Factors Associated with Adverse Outcomes among SARS-CoV-2 Positive Children in a Tertiary Government COVID-19 Referral Hospital in the Philippines
et al., Acta Medica Philippina, doi:10.47895/amp.v58i7.8392, Apr 2024
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000028 from 47 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
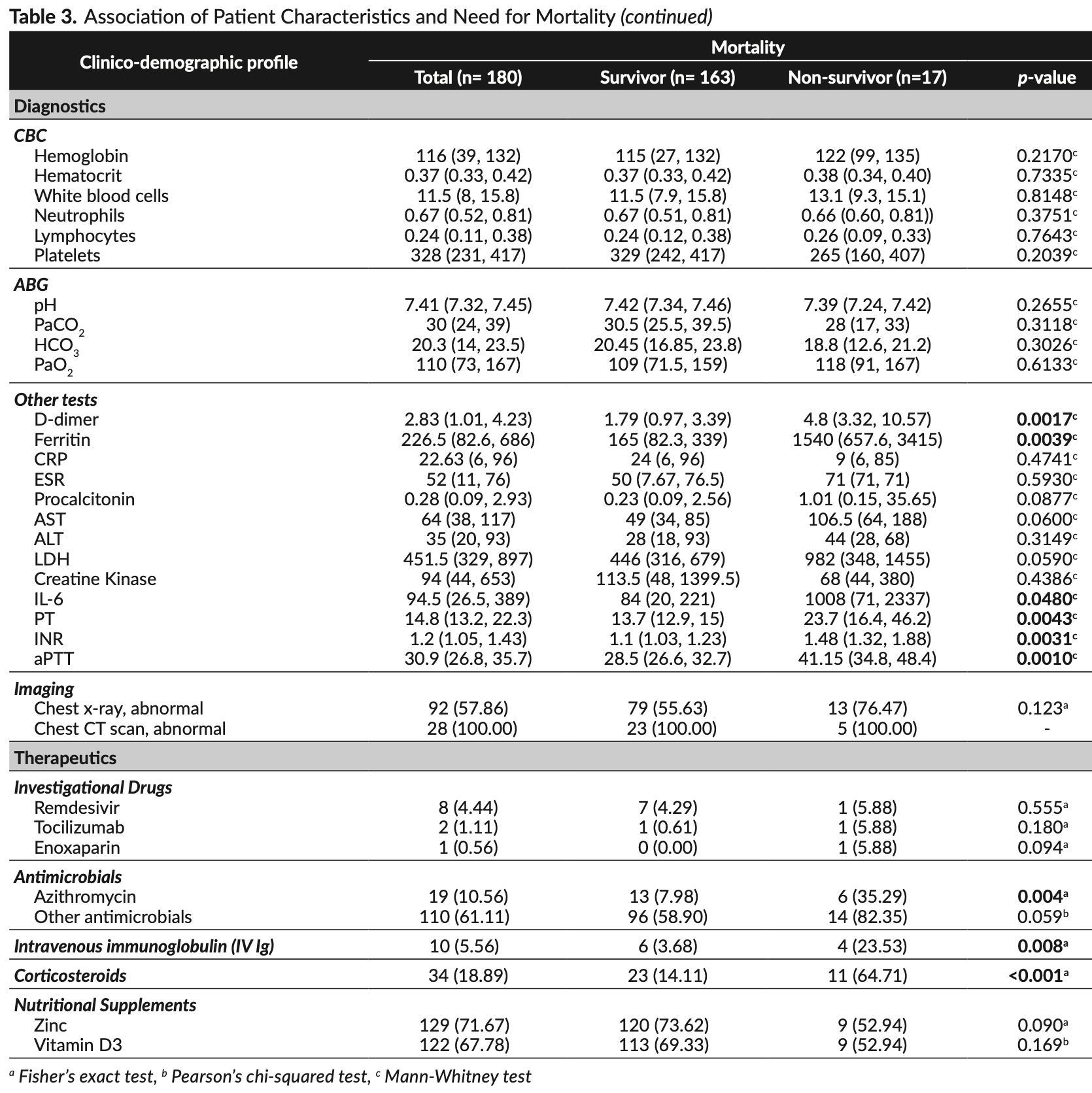
Retrospective 180 hospitalized pediatric COVID-19 patients in the Philippines showing lower mortality with vitamin D and zinc, and higher mortality with remdesivir, all without statistical significance. Remdesivir was given to few patients and authors do not provide information on the timing of treatment - confounding by indication may be significant.
Study covers zinc, vitamin D, and remdesivir.
|
risk of death, 55.5% lower, RR 0.44, p = 0.09, treatment 9 of 129 (7.0%), control 8 of 51 (15.7%), NNT 11, day 45.
|
|
risk of mechanical ventilation, 13.0% lower, RR 0.87, p = 0.67, treatment 22 of 129 (17.1%), control 10 of 51 (19.6%), NNT 39, day 45.
|
|
risk of ICU admission, 10.1% lower, RR 0.90, p = 0.84, treatment 25 of 129 (19.4%), control 11 of 51 (21.6%), NNT 46, day 45.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Milan et al., 30 Apr 2024, retrospective, Philippines, peer-reviewed, median age 11.0, 5 authors, study period 1 April, 2020 - 31 August, 2021.
Contact: markmilan31@gmail.com.
Factors Associated with Adverse Outcomes among SARS-CoV-2 Positive Children in a Tertiary Government COVID-19 Referral Hospital in the Philippines
Acta Medica Philippina, doi:10.47895/amp.v58i7.8392
Background and Objective. Pediatric COVID-19 epidemiology and factors associated with adverse outcomesmortality, need for invasive mechanical ventilation, and ICU admission, are largely unstudied. We described the clinicodemographic characteristics of Filipino pediatric COVID-19 patients and determined the factors associated with adverse outcomes. Methods. This is a retrospective cohort study of 180 hospitalized SARS-CoV-2-confirmed cases 0-18 years old from April 2020 to August 2021 in a tertiary COVID-19 referral hospital in Manila, National Capital Region. Crude associations were determined using chi-squared or Fisher's exact tests; and medians were compared using the Mann-Whitney test. Factors predictive of mortality were determined using Cox proportional hazards regression analysis. The survivor functions were depicted in graphs. Results. About 41.67% had mild disease, 58.33% were males, 39.4% aged 0-4 years, and 69.44% had at least one comorbidity. About 9.44% died (adjusted 9.2 persons per 1000 patient-days, 95% CI 5.5%-15.2%), 17.78% needed invasive mechanical ventilation, and 20% needed ICU admission. Independently, severe-critical COVID-19 (HRc 11.51, 95% CI 3.23, 41.06), retractions (HRc 10.30, 95% CI 3.27, 32.47), alar flaring (HRc 4.39, 95% CI 1.53, 12.58), cyanosis (HRc 4.39, 95% CI 1.72, 14.11), difficulty of breathing (HRc 7.99, 95% CI 2.25, 28.71), poor suck/appetite (HRc 4.46, 95% CI 1.59, 12.40), ferritin (HRc 1.01, 95% CI 1.00, 1.01), IL-6 (HRc 1.01, 95% CI 1.00, 1.01), aPTT (HRc 1.05, 95% CI 1.01, 1.10), IVIg (HRc 4.00, 95% CI 1.07, 14.92) and corticosteroid (HRc 6.01, 95% CI 2.04, 17.67) were significant hazards for mortality. In adjusted Cox analysis, only retractions (HRa 34.96, 95% CI 3.36, 363.79), seizure (HRa 9.98, 95% CI 1.76, 56.55), and corticosteroids (HRa 8.21, 95% CI 1.12, 60.38) were significantly associated with mortality while alar flaring appeared to be protective (HRa 0.10, 95% CI 0.01, 0.95). Several clinical characteristics were consistently associated with adverse outcomes. Conclusions. Majority of hospitalized pediatric COVID-19 patients were very young, males, had mild disease, and had at least one comorbidity. Mortality, invasive mechanical ventilation, and ICU admission were relatively low. Except for alar flaring which appeared to be protective, retractions, seizure, and use of corticosteroids were associated with adverse outcomes.
Statement of Authorship All authors certified fulfillment of ICMJE authorship criteria.
Author Disclosure All authors declared no conflicts of interest.
Appendix. Survival functions after Cox regression analysis, adjusted
References
Aimen, Attia, Junaid, Yasin, Farrah et al., Comorbidity and COVID-19 in children -a single center experience, Pak Pediatr J
Bai, Liu, Liu, Fu, Hu et al., Clinical analysis of 25 COVID-19 infections in children, Pediatr Infect Dis J, doi:10.1097/INF.0000000000002740
Campbell, Dubois, Savage, Hood-Pishchany, Sharma et al., Comorbidities associated with hospitalization and progression among adolescents with symptomatic Coronavirus Disease, J Pediatr, doi:10.1016/j.jpeds.2022.02.048
Castagnoli, Votto, Licari, Brambilla, Bruno et al., Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review, JAMA Pediatr, doi:10.1001/jamapediatrics.2020.1467
Chaiyakulsil, Sritipsukho, Satdhabudha, Bunjoungmanee, Tangsathapornpong et al., An epidemiological study of pediatric COVID-19 in the era of the variant of concern, PLoS One, doi:10.1371/journal.pone.0267035
Chilimuri, Sun, Alemam, Mantri, Shehi et al., Predictors of mortality in adults admitted with COVID-19: Retrospective cohort study from New York City, West J Emerg Med, doi:10.5811/westjem.2020.6.47919
Dessie, Zewotir, Mortality-related risk factors of COVID-19: A systematic review and meta-analysis of 42 studies and 423,117 patients, BMC Infect Dis, doi:10.1186/s12879-021-06536-3
Dong, Mo, Hu, Qi, Jiang et al., Epidemiology of COVID-19 among children in China, Pediatrics, doi:10.1542/peds.2020-0702
Fontana, Eagon, Trujillo, Scherer, Klein, Visceral fat adipokine secretion is associated with systemic inflammation in obese humans, Diabetes, doi:10.2337/db06-1656
Gonzalez-Dambrauskas, Vasquez-Hoyos, Camporesi, Cantillano, Dallefeld et al., Paediatric critical COVID-19 and mortality in a multinational prospective cohort, Lancet Reg Health Am, doi:10.1016/j.lana.2022.100272
Götzinger, Santiago-García, Noguera-Julián, Lanaspa, Lancella et al., COVID-19 Study Group. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study, Lancet Child Adolesc Health, doi:10.1016/S2352-4642(20)30177-2
Hoang, Chorath, Moreira, Evans, Burmeister-Morton et al., COVID-19 in 7780 pediatric patients: A systematic review, EClinicalMedicine, doi:10.1016/j.eclinm.2020.100433
Hobbs, Drobeniuc, Kittle, Williams, Byers et al., CDC COVID-19 Response Team. Estimated SARS-CoV-2 seroprevalence among persons aged <18 years-Mississippi, May-September 2020, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm7009a4
Kao, Orenstein, Anderson, The importance of advancing Severe Acute Respiratory Syndrome Coronavirus 2 vaccines in children, Clin Infect Dis, doi:10.1093/cid/ciaa712
Ladhani, Amin-Chowdhury, Davies, Aiano, Hayden et al., COVID-19 in children: analysis of the first pandemic peak in England, Arch Dis Child, doi:10.1136/archdischild-2020-320042
Lee, Chan, Hui, Ng, Wu et al., Effects of early corticosteroid treatment on plasma SARS-associated coronavirus RNA concentrations in adult patients, J Clin Virol, doi:10.1016/j.jcv.2004.07.006
Lima-Setta, Mc, Rodrigues-Santos, Das, Figueiredo et al., Multisystem inflammatory syndrome in children (MIS-C) during SARS-CoV-2 pandemic in Brazil: a multicenter, prospective cohort study, J Pediatr
Luca, Esposito, Cristiani, Mancino, Nenna et al., COVID-19 in children: A brief overview after three months experience, Paediatr Respir Rev, doi:10.1016/j.prrv.2020.05.006
Meena, Yadav, Saini, Yadav, Kumar, Clinical features and outcome of SARS-CoV-2 infection in children: A systematic review and meta-analysis, Indian Pediatr, doi:10.1007/s13312-020-1961-0
Oliveira, Colosimo, Simões, Silva, Mak et al., Clinical characteristics and risk factors for death among hospitalised children and adolescents with COVID-19 in Brazil: An analysis of a nationwide database, Lancet Child Adolesc Health, doi:10.1016/S2352-4642(21)00134-6
Otaola-Arca, Lara-Aguilera N Zuleta-Morales, Ortiz-Fritz, Multisystem inflammatory syndrome in children, Chile, May-August 2020, Emerg Infect Dis, doi:10.3201/eid2705.204591
Prata-Barbosa, Lima-Setta, Santos, Lanziotti, De Castro et al., Pediatric patients with COVID-19 admitted to intensive care units in Brazil: a prospective multicenter study, J Pediatr (Rio J), doi:10.1016/j.jped.2020.07.002
Sanchez-Larsen, Conde-Blanco, Viloria-Alebesque, Buendía, Oltra et al., COVID-19 prevalence and mortality in people with epilepsy: a nation-wide multicenter study, Epilepsy Behav, doi:10.1016/j.yebeh.2021.108379
Sharma, Kumar, Sodani, Sapre, Singh et al., Predictors of mortality in children admitted with SARS-COV-2 infection to a tertiary care hospital in North India, J Paediatr Child Health, doi:10.1111/jpc.15737
Toral, Alba, Molinaajr, The development of the Philippine General Hospital as a referral center in the COVID-19 pandemic: a qualitative study, Acta Med Philipp, doi:10.47895/amp.v55i2.2851
Tsankov, Allaire, Irvine, Lopez, Sauvé et al., Severe COVID-19 infection and pediatric comorbidities: A systematic review and meta-analysis, Int J Infect Dis, doi:10.1016/j.ijid.2020.11.163
Van Paassen, Vos, Hoekstra, Neumann, Boot et al., Corticosteroid use in COVID-19 patients: a systematic review and meta-analysis on clinical outcomes, Crit Care, doi:10.1186/s13054-020-03400-9
Wang, Yang, Chen, Guo, Liu et al., The proportion and effect of corticosteroid therapy in patients with COVID-19 infection: A systematic review and meta-analysis, PLoS One, doi:10.1371/journal.pone.0249481
Widjanarko, Nindya, Fernandez, Jovito, Comorbidities and COVID-19 severity in pediatric patients: systematic review and meta-analysis, Pediatrica Indonesiana, doi:10.14238/pi62.1.2022.51-60
Wong, Abbas, Chuah, Malisie, Pon et al., Comparative analysis of pediatric COVID-19 infection in Southeast Asia, South Asia, Japan, and China, Am J Trop MedHyg, doi:10.4269/ajtmh.21-0299
Wong-Chew, Noyola, Villa, Clinical characteristics and mortality risk factors in patients aged less than 18 years with COVID-19 in Mexico and Mexico City, An Pediatr, doi:10.1016/j.anpede.2022.03.001
Wu, Mcgoogan, Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention, JAMA, doi:10.1001/jama.2020.2648
Xue, Shen, COVID-19 in children and the importance of COVID-19 vaccination, World J Pediatr, doi:10.1007/s12519-021-00466-5
Yang, Sheng, Huang, Xiong, Jiang, Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: a multicentre, retrospective, cohort study, Lancet Oncol, doi:10.1016/S1470-2045(20)30310-7
Yonker, Shen, Kinane, Lessons unfolding from pediatric cases of COVID-19 disease caused by SARS-CoV-2 infection, Pediatr Pulmonol, doi:10.1002/ppul.24748
Zimmermann, Curtis, Coronavirus infections in children including COVID-19: an overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children, Pediatr Infect Dis J, doi:10.1097/INF.0000000000002660
DOI record:
{
"DOI": "10.47895/amp.v58i7.8392",
"ISSN": [
"2094-9278",
"0001-6071"
],
"URL": "http://dx.doi.org/10.47895/amp.v58i7.8392",
"abstract": "<jats:p>Background and Objective. Pediatric COVID-19 epidemiology and factors associated with adverse outcomes –mortality, need for invasive mechanical ventilation, and ICU admission, are largely unstudied. We described the clinicodemographic characteristics of Filipino pediatric COVID-19 patients and determined the factors associated with adverse outcomes.\r\nMethods. This is a retrospective cohort study of 180 hospitalized SARS-CoV-2-confirmed cases 0-18 years oldfrom April 2020 to August 2021 in a tertiary COVID-19 referral hospital in Manila, National Capital Region. Crudeassociations were determined using chi-squared or Fisher’s exact tests; and medians were compared using the Mann-Whitney test. Factors predictive of mortality were determined using Cox proportional hazards regression analysis. The survivor functions were depicted in graphs.\r\nResults. About 41.67% had mild disease, 58.33% were males, 39.4% aged 0-4 years, and 69.44% had at least onecomorbidity. About 9.44% died (adjusted 9.2 persons per 1000 patient-days, 95% CI 5.5%-15.2%), 17.78% needed invasive mechanical ventilation, and 20% needed ICU admission. Independently, severe-critical COVID-19 (HRc 11.51, 95% CI 3.23, 41.06), retractions (HRc 10.30, 95% CI 3.27, 32.47), alar flaring (HRc 4.39, 95% CI 1.53, 12.58), cyanosis (HRc 4.39, 95% CI 1.72, 14.11), difficulty of breathing (HRc 7.99, 95% CI 2.25, 28.71), poor suck/appetite (HRc 4.46, 95% CI 1.59, 12.40), ferritin (HRc 1.01, 95% CI 1.00, 1.01), IL-6 (HRc 1.01, 95% CI 1.00, 1.01), aPTT (HRc 1.05, 95% CI 1.01, 1.10), IVIg (HRc 4.00, 95% CI 1.07, 14.92) and corticosteroid (HRc 6.01, 95% CI 2.04, 17.67) were significant hazards for mortality. In adjusted Cox analysis, only retractions (HRa 34.96, 95% CI 3.36, 363.79), seizure (HRa 9.98, 95% CI 1.76, 56.55), and corticosteroids (HRa 8.21, 95% CI 1.12, 60.38) weresignificantly associated with mortality while alar flaring appeared to be protective (HRa 0.10, 95% CI 0.01,0.95). Several clinical characteristics were consistently associated with adverse outcomes.\r\nConclusions. Majority of hospitalized pediatric COVID-19 patients were very young, males, had milddisease, and had at least one comorbidity. Mortality, invasive mechanical ventilation, and ICU admission wererelatively low. Except for alar flaring which appeared to be protective, retractions, seizure, and use ofcorticosteroids were associated with adverse outcomes.\r\n </jats:p>",
"author": [
{
"ORCID": "http://orcid.org/0000-0001-7168-5076",
"affiliation": [],
"authenticated-orcid": false,
"family": "Milan, MD",
"given": "Mark Jason DC.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Molina, MD",
"given": "Al Joseph R.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ong-Lim, MD",
"given": "Anna Lisa T.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Uy, MD, MS",
"given": "Ma. Esterlita V.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Uy, MD",
"given": "Herbert G.",
"sequence": "additional"
}
],
"container-title": "Acta Medica Philippina",
"container-title-short": "Acta Med Philipp",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
4,
30
]
],
"date-time": "2024-04-30T08:34:23Z",
"timestamp": 1714466063000
},
"deposited": {
"date-parts": [
[
2024,
4,
30
]
],
"date-time": "2024-04-30T08:35:46Z",
"timestamp": 1714466146000
},
"indexed": {
"date-parts": [
[
2024,
5,
1
]
],
"date-time": "2024-05-01T00:28:51Z",
"timestamp": 1714523331228
},
"is-referenced-by-count": 0,
"issue": "7",
"issued": {
"date-parts": [
[
2024,
4,
30
]
]
},
"journal-issue": {
"issue": "7",
"published-online": {
"date-parts": [
[
2024,
4,
30
]
]
}
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc-nd/4.0",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
4,
30
]
],
"date-time": "2024-04-30T00:00:00Z",
"timestamp": 1714435200000
}
}
],
"link": [
{
"URL": "https://actamedicaphilippina.upm.edu.ph/index.php/acta/article/download/8392/5599",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://actamedicaphilippina.upm.edu.ph/index.php/acta/article/download/8392/5599",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "27557",
"original-title": [],
"prefix": "10.47895",
"published": {
"date-parts": [
[
2024,
4,
30
]
]
},
"published-online": {
"date-parts": [
[
2024,
4,
30
]
]
},
"publisher": "University of the Philippines Manila",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://actamedicaphilippina.upm.edu.ph/index.php/acta/article/view/8392"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Factors Associated with Adverse Outcomes among SARS-CoV-2 Positive Children in a Tertiary Government COVID-19 Referral Hospital in the Philippines",
"type": "journal-article",
"volume": "58"
}
