aggarwal, Detection of inflammatory biomarkers in saliva and urine: Potential in diagnosis, prevention, and treatment for chronic diseases, Exp. Biol. Med, doi:10.1177/1535370216638770
Ran, Zhao, Tan, Wang, Mizuno et al., Association between serum vitamin C and the blood pressure: A systematic review and meta-analysis of observational studies, Cardiovasc. Ther, doi:10.1155/2020/4940673
Rousseau, Minguet, Colson, Kellens, Chaabane et al., Post-intensive care syndrome after a critical COVID-19: Cohort study from a Belgian follow-up clinic, Ann. Intensive Care. 2021, doi:10.1186/s13613-021-00910-9
Saldeen, Saldeen, Importance of tocopherols beyond α-tocopherol: Evidence from animal and human studies, Nutr. Res, doi:10.1016/j.nutres.2005.09.019
Savic-Radojevic, Pljesa-Ercegovac, Matic, Simic, Radovanovic et al., Chapter Four-Novel Biomarkers of Heart Failure, Adv. Clin. Chem
Shi, Puto, N-Acetylcysteine to combat COVID-19: An evidence review, Ther. Clin. Risk Manag
Siegel, Nonparametric Statistics for the Behavioral Sciences
Sies, Oxidative stress: Introductory remarks
Sinclair, Taylor, Lunec, Girling, Barnett, Low plasma ascorbate levels in patients with type 2 diabetes mellitus consuming adequate dietary vitamin C, Diabet. Med, doi:10.1111/j.1464-5491.1994.tb00375.x
Steinbrenner, Duntas, Rayman, The role of selenium in type-2 diabetes mellitus and its metabolic comorbidities, Redox Biol, doi:10.1016/j.redox.2022.102236
Steven, Frenis, Oelze, Kalinovic, Kuntic et al., Vascular inflammation and oxidative stress: Major triggers for cardiovascular disease, Oxid. Med. Cell. Longev, doi:10.1155/2019/7092151
Sturup, Hayes, Peters, Development and application of a simple routine for the determination of selenium in serum by octopole reaction with ICPMS, Anal. Bioanal. Chem, doi:10.1007/s00216-004-2946-x
Thompson, Cooney, The potential physiological role of γ-tocopherol in human health: A qualitative review, Nutr. Cancer, doi:10.1080/01635581.2019.1653472
Trouba, Hamadeh, Amin, Germolec, Oxidative stress and its role in skin disease, Redox Signal, doi:10.1089/15230860260220175
Tsimikas, Brilakis, Lennon, Miller, Witztum et al., Relationship of IgG and IgM autoantibodies to oxidized low density lipoprotein with coronary artery disease and cardiovascular events, J. Lipid Res, doi:10.1194/jlr.M600361-JLR200
Turki, Hayot, Carnac, Pillard, Passerieux et al., Functional muscle impairment in facioscapulohumeral muscular dystrophy is correlated with oxidative stress and mitochondrial dysfunction. Free Radic, Biol. Med, doi:10.1016/j.freeradbiomed.2012.06.041
Virella, Carter, Saad, Crosswell, Game et al., Distribution of IgM and IgG antibodies to oxidized LDL in immune complexes isolated from patients with type 1 diabetes and its relationship with nephropathy. Distribution of IgM and IgG antibodies to oxidized LDL in immune complexes isolated from patients with type 1 diabetes and its relationship with nephropathy, Clin. Immunol
Vlasova, Sokolov, Kostevich, Mikhalchik, Vasilyev, Myeloperoxidase-induced oxidation of albumin and ceruloplasmin: Role of Tyrosines, Biochemistry, doi:10.1134/S0006297919060087
Wayner, Burton, Ingold, Barclay, Locke, The relative contributions of vitamin E, urate, ascorbate and proteins to the total peroxyl radical-trapping antioxidant capacity of human blood plasma, BBA
Xie, Xu, Bowe, Al-Aly, Long-term cardiovascular outcomes of COVID-19, Nat. Med, doi:10.1038/s41591-022-01689-3
Zhang, Penninger, Li, Zhong, Slutsky, Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: Molecular mechanisms and potential therapeutic target, Intensive Care Med, doi:10.1007/s00134-020-05985-9
Zhao, Tham, Lu, Lai, Lee et al., Simultaneous determination of vitamins C, E and carotene in human plasma by high-performance liquid chromatography with photodiode-array detection, J. Pharm. Pharm. Sci
Zuo, Prather, Stetskiv, Garrison, Meade et al., Inflammaging and oxidative stress in human diseases: From molecular mechanisms to novel treatments, Int. J. Mol. Sci, doi:10.3390/ijms20184472
DOI record:
{
"DOI": "10.3390/biomedicines11051308",
"ISSN": [
"2227-9059"
],
"URL": "http://dx.doi.org/10.3390/biomedicines11051308",
"abstract": "<jats:p>Background: Oxidative stress (OS) could cause various COVID-19 complications. Recently, we have developed the Pouvoir AntiOxydant Total (PAOT®) technology for reflecting the total antioxidant capacity (TAC) of biological samples. We aimed to investigate systemic oxidative stress status (OSS) and to evaluate the utility of PAOT® for assessing TAC during the recovery phase in critical COVID-19 patients in a rehabilitation facility. Materials and Methods: In a total of 12 critical COVID-19 patients in rehabilitation, 19 plasma OSS biomarkers were measured: antioxidants, TAC, trace elements, oxidative damage to lipids, and inflammatory biomarkers. TAC level was measured in plasma, saliva, skin, and urine, using PAOT and expressed as PAOT-Plasma, -Saliva, -Skin, and -Urine scores, respectively. Plasma OSS biomarker levels were compared with levels from previous studies on hospitalized COVID-19 patients and with the reference population. Correlations between four PAOT scores and plasma OSS biomarker levels were analyzed. Results: During the recovery phase, plasma levels in antioxidants (γ-tocopherol, β-carotene, total glutathione, vitamin C and thiol proteins) were significantly lower than reference intervals, whereas total hydroperoxides and myeloperoxidase (a marker of inflammation) were significantly higher. Copper negatively correlated with total hydroperoxides (r = 0.95, p = 0.001). A similar, deeply modified OSS was already observed in COVID-19 patients hospitalized in an intensive care unit. TAC evaluated in saliva, urine, and skin correlated negatively with copper and with plasma total hydroperoxides. To conclude, the systemic OSS, determined using a large number of biomarkers, was always significantly increased in cured COVID-19 patients during their recovery phase. The less costly evaluation of TAC using an electrochemical method could potentially represent a good alternative to the individual analysis of biomarkers linked to pro-oxidants.</jats:p>",
"alternative-id": [
"biomedicines11051308"
],
"author": [
{
"affiliation": [
{
"name": "Clinical Chemistry, University Hospital of Liège, Sart Tilman, 4000 Liège, Belgium"
}
],
"family": "Pincemail",
"given": "Joël",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-4157-6570",
"affiliation": [
{
"name": "Intensive Care Department, University Hospital of Liège, Sart Tilman, 4000 Liège, Belgium"
}
],
"authenticated-orcid": false,
"family": "Rousseau",
"given": "Anne-Françoise",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1939-3652",
"affiliation": [
{
"name": "Physical Medicine Rehabilitation and Sports Traumatology Department Sports, University Hospital of Liège, Sart Tilman, 4000 Liège, Belgium"
}
],
"authenticated-orcid": false,
"family": "Kaux",
"given": "Jean-François",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1846-1326",
"affiliation": [
{
"name": "Department of Cardiovascular Surgery, University Hospital of Liège, Sart Tilman, 4000 Liège, Belgium"
}
],
"authenticated-orcid": false,
"family": "Cheramy-Bien",
"given": "Jean-Paul",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Physical Medicine Rehabilitation and Sports Traumatology Department Sports, University Hospital of Liège, Sart Tilman, 4000 Liège, Belgium"
}
],
"family": "Bruyère",
"given": "Christine",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Physical Medicine Rehabilitation and Sports Traumatology Department Sports, University Hospital of Liège, Sart Tilman, 4000 Liège, Belgium"
}
],
"family": "Prick",
"given": "Jeanine",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Veterinary Medicine Faculty, FARAH, University of Liège, Sart Tilman, 4000 Liège, Belgium"
}
],
"family": "Stern",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Research Department, Institut Européen des Antioxydants (IEA), Oxystress Technologies PAOTScan, 54500 Vandœuvre-lès-Nancy, France"
}
],
"family": "Kaci",
"given": "Mouna-Messaouda",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Physical Medicine Rehabilitation and Sports Traumatology Department Sports, University Hospital of Liège, Sart Tilman, 4000 Liège, Belgium"
}
],
"family": "Maertens De Noordhout",
"given": "Benoît",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Biostatistics Department, University Hospital of Liège, Sart Tilman, 4000 Liège, Belgium"
}
],
"family": "Albert",
"given": "Adelin",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Physical Medicine Rehabilitation and Sports Traumatology Department Sports, University Hospital of Liège, Sart Tilman, 4000 Liège, Belgium"
}
],
"family": "Eubelen",
"given": "Céline",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Clinical Chemistry, University Hospital of Liège, Sart Tilman, 4000 Liège, Belgium"
}
],
"family": "Goff",
"given": "Caroline Le",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Intensive Care Department, University Hospital of Liège, Sart Tilman, 4000 Liège, Belgium"
}
],
"family": "Misset",
"given": "Benoît",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Clinical Chemistry, University Hospital of Liège, Sart Tilman, 4000 Liège, Belgium"
}
],
"family": "Cavalier",
"given": "Etienne",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Toxicology Department, University Hospital of Liège, Sart Tilman, 4000 Liège, Belgium"
}
],
"family": "Charlier",
"given": "Corinne",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Research Department, Institut Européen des Antioxydants (IEA), Oxystress Technologies PAOTScan, 54500 Vandœuvre-lès-Nancy, France"
}
],
"family": "Meziane",
"given": "Smail",
"sequence": "additional"
}
],
"container-title": "Biomedicines",
"container-title-short": "Biomedicines",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
4,
28
]
],
"date-time": "2023-04-28T09:46:06Z",
"timestamp": 1682675166000
},
"deposited": {
"date-parts": [
[
2023,
4,
28
]
],
"date-time": "2023-04-28T11:42:52Z",
"timestamp": 1682682172000
},
"funder": [
{
"name": "IEA"
}
],
"indexed": {
"date-parts": [
[
2023,
5,
17
]
],
"date-time": "2023-05-17T08:29:15Z",
"timestamp": 1684312155944
},
"is-referenced-by-count": 1,
"issue": "5",
"issued": {
"date-parts": [
[
2023,
4,
28
]
]
},
"journal-issue": {
"issue": "5",
"published-online": {
"date-parts": [
[
2023,
5
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
4,
28
]
],
"date-time": "2023-04-28T00:00:00Z",
"timestamp": 1682640000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2227-9059/11/5/1308/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1308",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
4,
28
]
]
},
"published-online": {
"date-parts": [
[
2023,
4,
28
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref_1",
"unstructured": "Sies, H. (1985). Oxidative Stress, Academic Press."
},
{
"DOI": "10.3390/cells11030552",
"doi-asserted-by": "crossref",
"key": "ref_2",
"unstructured": "Hajam, Y.A., Rani, R., Ganie, S.Y., Sheikh, T.A., Javaid, D., Qadri, S.S., Pramodh, S., Alsulimani, A., Alkhanani, M.F., and Harakeh, S. (2022). Oxidative Stress in Human Pathology and Aging: Molecular Mechanisms and Perspectives. Cells, 11."
},
{
"DOI": "10.2147/JIR.S275595",
"article-title": "Reactive oxygen species: Drivers of physiological and pathological processes",
"author": "Checa",
"doi-asserted-by": "crossref",
"first-page": "1057",
"journal-title": "J. Inflamm. Res.",
"key": "ref_3",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1089/ars.2006.8.1865",
"article-title": "Redefining oxidative stress",
"author": "Jones",
"doi-asserted-by": "crossref",
"first-page": "1865",
"journal-title": "Antioxid. Redox Signal.",
"key": "ref_4",
"volume": "8",
"year": "2006"
},
{
"DOI": "10.3390/antiox11081613",
"doi-asserted-by": "crossref",
"key": "ref_5",
"unstructured": "Nitti, M., Marengo, B., Furfaro, A.L., Pronzato, M.A., Marinari, U.M., Domenicotti, C., and Traverso, N. (2022). Hormesis and oxidative distress: Pathophysiology of reactive oxygen species and the open question of antioxidant modulation and supplementation. Antioxidants, 11."
},
{
"DOI": "10.1155/2019/7092151",
"article-title": "Vascular inflammation and oxidative stress: Major triggers for cardiovascular disease",
"author": "Steven",
"doi-asserted-by": "crossref",
"first-page": "7092151",
"journal-title": "Oxid. Med. Cell. Longev.",
"key": "ref_6",
"volume": "2019",
"year": "2019"
},
{
"DOI": "10.3390/ijms20184472",
"doi-asserted-by": "crossref",
"key": "ref_7",
"unstructured": "Zuo, L., Prather, E.R., Stetskiv, M., Garrison, D.E., Meade, J.R., Peace, T.I., and Zhou, T. (2019). Inflammaging and oxidative stress in human diseases: From molecular mechanisms to novel treatments. Int. J. Mol. Sci., 20."
},
{
"DOI": "10.5501/wjv.v5.i2.38",
"article-title": "Inflammatory and oxidative stress in rotavirus infection",
"author": "Guerrero",
"doi-asserted-by": "crossref",
"first-page": "38",
"journal-title": "World J. Virol.",
"key": "ref_8",
"volume": "5",
"year": "2016"
},
{
"DOI": "10.1007/s00134-020-05985-9",
"article-title": "Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: Molecular mechanisms and potential therapeutic target",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "586",
"journal-title": "Intensive Care Med.",
"key": "ref_9",
"volume": "46",
"year": "2020"
},
{
"article-title": "COVID-19: Hemoglobin, iron, and hypoxia beyond inflammation",
"author": "Cavezzi",
"first-page": "1271",
"journal-title": "A narrative review. Clin. Pract.",
"key": "ref_10",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1016/j.mehy.2020.110102",
"article-title": "SARS-CoV-2 infection pathogenesis is related to oxidative stress as a response to aggression",
"author": "Cecchini",
"doi-asserted-by": "crossref",
"first-page": "110102",
"journal-title": "Med. Hypotheses",
"key": "ref_11",
"volume": "143",
"year": "2020"
},
{
"DOI": "10.1016/j.amjms.2021.12.010",
"article-title": "Endothelial dysfunction in COVID-19 infection",
"author": "Otifi",
"doi-asserted-by": "crossref",
"first-page": "281",
"journal-title": "Am. J. Med. Sci.",
"key": "ref_12",
"volume": "363",
"year": "2022"
},
{
"DOI": "10.1155/2020/8844280",
"article-title": "SARS-CoV-2 and other respiratory viruses: What does oxidative stress have to do with it?",
"author": "Fernandes",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Oxid. Med. Cell. Longev.",
"key": "ref_13",
"volume": "2020",
"year": "2020"
},
{
"DOI": "10.1016/j.carpath.2020.107228",
"article-title": "Pathophysiological characteristics and therapeutic approaches for pulmonary injury and cardiovascular complications of coronavirus disease",
"author": "Geng",
"doi-asserted-by": "crossref",
"first-page": "107228",
"journal-title": "Cardiovasc. Pathol.",
"key": "ref_14",
"volume": "47",
"year": "2020"
},
{
"DOI": "10.1016/S2215-0366(20)30168-1",
"article-title": "Multidisciplinary research priorities for the COVID-19 pandemic: A call for mental health science",
"author": "Holmes",
"doi-asserted-by": "crossref",
"first-page": "547",
"journal-title": "Lancet Psychiatry",
"key": "ref_15",
"volume": "7",
"year": "2020"
},
{
"key": "ref_16",
"unstructured": "Haute Autorité de la Santé (HAS) Board (2020). Rapid Responses in the Context of COVID-19—Management of COVID+ Patients in Physical Medicine and Rehabilitation (MPR), and on Return Home, Haute Autorité de la Santé (HAS)."
},
{
"DOI": "10.1186/s13613-021-00910-9",
"article-title": "Post-intensive care syndrome after a critical COVID-19: Cohort study from a Belgian follow-up clinic",
"author": "Rousseau",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Ann. Intensive Care.",
"key": "ref_17",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1097/CCE.0000000000000491",
"article-title": "Cardiopulmonary exercise testing in critically ill coronavirus disease 2019 survivors: Evidence of a sustained exercise intolerance and hypermetabolism",
"author": "Joris",
"doi-asserted-by": "crossref",
"first-page": "e0491",
"journal-title": "Crit. Care Explor.",
"key": "ref_18",
"volume": "3",
"year": "2021"
},
{
"DOI": "10.1111/j.1440-1843.2008.01447.x",
"article-title": "Impact of oxidative stress on lung diseases",
"author": "Park",
"doi-asserted-by": "crossref",
"first-page": "27",
"journal-title": "Respirology",
"key": "ref_19",
"volume": "14",
"year": "2009"
},
{
"article-title": "The role of oxidative stress in cardiac disease: From physiological response to injury factor",
"author": "Schipani",
"first-page": "5732956",
"journal-title": "Oxid. Med. Cell. Longev.",
"key": "ref_20",
"volume": "2020",
"year": "2020"
},
{
"DOI": "10.1007/s00467-018-4005-4",
"article-title": "Oxidative stress in chronic kidney disease",
"author": "Daenen",
"doi-asserted-by": "crossref",
"first-page": "975",
"journal-title": "Pediatr. Nephrol.",
"key": "ref_21",
"volume": "34",
"year": "2019"
},
{
"DOI": "10.1111/j.1532-5415.2000.tb02603.x",
"article-title": "Cognitive decline is associated with systemic oxidative stress: The EVA Study",
"author": "Berr",
"doi-asserted-by": "crossref",
"first-page": "1285",
"journal-title": "J. Am. Geriatr. Soc.",
"key": "ref_22",
"volume": "48",
"year": "2015"
},
{
"DOI": "10.3390/antiox10020257",
"doi-asserted-by": "crossref",
"key": "ref_23",
"unstructured": "Pincemail, J., Cavalier, E., Charlier, C., Cheramy-Bien, J.-P., Brevers, E., Courtois, A., Fadeur, M., Meziane, S., Le Goff, C., and Misset, B. (2021). Oxidative stress status in COVID-19 patients hospitalized in intensive care unit for severe pneumonia. A pilot study. Antioxidants, 10."
},
{
"DOI": "10.3390/life11111166",
"doi-asserted-by": "crossref",
"key": "ref_24",
"unstructured": "Holford, P., Carr, A.C., Zawari, M., and Vizcaychipi, M.P. (2021). Vitamin C intervention for critical COVID-A pragmatic review of the current level of evidence. Life, 11."
},
{
"DOI": "10.20944/preprints202007.0113.v1",
"doi-asserted-by": "crossref",
"key": "ref_25",
"unstructured": "Moghaddam, A., Heller, R.A., Sun, Q., Seelig, J., Cherkezov, A., Seibert, L., Hackler, J., Seemann, P., Diegmann, J., and Pilz, M. (2020). Selenium deficiency is associated with mortality risk from COVID-19. Nutrients, 12."
},
{
"DOI": "10.1016/j.redox.2021.102181",
"article-title": "Lipid peroxidation as a hallmark of severity in COVID-19 patients",
"author": "Aller",
"doi-asserted-by": "crossref",
"first-page": "102181",
"journal-title": "Redox Biol.",
"key": "ref_26",
"volume": "48",
"year": "2021"
},
{
"DOI": "10.3390/ijms22073380",
"doi-asserted-by": "crossref",
"key": "ref_27",
"unstructured": "Munteanu, I.G., and Apetre, C. (2021). Analytical methods U-used in D-determining antioxidant activity: A review. Int. J. Mol. Sci., 22."
},
{
"DOI": "10.3390/antiox9040301",
"doi-asserted-by": "crossref",
"key": "ref_28",
"unstructured": "Carrion-Garcia, C.J., Guerra-Hernandez, E.J., Garcia-Villanova, B., Serafini, M., Sanchez, M.-J., Amiano, P., and Molina-Montes, E. (2020). Plasma non-enzymatic antioxidant capacity (NEAC) in relation to dietary NEAC, nutrient antioxidants and inflammation-related biomarkers. Antioxidants, 9."
},
{
"DOI": "10.3109/10715761003758114",
"article-title": "Non-enzymatic capacity assays: Limitations of use in medicine",
"author": "Bartosz",
"doi-asserted-by": "crossref",
"first-page": "711",
"journal-title": "Free Radic. Res.",
"key": "ref_29",
"volume": "44",
"year": "2010"
},
{
"article-title": "Mesure de la capacité antioxydante globale du plasma: Une revue critique",
"author": "Pincemail",
"first-page": "413",
"journal-title": "Ann. Biol. Clin.",
"key": "ref_30",
"volume": "72",
"year": "2014"
},
{
"DOI": "10.1001/jama.1993.03510240069035",
"article-title": "A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study",
"author": "Lemeshow",
"doi-asserted-by": "crossref",
"first-page": "2957",
"journal-title": "JAMA",
"key": "ref_31",
"volume": "270",
"year": "1993"
},
{
"DOI": "10.1016/0076-6879(79)62181-X",
"article-title": "Selected methods for the determination of ascorbic acid in animal cells, tissues and fluids",
"author": "Omaye",
"doi-asserted-by": "crossref",
"first-page": "3",
"journal-title": "Methods Enzym.",
"key": "ref_32",
"volume": "62",
"year": "1979"
},
{
"article-title": "Simultaneous determination of vitamins C, E and carotene in human plasma by high-performance liquid chromatography with photodiode-array detection",
"author": "Zhao",
"first-page": "200",
"journal-title": "J. Pharm. Pharm. Sci.",
"key": "ref_33",
"volume": "7",
"year": "2004"
},
{
"DOI": "10.1159/000423787",
"article-title": "Optimum plasma levels of antioxidant micronutrients—Ten years of antioxidant hypothesis on atherosclerosis",
"author": "Gey",
"doi-asserted-by": "crossref",
"first-page": "84",
"journal-title": "New Asp. Nutr. Status",
"key": "ref_34",
"volume": "51",
"year": "1994"
},
{
"DOI": "10.1016/0003-9861(67)90409-2",
"article-title": "A modification of the Ellman procedure for the estimation of protein sulfhydryl groups",
"author": "Butterworth",
"doi-asserted-by": "crossref",
"first-page": "716",
"journal-title": "Arch. Biochem. Biophys.",
"key": "ref_35",
"volume": "118",
"year": "1967"
},
{
"DOI": "10.1007/s00216-004-2946-x",
"article-title": "Development and application of a simple routine for the determination of selenium in serum by octopole reaction with ICPMS",
"author": "Sturup",
"doi-asserted-by": "crossref",
"first-page": "686",
"journal-title": "Anal. Bioanal. Chem.",
"key": "ref_36",
"volume": "381",
"year": "2005"
},
{
"key": "ref_37",
"unstructured": "Clinical and Laboratory Standards Institut (2010). Defining, Stabling and Verifying Reference Intervals in the Clinical Laboratory, Clinical and Laboratory Standards Institut. Approved Guideline, 3rd ed.; EP-28-A3c, 28, n°30."
},
{
"article-title": "Evaluation biologique du stress oxydant. Application en routine clinique",
"author": "Pincemail",
"first-page": "16",
"journal-title": "Nutr. Et Endocrinol.",
"key": "ref_38",
"volume": "Édition Spéciale",
"year": "2010"
},
{
"DOI": "10.1179/1351000212Y.0000000012",
"article-title": "On the potential increase of the oxidative stress status in patients with abdominal aortic aneurysm",
"author": "Pincemail",
"doi-asserted-by": "crossref",
"first-page": "139",
"journal-title": "Redox Rep.",
"key": "ref_39",
"volume": "17",
"year": "2012"
},
{
"DOI": "10.1016/j.freeradbiomed.2012.06.041",
"article-title": "Functional muscle impairment in facioscapulohumeral muscular dystrophy is correlated with oxidative stress and mitochondrial dysfunction",
"author": "Turki",
"doi-asserted-by": "crossref",
"first-page": "1068",
"journal-title": "Free Radic. Biol. Med.",
"key": "ref_40",
"volume": "53",
"year": "2012"
},
{
"DOI": "10.3390/diseases7010010",
"doi-asserted-by": "crossref",
"key": "ref_41",
"unstructured": "Pincemail, J., Kaci, M.-M., Kevers, C., Tabart, J., Elle, R.E., and Meziane, S. (2019). PAOT-Liquid® Technology: An easy electrochemical method for evaluating antioxidant capacity of wines. Diseases, 7."
},
{
"article-title": "Nanoemulsions and topical creams for the safe and effective delivery of lipophilic antioxidant coenzyme Q10",
"author": "Kaci",
"first-page": "12",
"journal-title": "J. Food Process Technol.",
"key": "ref_42",
"volume": "7",
"year": "2016"
},
{
"key": "ref_43",
"unstructured": "Pincemail, J., Kaci, M.-M., Cheramy-Bien, J.-P., and Defraigne, J.-O. (2019). Electrochemical methodology for evaluating skin oxidative stress status (OSS). Diseases, 7."
},
{
"key": "ref_44",
"unstructured": "Siegel, S. (1956). Nonparametric Statistics for the Behavioral Sciences, McGraw-Hill."
},
{
"key": "ref_45",
"unstructured": "Lindstrom, D.P., and Murray, R.P. (2010). Schaum’s Easy Outline of Statistics, McGraw-Hill Education. [2nd ed.]."
},
{
"article-title": "A guide to appropriate use of correlation coefficient in medical research",
"author": "Mukaka",
"first-page": "69",
"journal-title": "Malawi Med. J.",
"key": "ref_46",
"volume": "24",
"year": "2012"
},
{
"DOI": "10.1016/j.nmni.2021.100897",
"article-title": "Evaluation of oxidative stress level: Total antioxidant capacity, total oxidant status and glutathione activity in patients with COVID-19",
"author": "Karkhanei",
"doi-asserted-by": "crossref",
"first-page": "100897",
"journal-title": "New Microbes New Infect.",
"key": "ref_47",
"volume": "42",
"year": "2021"
},
{
"DOI": "10.1177/2050312121991246",
"article-title": "Deficiency of antioxidants and increased oxidative stress in COVID-19 patients: A cross-sectional comparative study in Jigawa, Northwestern Nigeria",
"author": "Muhammad",
"doi-asserted-by": "crossref",
"first-page": "2050312121991246",
"journal-title": "SAGE Open Med.",
"key": "ref_48",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.redox.2021.102041",
"article-title": "SARS-2-CoV2 infection impairs the metabolism and redox function of cellular glutathione",
"author": "Bartolini",
"doi-asserted-by": "crossref",
"first-page": "102041",
"journal-title": "Redox Biol.",
"key": "ref_49",
"volume": "45",
"year": "2021"
},
{
"DOI": "10.1155/2021/6615787",
"article-title": "Predicting severity and intrahospital mortality in COVID-19; the place and role of oxidative stress",
"author": "Cekerevac",
"doi-asserted-by": "crossref",
"first-page": "6615787",
"journal-title": "Oxidative Med. Cell. Longev.",
"key": "ref_50",
"volume": "2021",
"year": "2021"
},
{
"DOI": "10.1016/j.bbagen.2012.10.012",
"article-title": "Glutathione and infection",
"author": "Morris",
"doi-asserted-by": "crossref",
"first-page": "3329",
"journal-title": "Biochem. Biophys. Acta",
"key": "ref_51",
"volume": "1830",
"year": "2013"
},
{
"article-title": "The relative contributions of vitamin E, urate, ascorbate and proteins to the total peroxyl radical-trapping antioxidant capacity of human blood plasma",
"author": "Wayner",
"first-page": "408",
"journal-title": "BBA",
"key": "ref_52",
"volume": "924",
"year": "1987"
},
{
"article-title": "Myeloperoxidase-induced oxidation of albumin and ceruloplasmin: Role of Tyrosines",
"author": "Vlasova",
"first-page": "652",
"journal-title": "Biochemistry",
"key": "ref_53",
"volume": "84",
"year": "2019"
},
{
"DOI": "10.1080/01635581.2019.1653472",
"article-title": "The potential physiological role of γ-tocopherol in human health: A qualitative review",
"author": "Thompson",
"doi-asserted-by": "crossref",
"first-page": "808",
"journal-title": "Nutr. Cancer",
"key": "ref_54",
"volume": "72",
"year": "2020"
},
{
"DOI": "10.3390/nu5082860",
"article-title": "Regulation of vitamin C homeostasis during deficiency",
"author": "Lindblad",
"doi-asserted-by": "crossref",
"first-page": "2860",
"journal-title": "Nutrients",
"key": "ref_55",
"volume": "5",
"year": "2013"
},
{
"DOI": "10.1007/s00394-020-02455-2",
"article-title": "Association of low plasma antioxidant levels with all-cause mortality and coronary events in healthy middle-aged men from France and Northern Ireland in the PRIME study",
"author": "McKay",
"doi-asserted-by": "crossref",
"first-page": "2631",
"journal-title": "Eur. J. Nutr.",
"key": "ref_56",
"volume": "60",
"year": "2021"
},
{
"DOI": "10.1007/s00394-017-1469-0",
"article-title": "Effect of increasing fruit and vegetable intake by dietary intervention on nutritional biomarkers and attitudes to dietary change: A randomised trial",
"author": "Duthie",
"doi-asserted-by": "crossref",
"first-page": "1855",
"journal-title": "Eur. J. Nutr.",
"key": "ref_57",
"volume": "57",
"year": "2018"
},
{
"DOI": "10.3945/ajcn.2009.28687",
"article-title": "Working on the x-axis1,2",
"author": "Levine",
"doi-asserted-by": "crossref",
"first-page": "1121",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref_58",
"volume": "90",
"year": "2009"
},
{
"DOI": "10.1016/j.nutres.2005.09.019",
"article-title": "Importance of tocopherols beyond α-tocopherol: Evidence from animal and human studies",
"author": "Saldeen",
"doi-asserted-by": "crossref",
"first-page": "877",
"journal-title": "Nutr. Res.",
"key": "ref_59",
"volume": "25",
"year": "2005"
},
{
"DOI": "10.1016/j.freeradbiomed.2014.03.035",
"article-title": "Natural forms of vitamin E: Metabolism, antioxidant and anti-inflammatory activities and the role in disease prevention 543 and therapy",
"author": "Jiang",
"doi-asserted-by": "crossref",
"first-page": "76",
"journal-title": "Free Radic. Biol. Med.",
"key": "ref_60",
"volume": "72",
"year": "2014"
},
{
"article-title": "Clinical evaluation of glutathione concentrations after consumption of milk containing different subtypes of β-casein: Results from a randomized, cross-over clinical trial",
"author": "Deth",
"first-page": "1",
"journal-title": "Nutr. J.",
"key": "ref_61",
"volume": "15",
"year": "2016"
},
{
"DOI": "10.2147/TCRM.S273700",
"article-title": "N-Acetylcysteine to combat COVID-19: An evidence review",
"author": "Shi",
"doi-asserted-by": "crossref",
"first-page": "1047",
"journal-title": "Ther. Clin. Risk Manag.",
"key": "ref_62",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.1089/ars.2011.4145",
"article-title": "The role of selenium in inflammation and immunity: From molecular mechanisms to therapeutic opportunities",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "705",
"journal-title": "Antioxid. Redox Signal.",
"key": "ref_63",
"volume": "16",
"year": "2012"
},
{
"DOI": "10.1002/ejhf.1644",
"article-title": "Selenium and outcome in heart failure",
"author": "Bomer",
"doi-asserted-by": "crossref",
"first-page": "1415",
"journal-title": "Eur. J. Heart Fail.",
"key": "ref_64",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1016/j.redox.2022.102236",
"article-title": "The role of selenium in type-2 diabetes mellitus and its metabolic comorbidities",
"author": "Steinbrenner",
"doi-asserted-by": "crossref",
"first-page": "102236",
"journal-title": "Redox Biol.",
"key": "ref_65",
"volume": "50",
"year": "2022"
},
{
"DOI": "10.1016/S0300-483X(03)00159-8",
"article-title": "Copper toxicity, oxidative stress and antioxidant nutrients",
"author": "Gaetke",
"doi-asserted-by": "crossref",
"first-page": "147",
"journal-title": "Toxicology",
"key": "ref_66",
"volume": "189",
"year": "2003"
},
{
"DOI": "10.1007/s10787-017-0309-4",
"article-title": "Antioxidant and anti-inflammatory effects of zinc. Zinc-dependent NF-κB signaling",
"author": "Jarosz",
"doi-asserted-by": "crossref",
"first-page": "11",
"journal-title": "Inflammopharmacology",
"key": "ref_67",
"volume": "25",
"year": "2017"
},
{
"DOI": "10.1016/S0891-5849(98)00109-9",
"article-title": "Copper/zinc ratio and systemic oxidant load: Effect of aging and aging-related degenerative diseases",
"author": "Mezzetti",
"doi-asserted-by": "crossref",
"first-page": "676",
"journal-title": "Free Radic. Biol. Med.",
"key": "ref_68",
"volume": "25",
"year": "1998"
},
{
"DOI": "10.1016/j.clinbiochem.2010.12.017",
"article-title": "Cu/Zn Ratios are associated with nutritional status, oxidative stress, inflammation and Immune abnormalities in patients on peritoneal dialysis",
"author": "Guo",
"doi-asserted-by": "crossref",
"first-page": "275",
"journal-title": "Clin. Biochem.",
"key": "ref_69",
"volume": "44",
"year": "2011"
},
{
"DOI": "10.1016/j.jtemb.2013.04.002",
"article-title": "Copper/zinc and copper/selenium ratios, and oxidative stress as biochemical markers in recurrent aphthous stomatitis",
"author": "Ozturk",
"doi-asserted-by": "crossref",
"first-page": "312",
"journal-title": "J. Trace Elem. Med. Biol.",
"key": "ref_70",
"volume": "27",
"year": "2013"
},
{
"DOI": "10.7150/ijms.5291",
"article-title": "Effects of zinc supplementation on plasma Copper/Zinc ratios, oxidative stress, and immunological status in hemodialysis patients",
"author": "Guo",
"doi-asserted-by": "crossref",
"first-page": "79",
"journal-title": "Int. J. Med. Sci.",
"key": "ref_71",
"volume": "10",
"year": "2013"
},
{
"DOI": "10.1042/BJ20151227",
"article-title": "Protein oxidation and peroxidation",
"author": "Davies",
"doi-asserted-by": "crossref",
"first-page": "805",
"journal-title": "Biochem. J.",
"key": "ref_72",
"volume": "473",
"year": "2016"
},
{
"DOI": "10.3109/10715769809065821",
"article-title": "Measurement of lipid peroxidation",
"author": "Moore",
"doi-asserted-by": "crossref",
"first-page": "659",
"journal-title": "Free Radic. Res.",
"key": "ref_73",
"volume": "28",
"year": "1998"
},
{
"DOI": "10.1007/s12291-018-0746-x",
"article-title": "Plasma hydrogen peroxide: A myth or reality?",
"author": "Kumar",
"doi-asserted-by": "crossref",
"first-page": "118",
"journal-title": "Int. J. Clin. Biochem.",
"key": "ref_74",
"volume": "34",
"year": "2019"
},
{
"DOI": "10.1016/j.freeradbiomed.2012.07.013",
"article-title": "Ceruloplasmin (ferroxidase) oxidized hydroxylamine probes: Deceptive implications for free radical detection",
"author": "Ganini",
"doi-asserted-by": "crossref",
"first-page": "1514",
"journal-title": "Free Radic. Biol. Med.",
"key": "ref_75",
"volume": "53",
"year": "2012"
},
{
"DOI": "10.1016/bs.acc.2016.09.002",
"article-title": "Chapter Four—Novel Biomarkers of Heart Failure",
"author": "Matic",
"doi-asserted-by": "crossref",
"first-page": "93",
"journal-title": "Adv. Clin. Chem.",
"key": "ref_76",
"volume": "79",
"year": "2017"
},
{
"DOI": "10.1172/JCI117127",
"article-title": "Intact ceruloplasmin oxidatively modifies low density lipoprotein",
"author": "Ehrenwald",
"doi-asserted-by": "crossref",
"first-page": "1493",
"journal-title": "J. Clin. Investig.",
"key": "ref_77",
"volume": "93",
"year": "1994"
},
{
"DOI": "10.1016/0009-9120(94)00081-6",
"article-title": "Correlation between plasma malondialdehyde and ceruloplasmin activity values in rheumatoid arthritis",
"author": "Tuner",
"doi-asserted-by": "crossref",
"first-page": "193",
"journal-title": "Clin. Biochem.",
"key": "ref_78",
"volume": "28",
"year": "1995"
},
{
"DOI": "10.1089/ars.2019.7955",
"article-title": "Lipid Peroxidation in Atherosclerotic Cardiovascular Diseases",
"author": "Gianazza",
"doi-asserted-by": "crossref",
"first-page": "49",
"journal-title": "Antioxid. Redox Signal.",
"key": "ref_79",
"volume": "34",
"year": "2021"
},
{
"DOI": "10.1161/01.CIR.98.22.2390",
"article-title": "Effect of dietary patterns on measures of lipid peroxidation. Results from a randomized Clinical trial",
"author": "MillerIII",
"doi-asserted-by": "crossref",
"first-page": "2390",
"journal-title": "Circulation",
"key": "ref_80",
"volume": "98",
"year": "1998"
},
{
"DOI": "10.1016/j.clim.2008.02.005",
"article-title": "Distribution of IgM and IgG antibodies to oxidized LDL in immune complexes isolated from patients with type 1 diabetes and its relationship with nephropathy. Distribution of IgM and IgG antibodies to oxidized LDL in immune complexes isolated from patients with type 1 diabetes and its relationship with nephropathy",
"author": "Virella",
"doi-asserted-by": "crossref",
"first-page": "394",
"journal-title": "Clin. Immunol.",
"key": "ref_81",
"volume": "127",
"year": "2008"
},
{
"DOI": "10.1194/jlr.M600361-JLR200",
"article-title": "Relationship of IgG and IgM autoantibodies to oxidized low density lipoprotein with coronary artery disease and cardiovascular events",
"author": "Tsimikas",
"doi-asserted-by": "crossref",
"first-page": "425",
"journal-title": "J. Lipid Res.",
"key": "ref_82",
"volume": "48",
"year": "2007"
},
{
"DOI": "10.1038/s41591-022-01689-3",
"article-title": "Long-term cardiovascular outcomes of COVID-19",
"author": "Xie",
"doi-asserted-by": "crossref",
"first-page": "583",
"journal-title": "Nat. Med.",
"key": "ref_83",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1089/ars.2020.8030",
"article-title": "The role of myeloperoxidase in biomolecule modification, chronic inflammation, and disease",
"author": "Davies",
"doi-asserted-by": "crossref",
"first-page": "957",
"journal-title": "Antioxid. Redox Signal.",
"key": "ref_84",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1093/humrep/dem146",
"article-title": "Effect of different contraceptive methods on the oxidative stress status in women aged 40–48 years from the ELAN study in the province of Liège, Belgium",
"author": "Pincemail",
"doi-asserted-by": "crossref",
"first-page": "2335",
"journal-title": "Hum. Reprod.",
"key": "ref_85",
"volume": "22",
"year": "2007"
},
{
"DOI": "10.1177/1535370216638770",
"article-title": "Detection of inflammatory biomarkers in saliva and urine: Potential in diagnosis, prevention, and treatment for chronic diseases",
"author": "Prasad",
"doi-asserted-by": "crossref",
"first-page": "783",
"journal-title": "Exp. Biol. Med.",
"key": "ref_86",
"volume": "241",
"year": "2016"
},
{
"DOI": "10.1016/j.cca.2012.06.012",
"article-title": "Urinary biomarkers of oxidative stress",
"author": "Scarbrough",
"doi-asserted-by": "crossref",
"first-page": "1446",
"journal-title": "Clin. Chim. Acta",
"key": "ref_87",
"volume": "413",
"year": "2012"
},
{
"DOI": "10.1155/2016/5480267",
"article-title": "Salivary and urinary total antioxidant capacity as biomarkers of oxidative stress in humans",
"author": "Peluso",
"doi-asserted-by": "crossref",
"first-page": "5480267",
"journal-title": "Pathol. Res. Int.",
"key": "ref_88",
"volume": "2016",
"year": "2016"
},
{
"DOI": "10.3390/antiox8090409",
"doi-asserted-by": "crossref",
"key": "ref_89",
"unstructured": "Maciejczyk, M., Szulimowska, J., Taranta-Janusz, K., Werbel, K., Wasileewska, A., and Zalewska, A. (2019). Salivary FRAP as a marker of chronic kidney disease progression in children. Antioxidants, 8."
},
{
"DOI": "10.1155/2019/4393460",
"article-title": "Salivary antioxidant barrier, redox status, and oxidative damage to proteins and lipids in healthy children, adults, and the elderly",
"author": "Macieczyk",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Oxid. Med. Cell. Longev.",
"key": "ref_90",
"volume": "2019",
"year": "2019"
},
{
"DOI": "10.3390/antiox6010005",
"doi-asserted-by": "crossref",
"key": "ref_91",
"unstructured": "Evan, L.W., and Omaye, S.T. (2017). Use of saliva biomarkers to monitor efficacy of vitamin C in exercise-induced oxidative stress. Antioxidants, 6."
},
{
"article-title": "Hydrogen peroxide release kinetics into saliva from different whitening products: A double-blind, randomized clinical trial",
"author": "Silveira",
"first-page": "155",
"journal-title": "Clin. Oral. Investig.",
"key": "ref_92",
"volume": "16",
"year": "2011"
},
{
"DOI": "10.1111/idh.12342",
"article-title": "Evaluation of substantivity of hypochlorous acid as an antiplaque agent: A randomized controlled trial",
"author": "Lafaurie",
"doi-asserted-by": "crossref",
"first-page": "527",
"journal-title": "Int. J. Dent. Hyg.",
"key": "ref_93",
"volume": "16",
"year": "2018"
},
{
"DOI": "10.3390/app10031037",
"doi-asserted-by": "crossref",
"key": "ref_94",
"unstructured": "Polizzi, A., Torrisi, S., Santonocito, S., Di Stefano, M., Indelicato, F., and Lo Giudice, A. (2020). Influence of myeloperoxidase levels on periodontal disease: An applied clinical study. App. Sci., 10."
},
{
"DOI": "10.1089/15230860260220175",
"article-title": "Oxidative stress and its role in skin disease",
"author": "Trouba",
"doi-asserted-by": "crossref",
"first-page": "665",
"journal-title": "Redox Signal.",
"key": "ref_95",
"volume": "4",
"year": "2002"
},
{
"article-title": "Intrinsic skin aging: The role of oxidative stress",
"author": "Dahmane",
"first-page": "33",
"journal-title": "Acta Derm. Alp. Pannonica Adriat.",
"key": "ref_96",
"volume": "21",
"year": "2012"
},
{
"article-title": "Free radicals and extrinsic skin aging",
"author": "Dahmane",
"first-page": "135206",
"journal-title": "Dermatol. Res. Pract.",
"key": "ref_97",
"volume": "2012",
"year": "2012"
},
{
"article-title": "Noninvasive method of determining skin antioxidant/oxidant activity: Clinical and cosmetics applications",
"author": "Brainina",
"first-page": "528",
"journal-title": "Anal. Bioanal. Electrochem.",
"key": "ref_98",
"volume": "5",
"year": "2013"
},
{
"DOI": "10.1111/j.1464-5491.1994.tb00375.x",
"article-title": "Low plasma ascorbate levels in patients with type 2 diabetes mellitus consuming adequate dietary vitamin C",
"author": "Sinclair",
"doi-asserted-by": "crossref",
"first-page": "893",
"journal-title": "Diabet. Med.",
"key": "ref_99",
"volume": "11",
"year": "1994"
},
{
"DOI": "10.1155/2020/4940673",
"article-title": "Association between serum vitamin C and the blood pressure: A systematic review and meta-analysis of observational studies",
"author": "Ran",
"doi-asserted-by": "crossref",
"first-page": "4940673",
"journal-title": "Cardiovasc. Ther.",
"key": "ref_100",
"volume": "2020",
"year": "2020"
}
],
"reference-count": 100,
"references-count": 100,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2227-9059/11/5/1308"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Biochemistry, Genetics and Molecular Biology",
"Medicine (miscellaneous)"
],
"subtitle": [],
"title": "A Pilot Study on Oxidative Stress during the Recovery Phase in Critical COVID-19 Patients in a Rehabilitation Facility: Potential Utility of the PAOT® Technology for Assessing Total Anti-Oxidative Capacity",
"type": "journal-article",
"volume": "11"
}