Evaluation of Glycemic Control and Predictors of Severe Illness and Death in Patients With Diabetes Hospitalized With COVID-19
et al., Journal of Community Hospital Internal Medicine Perspectives, doi:10.55729/2000-9666.1127, Nov 2022
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 733 hospitalized COVID-19 patients with diabetes in the USA, showing lower risk of severity with metformin use.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of severe case, 33.0% lower, OR 0.67, p = 0.03, treatment 377, control 356, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Milosavljevic et al., 9 Nov 2022, retrospective, USA, peer-reviewed, mean age 67.4, 7 authors, study period 1 March, 2020 - 31 December, 2020.
Contact: jovmilosa@gmail.com.
Evaluation of Glycemic Control and Predictors of Severe Illness and Death in Patients With Diabetes Hospitalized With COVID-19
Journal of Community Hospital Internal Medicine Perspectives, doi:10.55729/2000-9666.1127
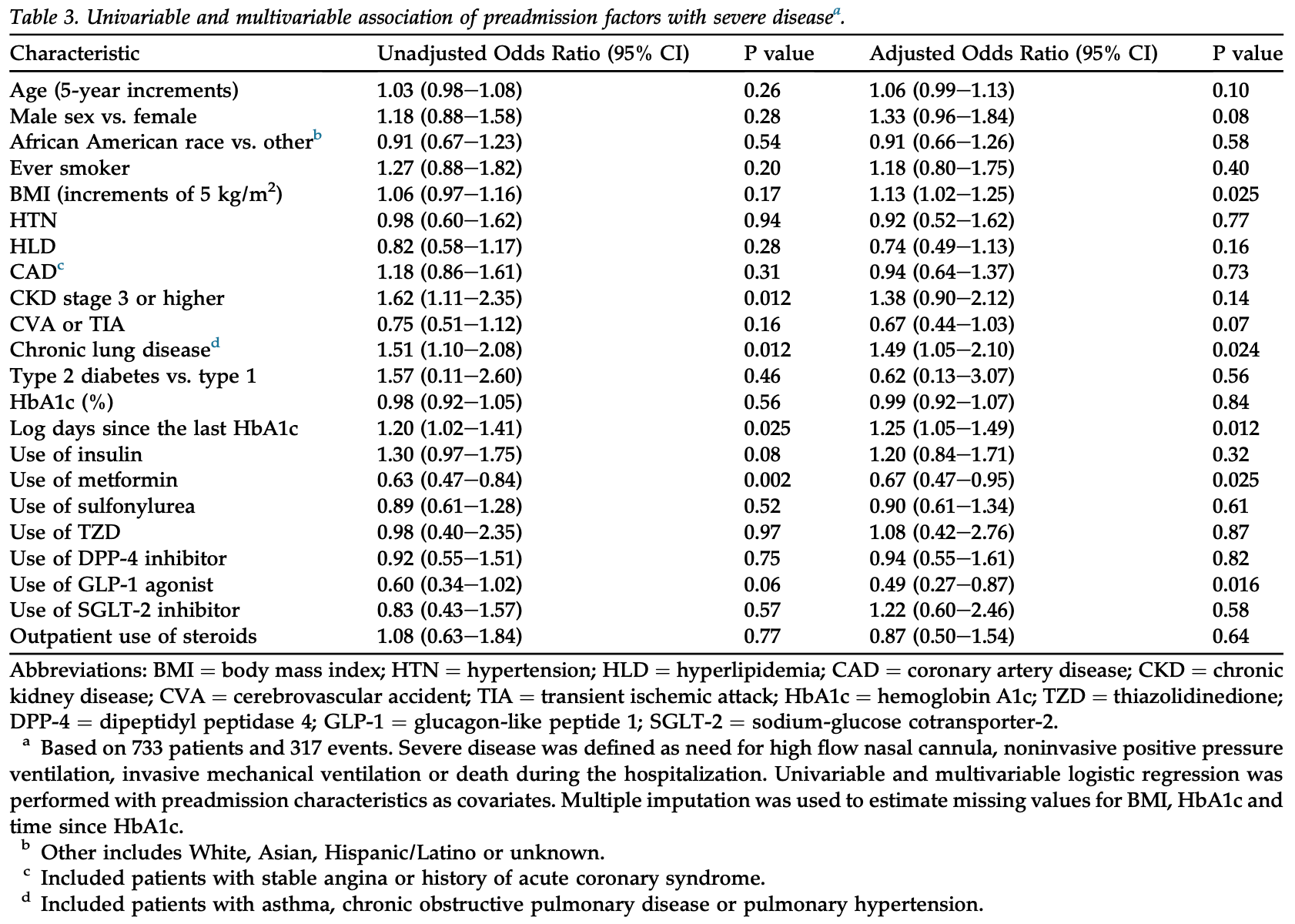
Objectives: To identify risk factors for severe disease and death among patients with diabetes and coronavirus disease 2019 (COVID-19) infection. Methods: This retrospective cohort study conducted at three hospitals included 733 consecutive patients with DM admitted with confirmed COVID-19 (March 1 -December 31, 2020). Multivariable logistic regression was performed to identify predictors of severe disease and death. Results: The mean age was 67.4 ± 14.3 years, 46.9% were males and 61.5% were African American. Among all patients, 116 (15.8%) died in the hospital. A total of 317 (43.2%) patients developed severe disease, 183 (25%) were admitted to an ICU and 118 (16.1%) required invasive mechanical ventilation. Increasing BMI (OR, 1.13; 95% CI, 1.02e1.25), history of chronic lung disease (OR, 1.49; 95% CI, 1.05e2.10) and increasing time since the last HbA1c test (OR, 1.25; 95% CI, 1.05e1.49) were the preadmission factors associated with increased odds of severe disease. Preadmission use of metformin (OR, 0.67; 95% CI, 0.47e0.95) or GLP-1 agonists (OR, 0.49; 95% CI, 0.27e0.87) was associated with decreased odds of severe disease. Increasing age (OR, 1.21; 95% CI, 1.09e1.34), co-existing chronic kidney disease greater than stage 3 (OR, 3.38; 95% CI, 1.67e6.84), ICU admission (OR, 2.93; 95% CI, 1.28e6.69) and use of invasive mechanical ventilation (OR, 8.67, 95% CI, 3.88e19.39) were independently associated with greater odds of in-hospital death. Conclusion: Several clinical characteristics were identified to be predictive of severe disease and in-hospital death among patients with underlying diabetes hospitalized with COVID-19.
Author contributions J.M.: data collection, data analysis, writing e original draft; N.P.: data collection, writing e original draft; M.T., S.J., J.L. and S.A.: data collection, writing e review & editing; A.T.: conceptualization, supervision, writing -review & editing. All authors read and approved the final manuscript.
Conflict of interest The authors declare that they have no competing or conflicts of interests.
References
Agarwal, Schechter, Southern, Crandall, Tomer, Preadmission diabetes-specific risk factors for mortality in hospitalized patients with diabetes and coronavirus disease 2019, Diabetes Care, doi:10.2337/dc20-1543
Aleem, Samad, Slenker, Emerging variants of SARS-CoV-2 and novel therapeutics against coronavirus (COVID-19)
Apicella, Campopiano, Mantuano, Mazoni, Coppelli et al., COVID-19 in people with diabetes: understanding the reasons for worse outcomes, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30238-2
Bai, Lian, Li, Zhang, Qiao, The active GLP-1 analogue liraglutide alleviates H9N2 influenza virus-induced acute lung injury in mice, Microb Pathog, doi:10.1016/j.micpath.2020.104645
Bello-Chavolla, Bahena, Opez, Ne, Predicting mortality due to SARS-CoV-2: a mechanistic score relating obesity and diabetes to COVID-19 outcomes in Mexico, J Clin Endocrinol Metab, doi:10.1210/clinem/dgaa346
Bode, Garrett, Messler, Glycemic characteristics and clinical outcomes of COVID-19 patients hospitalized in the United States, J Diabetes Sci Technol, doi:10.1177/1932296820924469
Buuren S Van, Groothuis-Oudshoorn, Mice: multivariate imputation by chained equations in R, J Stat Software, doi:10.18637/jss.v045.i03
Cariou, Hadjadj, Wargny, Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study, Diabetologia, doi:10.1007/s00125-020-05180-x
Dong, Du, Gardner, An interactive web-based dashboard to track COVID-19 in real time, Lancet Infect Dis, doi:10.1016/S1473-3099(20)30120-1
Hariyanto, Intan, Hananto, Putri, Kurniawan, Pre-admission glucagon-like peptide-1 receptor agonist (GLP-1RA) and mortality from coronavirus disease 2019 (Covid-19): a systematic review, meta-analysis, and metaregression, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2021.109031
Izcovich, Ragusa, Tortosa, Prognostic factors for severity and mortality in patients infected with COVID-19: a systematic review, PLoS One, doi:10.1371/journal.pone.0241955
Klonoff, Messler, Umpierrez, Association between achieving inpatient glycemic control and clinical outcomes in hospitalized patients with COVID-19: a multicenter, retrospective hospital-based analysis, Diabetes Care, doi:10.2337/dc20-1857
Kristan, Kim, Nelson, Predictors of severe COVID-19 in patients with diabetes: a multicenter review, Endocr Pract, doi:10.1016/j.eprac.2021.05.011
Leung, Niikura, Yang, Sin, COVID-19 and COPD, Eur Respir J, doi:10.1183/13993003.02108-2020
Liu, Zhang, Wang, Hyperglycemia is a strong predictor of poor prognosis in COVID-19, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108338
Marshall, Murthy, Diaz, A minimal common outcome measure set for COVID-19 clinical research, Lancet Infect Dis, doi:10.1016/S1473-3099(20)30483-7
Mehta, Kohn, Koliwad, Rushakoff, Lack of association between either outpatient or inpatient glycemic control and COVID-19 illness severity or mortality in patients with diabetes, BMJ Open Diabetes Res Care, doi:10.1136/bmjdrc-2021-002203
Mesas, Cavero-Redondo, Alvarez-Bueno, Predictors of in-hospital COVID-19 mortality: a comprehensive systematic review and meta-analysis exploring differences by age, sex and health conditions, PLoS One, doi:10.1371/journal.pone.0241742
Peters, Dixon, The effect of obesity on lung function, Expet Rev Respir Med, doi:10.1080/17476348.2018.1506331
Rosenthal, Cao, Gundrum, Sianis, Safo, Risk factors associated with in-hospital mortality in a US national sample of patients with COVID-19, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.29058
Wood, White, Royston, How should variable selection be performed with multiply imputed data?, Stat Med, doi:10.1002/sim.3177
Xian, Liu, Nilsson, Metformin inhibition of mitochondrial ATP and DNA synthesis abrogates NLRP3 inflammasome activation and pulmonary inflammation, Immunity, doi:10.1016/j.immuni.2021.05.004
Yan, Yang, Wang, Clinical characteristics and outcomes of patients with severe covid-19 with diabetes, BMJ Open Diabetes Research and Care, doi:10.1136/bmjdrc-2020-001343
Yang, Sun, Zhang, Zhang, The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2021.108977
Zhu, She, Cheng, Association of blood glucose control and outcomes in patients with COVID-19 and preexisting type 2 diabetes, Cell Metabol, doi:10.1016/j.cmet.2020.04.021
Zou, Hastie, Regularization and variable selection via the elastic net, J Roy Stat Soc B, doi:10.1111/j.1467-9868.2005.00503.x
DOI record:
{
"DOI": "10.55729/2000-9666.1127",
"ISSN": [
"2000-9666"
],
"URL": "http://dx.doi.org/10.55729/2000-9666.1127",
"author": [
{
"affiliation": [],
"family": "Milosavljevic",
"given": "Jovan",
"sequence": "first"
},
{
"affiliation": [],
"family": "Perkit",
"given": "Navya Reddy",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jhawar",
"given": "Sakshi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thomas",
"given": "Melbin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ling",
"given": "Justin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Amankwah",
"given": "Samuel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thomas",
"given": "Asha Mary",
"sequence": "additional"
}
],
"container-title": "Journal of Community Hospital Internal Medicine Perspectives",
"container-title-short": "Journal of Community Hospital Internal Medicine Perspectives",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
11,
10
]
],
"date-time": "2022-11-10T09:23:01Z",
"timestamp": 1668072181000
},
"deposited": {
"date-parts": [
[
2022,
11,
10
]
],
"date-time": "2022-11-10T09:23:01Z",
"timestamp": 1668072181000
},
"indexed": {
"date-parts": [
[
2022,
11,
11
]
],
"date-time": "2022-11-11T06:03:57Z",
"timestamp": 1668146637113
},
"is-referenced-by-count": 0,
"issue": "6",
"issued": {
"date-parts": [
[
2022,
11,
9
]
]
},
"journal-issue": {
"issue": "6",
"published-online": {
"date-parts": [
[
2022,
11,
9
]
]
}
},
"language": "en",
"member": "34701",
"original-title": [],
"page": "27-34",
"prefix": "10.55729",
"published": {
"date-parts": [
[
2022,
11,
9
]
]
},
"published-online": {
"date-parts": [
[
2022,
11,
9
]
]
},
"publisher": "Greater Baltimore Medical Center",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://scholarlycommons.gbmc.org/jchimp/vol12/iss6/5"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Internal Medicine"
],
"subtitle": [],
"title": "Evaluation of Glycemic Control and Predictors of Severe Illness and Death in Patients With Diabetes Hospitalized With COVID-19",
"type": "journal-article",
"volume": "12"
}
